Abstract
Aim
Centring on nursing homes, we analysed the implementation process of a tablet‐ and videoconferencing‐based telemedicine application from the perspectives of management, nursing staff and physicians.
Design
We used a qualitative design based on interviews to explore diverse perspectives on the implementation of telemedicine.
Methods
We conducted fourteen face‐to‐face or online interviews with a purposeful sample of five managers, six nurses and three general practitioners treating residents in Austrian nursing homes during the COVID‐19 pandemic. We condensed data using thematic analysis.
Results
Nursing home management implemented telemedicine rapidly, using a top‐down approach met with ambivalence by staff. On the part of nurses, their professional understanding of person‐centred care was challenged. Telemedicine also impacted cooperation between nurses and physicians, influencing their respective understanding of their roles. Working experience with digital nursing documentation had a positive effect on users' acceptance of the telemedicine solution.
Keywords: COVID‐19, nursing homes, patient care, physicians, tablets, telemedicine, videoconferencing
1. INTRODUCTION
The idea of telemedicine almost dates back to the initiation of telecommunication itself, with the first medical consultations via telephone and radio took place as early as a century ago (Moore, 1999). Telemedicine as it is known today is largely accomplished online and can potentially grant patients access to medical consultations regardless of their geographic or socioeconomic situation (Kahn, 2015), including rural areas (Hollingsworth, 2018), developing countries (Bali, 2018) or regions where certain medical procedures are illegal or hardly obtainable as is the case for abortion (Endler et al., 2019) Yet, application of telemedicine has rarely focused neither on nursing or elderly care settings in the past, nor in the on‐the‐ground experiences of implementation in its often‐multi‐professional teams.
1.1. Background
Telemedicine and telenursing particularly benefit patients with long‐term illness—requiring regular monitoring (Commission on Telemedicine, 2008). Recently, the COVID‐19 pandemic accelerated the rise of telemedicine, as virtual consultations eliminated the risk of infections and helped save time and resources for urgent cases that required in‐person care (Vidal‐Alaball et al., 2020).
While the use of telemedicine has continuously increased over the past decades, nursing homes and elderly care facilities were not a main target for implementing telemedical solutions for the longest time. This equally changed as COVID‐19 spread and nursing home residents proved to be especially vulnerable to infection. A recent study in the United Kingdom found that nurses' willingness to use telemedicine amidst the pandemic was very high and technical infrastructure to facilitate use mostly good (McGee et al., 2020). These positive tones mirror a recent study done in the French context, which describes the success of telemedicine implemented in 36 nursing homes prior to the pandemic and the advantage of its use during crisis management. It concluded with telemedicine's “great potential to deliver efficient, appropriate and safe care in the context of highly transmissible disease epidemics, both for screening and management.” (Cormi et al., 2020). A meta‐study report on New York found that telehealth applications had been implemented with increasing frequency since 2014 and the use had become still more common due to the pandemic. Overall, it found positive quantifiable impacts on factors such as reduced hospital admissions and easier access to specialized health professionals (Groom et al., 2021). In the same context, another study found that patients' readiness to use online consultations increased significantly during COVID‐19, though pre‐existing disparities in healthcare access could also be sharpened (Chunara et al., 2021). Focusing on the implementation process rather than outcomes, however, Rutledge and Gustin (2021) recently pointed out that telemedicine in nursing settings was best implemented following proper training for the nurses tasked with the use of such tools. They starkly highlight the fact that telemedicine's success is closely tied to organisational and structural affordances (Rutledge & Gustin, 2021). It is in this context that the present study accompanied the implementation process of telemedicine tools at the height of the COVID‐19 pandemic and subsequent lockdown measures in Austria, focusing on the diverse perspectives and experiences of management, nursing staff and physicians. Specifically, the present study aims to show how the implementation of telemedicine in nursing homes is managed structurally and organizationally, taking into account the impact of the COVID‐19 pandemic.
