Abstract
Pulmonary hamartomas are rare tumors and are mostly found incidentally in patients investigated for other pathologies. They are frequently small in size, though with some being reported as large as 25 centimeters (cm). We are reporting a case of a huge pulmonary hamartoma (measuring 25.5 × 17.5 × 15.5 cm and weighing about 2200 grams (g)) in a 33-year-old lady with a short duration history of breathlessness. The tumor had origin from the medial border of the left lung, extending into almost the entire left hemithorax and partly into the anterior mediastinum, with no local invasion. The left lower lobe had compression atelectasis due to mass. The mass was successfully resected. The histopathology report showed predominant adipose tissue and cartilaginous differentiation. There were also a few foci of papillary projections with predominant vascular areas, resembling immature placental villi, suggestive of placental transmogrification of the mass.
Keywords: Giant pulmonary hamartoma, Placental transmogrification
Introduction
A hamartoma is a benign, slow growing, self-limiting growth made up of an abnormal mixture of cells and tissues normally found in the area of the body where the growth occurs [1]. Pulmonary hamartomas constitute approximately 5–8% of solitary lung nodules and 75% of benign lung tumors [2]. Most of them originate in the parenchymal tissue on the outside of the lungs and about 10% form deep in the linings of the bronchi. Mostly, pulmonary hamartomas are asymptomatic with very slow annual growth. Rarely, these tumors increase rapidly in size, with minimal signs and symptoms. Here, we report a case with a rapidly enlarging pulmonary hamartoma with distinguishing histopathology with placental transmogrification [3].
Case report
A previously healthy 33-year-old lady presented to our out-patient department with a history of breathlessness of 2-month duration. Chest radiography demonstrated a mass in the left chest (Fig. 1). As the patient was totally asymptomatic before 2 months, it was assumed that the mass had achieved significant dimensions over last 2 months itself, as there was no previous X-ray to compare. A computed tomography (CT) scan of the chest revealed a large heterogeneous mass occupying the left hemithorax, compressing the left lung and extending into the anterior mediastinum with multiple small calcific foci. On physical examination, there was significant dullness over the left hemithorax with decreased breath sounds on auscultation. Laboratory tests and tumor markers were within normal limits. CT-guided biopsy was suggestive of pulmonary hamartoma. Surgical excision was warranted due to the huge size and rapid development of symptoms.
Fig. 1.
Chest radiography of the patient demonstrating a mass in the left chest
Surgical excision
