Abstract
Objective:
Widespread adoption of prehospital pelvic circumferential compression devices (PCCDs) by emergency medical services (EMS) systems has been slow and variable across the United States. We sought to determine the frequency of prehospital PCCD use by EMS providers. Secondarily, we hypothesized that prehospital PCCD use would improve early hemorrhagic shock outcomes.
Methods:
We conducted a single-center retrospective cohort study of 162 unstable pelvic ring injuries transported directly to our center by EMS from 2011 to 2020. Included patients received a PCCD during their resuscitation (prehospital or emergency department). Prehospital treatment details were obtained from the EMS medical record. The primary outcome was the proportion of patients who received a PCCD by EMS before hospital arrival. Secondarily, we explored factors associated with receiving a prehospital PCCD, and its association with changes in vital signs, blood transfusion, and mortality.
Results:
EMS providers documented suspicion of a pelvic ring fracture in 85 (52.8%) patients and 52 patients in the cohort (32.2%) received a prehospital PCCD. Wide variation in prehospital PCCD use was observed based on patient characteristics, geographic location, and EMS provider level. Helicopter flight paramedics applied a prehospital PCCD in 46% of the patients they transported (38/83); in contrast, the EMS organizations geographically closest to our hospital applied a PCCD in ≤5% of cases (2/47). Other predictors associated with receiving a prehospital PCCD included lower body mass index (p = 0.005), longer prehospital duration (p = 0.001) and lower Injury Severity Score (p < 0.05). We were unable to identify any improvements in clinical outcomes associated with prehospital PCCD, including early vital signs, number of blood transfusions within 24 hours, or mortality during admission (p > 0.05).
Conclusion:
Our results demonstrate wide practice variation in the application of prehospital PCCDs. Although disparate PCCD application across the state is likely explained by differences across EMS organizations and provider levels, our study was unable to identify any clinical benefits to the prehospital use of PCCDs. It is possible that the benefits of a prehospital PCCD can only be observed in the most displaced fracture patterns with the greatest early hemodynamic instability.
Keywords: pelvis fracture, prehospital, emergency medical services, pelvic circumferential compression device, pelvic binder
Introduction
Unstable pelvic ring injuries are often life threatening. Urgent pelvic ring stabilization is an important treatment principle to minimize ongoing hemorrhage (1–5). Pelvic circumferential compression devices (PCCD) are an effective nonsurgical approach for early stabilization of pelvic ring injuries (6–9). Given the relative simplicity of applying a PCCD and the time urgency of the intervention, many authors advocate for the use of PCCDs to be extended from the hospital to the prehospital setting (4, 10, 11). However, this approach has not been universally adopted by emergency medical services (EMS) systems because of concerns of sufficient personnel training (12), additional material costs, and application of the device without appropriate radiographs to confirm the potential for patient benefit (13, 14). Furthermore, some authors believe that applying a PCCD on patients with severe internal rotation pelvic fractures or acetabular fractures might exacerbate their injuries and cause more harm (1, 15, 16).
To help guide policy decisions that consider expanding prehospital use of PCCDs, we aimed to understand recent prehospital PCCD use among unstable pelvic ring fractures brought to our referral center. Secondarily, we sought to explore the effect of prehospital PCCD use on various clinical outcomes. We hypothesized that prehospital PCCDs would be placed on less than half of patients with unstable pelvic ring injuries, and that there would be significant improvement in patient outcomes with their use.
Methods
Design
We conducted a single-center retrospective cohort study of unstable pelvic ring fractures (AO/OTA 61-B/C) over a 10-year period, January 2011 through December 2020. The following Young and Burgess pelvic ring fracture classifications were considered unstable for inclusion: lateral compression (LC)-3, anterior-posterior compression (APC)-2 or 3, combined mechanism injuries (CMI), and vertical shear (VS) patterns. Each pelvis fracture was classified at the time of hospitalization by the treating orthopaedic trauma surgeon as part of a prospective registry. To be included in this cohort study, eligible fracture patterns also needed to be treated with a PCCD during resuscitation (prehospital or emergency department) to ensure the injury displacement was large enough to potentially benefit from a PCCD. Additional inclusion criteria were blunt or blast injury mechanisms, direct EMS transport to our level-I trauma center, and an available EMS medical record for data collection. Overall, 1527 pelvic fracture patients were screened for study inclusion. This study was approved by our Institutional Review Board.
Intervention
PCCDs were defined as any commercial pelvic binder or modified circumferential splint (e.g., linen sheet). Wide commercial binders are the most commonly used PCCD in our prehospital and in-hospital medical system; however, the binder style or design was not available for analysis. Prehospital PCCDs were applied by EMS service teams with provider levels ranging from emergency medical technician (EMT)-basic to physician. All EMS service teams are required to follow the same state-wide prehospital trauma protocols; however, the application of a PCCD is not mandated in the protocols nor are the devices ubiquitously available across all jurisdictions.
