Abstract
Objective
This study was undertaken to elucidate the mechanism of improved chondrocyte migration after juvenile articular cartilage fragmentation.
Design
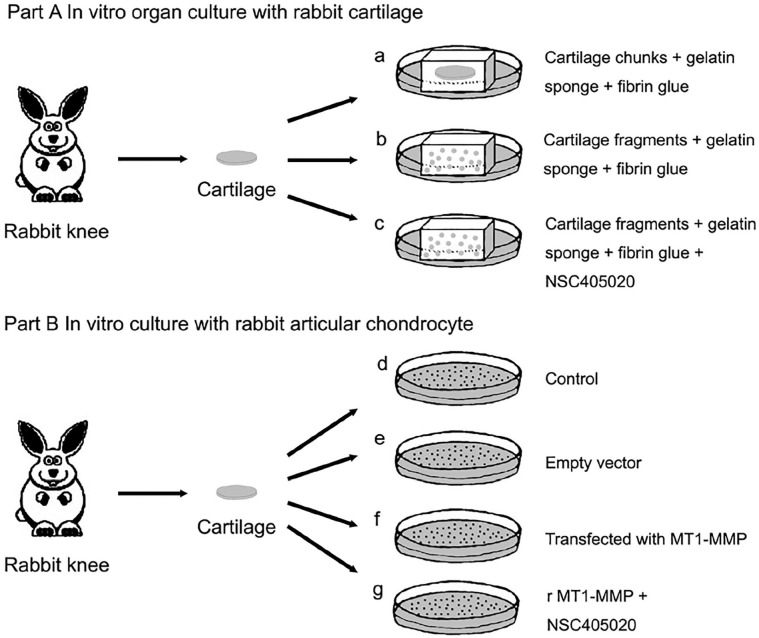
In vitro organ culture with rabbit cartilage fragments and cell culture with rabbit chondrocytes were performed. In part A, minced juvenile cartilage fragments (~0.5 × 0.5 × 0.5 mm) from rabbits, planted in gelatin sponge and fibrin glue, were cultured for 2, 4, or 6 weeks in vitro and compared with the cartilage chunks (~4 × 4 × 1 mm) and membrane type 1 matrix metalloprotease (MT1-MMP) inhibitor groups. Chondrocyte outgrowth was evaluated on histology and confocal laser scanning microscopy. MT1-MMP expression was compared between the cartilage fragment group and the cartilage chunks group. In part B, articular chondrocytes were harvested from juvenile rabbits, MT1-MMP was transfected into the cells, and cell migration was evaluated using the Transwell and wound healing tests.
Results
The histology and confocal microscopy results revealed that cell accumulation occurred at the edge of cartilage fragments, and outgrowth was better in the cartilage fragment group than those in the cartilage chunks group. Similar results were observed for MT1-MMP expression. After MT1-MMP inhibition, cells did not accumulate at the edge of the cartilage fragments, and chondrocyte outgrowth did not occur. Furthermore, overexpression of MT1-MMP enhanced the migration of articular chondrocytes.
Conclusions
Juvenile articular cartilage fragmentation improved chondrocyte migration by upregulating MT1-MMP.
Keywords: cartilage fragmentation, chondrocyte outgrowth, in vitro, MT1-MMP
Introduction
Particulated juvenile articular cartilage (PJAC; DeNovo NT; Zimmer Biomet Inc., Warsaw, IN, USA) allografts are novel biologics 1 used to repair osteochondral lesions of the knee,2,3 ankle, 4 shoulder, 5 wrist, 6 and metatarsal head. 7 Use of PJAC results in high clinical success rates, as the repaired cartilage is similar to hyaline cartilage.2,4,8 The PJAC will produce and/or maintain a cartilaginous matrix similar to native cartilage, thereby facilitating repair. 9 Cartilage minced into fragments increases tissue surface area, enabling cells that are essential for cartilage repair to migrate to defects and provide more space for proliferation.10,11 Increased cellular outgrowth from the minced cartilage fragments has been confirmed by several authors.10 -15 However, the molecular mechanism remains unclear.
The theory behind PJAC is that implanting healthy juvenile cartilage has a greater chondrogenic potential than using adult cartilage. 16 Recent reports have provided compelling evidence that juvenile chondrocytes are more efficient than adult chondrocytes at generating articular cartilage.17,18 Gene expression analysis indicated that cartilage developmental pathways are overrepresented in juvenile chondrocytes compared with adult chondrocytes. 19 In a study by Marmotti et al., 12 a histologic analysis showed that chondrocyte migration increased after human cartilage fragmentation, and that chondrocyte migration of young donors was better than that of older donors. Membrane type 1 matrix metalloproteinase (MT1-MMP), also called MMP 14, is highly expressed in juvenile cartilage compared with adult cartilage. 16 MT1-MMP plays an important role in cell migration, and could be responsible for the superior migration of chondrocytes in juvenile cartilage.
