ABSTRACT
The pandemic COVID-19 is continued to the massive burden of morbidity and mortality while disrupting economies and societies all over the world. At an earlier stage, wearing a face mask, social distancing, and hand hygiene were suggested to limit the transmission of this infection. The WHO, CDC, and other governing bodies were doing an effort to develop the coronavirus vaccine. Now COVID-19 vaccines are available to protect people against the coronavirus. People are hesitant about whether to receive a vaccination or do not to vaccinate. This study was aimed to analyze the COVID-19 vaccination willingness level of the general public of Pakistan to manage the COVID-19 disease. A multi-criteria decision-making method known as an analytical hierarchical method was applied to determine the COVID-19 vaccination willingness level of the public. The significant determinants of COVID-19 vaccination willingness were cues to action, perceived benefits, positive attitude, government recommendation, as well as perceived stress scoring high weights to the vaccination. Determinants of willingness to uptake the COVID-19 vaccine were individual decision, vaccine origin, adapting to change, and perceived barriers high obstacles to vaccinating. The determinants relating to the COVID-19 vaccine may help to increase the uptake of the vaccination program. The government may need communication campaigns to reinforce the benefits of the vaccine.
KEYWORDS: COVID-19 vaccine, vaccination decision-making, vaccination willingness level, analytical hierarchy process, MCDM
Introduction
The coronavirus, which was first discovered in China’s Hebei region, quickly spread through the world, resulting in millions of infected cases and fatalities. The COIVD-19 pandemic is a massive threat to the global health system, including disruption of societies and economies around the globe. Some effective preventive measures, such as social distance, wearing a face mask, and hand hygiene, were adopted to reduce the transmission of COVID-19.1 In the battle of a novel coronavirus, an effective vaccine is urgently required.2 However, some vaccines have been produced to protect against animal disease in response to coronaviruses such as infectious bronchitis virus in birds, feline coronavirus, and canine coronavirus.3 The family of Coronaviridae has also targeted the human through severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS).4,5 Several papers published in 2005 and 2006 indicated the development of novel medicine and vaccine to prevent SARS was the priority of public health organizations.6–8
A COVID-19 vaccine is intended to protect the public against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), caused by coronavirus disease 2019 (COVID-19). The literature related to coronavirus functions caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and Middle East respiratory syndrome (MERS), enabled the vaccine industries for rapid development of a vaccine in early 2020.9,10 Vaccines are a significantly effective tool to protect people against deadly diseases and save millions of lives every year. Public health officials and multiple countries have shown positive indications about COVID-19 vaccines, while numerous vaccines are approved to protect against SARS-CoV-2.
Epidemic in Pakistan
Poliomyelitis (polio) is an infectious viral disease that affects young children. The polio disease is transmitted from person to person and specifically spread through the fecal-oral route. The symptoms of the poliovirus include fatigue, fever, headache, vomiting, and pain in the limbs. In 2014, Pakistan had the largest number of polio cases in the world. In Pakistan, the polio immunization campaign was initially started in 1974.11,12 Officially, the eradication was started in 1994.11 Pakistan is one of two remaining countries in the world where polio is still considered a viral infection.13–15 Several factors that affect polio eradication: perception of public, poor health infrastructure, climate, and misinformation campaigns.16–20
The coronavirus reached Pakistan on 26th February 2020 when two COVID-19 cases were registered. Pakistan has the 2nd highest confirmed COVID-19 cases in South Asia (after India), 9th highest cases in Asia, and 31st highest COVID-19 confirmed cases in the world. The AstraZeneca Sinopharm COVID-19 vaccines were approved for emergency use.
Theoretical models of vaccine behavior
In literature, two health behavior theories (Health Belief Model and Theory of Planned Behavior) have been utilized to predict the perception of individuals toward vaccination intention.21–23 HBM was considered to predict the human behavior of influenza vaccination uptake in past studies. On the other hand, the theory of planned behavior (TPB) indicates that behavior is determined by the attitude of the public to get COVID-19 vaccine (positivity, perceived benefits, and value), social norms (society support, and accurate information to get vaccinate coronavirus vaccine), perceived behavior (individual ability/control to decide against vaccination). The TPB has been effectively applied to immunization uptake in the past research.24–28
Vaccination decision-making toward COVID-19 vaccine
In the most recent decade, vaccine scandals and serious side effects of vaccination reported have raised distrust and vaccine hesitancy in the health system. In the past, pandemics such as influenza-HINI caused significant illness, hospitalization, and deaths. During influenza-HINI, a vaccine was launched, people vaccine acceptance rate lied between 8% and 67%.29 The vaccine acceptance rate in various countries such as United State: 64%, UK 56.1% (swine flu), and Hong Kong 50.5% A/H7N9.30–32 A study conducted in China revealed high acceptance of COVID-19 vaccination among healthcare workers as comhpared to the general public. An investigation reported that the influenza vaccine uptake and COVID-19 vaccination rate 49% and 63% were recorded in public hospital nurses.33 In the United States, a survey showed COVID-19 vaccination increased from 61.9% to 68.0%, and no intention to get vaccination decreased from 38.1% to 32.1%.34 An online public opinion survey was performed to investigate the vaccination hesitancy in Polish medical communication. The study results showed 86.3% persuade safety and efficacy of vaccination.35 Since perception and vaccination intention toward COVID-19 vary.