Medical Record Review
The data extracted from the EMS medical record included initial prehospital vital signs, injury characteristics, and EMS service team characteristics. No blood products were delivered by EMS personnel during the study period. From the hospital medical record, we were able to obtain patient characteristics, first hospital vital signs, and mortality. We identified the number of patients with EMS documentation of a suspected pelvic ring injury such as pelvic instability or palpable pubic symphyseal pain or diastasis. We also determined if the PCCD was applied prehospital by EMS personnel or in the emergency department. The Injury Severity Score (ISS) was used to summarize the severity of multiply injured patients and control for potential confounding (17). Additionally, the age-adjusted shock index (ASI) was used to standardize and describe patients’ hemodynamic status. ASI is defined as the product of age multiplied by the shock index (SI) [heart rate (HR) divided by systolic blood pressure (SBP)]. The risk of requiring a massive transfusion substantially rises with a SI >0.9 (18). Similar to the SI, higher numbers of ASI reflect increasing severity of hemorrhagic shock.
Study Outcomes
The primary outcome was the proportion of patients who received a PCCD by EMS before hospital arrival. Secondarily, we calculated the proportion of patients with EMS medical record documentation of a suspected pelvic ring injury. This was used as a sensitivity analysis of our primary outcome because commercial PCCDs were not available in all jurisdictions during the entire study period. Our secondary outcomes included changes in vital signs between the initial prehospital assessment and first hospital assessment, the volume of packed red blood cell (pRBC) transfusion within the first 24 hours of admission, and the in-hospital mortality.
Statistical Analysis
Descriptive statistics were performed for all key variables. The categorical variables, summarized as counts and percentages, were compared based on timing of treatment (prehospital versus emergency department) using Chi-square tests. Fischer’s exact test was used when 20% of the expected cell counts had 5 or fewer observations. Continuous variables, described as mean values and standard deviations (SD), were compared based on timing of treatment using Student’s t-test. To investigate factors associated with PCCD placement, we developed an initial model that included factors with a statistically significant bivariate association. Factors with more than three levels were collapsed into clinically meaningful or policy relevant groups. The EMS team and EMS provider variables were collinear and, therefore, only EMS team was included in the model. Multivariable linear regression models were used in assessing continuous treatment outcomes: first hospital vital signs (SBP, HR, ASI, Glasgow Coma Scale [GCS]), change in hospital vital signs (SBP, HR, ASI, GCS) from baseline, number of pRBCs transfused, and duration of hospital admission. Multivariable logistic regression models were used in assessing categorical treatment outcomes: number of patients transfused pRBCs and in-hospital mortality. The alpha level was set at <0.05 for all statistical tests. All analyses were performed using JMP Pro, Version 14 (SAS Institute, Cary, NC).
Results
One hundred sixty-two eligible fracture patients were included (Figure 1). Table 1 outlines the patient demographics and injury details of the study population. The mean age of included patients was 42 years (SD 16 years) and the majority of patients were male (75%). The most common mechanism of injury involved motor vehicle collisions (83%), with motorcycle collisions causing 40% of the injuries. APC-2 injuries were the most common fracture pattern (47%). The vast majority of patients were transported by four EMS groups—three county-level fire department ambulance services and one state-level aviation service. Eighty-three percent of patients were treated by a paramedic. The average first vital signs obtained by the EMS providers in the field demonstrated wide variation with a mean SBP of 123 mmHg (SD 31), HR of 104 bpm (SD 27), and an ASI of 36 (SD 17) (Table 2).
Figure 1.