The purpose of this study was to investigate the molecular mechanism of increased chondrocyte outgrowth after juvenile cartilage fragmentation. It was hypothesized that (1) outgrowth of chondrocytes would be increased in juvenile cartilage fragments compared with juvenile cartilage chunks, (2) expression of MT1-MMP would be increased after fragmentation of juvenile cartilage, and (3) overexpression of MT1-MMP would enhance migration of articular chondrocytes.
Methods
Approvals were obtained from the Ethical Committee of the First Affiliated Hospital of University of South China. Care for the animals was in accordance with the “Guiding Directives for Human Treatment of Laboratory Animals” issued by the National Ministry of Science and Technology (2006). The study experimental design is depicted in Figure 1 .
Figure 1.
Study design. Part A shows the in vitro organ culture of rabbit cartilage. Cartilage chunks were loaded onto the gelatin sponge and fibrin glue scaffolds and cultured in normal media (a). Minced cartilage fragments were loaded onto the gelatin sponge and fibrin glue scaffolds and cultured in normal media (b) or media containing the membrane type 1 matrix metalloprotease (MT1-MMP) inhibitor, NSC405020 (c). Part B shows the in vitro cell culture with rabbit articular chondrocytes. Rabbit articular chondrocytes were cultured in normal media (d), normal media + an empty vector (e), normal media + a vector-transfected with MT1-MMP (f), and a vector-transfected with MT1-MMP + media containing the MT1-MMP inhibitor, NSC405020 (g).
Part A: In Vitro Organ Culture with Rabbit Cartilage
An In Vitro Culture Model: Minced Juvenile Cartilage Fragment
Fifty 4-week-old immature New Zealand White rabbits (Animal Laboratories of the University of South China, Hengyang, China) were euthanized by cervical dislocation, and bilateral knee joints were peeled off under sterile conditions. Ninety-nine cartilage chunks (~4 × 4 × 1 mm) were obtained from the femoral trochlea of both knees using a No. 10 scalpel while avoiding the harvest of the physis and bone. Cartilage chunks were excised and rinsed 3 times in phosphate-buffered saline (PBS, Procell, Wuhan, China) containing penicillin and streptomycin (Procell), transferred to a Petri dish, and divided into three groups. Group A was a control group with cartilage chunks (n = 33), in group B (cartilage fragments, n = 33) and group C (cartilage fragments + an MT1-MMP inhibitor, n = 33), the cartilage was chopped with a sterile scalpel into small fragments (~0.5 × 0.5 × 0.5 mm) under sterile conditions in transfer PBS medium.
Cartilage fragments (10-15 mg) were evenly seeded on gelatin sponge (1 × 1× 3 mm), retained in a coating of approximately 200 µL of fibrin glue (Lai Shi, Shanghai, China), and stabilized using 200 µL of thrombin previously diluted with 500 IU/mL calcium chloride.
Explants (n = 33/treatment) were placed in 6-well plates and incubated for 1 hour at 37 °C in 5 mL of Dulbecco’s modified Eagle’s medium (DMEM; Hyclone, Logan, UT, USA) containing 1,000 units/mL of penicillin/streptomycin and 25 g/mL fungizone (Sigma, St. Louis, MO, USA). The explants were cultured at 37 °C in an atmosphere of 5% CO2 and 95% air in DMEM, containing 10% heat-inactivated fetal bovine serum, 0.1 mM nonessential amino acids, 10 mM HEPES buffer solution, 100 U/mL penicillin/streptomycin, 0.25 g/mL fungizone, and 37.5 g/mL l-ascorbic acid 2-phosphate (Sigma). In group C, an MT1-MMP inhibitor (NSC405020, Selleck, Shanghai, China) was added to the culture medium. The explants were cultured for 2, 4, or 6 weeks. The medium was replaced every 3 days, and the plates were replaced weekly. The explants were assessed by histology, confocal laser scanning microscopy (CLSM), and immunofluorescence.
Histologic Evaluation
The explants (n = 8/treatment/time point, total 24 in every group) used for the histologic evaluation were fixed in formalin and embedded in paraffin. Sections (5-μm thick) were cut and stained with hematoxylin and eosin (H&E). A pathologist blinded to the treatment groups quantified the histologic findings on the H&E sections using a 0- to 3-point scale 11 (0, no cell outgrowth; 1, cell accumulation at the edge of the fragments; 2, outgrowth without matrix formation; 3, cell outgrowth with matrix formation).