2. THE “TELEMEDICINE DURING COVID‐19”‐STUDY
This study took place in a state‐financed, not‐for‐profit nursing home collective in Vienna, Austria. The nine nursing homes in this collective accommodate between 40–270 residents. The average stay of residents is 22 months. Many of the Registered nurses working in the respective nursing homes have completed specialized education in person‐centred care. Visiting physicians provide general and specialized medical care.
A research cooperation was initiated in January 2020, shortly before the COVID‐19 hit Austria, between the Ludwig Boltzmann Institute for Digital Health and Patient Safety and the nursing home collective. The aim was to develop a telemedical tool in participating nursing homes and to accompany the implementation process ethnographically. As COVID‐19 became an increasing concern in late February 2020, we revised both the implementation strategy and the accompanying ethnographic study design. Due to the pressing need to introduce telemedicine, the nursing home management opted for an existing, though new‐to‐them technology to be implemented right away. The technology consisted of tablets and a commercially available free‐to‐use video conferencing software (Zoom©, Zoom Video Communications, Inc.) to enable virtual communication between physicians, nurses and residents during virtual medical visits. Videoconferencing had not been used for medical (or other) purposes in this setting before. The implementation process was therefore followed closely in the course of our study by conducting interviews with management, nursing staff and general practitioners during the initial phases of implementation and continued use.
2.1. Study design and methods
In the following, we are guided by the COREQ reporting criteria for qualitative research (Tong et al., 2007). We used a qualitative, exploratory design (Nathan et al., 2019). We carried out qualitative interviews with nursing home management, nurses and physicians. Interviews were carried out by PP and ME between June–August 2020, following the earliest phase of implementation of the tool. At this time, the first lockdown in Austria had ended, but national safety measures changed quickly and access to nursing homes was not always possible. Our adapted qualitative research design therefore focused on in‐person and online interviews in order to gather data about the implementation process of the telemedical tool.
We conducted four in‐person interviews and switched to video interviews when safety measures were reinforced, carrying out seven interviews via Zoom. In three cases, two people were interviewed at the same time due to time constraints and shift affordances. The interviews lasted between 25–95 min. We used an interview guide, but allowed enough flexibility for interview partners to expand beyond the questions asked or asked follow‐up questions whether the situation provided it. Overall, questions focused on our interview partners' experiences with using the tool, technology readiness and acceptance, assessment of the tool's usefulness and general questions about medical care during lockdown. The guide was also adapted slightly depending on whether we interviewed management, nurses or physicians, focusing on their respective role in nursing homes. For example, general practitioners were asked: Can you describe to me how telemedicine usually works? And nurses were asked: What has changed compared with the care before telemedicine was implemented?
Before the interviews started, all participants received information on the purpose of the interview and gave their verbal consent to participate. At the end of the interview, participants provided written informed consent. All interviews were conducted in German, recorded, transcribed verbatim, and translated by the authors for publication.
2.1.1. Participants
We used a purposeful sampling method to gather multiple perspectives on the implementation of telemedicine (Patton, 2015). We then sent information material about the study to the managers of nine nursing homes who had been informed about the study by central management. Managers from seven nursing homes agreed to participate. One manager declined and gave a detailed account of the situation in the nursing home about the implementation of the telemedical tool. Another manager declined participation because the telemedical tool had not been implemented in the respective nursing home. Nursing home managers who agreed to be interviewed were asked to name one member of the nursing staff and physicians who might be willing to be interview partners. Using this sampling method, we interviewed five managers, six nurses and three general practitioners overall, all of whom had many years of experience working in nursing homes.
2.1.2. Data analysis
We condensed data and identified themes by using thematic analysis per Braun and Clarke, following a six‐step process (Braun & Clarke, 2006): Two researchers (ME und PP) independently read the transcripts to obtain a sense of the whole transcript. Subsequently, they constructed inductive codes and identified themes. During further analysis, these themes were compared iteratively to generate seven main themes with multiple values of subthemes, respectively (Figure 1). Out of these, we defined four key areas that impacted the implementation process: experiences with existing technologies in use, person‐centred care as a guiding principle, changes in work processes and professional cooperation, and the impact of the COVID‐19 crisis situation.