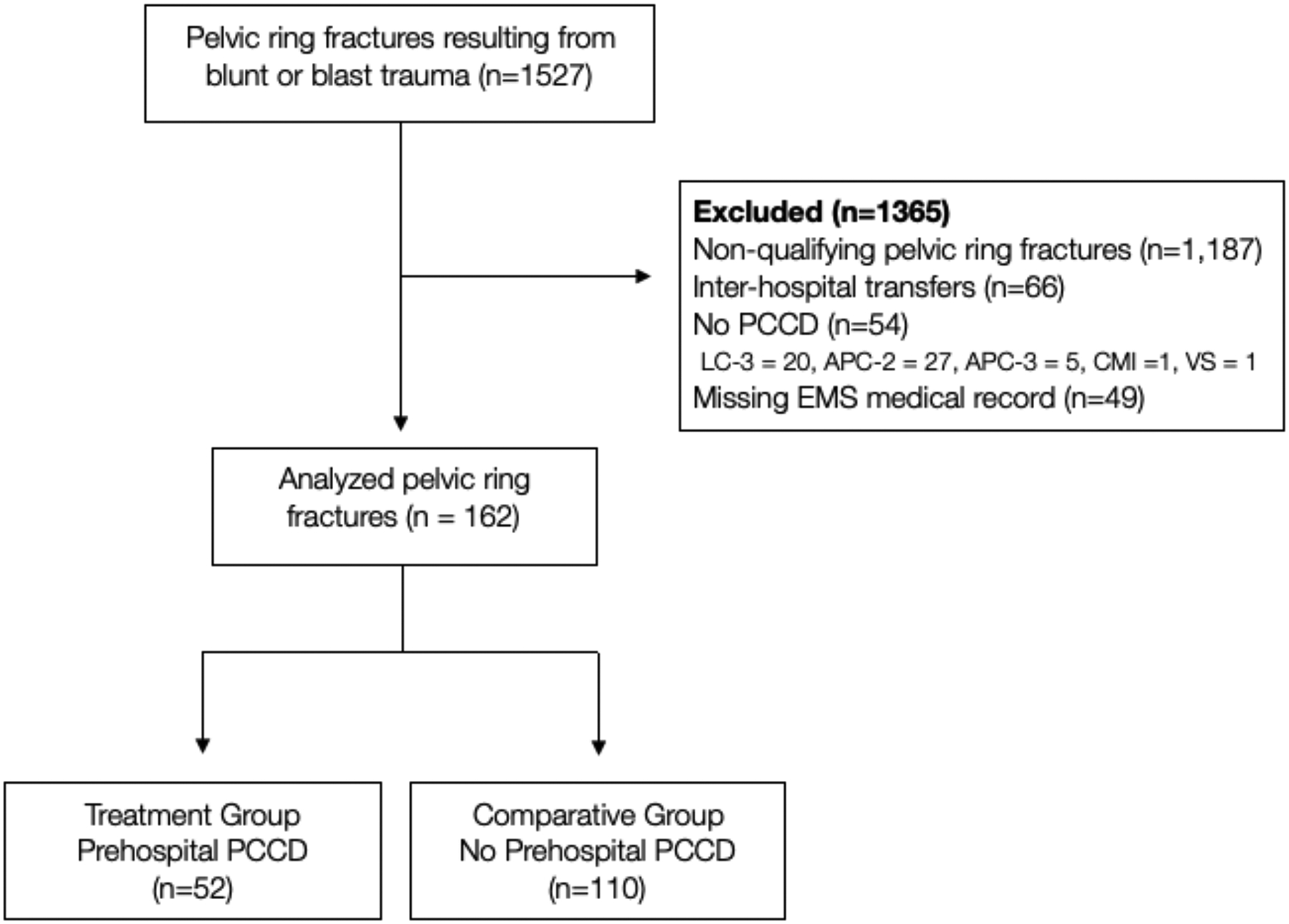
Flow diagram of study patients.
Qualifying pelvic ring fractures: LC3, APC2–3, CMI, and VS patterns of the Young and Burgess pelvic ring fracture classification system. PCCD: Pelvic Circumferential Compression Device. EMS: Emergency Medical Services
Table 1:
Characteristics of study patients
| All N = 162 |
Prehospital PCCD n = 52 |
No Prehospital PCCD n = 110 |
p-value ** | |
|---|---|---|---|---|
| Age, years, mean (SD) | 42.0 (16.0) | 39.5 (16.8) | 43.1 (15.6) | 0.20 |
| Female sex, n (%) | 40 (25%) | 12 (23%) | 28 (25%) | 0.74 |
| Race, n (%) | 0.001 | |||
| White | 92 (57%) | 41 (79%) | 51 (46%) | |
| Black | 54 (33%) | 9 (17%) | 45 (41%) | |
| Asian | 3 (2%) | 1 (2%) | 2 (2%) | |
| Other | 13 (8%) | 1 (2%) | 12 (11%) | |
| BMI, kg/m2, mean (SD) | 29.2 (5.9) | 27.4 (4.7) | 30.0 (6.2) | 0.005 |
| Mechanism of Injury, n (%)* | 0.70 | |||
| MV-Motorcyclist | 65 (40%) | 18 (35%) | 47 (43%) | |
| MV-Occupant | 44 (27%) | 16 (31%) | 28 (25%) | |
| MV-Pedestrian | 23 (14%) | 7 (13%) | 16 (15%) | |
| MV-Cyclist | 3 (2%) | 0 (0%) | 3 (3%) | |
| Fall from height >10 feet | 5 (3%) | 1 (2%) | 4 (4%) | |
| Fall from height <10 feet | 2 (1%) | 1 (2%) | 1 (1%) | |
| Machinery/ equipment | 2 (1%) | 1 (2%) | 1 (1%) | |
| Other | 18 (11%) | 8 (15%) | 10 (9%) | |
| EMS team, n (%)* | <0.001 | |||
| Helicopter service team 1 | 83 (51%) | 38 (73%) | 45 (41%) | |
| Ground service team 1 | 29 (18%) | 1 (2%) | 28 (5%) | |
| Ground service team 2 | 18 (11%) | 1 (2%) | 17 (15%) | |
| Ground service team 3 | 16 (10%) | 6 (12%) | 10 (9%) | |
| Ground service team 4 | 2 (1%) | 2 (4%) | 0 (0%) | |
| Ground service team 5 | 6 (4%) | 1 (2%) | 5 (5%) | |
| Other service teams | 8 (5%) | 3 (6%) | 5 (5%) | |
| EMS provider level, n (%)* | 0.01 | |||
| EMT-Basic | 7 (4%) | 1 (2%) | 6 (5%) | |
| EMT-Advanced or local equivalent | 12 (7%) | 0 (0%) | 12 (11%) | |
| EMT-Paramedic | 135 (83%) | 48 (92%) | 87 (79%) | |
| Physician | 3 (2%) | 2 (4%) | 1 (1%) | |
| Missing† | 5 (3%) | 1 (2%) | 4 (4%) | |
| Young-Burgess classification, n (%) | 0.68 | |||
| LC3 | 39 (24%) | 12 (23%) | 27 (25%) | |
| APC-2 | 77 (47%) | 26 (50%) | 51 (46%) | |