Confocal Laser Scanning Microscopy
To assess cell accumulation at the edge of the fragments and outgrowth from the fragments, the explants (n = 3/treatment/time point, total 9 in every group) were stained with reagents from the Viability/Cytotoxicity Assay Kit for Animal Live and Dead Cells (Biotium Inc., Hayward, CA, USA). Briefly, the explants were labeled for 30 minutes with 6 µL of EthD-III (ethidium homodimer III) and 3 µL of calcein AM (calcein acetoxymethyl ester) in 3 mL of PBS and washed 3 times in PBS. Images of the interface were obtained with a CLSM system (LSM510; Carl Zeiss Instruments, Thornwood, NY, USA).
Immunofluorescence Evaluation
Immunofluorescence staining was performed in groups A and B using a primary mouse monoclonal antibody against MT1-MMP. Sections were incubated overnight at 4 °C with the primary antibody and treated with biotinylated goat anti-mouse IgG (Abcam, Cambridge, MA, USA) for 15 minutes at room temperature. PBS was used as a negative control. Nuclei were stained with DAPI. The difference in fluorescence intensity was evaluated semiquantitatively using Image J software. 10
Part B: In Vitro Culture of Rabbit Articular Chondrocytes
Five New Zealand White rabbits (Centers for Disease Control and Prevention, Hubei, China) aged 2 to 3 weeks were euthanized by cervical dislocation, and bilateral knee joints were peeled off under sterile conditions. Articular cartilage was excised and rinsed 3 times in PBS (Procell, Wuhan, China) containing penicillin and streptomycin (Procell). The cartilage was minced and transferred to a culture dish containing 0.2% collagenase II (Sigma, St. Louis, MO, USA) and shaken in a 37 °C water bath for 4 to 6 hours. Digestion was stopped, and large tissues were disrupted in the liquid by gently blowing with a pipette. The digested tissue/cell suspension was centrifuged at 300 × g for 5 minutes, and the precipitate was resuspended in DMEM containing 10% heat-inactivated fetal bovine serum, 0.1 mM nonessential amino acids, 10 mM HEPES buffer solution, 100 U/mL penicillin/streptomycin, 0.25 g/mL fungizone, and 37.5 g/mL l-ascorbic acid 2-phosphate (Sigma). The cells were incubated in a 37 °C, 5% CO2 incubator, and the medium was changed every 3 days until the cells reached 80% to 90% confluence, as determined under a microscope. Then the cells were subcultured. The chondrocytes were identified with type II collagen immunofluorescence. Third passage cells were used for all the experiments to allow for sufficient expansion of the cells. Chondrocytes came from 5 different rabbits cultured separately.
Recombinant AdMaxTM Adenovirus Vector Packaging, Purification, and Titration
Rabbit MT1-MMP cDNA (1,767 bp) was obtained from Sino Biological Inc. (Beijing, China). The recombinant AdMaxTM packaging plasmid was obtained by simultaneously digesting the pDC316-mCMV-tdTomato plasmid (Wuhan Viral Therapy Technologies, Co. Ltd., Wuhan. China) with NheIase and NotIase (New England Biolabs, Beverly, MA, USA). Rabbit MT1-MMP cDNA and the recombinant AdMaxTM packaging plasmid were integrated using T4 DNA ligase (New England Biolabs). The integrated product was used to transfect JM109 competent cells (Wuhan Viral Therapy Technologies) and cultured in an agarose medium containing ampicillin (Aladdin, Shanghai, China). Monoclonal colonies were selected and inoculated into Luria broth (LB) culture media (Biofavor Biotech, Co. Ltd., Wuhan, China) containing ampicillin overnight. The pDC316-mCMV-tdTomato-rMT1-MMP plasmid was extracted, and the base sequence was analyzed. Then, HEK293 cells were transfected with the purified pDC316-mCMV-tdTomato-rMT1-MMP plasmid using Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA). The third passage virus was purified using a ViraBind Adenovirus Purification Kit VPK-100 (Cell Biolabs, San Diego, CA, USA), followed by the determination of virus biological titers (virus titer = 1 × 1010 PFUs [plaque forming units]/mL).
