Abstract
We present the case of a female teenager who sustained nitrous oxide burns to the medial aspect of both thighs from contact with a nitrous oxide canister being used to fill balloons. There was a delay in presentation as the injury was not initially recognised. These burns were initially assessed as being superficial partial-thickness burns but took a prolonged time to heal despite regular wound care. This was complicated by a lack of adherence to recommended treatment for much of the patient care as well as the patient testing positive for COVID-19 during their management, which prevented surgery and significantly extended time to healing. While small numbers of similar cases have been previously described this is the first reported case outside of the Netherlands and in a child. Being aware of such cases ensures early referral to specialist burn care for appropriate management to give patients the best possible outcome.
Keywords: trauma, medical-surgical nursing, paediatrics, drug misuse (including addiction), plastic and reconstructive surgery
Background
Nitrous oxide, also known as laughing gas, is a popular drug of abuse. Data from 2019/20 suggested 2.4% of 16–59 years old, and 8.7% of UK 16–24 years old had used nitrous oxide as a recreational drug in the past 12 months, making it the second most commonly used illicit drug among young people.1
In the medical context, it is utilised as an anaesthetic gas and as an equimolar mixture with oxygen as analgesia for dressing changes, minor procedures and in childbirth. In a concentrated form, however, this colourless gas with a subtly sweet odour and taste provides a short lasting, euphoric, relaxing sensation, sometimes associated with episodes of laughter that can be exploited for recreational means. Although comparatively safer than many drugs its recreational use is still associated with side effects including headaches, dizziness, paranoia, hypoxia and 23 deaths in the five most recent years for which data is available.2
In the UK, the sale or supply of nitrous oxide for recreational inhalation is illegal under the Psychoactive Substances Act (2016), with offenders being liable to up to 7 years in prison and unlimited fines. However, nitrous oxide is readily available for purchase in the UK for other legitimate uses including the catering industry, in aerosols, and in motor racing, presenting a number of potential means by which it may be purchased.
Case presentation
A teenage female patient was referred to our Regional Burns Unit having sustained cold injury to her inner thighs 1 day prior. She had been inflating balloons with nitrous oxide from a large canister, which she had purchased illicitly. She was wearing jeans at the time and the total estimated contact time was 30 min. Only minimal discomfort had been noted during this period and she was not aware of any burns; as a result, no first aid was performed. On awaking the next morning, she discovered large blisters to both thighs which were painful and made it difficult to ambulate, resulting in her attending the emergency department. Aside from being a smoker she was otherwise fit and well prior to her injury. There was a history of contact with social services.
On assessment 2% total body surface area burns were identified to the upper medial thighs; 1.25% to the right thigh and 0.75% to the left thigh (figure 1). The burns were blanching and sensate bilaterally and assessed to be mostly superficial partial thickness (second-degree burns). The patient was admitted for dressing management, analgesia and paediatric team review.
Figure 1.
Distribution of burn injuries on day 1.
Treatment
This patient was dressed with UrgoTul SSD silver dressings (UrgoMedical) throughout her admission. On day 4 review of the burns, they appeared deeper in nature (mid to deep dermal). While in hospital she required frequent (often multiple times a day) dressing changes or adjustments, due to dressings slipping or being excessively wet. After 10 days of inpatient care, her dressings were manageable as an outpatient and she was discharged.
Her burn wounds continued to be dressed with silver dressings on an outpatient basis. On day 21 postinjury, there were remaining areas of eschar, therefore honey dressings were applied. After 27 days significant areas remained unhealed. In view of the slow healing, a decision was made to proceed to debridement of burn and split-thickness skin grafting. A preoperative COVID-19 PCR test was unexpectedly positive and in view of this surgery was cancelled after discussion with the patient, their family and the wider multidisciplinary team. It was felt the benefit of any surgery would be outweighed by the increased risks in operating on a COVID-19 patient.3 This is also in keeping our local policy and with many other Burns Centres’ practice for COVID-19 patients.4 As the patient had to isolate at home she was managed remotely with telemedicine review and self-dressing using honey to further lift any residual eschar. Once able to return to the clinic she had ongoing dressings; as the wound had begun to overgranulate 1% hydrocortisone ointment and Mepilex Border (Mölnlycke) dressings were used.