| APC-3 | 37 (23%) | 11 (21%) | 26 (24%) | |
| CMI | 3 (2%) | 2 (4%) | 1 (1%) | |
| VS | 6 (4%) | 1 (2%) | 5 (5%) | |
| Injury Severity Score, mean (SD) | 25.3 (14.4) | 21.6 (12.9) | 27.3 (14.9) | 0.03 |
| REBOA | 21 (13%) | 4 (8%) | 17 (15%) | 0.26 |
| Pelvic embolization | 53 (33%) | 17 (33%) | 36 (33%) | 0.99 |
| Pelvic packing | 35 (21%) | 11 (21%) | 24 (22%) | 0.91 |
| Missing† | 8 (5%) | 1 (2%) | 7 (6%) | |
| 911 call to hospital interval, minutes, mean (SD) | 55.0 (21.5) | 63.0 (19.4) | 51.1 (21.5) | 0.001 |
Percentages may not total 100 due to rounding
Student t-test for continuous variables; Chi-square test for categorical variables and Fisher’s exact test for variables with 20% of expected cell counts fewer than 5 observations.
Missing not included in chi-square and Fisher’s tests of association
PCCD, pelvic circumferential compression devices; SD, standard deviation; BMI, body mass index; MV, motor vehicle; LC, lateral compression; APC, anteroposterior compression; CMI, combined mechanical injury; VS, vertical shear; EMS, emergency medical services, EMT, emergency medical technician; REBOA, resuscitative endovascular balloon occlusion of aorta.
Table 2.
Vital signs of study patients
| All N = 162 |
Prehospital PCCD n = 52 |
No Prehospital PCCD n = 110 |
p-value * | |
|---|---|---|---|---|
| First EMS vital signs | ||||
| SBP, mmHg, mean (SD) | 122.9 (31.4) | 120.2 (26.9) | 124.2 (33.4) | 0.42 |
| HR, bpm, mean (SD) | 103.5 (27.2) | 104.2 (26.7) | 103.2 (27.6) | 0.82 |
| ASI, mean (SD) | 36.0 (16.5) | 34.7 (16.9) | 36.7 (16.4) | 0.48 |
| GCS, mean (SD) | 12.3 (4.2) | 12.9 (3.5) | 11.9 (4.5) | 0.14 |
| First hospital vital signs | ||||
| SBP, mmHg, mean (SD) | 115.0 (34.4) | 115.6 (28.9) | 114.7 (37.3) | 0.88 |
| HR, bpm, mean (SD) | 105.0 (30.9) | 103.2 (29.0) | 106.0 (32.1) | 0.62 |
| ASI, mean (SD) | 40.1 (20.9) | 36.3 (19.3) | 42.2 (21.6) | 0.12 |
| GCS, mean (SD) | 12.3 (4.3) | 13.4 (3.7) | 11.8 (4.4) | 0.04 |
Student t-test for continuous variables
SD, standard deviation; EMS, emergency medical services; SBP, systolic blood pressure; HR, heart rate; ASI, age-adjusted shock index; GCS, Glasgow Coma Scale.