Adenoviral Transduction
Each primary rabbit chondrocytes sample was divided into 4 parts and plated separately at a density of 5 × 105 cells/well in12-well plates, and only 4 wells were used in each plate. The first well was left untreated (Control group). In the second well, the cells were incubated with the Ad5-pDC316-mCMV-tdTomato empty vector (empty vector group). The 2 remaining wells were incubated with the Ad5-pDC316-mCMV-tdTomato-rMT1-MMP vector at 37 °C with an MOI (multiplicity of infection) of 50 (rMT1-MMP group), 1 of the 2 wells transfected with MT1-MMP were cultured in media containing 100 μM NSC405020 for 24 hours until after the transfection was completed (rMT1-MMP + NSC405020group).
Transwell Filter Migration Assay
Chondrocyte migration was evaluated using the Transwell plate according to a previously described protocol. 20 The cells of each group were centrifuged (1,000 rpm for 5 minutes) separately and collected. Transwell filters (BD Life Sciences, San Jose, CA, USA) with 8.0 μm pores were used for the migration assay. A 600-μL aliquot of articular chondrocyte complete medium was added to the outer chambers of the 24-well plate, and the inner chambers were filled with 200 μL of each cell suspension (cells were diluted to 5 × 105 cell/mL using serum-free DMEM/F12 medium) and incubated for 48 hours at 37 °C. The migrated cells of the upper chamber were fixed with 4% paraformaldehyde and stained with crystal violet (Aladdin) for 20 minutes at room temperature. The cells on the upper surface of the filter were wiped off with a cotton swab, and the cells that migrated to the lower surface of the filter were photographed under a microscope. Five randomized fields on each filter were observed, and the cells were counted and calculated. Five independent experiments were carried out.
Wound Healing/Scratch Assay
The wound healing/scratch test was performed according to a previously described protocol. 21 Briefly, 4 groups of chondrocytes were seeded into 6-well plates. After cell confluence reached 90%, similar straight scratches were made in the monolayers of each well using a 10-μL sterile pipette tip. This was followed by 3 washes with PBS. At the 0-, 24-, and 48-hour time points, 3 photomicrographs were taken of each wound (at 100× magnification). The area between the wound edges was measured and analyzed using Image J software (National Institutes of Health, Bethesda, MD, USA).The average area of the 3 photomicrographs was reconded. Five independent experiments were carried out.
Statistical Analysis
Differences in the histologic, immunofluorescence, transwell filter migration, and wound healing/scratch assay results were evaluated among the groups using the Kruskal-Wallis H test. The Mann-Whitney U test was used for paired comparisons. Data were analyzed with SPSS 17.0 software (IBM Corp., Armonk, NY, USA). A P value <0.05 was considered significant.
Results
Part A: In Vitro Organ Culture with Rabbit Cartilage Fragments
Histological Evaluation
Representative H&E-stained images are shown in Figure 2 . Cells accumulated at the edge of the fragments in group A that were similar at 2, 4, and 6 weeks (P > 0.05). Cell outgrowth increased over time in group B (P < 0.01). Chondrocyte release from the cartilage fragments into the scaffolds in group B were detected at 2 weeks. Chondrocyte outgrowth increased at 4 weeks. More chondrocytes accumulated in the scaffolds at 6 weeks, and the synthesis of extracellular matrix was detected. No chondrocyte outgrowth was detected in group C at any time point (P > 0.05). Group B had higher histology score than groups A and C at 2, 4,and 6 weeks (P < 0.01) ( Table 1 ).
Figure 2.
Histologic analysis of chondrocyte outgrowth. Sections of paraffin-embedded juvenile cartilage explants were sectioned and stained with hematoxylin and eosin (H&E). Scale bar = 500 μm. C, cartilage tissue; O, outgrowth of chondrocytes.
Table 1.
Histological Scores of Chondrocyte Outgrowth at 2, 4, and 6 Weeks, and Immunofluorescence Semiquantitative Analysis of Fluorescence Intensity of Membrane Type 1 Matrix Metalloproteinase (MT1-MMP) at 0, 2, and 4 weeks a .
| Group A | Group B | Group C | |
|---|---|---|---|
| Histology | |||
| 2 weeks | 0.50 ± 0.54 | 1.88 ± 0.35 b | 0.00 ± 0.00 c |
| 4 weeks | 0.75 ± 0.46 | 2.25 ± 0.46 b | 0.13 ± 0.35 c |
| 6 weeks | 0.75 ± 0.46 | 2.75 ± 0.46b,d | 0.13 ± 0.35 c |
| Immunofluorescence | |||
| 0 weeks | 430.00 ± 67.82 | 438.00 ± 42.48 | |
| 2 weeks | 770.50 ± 107.77 | 3171.50 ± 464.11 b | |
| 4 weeks | 981.88 ± 177.42 | 4849.25 ± 602.33 b | |
Histological evaluation and immunofluorescence data are presented as means ± standard deviations.