An appropriate COVID-19 vaccine is important to interrupt the spread of SARS-CoV-2. However, several factors are affected for COVID-19 vaccination, including efficacy, risk of severe side effects, lack of knowledge, affordability, experience with past vaccination, views on vaccine program, health literacy, approval of the vaccine, and lack of trust in the health system.
The vaccination decision is determined by multi-dimensional causes, typically it is considered a multiple-criteria decision-making problem. The literature presented, multi-criteria decision-making methods and operational research techniques have received greater attention in the healthcare field.36–40 For example, An AHP method is used to identify and prioritize precautionary measures to minimize the spread of COVID-19.41 The AHP technique with health technology assessment (HTA) was constructed to facilitate hospitals in the selection of medical devices in uncertain conditions.42 A multi-criteria decision-making method was used to prioritize the groups for allocation of COVID-19 vaccine, the results indicated healthcare personal, people with high-risk health, elder people, are prioritized to take vaccine dose first.43
The ministry of health Pakistan is making effort to stop polio disease permanently. The COVID-19 is also a huge challenge for the health sector to defect it. The health officials are doing best for COVID-19 vaccination, but people are hesitant to them vaccinated. Therefore, this study was aimed to determine the COVID-19 vaccine’s vaccination willingness level (i.e., identify various factors that are significant for vaccination and obstacles to vaccination) in Pakistan. For this purpose, a multi-criteria decision-making method is proposed. This research might be helpful to authorities to control coronavirus disease through vaccination. To measure the COVID-19 vaccination of participants, the following decision-making determinants of COVID-19 vaccination are considered in this study: individual determinants, experience with COVID-19, vaccine attribute, vaccine convenience, and health belief. Further, these determinants are categorized into 20 sub-components. The illustration of COVID-19 vaccination determinants is presented in Figure 1.
Figure 1.
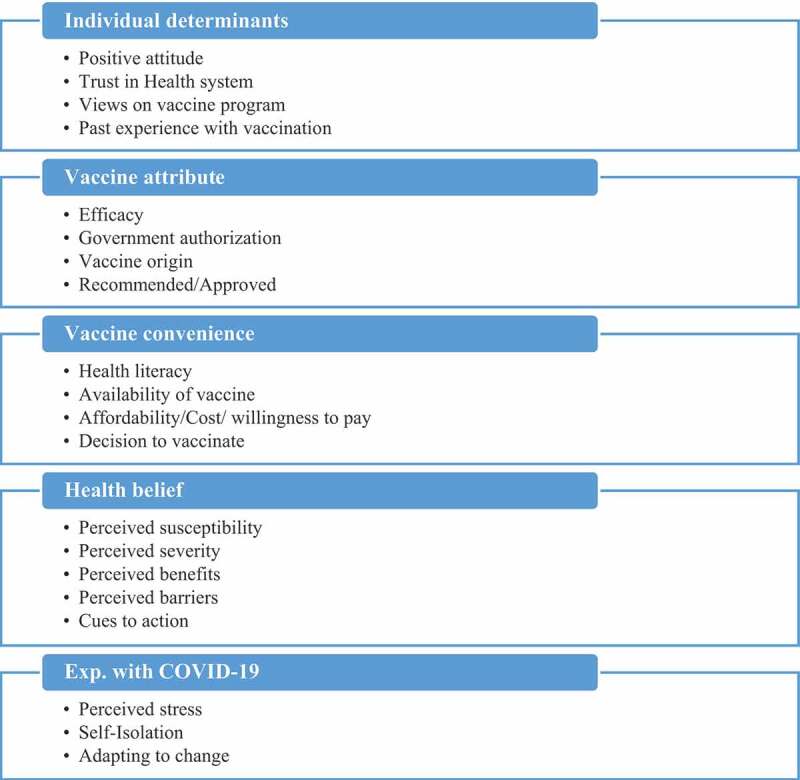
Illustration of COVID-19 determinants in the framework of MCDM.21–28
Materials and methods
Survey design and study participants
A web-based survey was used to collect information from the general population of Pakistan. An online survey questionnaire was adopted due to the ongoing COVID-19 outbreak. The questionnaire was aimed to ask the participants about their perception in response to the COVID-19 vaccination. Four cities were chosen for this study; Lahore, Karachi, Islamabad, Faisalabad, and Peshawar. The mentioned cities were chosen based on the geographical presence that enables the researcher to receive information in the restricted area during the COVID-19 pandemic. The target population in this survey was adults aged 18 years and older. A convenience sampling technique under-sample recruitment was adopted to collect data from respondents. The online survey was completely voluntary and no financial incentives were provided. The sample size of the targeted population is followed by the rule of thumb method, i.e. a minimum of 10 times of variables.44–48 In this study, a total of 25 vaccination willingness determinants including sub-determinant were considered. If we take 10 times of selected sample size according to thumb rule, should be 250. Our selected sample size is 1000 which is more than the minimum sample size required. The survey detail is given in Table 1.