Over the course of this patient’s care, three sets of burn wound swabs (one swab from each thigh each time) were sent—none grew any pathogens. This is fewer swabs than would be typical in our practice but reflected the high number of missed appointments, with many dressings being done outside of the burn’s unit, and a period of self-isolation in the middle of the patient’s care. At no point were the burn wounds clinically infected and the patient never required antibiotics.
Outcome and follow-up
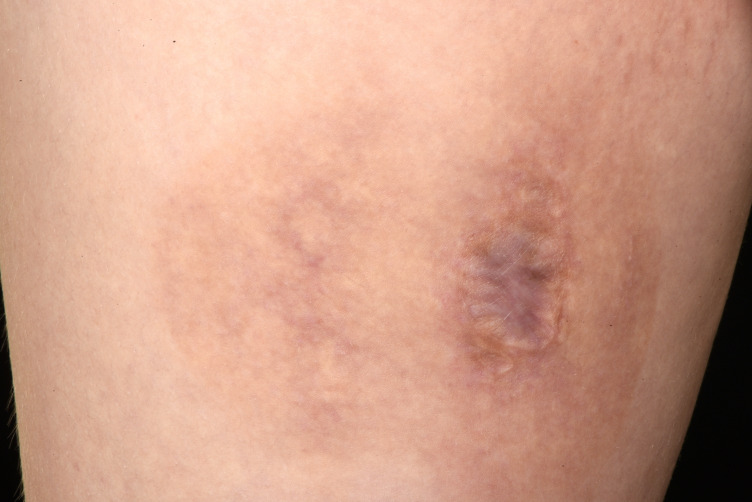
Frequently missed appointments continued and due to combination of this, difficulty getting the patient to attend for preoperative COVID-19 tests, and concerns about whether she would adhere to appropriate wound care postoperatively; it was decided not reschedule surgery, especially as the wounds continued to heal. The patient was fully involved in this decision and was in agreement. The majority of wounds had healed within 63 days by which point only four very small areas remained. Ultimately the wounds completely healed within 82 days (significantly longer than expected from the initial assessment) and the patient was discharged with scar management advice and a referral to the scar clinic for follow-up in view of residual scarring (figures 2 and 3).
Figure 2.
Left: Scarring 10 months after the injury (7 months after healing)
Figure 3.
Right: Scarring 10 months after the injury (7 months after healing)
Discussion
Historical reports of nitrous oxide-associated burns have mainly concerned accidents affecting anaesthetists in the theatre environment5 6 or in drug users inhaling directly from nitrous oxide cylinders.7–9 While similar injuries to this patient have been reported in the literature, all previous cases have been in the Netherlands and managed operatively.10 11 The largest case series, consisting of 20 patients, reported in most cases that the burns initially appeared relatively mild but appeared to worsen over the following days or not heal as anticipated, similar to our experience in this case.10
A number of factors may contribute to the severity of injuries like this. Nitrous oxide in cylinders is stored with both liquid and gaseous components. As the stream of gas is released it rapidly cools to around −55°C and further liquid is vaporised to replace the lost gas. The cylinder cools due to the latent heat of vaporisation of the liquid nitrous oxide. This results in significant cooling of the remaining liquid nitrous oxide and energy is drawn in from the surroundings to maintain this process, resulting in cooling of the cylinder. This can be seen in the development of frost forming on discharging cylinders.12 As this cooling may occur gradually the user may not notice this. Nitrous oxide is also easily lost into the surrounding environment while filling balloons and people may not be aware they are inhaling it. The analgesic effects of inhaling nitrous oxide released when filling the balloons may contribute to a reduced awareness of pain from the developing burn injury. This lack of awareness can also result in a lack of first aid as in this case. Had the patient been aware of the freezing injury and followed best practice guidelines with rewarming within 12 hours of the injury this may have helped to lessen the injury.13 The different pathophysiology of cold burn injuries from thermal injuries is also significant with both intracellular and extracellular effects from crystallisation, electrolyte shifts and direct cell membrane damage, as well as vasoconstriction, thromboembolism and endothelial injury. There can also be a secondary injury as tissues thaw which may cause the burn to worsen after the injury occurred.14
Further contributing factors to poor healing may have included poor adherence to recommended treatment—appointments were frequently missed, dressings became wet and frequently slipped. In addition, the patient tested COVID-19 positive which prevented planned surgical management and required remote management of dressings during the isolation period.