Indicates significant difference compared with group A.
Indicates significant difference compared with group B.
Indicates significant difference along with the time points.
Confocal Laser Scanning Microscopy
Representative images are shown in Figure 3 . Cell outgrowth was detected in group B at 2 weeks but not in group A or C. Cell outgrowth increased in group B at 4 weeks. Cell accumulation was detected at the edge of the cartilage chunks in group A. No cell accumulation or outgrowth was observed in group C. Cell outgrowth into the scaffolds increased after 6 weeks in group B. Cell accumulation at the edge of the cartilage chunks and a blank cell-free zone were found along the edge of the cartilage columns in group A, indicating complete release of the cells to the edge. No cell accumulation or outgrowth was found in group C.
Figure 3.
Cell accumulation at the fragments edges and fragment outgrowth was observed by confocal laser scanning microscopy. Frozen sections were sectioned and stained with EthD-III (ethidium homodimer III) and calcein AM (calcein acetoxymethyl ester). Scale bar = 200 μm. C, cartilage tissue; O, outgrowth of chondrocytes; green indicates live cells, red indicates dead cells, arrows indicate cell accumulation at the edge of the cartilage fragments. Scale bar = 200 μm.
Immunofluorescence
A semiquantitative comparative analysis of fluorescence intensities in the different cell populations using Image J software showed increased MT1-MMP expression in groups A and B over time (P < 0.05). Additionally, the fluorescence intensity in group B was higher than that in group A at 2 and 4 weeks (P < 0.01). Representative images are shown in Figure 4 .
Figure 4.
Immunofluorescence demonstrating membrane type 1 matrix metalloprotease (MT1-MMP) expression. Scale bar = 100 µm, red indicates positive MT1-MMP expression, white indicates nuclei. Representative photomicrographs of groups A and B at 2 weeks (a, d), 4 weeks (b, e), and 6 weeks (c, f).
Part B: In Vitro Culture with Rabbit Articular Chondrocyte
Transwell Filter Migration Assay
Representative images of the Transwell filter migration assay are shown in Figure 5 . The migratory ability of the different chondrocyte groups was detected with the Transwell filter migration assay. The results showed that the number of migrating chondrocytes was significantly higher during the same period than in the other groups after MT1-MMP was overexpressed (P < 0.05). No significant difference in the number of migrated cells was detected between the control and empty vector groups (P > 0.05). However, the rMT1MMP + NSC405020 group had a significantly higher number of migrating cells compared with the control and empty vector groups (P < 0.05).
Figure 5.

Chondrocyte migratory ability using the Transwell filter migration assay. Photomicrographs show chondrocyte migration after crystal violet staining, Scale bar = 200 µm. Normal medium (a); normal media + an empty vector (b); normal media + a vector-transfected with membrane type 1 matrix metalloprotease (MT1-MMP) (c); a vector-transfected MT1-MMP with + media containing the MT1-MMP inhibitor, NSC405020 (d).
Wound Healing/Scratch Assay
Representative images of the scratch (wound) assay are shown in Figure 6 . The migratory ability of different chondrocyte groups was examined by the wound healing/scratch assay. The results showed no significant difference in the scratch area between the groups at 0 and 24 hours ( Table 2 ). At 48 hours of culture, the ratio of the remaining scratch area in the transfection group was significantly lower than that in the other groups (P < 0.05), suggesting that MT1-MMP overexpression improved chondrocyte migration. The ratio of the remaining scratch area in the rMT1-MMP + NSC405020 group was significantly lower than that of the control (P < 0.05).
Figure 6.
Chondrocyte migration ability was assessed with the wound healing/scratch assay. Photographs of cell migration at 0, 24, and 48 hours of culture, Scale bar = 100 µm. Normal media (a, e, i), normal media + an empty vector (b, f, j); normal media + a vector-transfected with membrane type 1 matrix metalloprotease (MT1-MMP) (c, g, k); a vector-transfected with MT1-MMP + medium containing the MT1-MMP inhibitor, NSC405020 (d, h, l).
Table 2.