Wide variation in prehospital PCCD use was observed based on patient characteristics, geographic location, and EMS provider level (Table 1). EMS providers documented suspicion of an unstable pelvic ring fracture in 85 patients (52.8%). Fifty-two patients in the cohort received a prehospital PCCD (32.2%), which represents 61% of suspected pelvic ring fractures. The remaining 110 pelvic fracture patients received a PCCD in the hospital. We were unable to detect any differences in fracture patterns between the patients who received a prehospital PCCD and the patients treated with a PCCD upon hospital arrival (Table 1). Furthermore, no differences were found between first EMS vital signs and GCS (Table 2). Helicopter flight paramedics applied a prehospital PCCD in 46% of the study patients they transported (n = 38/83); in contrast, the local EMS organizations geographically closest to our hospital applied a PCCD in ≤5% of cases (n = 2/47). In our multivariable model, only two characteristics remained associated with the odds of receiving a prehospital PCCD (Table 3). Specifically, there was increased odds of receiving a prehospital PCCD among patients with lower ISS (OR 0.96, 95% CI 0.92 to 0.99, p = 0.01) and lower odds of receiving a prehospital PCCD was associated with treatment by county EMS services geographically adjacent to the hospital (odds ratio [OR] 0.10, 95% confidence interval [CI], 0.01 to 0.47, p = 0.01).
Table 3.
Factors associated with binder placement
| Factors | Unadjusted Model | Adjusted model | ||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Race | ||||||
| White | Ref (1.00) | Ref (1.00) | ||||
| Black | 0.25 | 0.11 to 0.57 | 0.001 | 0.45 | 0.14 to 1.29 | 0.14 |
| Other | 0.18 | 0.04 to 0.83 | 0.03 | 0.18 | 0.01 to 1.42 | 0.15 |
| BMI, kg/m2 | ||||||
| ≤ 30 | Ref (1.00) | Ref (1.00) | ||||
| > 30 | 0.32 | 0.15 to 0.69 | 0.004 | 0.40 | 0.15 to 1.01 | 0.06 |
| ISS, per 1-point increase | 0.97 | 0.94 to 0.99 | 0.03 | 0.96 | 0.92 to 0.99 | 0.01 |
| EMS teams | ||||||
| Other service teams | Ref (1.00) | Ref (1.00) | ||||
| Local ground service teams | 0.07 | 0.02 to 0.36 | 0.001 | 0.10 | 0.01 to 0.47 | 0.01 |
| Helicopter service team | 1.41 | 0.61 to 3.25 | 0.42 | 1.40 | 0.50 to 4.06 | 0.52 |
| 911 call to hospital interval, per 10-minute increase | 1.33 | 1.11 to 1.61 | 0.003 | 1.19 | 0.96 to 1.47 | 0.10 |
CI, confidence interval; BMI, body mass index; ISS, Injury Severity Score; EMS, emergency medical services.
After adjusting for ISS and EMS service teams, prehospital PCCD patients were associated with a shorter hospital admission duration (−6.6 days, 95% CI, −12.8 to −0.42, p = 0.04). However, we were unable to identify any improvements in their remaining clinical outcomes, including early vital signs, pRBC blood transfusion within 24 hours, or inpatient mortality (Table 4). Even when considering the wide uncertainty around the clinical outcome estimates, the differences between groups for physiologic changes from initial injury assessment to initial hospital assessment did not approach clinical significance [SBP (−0.5 mmHg, 95% CI −19.0 to 18.1), HR (−7.0 bpm, 95% CI 17.2 to 3.13), ASI (−2.6, 95% CI 10.0 to 4.8), or GCS (0.1, 95% CI −1.1 to 1.2)]. Similarly, our adjusted models suggest the use of a prehospital PCCD did not affect the odds for receiving pRBC transfusions (p = 0.86) or inpatient mortality (p = 0.44).
Table 4.