Table 1.
Survey detail
| Study features | Values |
|---|---|
| Time frame | March, April, and May (2021) |
| Cities | Lahore, Karachi, Islamabad, Faisalabad, and Peshawar. |
| Sample size | 1000 |
| Valid responses | 910 |
| Response percentage | 91% |
Analytical hierarchical process
The analytical hierarchical process was proposed by Saaty.49 This method has numerous applications in many areas, particularly in the health sector which plays a role in setting priorities between main and sub-criteria, as well as ranking the alternates in the decision-making process which enable the decision-makers to make the best decision.
The AHP method includes the following steps:
Identify the decision criteria (main criteria and sub-criteria),
Develop the pairwise comparison matrix of each criterion,
Calculate the weights of criteria,
Compute the consistency ratio (CR) using Equation (4) to strengthen the consistency of comparison matrices. If CR exceeds 10%, means comparison matrices are too inconsistent and therefore need to revise the set of judgments.
Calculation of weights and consistency
A pairwise comparison scale was developed by Saaty50 shown in Table 2 where participants’ judgment on vaccination decision criteria is presented. It is worth mentioning that individuals were instructed to assign a weight to each decision criteria with different linguistics terms. The decision-makers provided their judgments on the main decision criteria and sub-decision criteria. Saaty’s AHP method was used to develop pairwise comparison matrices of decision criteria to compute the weights.51
Table 2.
Pairwise comparison scale
| Linguistics terms | Values |
|---|---|
| Weak | 1 |
| Moderate | 3–1/3 |
| Strong | 5–1/5 |
| Very strong | 7–1/7 |
| Extreme | 9–1/9 |
| Intermediate | 2–1/2, 4–1/4, 6–1/6, 8–1/8 |
Let A = {Aj | j = 1, 2 … n} be the set of COVID-19 vaccination decision criteria. The result of the pairwise comparison on n COVID-19 vaccination determinants can be summarized in an (n _ n) evaluation matrix A in which every element aij (i,j = 1,2, …,n) is the quotient of weights of the criteria, as shown:
| (1) |
In the next step, the mathematical process commences to normalize and find the relative weights for each matrix. The relative weights are given by the right eigenvector (w) corresponding to the largest eigenvalue , as
| (2) |
If the pairwise comparisons are completely consistent, the matrix A has rank 1 and max = n. In this case, weights can be obtained by normalizing any of the rows or columns of matrix A.
It should be noted that the quality of the output of the AHP is strictly related to the consistency of the pairwise comparison judgments. The consistency is defined by the relation between the entries of A: aij _ ajk = aik. The consistency index (CI) is
| (3) |
The final consistency ratio (CR), usage of which lets someone conclude whether the evaluations are sufficiently consistent, is calculated as the ratio of the CI and the random index (RI), as indicated. The RI values are given in Table 3.
| (4) |
Table 3.
Random index.52
| n | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| RI | 0 | 0 | 0.58 | 0.90 | 1.12 | 1.24 | 1.32 | 1.41 | 1.45 |
Results
Of 1000 online survey invitees, 910 (91%) provided their consent in response to COVID-19 vaccination. Table 4 shows statistics summary of characteristics of participants, 317 (34.83%) were aged between 26 and 35 years, followed by the young cohort 260 (28.57%) aged between 18 and 25 years, 185 (20.32%) aged between 36 and 45 years, and 148 (16.26%) aged between 45 years old and above. Of 910 respondents, male 530 (58.25%), and female 380 (41.75%). Most of the participants belong to Lahore city 315 (34.62%), Karachi 190 (20.88%), Islamabad 185 (20.33%), Faisalabad 153 (16.81%), and the lowest respondent’s rate from Peshawar 67 (7.36%).
Table 4.