The Number of Cell Migrations in the Transwell Filter Migration Assay Incubated for 48 Hours and the Area of Scratches at 0, 24, and 48 Hours a .
| Control | Empty Vector | rMT1-MMP | rMT1-MMP + NSC405020 | |
|---|---|---|---|---|
| Transwell filter migration assay | 56.00 ± 5.61 | 54.60 ± 5.03 | 94.60±6.66 b | 66±4.69c,d |
| Wound healing/ scratch assay | ||||
| 0 hours | 1.00 ± 0.00 | 1.00 ± 0.00 | 1.00 ± 0.00 | 1.00 ± 0.00 |
| 24 hours | 0.70 ± 0.03 | 0.69 ± 0.03 | 0.41 ± 0.05 | 0.69 ± 0.03 |
| 48 hours | 0.35 ± 0.03 | 0.32 ± 0.04 | 0.00 ± 0.00 b | 0.25 ± 0.03 c |
Transwell filter migration assay was evaluated using number of migrating chondrocytes. Wound healing/ scratch assay was evaluated using the ratio of remaining scratch area. Data are presented as means ± standard deviations.
Indicates significant difference compared with other groups.
Indicates significant difference compared with control group.
Indicates significant difference compared with empty vector group.
Discussion
There were 3 important findings in the current study. The first was that cells accumulated at the edge of the cartilage fragments, and that outgrowth was better in the cartilage fragment group than in the cartilage chunk group. The second was that expression of MT1-MMP was also higher in the cartilage fragment group than those in the cartilage chunk group. The third was that overexpression of MT1-MMP enhanced the migration of articular chondrocytes, while inhibition of MT1-MMP reduced migration of these cells.
PJACs are mainly used for cartilage lesions of the knee and ankle.2 -4 Farr et al. 2 treated articular cartilage lesions on the femoral condyle or trochlea groove of the knee using PJAC. 2 This group found significantly better clinical outcomes than that following bone marrow stimulation, and the repaired tissue was high in collagen II expression. Lanham et al. 4 used PJAC to repair the articular cartilage lesions of the talus, and the clinical outcomes were better than when using iliac crest bone marrow aspirate concentrate/collagen scaffolds. The use of PJAC has widely broadened in recent years. One study used PJAC to treat osteochondral lesions of the glenohumeral joint. 5 Hess et al. 6 used PJAC to repair a chondral lesion on the scaphoid. Van Dyke et al. 7 implanted PJAC to correct an osteochondral defect of the first metatarsal head. After PJAC implantation, repaired cartilage becomes similar to hyaline cartilage, making implantation a one-stage surgery.
Many authors have confirmed the chondrocyte migration and outgrowth of minced cartilage fragments seen in our study.10 -15 In 2012, Marmotti et al. 13 observed time-dependent cell outgrowth from rabbit cartilage fragments. Marmotti et al. 14 also observed an age-dependent cellular outgrowth from human cartilage fragments in vitro and showed that more chondrocytes were released by young cartilage than by adult cartilage. The authors also showed that TGF-β1, and to a greater extent G-CSF, could accelerate this outgrowth. 12 Tsuyuguchi et al. 15 found that minced cartilage exhibited superior cell migration, proliferation, and glycosaminoglycan content than isolated chondrocytes. We confirmed an inverse relationship between the ability of cells to migrate and the size of meniscal fragments, which was similar to cartilage. 22 Several studies have reported that mincing fragments increases the tissue surface area, enabling cells essential for cartilage repair to migrate to defects, providing more space for proliferation.10,11
MT1-MMP is highly expressed in cancer cells, where it plays a critical role in cancer cell proliferation, invasion, and metastasis. MT1-MMP cleaves the cellular adhesion molecule CD44 and other proteins, triggering MMP activation cascades. 23 Liu et al. 16 reported that the MT1-MMP gene is upregulated in juvenile cartilage compared with adult cartilage. MT1-MMP activates pro-MMP2, which in turn activates pro-MMP13. Broad-spectrum MMP13 cleaves local type II collagen, aggrecan, and pericellular extracellular matrix (ECM) components. Activating the MMP cascade not only increases chondrocyte mobility by detaching these cells from the surrounding ECM but also opens up a migratory pathway by digesting the pericellular ECM barrier. In our in vitro organ culture of tissue fragments, MT1-MMP expression was upregulated during culture and correlated with chondrocyte outgrowth. This outgrowth was inhibited by blocking MT1-MMP. In the cellular assays of this study, MT1-MMP overexpression improved chondrocyte migration that was subsequently blocked by addition of the MT1-MMP inhibitor. Thus, we confirmed that MT1-MMP upregulation plays an important role in chondrocyte outgrowth after the fragmentation of juvenile cartilage. However, the upstream and downstream signaling pathways need further investigation.
The rMT1-MMP + NSC405020 group had a significantly greater number of migrating cells compared with the control and empty vector groups, showing that the effect of improved migration by MT1-MMP was only partially blocked by the exogenous MT1-MMP inhibitor. This could have occurred because NSC 405020 specifically targets the PEX (hemopexin) domain rather than the catalytic domain of MT1-MMP. Furthermore, the mechanisms of improved migration by MT1-MMP in chondrocytes was multiple.