Association between binder placement and outcome variables
| Continuous outcomes | Unadjusted model | Adjusted model* | ||||
|---|---|---|---|---|---|---|
| Prehospital PCCD n = 52 |
No Prehospital PCCD n = 110 |
Mean difference (95% CI) |
p-value | Mean difference (95% CI) |
p-value | |
| Vital signs, from EMS to hospital: | ||||||
| SBP, mmHg, mean (SD) | −5.1 (35.5) | −9.5 (44.8) | 4.4 (−10.8 to 19.7) | 0.57 | −0.5 (−19.0 to 18.1) | 0.96 |
| HR bpm, mean (SD) | −2.0 (22.1) | 2.8 (27.8) | −4.8 (−14.3 to 4.6) | 0.31 | −7.0 (−17.2 to 3.13) | 0.17 |
| ASI, mean (SD) | 1.4 (11.9) | 3.3 (20.2) | −2.0 (−8.4 to 4.5) | 0.55 | −2.6 (−10.0 to 4.8) | 0.48 |
| GCS, mean (SD) | 0.7 (2.2) | 0.0 (2.6) | 0.6 (−0.3 to 1.6) | 0.18 | 0.1 (−1.1 to 1.2) | 0.92 |
| Number of pRBC transfused, mean (SD) | 6.6 (16.2) | 5.3 (7.9) | 1.3 (−2.5 to 5.2) | 0.50 | 3.1 (−2.0 to 8.1) | 0.23 |
| Duration of admission, days, mean (SD) | 15.5 (14.3) | 21.0 (17.5) | −5.5 (−11.1 to 0.15) | 0.06 | −6.6 (−12.8 to −0.42) | 0.04 |
| Categorical outcomes | Unadjusted model | Adjusted modela | ||||
| Prehospital PCCD n = 52 |
No Prehospital PCCD n = 110 |
OR (95% CI) |
p-value | Mean difference (95% CI) |
p-value | |
| Mortality, n (%) | 5 (10%) | 11 (10%) | 0.96 (0.31 to 2.91) | 0.94 | 1.78 (0.41 to 7.80) | 0.44 |
| Patients transfused pRBC, n (%) | 28 (54%) | 72 (67%) | 0.58 (0.29 to 1.13) | 0.11 | 0.93 (0.40 to 2.12) | 0.86 |
Adjusted model includes Injury Severity Score and emergency medical services teams
PCCD, pelvic circumferential compression devices; CI, confidence interval; EMS, emergency medical services; SBP, systolic blood pressure; SD, standard deviation; HR, heart rate; ASI, age-adjusted shock index; GCS, Glasgow Coma Scale; pRBC, packed red blood cells; OR, odds ratio.
Discussion
We conducted a retrospective review to determine the frequency of prehospital PCCD use for patients with unstable pelvic ring injuries. EMS providers documented suspicion of a pelvis fracture in half of the study cohort, and applied a prehospital PCCD in nearly two-thirds of suspected cases. Ultimately, one-third of the patients that received a PCCD during their resuscitation had the device applied in the prehospital setting. ISS and the EMS service team were the strongest predictors of prehospital PCCD use. Despite these findings, no significant differences were detected in critical care outcomes between patients who received a PCCD during prehospital care versus in the emergency department. However, prehospital PCCD use was associated with a shorter hospital length of stay.
The proportion of unstable pelvic ring fractures suspected by EMS in our cohort is consistent with previous work by Lustenberger et al. (19). In their study, 7201 patients were diagnosed with a pelvic ring injury, and 56% of diagnosed pelvic ring fractures were suspected in the field. This percentage is similar to the findings in our cohort. In a separate study, Zingg et al. (10) assessed prehospital PCCD application and the effect of prehospital PCCD on various patient outcomes. The authors reported 23% of their patients received a PCCD in the field, similar to the one-third found in our study. Furthermore, prehospital PCCD use did not affect mortality or patient vitals, but was associated with a shorter hospital admission. These findings also are consistent with our data.
Although many of our findings are consistent with previous studies, Zingg et al. (10) did not find ISS to be a predictive factor of prehospital PCCD placement. The authors evaluated this association with patients who had Tile type B or C pelvic ring fractures. This analysis only included 105 patients and might have been underpowered to detect the association. Another study reviewed the effect of early pelvic binder use in emergency management (7). Those findings revealed that early binder use was associated with a lower mean number of blood transfusions and a lower mortality rate. These results differed from ours, potentially due to the comparison of their early binder group with historical controls. Advances in resuscitation practices, such as 1:1:1 transfusion protocols, likely coincided with their change in practice to use pelvic binders earlier. We attempted to minimize this potential bias by collecting all subjects (prehospital PCCD and hospital PCCD) from the same time period; however, these potential non-causal associations cannot be excluded.
There are many important findings in our study that merit further discussion. Although all EMS service teams are required to follow the same state-wide prehospital trauma protocols, only half of patients were suspected to have a pelvic ring fracture, and one-third of patients received a prehospital PCCD. PCCD availability varied across local jurisdictions and this likely contributed to differences in their use. For example, the EMS teams with the lowest prehospital PCCD use only provided devices to their EMS supervisors to mitigate the challenges associated with training and ongoing competency evaluations for an infrequent procedure. Furthermore, patients with lower ISS were more likely to receive a prehospital PCCD. While initially counterintuitive, it is possible that patients with lower ISS required fewer other prehospital interventions, which allowed for more focused management of pelvic injuries with PCCDs. Finally, although availability of PCCDs varied across local jurisdictions, there might also be variation in the EMS service teams’ training as it relates to indications for use of PCCDs.