This injury is not only significant for the patient, due to the long time to healing with both prolonged inpatient and outpatient stays there was a considerable financial cost; the estimated total cost of care using patient level information and costing system data was over £25 000.
Patient’s perspective.
Patient was given the opportunity to provide their perspective but declined to do so.
Learning points.
We present the first reported case of burns associated with filling balloons with nitrous oxide outside the Netherlands.
As with similar cases reported in the Netherlands, this burn appeared relatively more superficial on first assessment but was subsequently found to be deeper.
Poor adherence to treatment complicated this case, as did a concurrent COVID-19 infection which prevented surgical management; these factors contributed to the long healing time.
It is important that both burns services and referrers are aware of these types of injury and early involvement of specialist burns services is advised.
Footnotes
Contributors: All authors were involved in the care of this patient, contributed to the writing of the case report and approved the final draft.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained from parent(s)/guardian(s).
References
- 1.Office for National Statistics . Drug misuse in England and Wales: year ending March 2020, 2020. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/articles/drugmisuseinenglandandwales/yearendingmarch2020
- 2.Office for National Statistics . Drug-related deaths involving nitrous oxide in England and Wales, 1993 to 2017, 2018. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/adhocs/009096drugrelateddeathsinvolvingnitrousoxideinenglandandwales1993to2017
- 3.Nepogodiev D, Bhangu A, Glasbey JC, et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. The Lancet 2020;396:27–38. 10.1016/S0140-6736(20)31182-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barret JP, Chong SJ, Depetris N, et al. Burn center function during the COVID-19 pandemic: an international multi-center report of strategy and experience. Burns 2020;46:1021–35. 10.1016/j.burns.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Craig DB. Thermal injury by liquid nitrous oxide. Can Anaesth Soc J 1982;29:181. 10.1007/BF03008000 [DOI] [PubMed] [Google Scholar]
- 6.Yamashita M, Motokawa K, Watanabe S. Do not use the "innovated" cylinder valve handle for cracking the valve. Anesthesiology 1986;64:658. 10.1097/00000542-198605000-00025 [DOI] [PubMed] [Google Scholar]
- 7.Hwang JC, Himel HN, Edlich RF. Frostbite of the face after recreational misuse of nitrous oxide. Burns 1996;22:152–3. 10.1016/0305-4179(95)00090-9 [DOI] [PubMed] [Google Scholar]
- 8.Chan SA, Alfonso KP, Comer BT. Upper aerodigestive tract frostbite from inhalation of automotive nitrous oxide. Ear Nose Throat J 2018;97:E13–14. 10.1177/014556131809700903 [DOI] [PubMed] [Google Scholar]
- 9.Rowbottom S. Nitrous oxide abuse. Anaesth Intensive Care 1988;16:241–2. [PubMed] [Google Scholar]
- 10.Baran KC, van Munster IG, Vries AM-de, de VAM, et al. Severe nitrous-oxide frostbite injuries on the rise in The Netherlands; let’s raise awareness. Burns 2020;46:1477–9. 10.1016/j.burns.2020.04.016 [DOI] [PubMed] [Google Scholar]
- 11.Quax MLJ, Van Der Steenhoven TJ, Antonius Bronkhorst MWG, et al. Frostbite injury: an unknown risk when using nitrous oxide as a Party drug. Acta Chir Belg 2020;16:1–4. 10.1080/00015458.2020.1782160 [DOI] [PubMed] [Google Scholar]
- 12.Jones PL. Some observations on nitrous oxide cylinders during emptying. Br J Anaesth 1974;46:534–8. 10.1093/bja/46.7.534 [DOI] [PubMed] [Google Scholar]
- 13.Hallam M-J, Cubison T, Dheansa B, et al. Managing frostbite. BMJ 2010;341:c5864–6. 10.1136/bmj.c5864 [DOI] [PubMed] [Google Scholar]
- 14.Nizamoglu M, Tan A, Vickers T, et al. Cold burn injuries in the UK: the 11-year experience of a tertiary burns centre. Burn Trauma 2016;4:1–8. 10.1186/s41038-016-0060-x [DOI] [PMC free article] [PubMed] [Google Scholar]