Sociodemographic characteristics of survey
| Sociodemographic characteristics | n (%) | |
|---|---|---|
| Age | 18–25 | 260 (28.57) |
| 26–35 | 317 (34.83) | |
| 36–45 | 185 (20.32) | |
| Above 45 | 148 (16.26) | |
| Gender | Male | 530 (58.25) |
| Female | 380 (41.75) | |
| Education | Uneducated | 25 (2.75) |
| Primary | 70 (7.69) | |
| High school | 185 (20.33) | |
| Graduation | 391 (42.97) | |
| Post-graduation | 239 (26.26) | |
| Residence | Lahore | 315 (34.62) |
| Karachi | 190 (20.88) | |
| Islamabad | 185 (20.33) | |
| Faisalabad | 153 (16.81) | |
| Peshawar | 67 (7.36) | |
Furthermore, the analytical hierarchical process well known as the multi-criteria decision-making method was proposed to measure the individual COVID-19 vaccination willingness level. The participants were assigned weights to COVID-19 vaccination decision criteria both main determinants as well as sub-determinants. In the next step, comparison matrices were developed with relative weights to analyze the vaccination willingness level toward COVID-19. The major vaccination determinants: health belief hold the highest weight, 32.61%. It means participants’ health beliefs are particularly important to get them vaccinated. The individual determinants (19.89%), vaccine convenience (17.32%), vaccine attribute (15.54%), and experience with COVID-19 (14.64%) were also significant but not much important. The main vaccination determinants weights are presented in Table 5. The consistency ratio of pairwise comparison matrices has also been verified and outcomes are tolerable.
Table 5.
COVID-19 vaccination decision criteria and CR
| Main determinants | Individual determinants | Vaccine attribute | Vaccine convenience | Health belief | Exp. with COVID-19 | Percentages | |
|---|---|---|---|---|---|---|---|
| Individual determinants | 1 | 3 | 1 | 0.33 | 2 | 19.89% | CI = 0.029 |
| Vaccine attribute | 0.33 | 1 | 3 | 0.5 | 1 | 15.54% | CR = 1.12 |
| Vaccine convenience | 1 | 0.33 | 1 | 2 | 0.33 | 17.31% | CR = 0.025 |
| Health belief | 3 | 2 | 0.5 | 1 | 5 | 32.60% | |
| Exp. with COVID-19 | 0.50 | 1 | 3 | 0.10 | 1 | 14.64% |
The COVID-19 vaccination sub-determinants along with percentages have been shown in Table 6 and Figure 2. People’s health belief is important to determine coronavirus vaccination willingness level. The determinants; cues to action, perceived benefits and perceived susceptibility bear high weights indicated people do have sufficient resources and adequate information to get vaccinated themselves. Perceived barriers and perceived severity make people inconvenient to receive COVID-19 vaccination.
Table 6.
COVID-19 vaccination determinants (%)
| COVID-19 vaccination determinants | % of main determinants | % of sub determinants |
|---|---|---|
| Individual determinants | 19.89% | |
| Positive attitude | 37.58% | |
| Trust in health system | 21.81% | |
| Views on vaccine program | 23.87% | |
| Past experience with vaccination | 16.73% | |
| Vaccine attribute | 15.54% | |
| Efficacy | 20.84% | |
| Government authorization | 17.61% | |
| Vaccine origin | 13.73% | |
| Recommended/approved | 47.81% | |
| Vaccine convenience | 17.31% | |
| Health literacy | 33.92% | |
| Availability of vaccine | 15.71% | |
| Affordability | 38.92% | |
| Decision to vaccinate | 11.43% | |
| Health belief | 32.60% | |
| Perceived susceptibility | 19.94% | |
| Perceived severity | 12.96% | |
| Perceived benefits | 27.17% | |
| Perceived barriers | 7.24% | |
| Cues to action | 32.67% | |
| Exp. with COVID-19 | 14. 64% | |
| Perceived stress | 50.35% | |
| Self-isolation | 37.81% | |
| Adapting to change | 14.86% |
Figure 2.
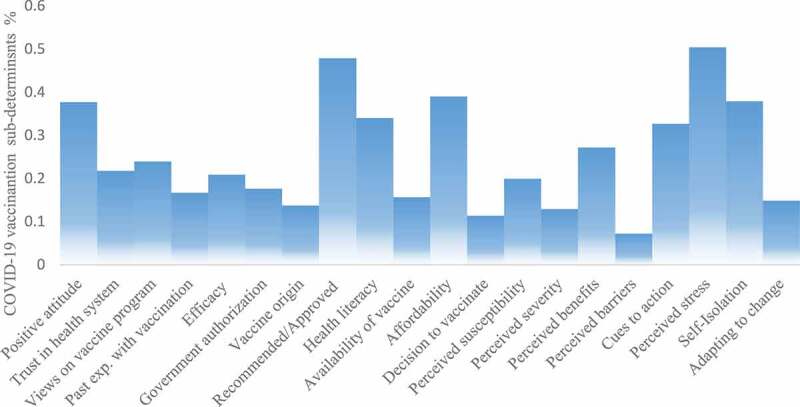
The influential sub-determinants of the COVID-19 vaccine.
The individual determinants result showed people have a positive attitude toward COVID-19 vaccination but rumors, past experiences with vaccination (such as polio vaccination), trust in the health system, and views on the vaccination programs revealed people are worried and do not have a will to uptake vaccine.