When considering the results of the study, many of our findings must be interpreted in the context of the study design. We are mindful that the retrospective design limits our ability to determine if EMS personnel suspected a pelvic ring injury but did not document their findings. Similarly, we are unable to determine the frequency of improper prehospital PCCD placement, which could also limit the effectiveness of the intervention. Additionally, the varied availability of PCCDs across different EMS jurisdictions prevents us from determining if more patients would have received a PCCD if they had been available to all levels of EMS providers; this seems likely since the number of cases that received a PCCD is less than the number of patients with documented suspicion of a pelvis fracture.
Other important limitations of this study include the potential for residual confounding despite adjusting for known confounders in our analyses. We initially identified that African-American patients were less likely to receive a prehospital PCCD; however, race and EMS jurisdictions were also highly associated. The closest EMS service teams had the lowest percentage of prehospital PCCD use and also serve the largest inner-city African-American populations. When we included race in our multivariable regression model with EMS service team, the explanatory effect of the race variable no longer met statistical significance, yet, the model indicated some variance was still associated with race. It is unclear if this represents residual confounding or if race actually affects prehospital PCCD use. Residual confounding may also be affecting the estimated effect of PCCDs on critical care outcomes. Given the differences in ISS among patients receiving a PCCD prehospital or in the emergency department, it is possible that the shorter length of stay observed in the prehospital PCCD remains a reflection of their lower injury severity. Regardless, this finding merits further investigation, and larger clinical trials or observational datasets should be explored.
Despite noted limitations, the study has many strengths. Although our study has relatively few patients treated with a prehospital PCCD, our cohort adds to other previously reported single-center studies facilitating more stable effect size estimates. Furthermore, our sample only includes unstable pelvic ring fractures that received a PCCD, and therefore, could have potentially benefited from the intervention. Finally, data was combined from our hospital records and many EMS jurisdictions that use a state-wide medical record. This facilitated our ability to explore new variables that could potentially be associated with prehospital PCCD use, such as: the EMS service team, EMS provider level, patient race, patient BMI, and duration between 911 call to hospital arrival.
Conclusion
There is wide practice variation in the application of prehospital PCCDs and the disparate PCCD application across the state is likely explained by differences across EMS organizations, provider levels, and PCCD availability. Our work revealed that prehospital PCCDs is associated with a shorter hospital length of stay for patients with unstable pelvic ring fractures; however, we advise caution interpreting this finding. Our study was unable to identify any improvements in vital signs, blood transfusion, or mortality associated with prehospital PCCD use. It is possible that early benefits of a prehospital PCCD can only be observed in the most displaced fracture patterns with the greatest early hemodynamic instability. Given the diagnostic uncertainty faced by EMS providers, it is our opinion that prehospital PCCD use should continue to be promoted until definitive evidence of harm or efficacy is obtained from multi-center studies. In the interim, our study highlights opportunities for improvement in prehospital pelvis fracture assessment and increased standardization of EMS protocols.
Disclosure of interest
The authors report no conflict of interest.
Mr. O’Hara reported receiving stock or stock options from Arbutus Medical, Inc. unrelated to this research.
Dr. Pollak reported receiving royalties from Globus and Zimmer Biomet unrelated to this research.
Dr. Slobogean reported receiving research funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases to partially support this work (K24AR076445), and the Patient-Centered Outcomes Research Institute and the US Department of Defense unrelated to this research; serving as a paid consultant with Smith & Nephew and Zimmer Biomet unrelated to this research; and receiving personal fees from Nuvasive Orthopaedics unrelated to this research.
Data availability statement
Raw data were generated at the R Adams Shock Trauma Center, University of Maryland. Derived data supporting the findings of this study are available from the corresponding author (GS) upon reasonable request.