A left posterolateral thoracotomy approach was utilized. A giant fibrocartilaginous tumor was seen arising from the medial border of the left lung, occupying most of the left hemithorax and extending partly to the anterior mediastinum. The upper lobe of the left lung was identified. The lower lobe was completely atelectatic due to compression by the mass. The mass was free from surrounding structures, with no local invasion. Left phrenic nerve was visualized and safeguarded. The tumor was dissected clear of the surrounding tissues, using combined blunt and sharp dissection, and was removed en bloc (Fig. 2—excised mass).
Fig. 2.
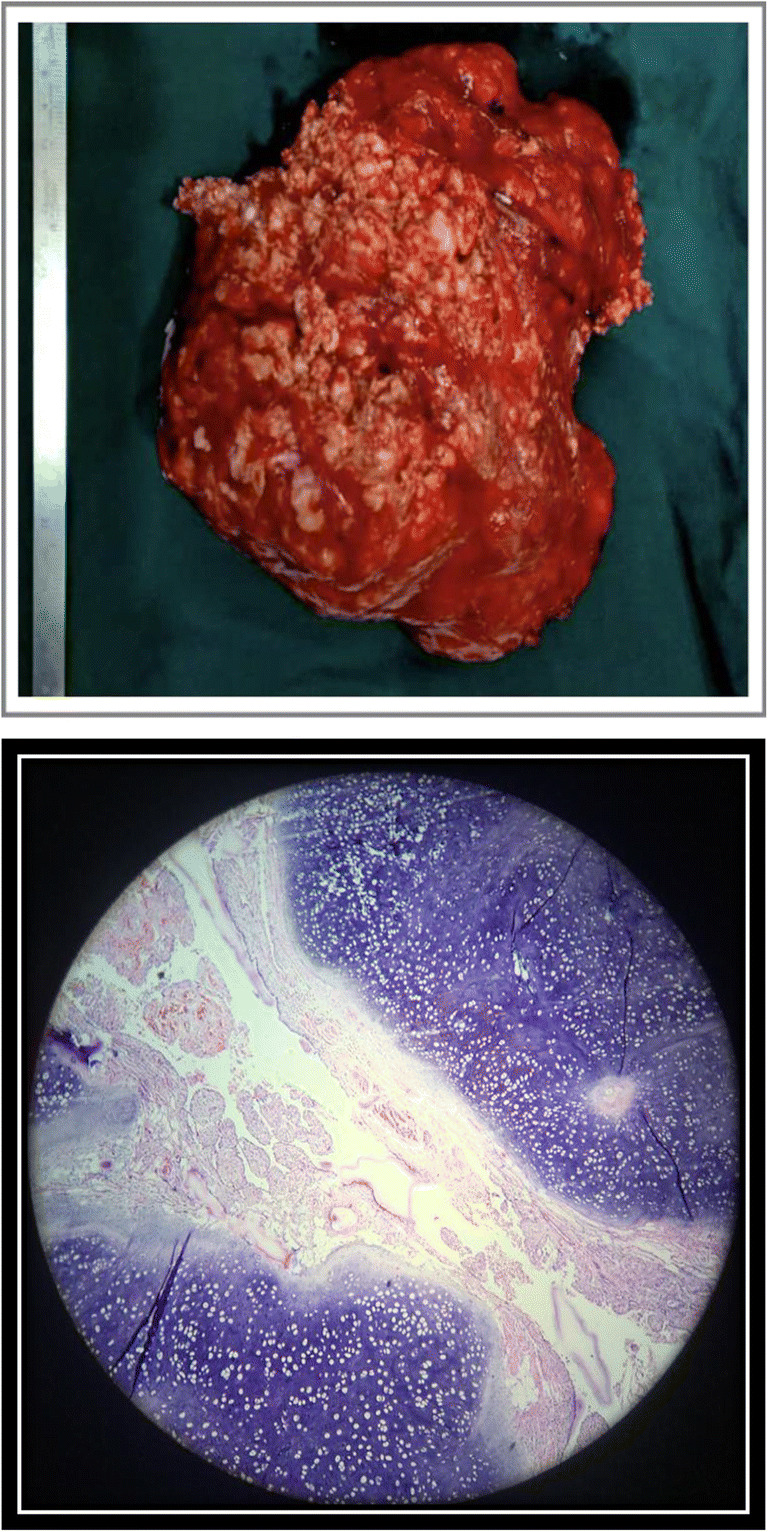
Tumor dissection and en bloc removal. On histopathological examination, few foci of papillary projections were seen resembling immature placental villi, suggestive of placental transmogrification of the lung mass
Gross examination of the specimen showed a lobular, well-circumscribed mass consisting of fibrocartilaginous tissue mixed with adipose tissue, consistent with hamartoma. It measured 25.5 × 17.5 × 15.5 centimeters (cm) in size and weighing about 2200 grams (g).
Histopathologically, it was diagnosed as a pulmonary hamartoma with predominantly adipose and cartilaginous differentiation. Few foci of papillary projections, with predominant vascular areas, were also seen resembling immature placental villi suggestive of placental transmogrification [3] of the lung mass (Fig. 2, histopathological examination, HPE).
The patient’s postoperative course was uneventful. She was discharged on postoperative day 5. The patient was doing well at 6-month follow-up.
Discussion
Hamartoma [1] is a benign, focal developmental malformation that resembles a neoplasm in the tissue of its origin. It is composed of tissue elements normally found at that site, but they are growing in a disorganized manner. It is the most common form of benign lung tumors, accounting for 75% of the group [2]. Its incidence is 0.025–0.3%. Mostly, they are parenchymal, which are peripheral in location, with endobronchial lesions, which are central, constituting only about 10%. They are commonly diagnosed in the fifth and sixth decade of life, with male to female ratio being 4:1 [4]. Majority of these tumors are very slow growing, with no or minimal symptoms, especially the peripheral parenchymal variety, which is the commoner one. The endobronchial hamartomas may present with hemoptysis or pneumonia due to obstruction atelectasis. Rarely, these tumors grow in size rapidly to huge diameters, with minimal symptoms or no symptoms at all, warranting surgical excision.
In our case, the patient was a 33-year-old female, with no previous admissions, and with a short duration of symptoms. CT scan showed a large heterogeneous tumor with speckled popcorn calcification.
Additionally, the histopathological evaluation was consistent with pulmonary hamartoma, but with transmogrification [3] of the lung epithelium into placental tissue. Most reported cases are associated with either bullous emphysema or with pulmonary fibrochondromatous hamartomas. Placental transmogrification of the lung, a term first introduced in 1979 [5], is used to describe a peculiar histologic pattern characterized by formation of placental chorionic villi–like structures in the lung parenchyma, but sans the biological or biochemical attributes of a placenta [3].