The vaccine attribute results expressed that the COVID-19 approved vaccines, government authorization, and efficacy weights indicated people vaccination willingness positively. Vaccine origin made people hesitant toward COVID-19 vaccination. Health literacy, affordability/willingness to pay, and individual decision are significant barriers to vaccinating the COIVD-19 vaccine. The people with COIVD-19 positive tests (Exp. with COVID-19), are so much depressed and do prefer self-isolation means not willing to get vaccinated.
Discussions
Vaccination is essential in protecting people from deadly diseases. However, the vaccination acceptance rate varies with time, geography, socioeconomic class, ethnicity, and human behavior.29,30,53–55 This study contained a web-based questionnaire and collected responses from major cities of Pakistan (Lahore, Karachi, Islamabad, Faisalabad, and Peshawar). In our study, a multi-criteria-decision-making method was applied to measure the COVID-19 vaccination willingness level in a novel way. In the proposed paradigm, each individual’s belief and subjective judgment on vaccination decision analysis are formulated in the framework of the multi-criteria decision-making method. Online surveys were conducted to demonstrate the effectiveness of the proposed model. Our findings suggest that perceived barriers, perceived severity, trust in the health system, experience with vaccination, and views on vaccination programs are the key barriers to a vaccine. The past research found that mistrust in the healthcare system, poor vaccination knowledge, efficacy are the obstacle to receiving the COVID-19 vaccine.56–60 Our study also investigated individual determinants that predict unwillingness and uncertainty to get vaccinated against novel coronavirus. The group of an uncertain individual can be a potential intervention. Such findings were also reported by European studies61 and in England.57 Furthermore, older people revealed less willingness to receive the vaccine, another matter of concern because such people are also at higher risk of morbidity and mortality, and this group must be on priority to get vaccinated.62
During the time that this study was being finalized, the novel coronavirus disease and its variants are continuing to unfold rather than abating, with spikes happening in different countries. However, the chances of putting an end to COVID-19 have completely changed, as numerous vaccines have made the news throughout the world, with extremely encouraging clinical trial outcomes. It is hoped that the analytical findings will provide some insights to the health department to influence the people vaccination behaviors in the following ways.
The findings might be beneficial to the health sector to increase COVID-19 vaccination in Pakistan. To overcome COVID-19 vaccine hesitancy barriers, the authorities may influence people’s intention toward COVID-19 vaccination via mass media/social media. The government may also develop and disseminate content such as videos, online flyers, and leaflets in the different languages spoken in the country, and engage stakeholders such as health professionals, religious scholars, and community leaders to counter fake rumors about the coronavirus vaccine. The government may adopt a “nude behavioral science approach” to boost the vaccination rate. The ministry may implement “health in all policies” to provide health equity to communities and people. It could be a significant way to build people’s trust in the health system.
Strength and limitation of the study
The strength of this study includes a diverse sample that focused on theoretical determinants. It might explain various factors in response to COVID-19 vaccination willingness and vaccine hesitancy. Such outcomes may provide guidelines to improve the COVID-19 vaccine uptake. The limitations of this study include reliance on convenience samples where population weights were considered from cities of Pakistan. It restricts our ability to interpret results at a national level. However, this study was conducted to analyze various determinants that relate to uptake due to which people might be hesitant. In the future, a population survey could be conducted in more cities to find the accurate percentage of vaccination. The hesitancy might differ by gender, age, and race within the population.
Despite limitations, the study used a multi-criteria decision-making model to examine the determinants of COVID-19 vaccination willingness. This study includes a set of determinants that reveal their importance to analyze the vaccination willingness of the public toward the COVID-19 vaccine.
Conclusion
The vaccination benefits emphasized increasing the probability of immunization and reducing the burden of infectious diseases. The vaccination decision-making is significant to control the diseases. The COVID-19 vaccination rate varies in different regions of the world. A multi-criteria decision-making method is an effective approach to determine the vaccination willingness level in response to the coronavirus. Individuals’ perception about vaccination is measured through hierarchical and comparison matrices using vaccination multi-decision criteria. This paradigm can be a benefit for better understanding an individual’s vaccination decision analysis through MCDM because it is also considered subjective judgment of participants. The proposed model indicated that the participant’s perceived severity, cues to action, perceived stress, vaccine approval, affordability, perceived susceptibility, trust in the health system, and views on vaccine program were showed significant determinants toward vaccination willingness of COVID-19 vaccine.
Funding Statement
The authors reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the authors.
Ethical approval
Ethical approval was not required because Pakistani individuals were asked about his/her perception in response to COVID-19 vaccination.