References
- 1.Marmor M, El Naga AN, Barker J, Matz J, Stergiadou S, Miclau T. Management of pelvic ring injury patients with hemodynamic instability. Front Surg. 2020;7:588845. doi: 10.3389/fsurg.2020.588845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pap R, McKeown R, Lockwood C, Stephenson M, Simpson P. Pelvic circumferential compression devices for prehospital management of suspected pelvic fractures: a rapid review and evidence summary for quality indicator evaluation. Scand J Trauma Resusc Emerg Med. 2020;28(1):65. doi: 10.1186/s13049-020-00762-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, Kluger Y, Moore EE, Peitzman AB, Ivatury R, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017;12:5. doi: 10.1186/s13017-017-0117-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gardner MJ, Routt ML. The antishock iliosacral screw. J Orthop Trauma. 2010;24(10):86–89. doi: 10.1097/BOT.0b013e3181c81d65 [DOI] [PubMed] [Google Scholar]
- 5.Tachibana T, Yokoi H, Kirita M, Marukawa S, Yoshiya S. Instability of the pelvic ring and injury severity can be predictors of death in patients with pelvic ring fractures: a retrospective study. J Orthop Traumatol. 2009;10:79–82. doi: 10.1007/s10195-009-0050-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benders KEM, Leenen LPH. Management of hemodynamically unstable pelvic ring fractures. Front Surg. 2020;7:601321. doi: 10.3389/fsurg.2020.601321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsu SD, Chen CJ, Chou YC, Wang SH, Chan DC. Effect of early pelvic binder use in the emergency management of suspected pelvic trauma: a retrospective cohort study. Int J Environ Res Public Health. 2017;14(10):1217. doi: 10.3390/ijerph14101217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agri F, Bourgeat M, Becce F, Moerenhout K, Pasquier M, Borens O, Yersin B, Demartines N, Zingg T. Association of pelvic fracture patterns, pelvic binder use and arterial angio-embolization with transfusion requirements and mortality rates; a 7-year retrospective cohort study. BMC Surg. 2017;17:104. doi: 10.1186/s12893-017-0299-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Costantini TW, Coimbra R, Holcomb JB, Podbielski JM, Catalano R, Blackburn A, Scalea TM, Stein DM, Williams L, Conflitti J, et al. Current management of hemorrhage from severe pelvic fractures: results of an American association for the surgery of trauma multi-institutional trial. J Trauma Acute Care Surg. 2016;80(5):717–723. doi: 10.1097/TA.0000000000001034 [DOI] [PubMed] [Google Scholar]
- 10.Zingg T, Piaget-Rossel R, Steppacher J, Carron PN, Dami F, Borens O, Albrecht R, Darioli V, Taffe P, Maudet L, et al. Prehospital use of pelvic circumferential compression devices in a physician-based emergency medical service: a 6-year retrospective cohort study. Sci Rep. 2020;10(1):5106. doi: 10.1038/s41598-020-62027-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee C, Porter K. The prehospital management of pelvic fractures. Emerg Med J. 2007;24(2):130–133. doi: 10.1136/emj.2006.041384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vaidya R, Roth M, Zarling B, Zhang S, Walsh C, Macsuga J, Swartz J. Application of circumferential compression device (binder) in pelvic injuries: room for improvement. West J Emerg Med. 2016;17(6):766–774. doi: 10.5811/westjem.2016.7.30057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weaver MJ, Heng M. Orthopedic approach to the early management of pelvic injuries. Curr Trauma Rep. 2015;1:16–25. [Google Scholar]
- 14.Fagg JAC, Acharya MR, Chesser TJS, Ward AJ. The value of ‘binder-off’ imaging to identify occult and unexpected pelvic ring injuries. Injury. 2018;49(2):284–289. doi: 10.1016/j.injury.2017.11.023 [DOI] [PubMed] [Google Scholar]
- 15.Suzuki T, Kurozumi T, Watanabe Y, Ito K, Tsunoyama T, Sakamoto T. Potentially serious adverse effects from application of a circumferential compression device for pelvic fracture: a report of three cases. Trauma Case Rep. 2020;26:100292. doi: 10.1016/j.tcr.2020.100292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tran TN, Brasel KJ, Karmy-Jones R, Rowell S, Schreiber MA, Shatz DV, Albrecht RM, Cohen MJ, DeMoya MA, Biffl WL, et al. Western trauma association critical decisions in trauma: management of pelvic fracture with hemodynamic instability-2016 updates. J Trauma Acute Care Surg. 2016;81:6. doi: 10.1097/TA.0000000000001230 [DOI] [PubMed] [Google Scholar]
- 17.Holtenius J, Bakhshayesh P, Enocson A. The pelvic fracture - indicator of injury severity or lethal fracture? Injury. 2018;49(8):1568–1571. doi: 10.1016/j.injury.2018.06.016 [DOI] [PubMed] [Google Scholar]
- 18.Rau CS, Wu SC, Kuo SC, Pao-Jen K, Shiun-Yaun H, Chen YC, Hsieh HY, Hsieh CH, Liu HT. Prediction of massive transfusion in trauma patients with shock index, modified shock index, and age shock index. Int J Environ Res Public Health. 2016;5;13(7):683. doi: 10.3390/ijerph13070683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lustenberger T, Walcher F, Lefering R, Schweigkofler U, Wyen H, Marzi I, Wutzler S, TraumaRegister DGU. The reliability of the pre-hospital physical examination of the pelvis: a retrospective, multicenter study. World J Surg. 2016;40(12):3073–3079. doi: 10.1007/s00268-016-3647-2 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Raw data were generated at the R Adams Shock Trauma Center, University of Maryland. Derived data supporting the findings of this study are available from the corresponding author (GS) upon reasonable request.