Gelatin sponges are commercially available products that are widely used in clinical medicine. These sponges are porous and have good biocompatibility and biodegradability, making them good scaffold material for tissue engineering. 24 However, gelatin sponges are soft and easily break after immersion in the culture medium; therefore, it is difficult to transfer and change the plate during culturing. We used fibrin glue to cover and fix the cartilage fragments and gelatin sponge. The fibrin glue broke off little by little and did not hamper chondrocyte outgrowth.13,25 The chondrocytes were released from the cartilage fragments and grew into the scaffold, forming matrix in group B of this study.
In the current study, excellent cell outgrowth and matrix formation were found in the juvenile cartilage fragmentation group compared with the cartilage chunks group. This outgrowth and matrix formation was inhibited by the MT1-MMP inhibitor, which could be a key inhibitor of this mechanism. The results of our study actively promote using juvenile cartilage implantations in the repair of articular cartilage defects.
There are several limitations to this study. First, the cartilage used was from rabbits, which is not equal to human cartilage. Furthermore, the in vitro environment was different from the in vivo environment; therefore, in vivo observations of minced juvenile cartilage implantations and the effects of MT1-MMP are needed.
In conclusion, in this study, we showed that juvenile articular cartilage fragmentation improved chondrocyte migration by upregulating MT1-MMP.
Footnotes
Acknowledgments and Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grants from the Natural Science Foundation of Hunan Province (2019JJ40270), and grants from the Health Commission of Hunan Province (20201907).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: Our study was approved by the Ethical Committee of the First Affiliated Hospital of University of South China (2015030).
ORCID iD: Zhu Dai  https://orcid.org/0000-0003-1512-2775
https://orcid.org/0000-0003-1512-2775
References
- 1. Christensen BB, Olesen ML, Hede KTC, Bergholt NL, Foldager CB, Lind M. Particulated cartilage for chondral and osteochondral repair: a review. Cartilage. Epub 2020 February 13. doi: 10.1177/1947603520904757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Farr J, Tabet SK, Margerrison E, Cole BJ. Clinical, radiographic, and histological outcomes after cartilage repair with particulated juvenile articular cartilage: a 2-year prospective study. Am J Sports Med. 2014;42(6):1417-25. [DOI] [PubMed] [Google Scholar]
- 3. Wang T, Belkin NS, Burge AJ, Chang B, Pais M, Mahony G, et al. Patellofemoral cartilage lesions treated with particulated juvenile allograft cartilage: a prospective study with minimum 2-year clinical and magnetic resonance imaging outcomes. Arthroscopy. 2018;34(5):1498-505. [DOI] [PubMed] [Google Scholar]
- 4. Lanham NS, Carroll JJ, Cooper MT, Perumal V, Park JS. A comparison of outcomes of particulated juvenile articular cartilage and bone marrow aspirate concentrate for articular cartilage lesions of the talus. Foot Ankle Spec. 2017;10(4):315-321. [DOI] [PubMed] [Google Scholar]
- 5. Seidl AJ, Kraeutler MJ. Management of articular cartilage defects in the glenohumeral joint. J Am Acad Orthop Surg. 2018;26(11):e230-7. [DOI] [PubMed] [Google Scholar]
- 6. Hess DE, Werner BC, Deal DN. Use of particulated juvenile articular cartilage allograft for osteochondral lesions of the wrist. Hand (N Y). 2017;12(5):NP62-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Van Dyke B, Berlet GC, Daigre JL, Hyer CF, Philbin TM. First metatarsal head osteochondral defect treatment with particulated juvenile cartilage allograft transplantation: a case series. Foot Ankle Int. 2018;39(2_suppl):236-41. [DOI] [PubMed] [Google Scholar]
- 8. Stevens HY, Shockley BE, Willett NJ, Lin AS, Raji Y, Guldberg RE, et al. Particulated juvenile articular cartilage implantation in the knee: a 3-year EPIC-µCT and histological examination. Cartilage. 2014;5(2_suppl):74-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Seow D, Yasui Y, Hurley ET, Ross AW, Murawski CD, Shimozono Y, et al. Extracellular matrix cartilage allograft and particulate cartilage allograft for osteochondral lesions of the knee and ankle joints. Am J Sports Med. 2018;46(7):1758-66. [DOI] [PubMed] [Google Scholar]