References
- 1.World Health Organization . Coronavirus disease (COVID-19) advice for the public. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-forpublic#:~:text=If%20COVID%2D19%20is%20spreading,a%20bent%20elbow%20or%20tissue
- 2.WHO (World Health Organization) . WHO guide for standardization of eco- nomic evaluations of immunization programmes (No. WHO/IVB/19.10). Geneva: World Health Organization; 2019 [Google Scholar]
- 3.Cavanagh D. Severe acute respiratory syndrome vaccine development: experiences of vaccination against avian infectious bronchitis coronavirus. Avian Pathol. 2003. Dec 1;32(6):567–82. doi: 10.1080/03079450310001621198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gao W, Tamin A, Soloff A, D’Aiuto L, Nwanegbo E, Robbins PD, Bellini WJ, Barratt-Boyes S, Gambotto A.. Effects of a SARS-associated coronavirus vaccine in monkeys. Lancet. 2003. Dec 6;362(9399):1895–96. doi: 10.1016/S0140-6736(03)14962-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim E, Okada K, Kenniston T, Raj VS, AlHajri MM, Farag EA, AlHajri F, Osterhaus AD, Haagmans BL, Gambotto A. Immunogenicity of an adenoviral-based Middle East respiratory syndrome coronavirus vaccine in BALB/c mice. Vaccine. 2014. Oct 14;32(45):5975–82. doi: 10.1016/j.vaccine.2014.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenough TC, Babcock GJ, Roberts A, Hernandez HJ, Thomas WD Jr, Coccia JA, Graziano RF, Srinivasan M, Lowy I, Finberg RW, et al. Development and characterization of a severe acute respiratory syndrome—associated coronavirus—neutralizing human monoclonal antibody that provides effective immunoprophylaxis in mice. J Infect Dis. 2005. Feb 15;191(4):507–14. doi: 10.1086/427242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tripp RA, Haynes LM, Moore D, Anderson B, Tamin A, Harcourt BH, Jones LP, Yilla M, Babcock GJ, Greenough T, et al. Monoclonal antibodies to SARS-associated coronavirus (SARS-CoV): identification of neutralizing and antibodies reactive to S, N, M and E viral proteins. J Virol Methods. 2005. Sep 1;128(1–2):21–28. doi: 10.1016/j.jviromet.2005.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roberts A, Thomas WD, Guarner J, Lamirande EW, Babcock GJ, Greenough TC, Vogel L, Hayes N, Sullivan JL, Zaki S, et al. Therapy with a severe acute respiratory syndrome–associated coronavirus–neutralizing human monoclonal antibody reduces disease severity and viral burden in golden Syrian Hamsters. J Infect Dis. 2006. Mar 1;193(5):685–92. doi: 10.1086/500143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li YD, Chi WY, Su JH, Ferrall L, Hung CF, Wu TC. Coronavirus vaccine development: from SARS and MERS to COVID-19. J Biomed Sci. 2020. Dec;27(1):1–23. doi: 10.1186/s12929-020-00695-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.COVID-19 vaccine development pipeline . Vaccine centre, London School of Hygiene and Tropical Medicine. 2021. Mar 1.
- 11.Global Polio Eradication Initiative > Data and monitoring > Polio this week . Pakistan launches new polio vaccine, aims for 2016 wipeout. Yahoo News. [accessed 2015 Oct 20]. www.polioeradication.org.
- 12.BBC . Polio in Pakistan: drop of 70% recorded this year. BBC. 2015. Jun 3 [accessed 2015 Jun 3]. Aim to Completely Eradicate Polio by Next Year: Pakistan.
- 13.Global Polio Eradication Initiative Key countries . [accessed 2019 Dec 23]. https://www.endpolio.com.pk/polioin-Pakistan.
- 14.Obregón R, Chitnis K, Morry C, Feek W, Bates J, Galway M, Ogden E. Achieving polio eradication: a review of health communication evidence and lessons learned in India and Pakistan. Bull World Health Organ. 2009;87(8):624–30. doi: 10.2471/BLT.08.060863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jorba J, Diop OM, Iber J, Sutter RW, Wassilak SG, Burns CC. Update on vaccine-derived polioviruses—worldwide, January 2015–May 2016. Morbidity Mortality Weekly Rep. 2016. Aug 5;65(30):76.9503–9. [DOI] [PubMed] [Google Scholar]
- 16.Larson H. The CIA’s fake vaccination drive has damaged the battle against polio. The Guardian; 2012.
- 17.Imran Ali Teepu . WHO rejects polio imad rumours. Dawn. 2012. Feb 26.
- 18.Loyn D. Alarm as Kabul records polio case. BBC News. 2014. Feb 11.
- 19.Nebehay S. CORRECTED-Pakistan, Afghanistan must step up fight against polio - WHO. Reuters. 2015. Aug 18.
- 20.Explainer: why polio remains endemic in Afghanistan, Pakistan, and Nigeria. Radio Free Europe. 2012. Dec 20.