Placental transmogrification associated with pulmonary hamartoma has been reported in 6 out of 38 cases during 18 years (1982–1999) in a series published by Ruliang et al. [3] In this series, immunohistochemical analysis was performed on paraffin-embedded tissues, using monoclonal antibodies against Ki-67 and thyroid transcription factor 1 (TTF-1) and polyclonal antibodies against c-Kit antigen (a stem cell factor receptor/mast cell growth factor receptor), in conjunction with Leder stain for naphthol-AS D-chloroacetate esterase. The epithelium lining the papillary projections was positive for TTF-1 (70–90%) and Ki-67 (3–5%).
Placental transmogrification, or placentoid bullous lesion of the lung, is an unusual condition in which the alveoli develop a peculiar villous configuration that resembles placental villi at low microscopic magnification. Villous appearance probably results from the development of edema and fibrosis in the residual strands of alveolar tissue present in the enlarged airspaces of severe emphysema. Placental transmogrification of the lung has been described in patients with severe emphysema induced by cigarette smoking, congenital giant bullous emphysema, and fibrochondromatous hamartomas of the lung.
Apart from the above 6 cases, about 30 cases of placental transmogrification of the lung associated with other pathologies like emphysema, lung bullae, Swyer-James (MacLeod) syndrome, solitary pulmonary nodule, and lung carcinoma have been found on review of literature [6–9]. The age of presentation varied from 14 to 72 years.
Additionally, only 12 such cases of giant pulmonary hamartoma (diameter > 9 cm) have been reported in literature to date [10, 11].
Placental transmogrification is a histopathological finding and no tests so far have been used to predict it preoperatively. It has no functional significance. Surgical resection is usually curative and leads to successful improvement of symptoms and quality of life. Lymph node dissection is unnecessary.
A young female patient with large size of the tumor and the histology makes it an unusual presentation.
Funding
None.
Declarations
Ethics approval
Required ethics approval was taken from the institutional ethics committee.
Informed consent
Permission to write and publish this case report with intraoperative pictures was obtained from the patient and approved by the institutional review board.
Statement of human and animal rights
This was not an experimental study. No humans or animals were harmed during the procedure.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Batsakis JG. Pathology consultation. Nomenclature of developmental tumors. Ann Otol Rhinol Laryngol. 1984;93:98–99. doi: 10.1177/000348948409300122. [DOI] [PubMed] [Google Scholar]
- 2.De Cicco C, Bellomi M, Bartolomei M, et al. Imaging of lung hamartomas by multidetector computed tomography and positron emission tomography. Ann Thorac Surg. 2008;86:1769–1772. doi: 10.1016/j.athoracsur.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 3.Ruliang X, Melissa M, Jaishree J, Yara D, Jonathan M. Placental transmogrification of the lung is a histologic pattern frequently associated with pulmonary fibrochondromatous hamartoma. Arch Pathol Lab Med. 2002;126:562–566. doi: 10.5858/2002-126-0562-PTOTLI. [DOI] [PubMed] [Google Scholar]
- 4.Saadi MM, Barakeh DH, Husain S, Hajjar WM. Large multicystic pulmonary chondroid hamartoma in a child presenting as pneumothorax. Saudi Med J. 2015;36:487–489. doi: 10.15537/smj.2015.4.10210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McChesney T. Placental transmogrification of the lung: a unique case with remarkable histopathologic features. Lab Invest. 1979;40:245–246. [Google Scholar]
- 6.Buch A, Kini U. A case report of pulmonary placental transmogrification with review of literature. Indian J Chest Dis Allied Sci. 2006;48:147–150. [PubMed] [Google Scholar]
- 7.Saito Y, Ikeya T, Hoshi E, Takahashi N, Murai K, Kawabata Y, Colby TV. Placental transmogrification of the lung presenting as a small solitary nodule. Ann Thorac Surg. 2009;87:950–952. doi: 10.1016/j.athoracsur.2008.07.063. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro M, Vidal C, Lipskar AM, Gil J, Litle VR. Placental transmogrification of the lung presenting as emphysema and a lung mass. Ann Thorac Surg. 2009;87:615–616. doi: 10.1016/j.athoracsur.2008.05.076. [DOI] [PubMed] [Google Scholar]
- 9.Jenkins JM, Attia RQ, Green A, Cane P, Pilling J. A case of pulmonary placental transmogrification. Asian Cardiovasc Thorac Ann. 2016;24:811–813. doi: 10.1177/0218492316661462. [DOI] [PubMed] [Google Scholar]
- 10.Ganti S, Milton R, Davidson L, Anikin V. Giant pulmonary hamartoma. J Cardiothorac Surg. 2006;1:19. doi: 10.1186/1749-8090-1-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agarwala A, Sengupta A, Basuthakur S. Giant pulmonary hamartoma: A rare entity. J Assoc Chest Physicians. 2014;2:87–9.



