This editorial refers to ‘Physical activity and fitness in the community: the Framingham Heart Study’ by M. Nayor et al.,doi:10.1093/eurheartj/ehab580.
The transportation of oxygen from ambient air to various cells throughout our body is pivotal for sustaining the function of the body and life, requiring adequate function of pulmonary ventilation and gas diffusion, oxygen transport by haemoglobin, as well as cardiac and vascular function. Indeed, diagnosing and treating the pathophysiological processes affecting this chain of oxygen transport represents the daily bread and butter in clinical practice for numerous medical professionals. Thus, it is not surprising that cardiorespiratory fitness, referring to the ability of the cardiovascular and respiratory systems to supply oxygen during sustained physical activity, has been established as a powerful predictor of mortality and cardiovascular disease,1 as well as several other clinically important conditions.2 The possible clinical utility of cardiorespiratory fitness measured as peak oxygen uptake (VO2peak) by gold-standard cardiopulmonary exercise testing has also been shown by improving risk prediction of coronary heart disease when adding VO2peak to established risk prediction models.3
Regular physical activity improves VO2peak, but most of the previous large population studies looking into the associations between physical activity and cardiorespiratory fitness have used self-reported measures of physical activity, susceptible to recall and social desirability bias, or they have used measures of fitness less accurate than VO2peak directly measured by cardiopulmonary exercise testing. In this issue of the European Heart Journal, Nayor and colleagues4 report associations between different components of accelerometry-measured physical activity obtained twice over an 8-year time span with directly measured VO2peak measured on the second occasion. Data were gathered as a part of the Framingham Heart Study including data from 1720 community-dwelling middle-aged adults on both occasions. Although also presenting cross-sectional data from 2070 individuals, the authors deserve particular credit for the reported associations between changes in different components of physical activity with VO2peak and other oxygen uptake kinetics during various phases of exercise, including initiation, early and late phase, peak, and recovery. Their repeated measures of objectively measured physical activity over the 8-year period, one of the notable features of the study, showed how a 17 min increase in daily moderate to vigorous physical activity had a similar effect on VO2peak as reducing sedentary time by roughly 4 h per day or by walking 4300 extra steps. Although the numbers show that moderate to vigorous physical activity is more time efficient in increasing VO2peak, and that we maybe should ‘make the steps count’ more than count the steps, the results for steps walked were actually quite encouraging. Light physical activity such as daily steps is hard to quantify by self-report since it is often incidental and unplanned, and thus these results based on objective measures add significantly to the literature indicating that incidental physical activity also has a role in maintaining cardiorespiratory fitness. Larger effect sizes for oxygen uptake kinetic measures such as, but not limited to, oxygen uptake efficiency slope, VO2 at ventilatory anaerobic threshold, VO2/work slope, oxygen pulse, and VO2 recovery delay were seen for the moderate to vigorous physical activity measures compared with both sedentary time and steps per day. These measures are of interest not only because they are valuable in, for example, heart failure evaluation,5–7 but also because several of them do not require maximal effort. Thus, they may be more accessible in diagnostic settings for patients not willing or able to exercise to exhaustion, and they may also be used to monitor physical activity interventions, as the authors pointed out.
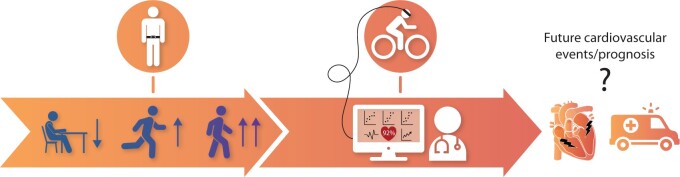
However, prognostic implications of several of the oxygen uptake kinetic measures have not been extensively studied in free-living individuals or unselected populations. Such data would add to the current findings and deserve focus in future studies. This was also touched upon in the 2016 focused update on cardiopulmonary exercise testing in specific patient populations from the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) and the American Heart Association (AHA), where the need for research on the clinical impact of exercise testing in apparently healthy populations was highlighted.8 The study by Nayor and colleagues is a step on the way to increasing knowledge of the utility of exercise testing in general populations. However, there is still work to be done before the clinical impact of several of their findings is well defined (Graphical Abstract).
Graphical Abstract.
Repeated measures of accelerometry-measured daily moderate to vigorous physical activity, step count, and sedentary time were associated with VO2peak and oxygen uptake kinetics at various stages of exercise. However, how the oxygen uptake kinetic measures beside VO2peak are related to future cardiac conditions and prognosis in the general population is largely unknown.