- 21.Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974. Dec;2(4):354–86. doi: 10.1177/109019817400200405. [DOI] [Google Scholar]
- 22.Myers LB, Goodwin R. Determinants of adults’ intention to vaccinate against pandemic swine flu. BMC Public Health. 2011. Dec;11(1):1–8. doi: 10.1186/1471-2458-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coe AB, Gatewood SB, Moczygemba LR. The use of the health belief model to assess predictors of intent to receive the novel (2009) H1N1 influenza vaccine. Inov Pharm. 2012. Jan 1;3(2):1. doi: 10.24926/iip.v3i2.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gerend MA, Shepherd JE. Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med. 2012. Oct 1;44(2):171–80. doi: 10.1007/s12160-012-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fisher WA, Kohut T, Salisbury CM, Salvadori MI. Understanding human papillomavirus vaccination intentions: comparative utility of the theory of reasoned action and the theory of planned behavior in vaccine target age women and men. J Sex Med. 2013. Oct 1;10(10):2455–64. doi: 10.1111/jsm.12211. [DOI] [PubMed] [Google Scholar]
- 26.Agarwal V. A/H1N1 vaccine intentions in college students: an application of the theory of planned behavior. J Am Coll Health. 2014. Aug 18;62(6):416–24. doi: 10.1080/07448481.2014.917650. [DOI] [PubMed] [Google Scholar]
- 27.Ajzen I. The theory of planned behavior. Organizational Behav Hum Decis Processes. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 28.Fishbein M, and Ajzen I. Predicting and changing behavior: the reasoned action approach. New York: Psychology press; 2011. Feb 14. [Google Scholar]
- 29.Larson HJ, Clarke RM, Jarrett C, Eckersberger E, Levine Z, Schulz WS, Paterson P. Measuring trust in vaccination: a systematic review. Hum Vaccines Immunother. 2018. Jul 3;14(7):1599–609. doi: 10.1080/21645515.2018.1459252. (use in discussion as well). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiao X, Wong RM. Vaccine hesitancy and perceived behavioral control: a meta-analysis. Vaccine. 2020. Jul 14;38(33):5131–38. doi: 10.1016/j.vaccine.2020.04.076. (Use in discussion as well). [DOI] [PubMed] [Google Scholar]
- 31.Chan EY, Cheng CK, Tam GC, Huang Z, Lee PY. Willingness of future A/H7N9 influenza vaccine uptake: a cross-sectional study of Hong Kong community. Vaccine. 2015. Sep 11;33(38):4737–40. doi: 10.1016/j.vaccine.2015.07.046. [DOI] [PubMed] [Google Scholar]
- 32.Abbas KM, Kang GJ, Chen D, Werre SR, Marathe A. Demographics, perceptions, and socioeconomic factors affecting influenza vaccination among adults in the United States. PeerJ. 2018. Jul 13;6:e5171. doi: 10.7717/peerj.5171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kwok KO, Li KK, Wei WI, Tang A, Wong SY, Lee SS. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. 2021. Feb 1;114:103854. doi: 10.1016/j.ijnurstu.2020.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nguyen KH, Srivastav A, Razzaghi H, Williams W, Lindley MC, Jorgensen C, Abad N, Singleton JA. COVID‐19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination—United States, September and December 2020. doi: 10.1111/ajt.16560. [DOI] [PMC free article] [PubMed]
- 35.Grochowska M, Ratajczak A, Zdunek G, Adamiec A, Waszkiewicz P, Feleszko W. A comparison of the level of acceptance and hesitancy towards the influenza vaccine and the forthcoming COVID-19 vaccine in the medical community. Vaccines. 2021. May;9(5):475. doi: 10.3390/vaccines9050475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rais A, Viana A. Operations research in healthcare: a survey. Int Trans Oper Res. 2011. Jan;18(1):1–31. doi: 10.1111/j.1475-3995.2010.00767.x. [DOI] [Google Scholar]
- 37.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015. Aug 14;33(34):4161–64. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 38.Adunlin G, Diaby V, Xiao H. Application of multicriteria decision analysis in health care: a systematic review and bibliometric analysis. Health Expectations. 2015. Dec;18(6):1894–905. doi: 10.1111/hex.12287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Enayati S, Özaltın OY. Optimal influenza vaccine distribution with equity. Eur J Oper Res. 2020. Jun 1;283(2):714–25. doi: 10.1016/j.ejor.2019.11.025. [DOI] [Google Scholar]
- 40.Silal SP. Operational research: a multidisciplinary approach for the management of infectious disease in a global context. Eur J Oper Res. 2021. Jun 16;291(3):929–34. doi: 10.1016/j.ejor.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sarwar A, Imran M. Prioritizing infection prevention and control activities for SARS-CoV-2 (COVID-19): a multi-criteria decision-analysis method. J Healthcare Leadersh. 2021;13:77. doi: 10.2147/JHL.S292606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ivlev I, Vacek J, Kneppo P. Multi-criteria decision analysis for supporting the selection of medical devices under uncertainty. Eur J Oper Res. 2015. Nov 16;247(1):216–28. doi: 10.1016/j.ejor.2015.05.075. [DOI] [Google Scholar]