- 10. Lu Y, Dhanaraj S, Wang Z, Bradley DM, Bowman SM, Cole BJ, et al. Minced cartilage without cell culture serves as an effective intraoperative cell source for cartilage repair. J Orthop Res. 2006;24:1261-70. [DOI] [PubMed] [Google Scholar]
- 11. Dai Z, Li K, Chen Z, Liao Y, Yang L, Liu C, et al. Repair of avascular meniscal injuries using juvenile meniscal fragments: an in vitro organ culture study. J Orthop Res. 2013;31(10):1514-9. [DOI] [PubMed] [Google Scholar]
- 12. Marmotti A, Bonasia DE, Bruzzone M, Rossi R, Castoldi F, Collo G, et al. Human cartilage fragments in a composite scaffold for single-stage cartilage repair: an in vitro study of the chondrocyte migration and the influence of TGF-β1 and G-CSF. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1819-33. [DOI] [PubMed] [Google Scholar]
- 13. Marmotti A, Bruzzone M, Bonasia DE, Castoldi F, Rossi R, Piras L, et al. One-step osteochondral repair with cartilage fragments in a composite scaffold. Knee Surg Sports Traumatol Arthrosc. 2012;20(12):2590-601. [DOI] [PubMed] [Google Scholar]
- 14. Marmotti AG, Peretti GM, Mattia S, Mangiavini L, Bonasia DE, Dettoni F, et al. One-step cartilage repair with minced chondral fragment on a composite scaffold: an in vitro human study at low oxygen tension. J Biol Regul Homeost Agents. 2017;31(4 Suppl 1):113-20. [PubMed] [Google Scholar]
- 15. Tsuyuguchi Y, Nakasa T, Ishikawa M, Miyaki S, Matsushita R, Kanemitsu M, et al. The benefit of minced cartilage over isolated chondrocytes in atelocollagen gel on chondrocyte proliferation and migration. Cartilage. 2021;12(1):93-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Liu H, Zhao Z, Clarke RB, Gao J, Garrett IR, Margerrison EEC. Enhanced tissue regeneration potential of juvenile articular cartilage. Am J Sports Med. 2013;41(11):2658-67. [DOI] [PubMed] [Google Scholar]
- 17. Adkisson HD, 4th, Martin JA, Amendola RL, Milliman C, Mauch KA, Katwal AB, et al. The potential of human allogeneic juvenile chondrocytes for restoration of articular cartilage. Am J Sports Med. 2010;38(7):1324-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Smeriglio P, Lai JH, Dhulipala L, Behn AW, Goodman SB, Smith RL, et al. Comparative potential of juvenile and adult human articular chondrocytes for cartilage tissue formation in three-dimensional biomimetic hydrogels. Tissue Eng Part A. 2015;21(1-2):147-55. [DOI] [PubMed] [Google Scholar]
- 19. Taylor SE, Lee J, Smeriglio P, Razzaque A, Smith RL, Dragoo JL, et al. Identification of human juvenile chondrocyte-specific factors that stimulate stem cell growth. Tissue Eng Part A. 2016;22(7-8):645-53. [DOI] [PubMed] [Google Scholar]
- 20. Deng M, Mei T, Hou T, Luo K, Luo F, Yang A, et al. TGFβ3 recruits endogenous mesenchymal stem cells to initiate bone regeneration. Stem Cell Res Ther. 2017;8:258. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 21. Li F, Yao J, Hao Q, Duan Z. MiRNA-103 promotes chondrocyte apoptosis by down-regulation of Sphingosine kinase-1 and ameliorates PI3K/AKT pathway in osteoarthritis. Biosci Rep. 2019;39:BSR20191255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dai Z, Li KH, Chen ZW, Hou ZX, Deng Y. Relationship between the migratory, metabolic and proliferative ability of fibrochondrocytes and the meniscal fragment size: an in vivo study. J Int Med Res. 2013;41(3):688-96. [DOI] [PubMed] [Google Scholar]
- 23. Sakamoto T, Seiki M. Integrated functions of membrane-type 1 matrix metalloproteinase in regulating cancer malignancy: beyond a proteinase. Cancer Sci. 2017;108(6):1095-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Otani Y, Komura M, Komura H, Ishimaru T, Konishi K, Komuro H, et al. Optimal amount of basic fibroblast growth factor in gelatin sponges incorporating β-tricalcium phosphate with chondrocytes. Tissue Eng Part A. 2015;21(3-4):627-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Andjelkov N, Hamberg H, Bjellerup P. No outgrowth of chondrocytes from non-digested particulated articular cartilage embedded in commercially available fibrin matrix: an in vitro study. J Orthop Surg Res. 2016;11:23. [DOI] [PMC free article] [PubMed] [Google Scholar]