Although the study investigated several interesting aspects, it also helps in identifying some knowledge gaps deserving further research. For example, although the authors elegantly evaluated key components of physical activity, it would have been interesting to see the associations for moderate and vigorous intensity physical activity separately, as some studies have indicated larger effects on VO2peak of high-intensity exercise compared with moderate intensity in both healthy and diseased individuals.9 Also, repeated measures of VO2peak would have strengthened their design, and it is worth noting that VO2peak was measured using cycle ergometry, which is known to yield lower VO2peak values than treadmill exercise in general populations.10 However, even when considering the impact of exercise modality on VO2peak, the mean VO2peak of 23.6 mL/kg/min from the current study is lower than values seen in studies from Europe,11 , 12 probably partly explained by, for example, the higher body mass index in the present sample. This implies that generalization of findings should be done with caution. For example, in a fitter sample, the number of steps per day, mostly reflecting low-intensity physical activity, may not have shown the same effect on VO2peak or oxygen uptake kinetics as was found here. Finally, their study is an example of the vast amount of information available from exercise testing and, with present-day and future’s developments in technology and informatics, it is obvious that we might just have seen a glimpse of the potential impact of exercise testing in cardiopulmonary medicine.
In the end, Nayor and colleagues have some encouraging findings which should resonate in the general public as well, as their findings indicate that moderate increases in daily walking or slight increases in moderate to vigorous physical activity may compensate our increasingly sedentary lifestyle. Although the reported effect estimates may seem small, when considering the strong relationship between cardiorespiratory fitness and health outcomes, the benefit on the health of a population by modest increases in regular activity may be substantial.
Funding
None declared.
Conflict of interest: none declared.
Contributor Information
Jon Magne Letnes, Department of Circulation and Medical Imaging, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology, Trondheim, Norway; Clinic of Cardiology, St Olavs University Hospital, Trondheim, Norway.
Bjarne M Nes, Department of Circulation and Medical Imaging, Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology, Trondheim, Norway; Clinic of Cardiology, St Olavs University Hospital, Trondheim, Norway.
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
References
- 1. Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, Sugawara A, Totsuka K, Shimano H, Ohashi Y, Yamada N, Sone H. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women. JAMA 2009;301:2024–2035. [DOI] [PubMed] [Google Scholar]
- 2. Ross R, Blair SN, Arena R, Church TS, Després J-P, Franklin BA, Haskell WL, Kaminsky LA, Levine BD, Lavie CJ, Myers J, Niebauer J, Sallis R, Sawada SS, Sui X, Wisløff U. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a Scientific Statement from the American Heart Association. Circulation 2016;134:e653–e699. [DOI] [PubMed] [Google Scholar]
- 3. Letnes JM, Dalen H, Vesterbekkmo EK, Wisløff U, Nes BM. Peak oxygen uptake and incident coronary heart disease in a healthy population: the HUNT Fitness Study. Eur Heart J 2019;40:1633–1639. [DOI] [PubMed] [Google Scholar]
- 4. Nayor M, Chernofsky A, Spartano NL, Tanguay M, Blodgett JB, Murthy VL, Malhotra R, Houstis NE, Velagaleti RS, Murabito JM, Larson MG, Vasan RS, Shah RV, Lewis GD. Physical activity and fitness in the community: the Framingham Heart Study. Eur Heart J 2021;42:4565–4575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guazzi M, Adams V, Conraads V, Halle M, Mezzani A, Vanhees L, Arena R, Fletcher GF, Forman DE, Kitzman DW, Lavie CJ, Myers J. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Eur Heart J 2012;33:2917–2927. [DOI] [PubMed] [Google Scholar]
- 6. Agostoni P, Dumitrescu D. How to perform and report a cardiopulmonary exercise test in patients with chronic heart failure. Int J Cardiol 2019;288:107–113. [DOI] [PubMed] [Google Scholar]
- 7. Bailey CS, Wooster LT, Buswell M, Patel S, Pappagianopoulos PP, Bakken K, White C, Tanguay M, Blodgett JB, Baggish AL, Malhotra R, Lewis GD. Post-exercise oxygen uptake recovery delay: a novel index of impaired cardiac reserve capacity in heart failure. JACC: Heart Fail 2018;6:329–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guazzi M, Arena R, Halle M, Piepoli MF, Myers J, Lavie CJ. 2016 focused update: clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Eur Heart J 2018;39:1144–1161. [DOI] [PubMed] [Google Scholar]
- 9. Wisløff U, Støylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram PM, Tjønna AE, Helgerud J, Slørdahl SA, Lee SJ, Videm V, Bye A, Smith GL, Najjar SM, Ellingsen Ø, Skjærpe T. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation 2007;115:3086–3094. [DOI] [PubMed] [Google Scholar]
- 10. Kaminsky LA, Imboden MT, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing using cycle ergometry: data from the Fitness Registry and the Importance of Exercise National Database (FRIEND) registry. Mayo Clin Proc 2017;92:228–233. [DOI] [PubMed] [Google Scholar]
- 11. Kaminsky LA, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing data from the Fitness Registry and the Importance of Exercise National Database. Mayo Clin Proc 2015;90:1515–1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rapp D, Scharhag J, Wagenpfeil S, Scholl J. Reference values for peak oxygen uptake: cross-sectional analysis of cycle ergometry-based cardiopulmonary exercise tests of 10 090 adult German volunteers from the Prevention First Registry. BMJ Open 2018;8:e018697. [DOI] [PMC free article] [PubMed] [Google Scholar]