- 43.Hezam IM, Nayeem MK, Foul A, Alrasheedi AF. COVID-19 Vaccine: a neutrosophic MCDM approach for determining the priority groups. Results Phys. 2021. Jan 1;20:103654. doi: 10.1016/j.rinp.2020.103654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hair JF, Black WC, Babin BJ, Anderson RE, and Tatham RL. 2006. Multivariate data analysis. Vol. 6. Upper Saddle River: Pearson Prentice Hall. [Google Scholar]
- 45.Hair JF, Anderson RE, Babin BJ, and Black WC. 2010. Multivariate data analysis: a global perspective. Vol. 7. Upper Saddle River: Pearson. [Google Scholar]
- 46.Diaz-Ledezma C, Parvizi J. Surgical approaches for cam femoroacetabular impingement: the use of multicriteria decision analysis. Clin Orthop Relat Res. 2013. Aug;471(8):2509–16. doi: 10.1007/s11999-013-2934-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Diaz-Ledezma C, Lichstein PM, Dolan JG, Parvizi J. Diagnosis of periprosthetic joint infection in medicare patients: multicriteria decision analysis. Clin Orthop Relat Res. 2014. Nov;472(11):3275–84. doi: 10.1007/s11999-014-3492-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Munoz DA, Nembhard HB, Kraschnewski JL. Quantifying complexity in translational research: an integrated approach. Int J Health Care Qual Assur. 2014. Oct 7;27(8):760–76. doi: 10.1108/IJHCQA-01-2014-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saaty TL. A scaling method for priorities in hierarchical structures. J Math Psychol. 1977. Jun 1;15(3):234–81. doi: 10.1016/0022-2496(77)90033-5. [DOI] [Google Scholar]
- 50.Saaty TL. Highlights and critical points in the theory and application of the analytic hierarchy process. Eur J Oper Res. 1994. May 5;74(3):426–47. doi: 10.1016/0377-2217(94)90222-4. [DOI] [Google Scholar]
- 51.Karayalcin II. The analytic hierarchy process: planning, priority setting, resource allocation: Thomas L. £ 15.65. New York (NY): SAATY McGraw-Hill; 1980. p. xiii+ 287. [Google Scholar]
- 52.Saaty TL, and Vargas LG. Prediction, projection and forecasting: applications of the analytic hierarchy process in economics, finance, politics, games and sports. Springer Netherlands Copyright Holder - Springer Science+Business Media New York: Springer; 1991. [Google Scholar]
- 53.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014. Apr 17;32(19):2150–59. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 54.Habersaat KB, Jackson C. Understanding vaccine acceptance and demand—and ways to increase them. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz. 2020. Jan;63(1):32–39. doi: 10.1007/s00103-019-03063-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cooper S, Schmidt BM, Sambala EZ, Swartz A, Colvin CJ, Leon N, Betsch C, Wiysonge CS. Factors that influence parents’ and informal caregivers’ acceptance of routine childhood vaccination: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2019. Feb;2019(2). doi: 10.1002/14651858.CD013265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thunstrom L, Ashworth M, Finnoff D, Newbold S. Hesitancy towards a COVID-19 vaccine and prospects for herd immunity. Available at SSRN 3593098. 2020. Jun 30. Thunstrom, Linda and Ashworth, Madison and Finnoff, David and Newbold, Stephen, Hesitancy Towards a COVID-19 Vaccine and Prospects for Herd Immunity (June 30, 2020). doi: 10.2139/ssrn.3593098. [DOI] [PMC free article] [PubMed]
- 57.Sherman SM, Smith LE, Sim J, Amlôt R, Cutts M, Dasch H, Rubin GJ, Sevdalis N. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccines Immunother. 2021. Jun 3;17(6):1612–21. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rhodes A, Hoq M, Measey MA, Danchin M. Intention to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2021. May 1;21(5):e110. doi: 10.1016/S1473-3099(20)30724-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Williams L, Gallant AJ, Rasmussen S, Brown Nicholls LA, Cogan N, Deakin K, Young D, Flowers P. Towards intervention development to increase the uptake of COVID‐19 vaccination among those at high risk: outlining evidence‐based and theoretically informed future intervention content. Br J Health Psychol. 2020. Nov;25(4):1039–54. doi: 10.1111/bjhp.12468. [DOI] [PubMed] [Google Scholar]
- 60.Faasse K, Newby J. Public perceptions of COVID-19 in Australia: perceived risk, knowledge, health-protective behaviors, and vaccine intentions. Front Psychol. 2020;11. doi: 10.3389/fpsyg.2020.551004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, Schreyögg J, Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. doi. 10.1007/s10198-020-01208-6 [DOI] [PMC free article] [PubMed]
- 62.Jamison AM, Quinn SC, Freimuth VS. You don’t trust a government vaccine”: narratives of institutional trust and influenza vaccination among African American and white adults. Soc Sci Med. 2019. Jan 1;221:87–94. doi: 10.1016/j.socscimed.2018.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]