FIGURE 1.
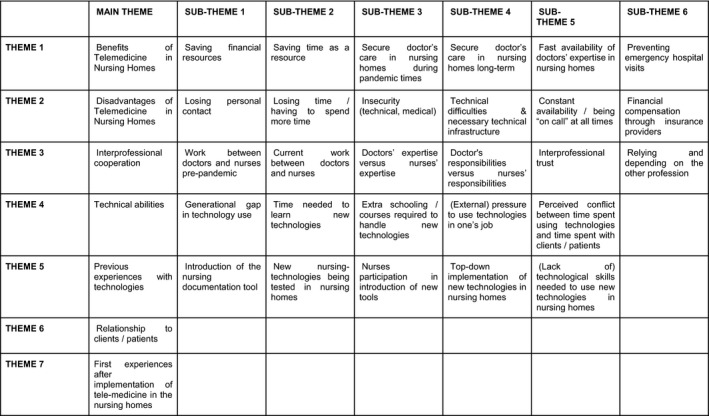
Implementing telemedicine—themes and subthemes
Throughout the analysis, meetings were held to discuss findings across all interviews and disaggregated for professional groups. Furthermore, preliminary findings were discussed with experts from the nursing organization and fellow researchers to receive feedback and gain further contextual knowledge.
3. RESULTS
In the following, we take a closer look at the impact of the pandemic on the implementation process of telemedical tools. In order to showcase multi‐professional perspectives, we present themes and views from all our participants, across all three professions, rather than artificially separated stances—this mirrors daily practice in the nursing homes. We were able to identify how the implementation of the telemedical tool was shaped by users' experiences with existing technology and professional concepts of good care, and how the tool in turn shaped working relationships between professionals and the tasks performed on a daily basis.
3.1. Experiences with existing technology
A major factor that impacted participants' views on telemedicine was the—unrelated—electronic nursing documentation tool which became obligatory to use in 2016. Nursing staff were responsible for planning and documenting the care process and physicians' visits using this system. It was also accessible remotely for general practitioners caring for residents.
Nurses described that they had difficulties with this tool, as it forced them to document even miniscule tasks performed almost automatically in everyday nursing routines. They felt the electronic documentation tool was a means to control actions that, for them, were immanent to the nursing profession. They also noted how much time was required for the mandatory documentation steps. In their opinion, the bureaucratic effort was increased, not decreased, when the documentation system was made digital years prior. They noted that the switch to the electronic documentation system was very difficult to adapt to, especially for older nurses close to retirement age, as they were not digital “natives.” As one manager stated, “The only reason (the nurses) learned was because it was obligatory… They really had to start from the ground up. Many didn't even have a computer at home before, so they had to learn basic skills, like using a keyboard” (Interview 1).
Furthermore, not all medical professionals involved in patient care were provided access to the system. As the same manager noted, “Pharmacies, the physiotherapist, all of those stakeholders … It would be great if they could be connected to the system, and would be notified (of updates) automatically” (Interview 1). Nurses objected to the fact that the tool was not user‐friendly enough and had not been developed in cooperation with the primary user group, namely nurses in a geriatric setting. More so, the tool's technical capabilities did not match the broader multi‐professional setting of the nursing home.
During the lockdown in spring 2020, at least some physicians started using the electronic nursing documentation independently for documentation purposes, although many of them had previously been reluctant to use it. Nursing staff, in turn, welcomed that lockdown had promoted the shared use of the documentation system, which facilitated coordination with physicians. One general practitioner believed that electronic documentation enabled him to “plan” his visits in the nursing home “more efficiently” and enabled him to respond to emergency calls remotely.
Nursing staff perceived the level of individual technological competence as an important predisposing factor about the extent of use of the videoconferencing application. They recounted that due to the crisis, the telemedical tool was implemented without consulting with nursing staff on their perspectives, which resulted in some staff being overwhelmed. As one manager said: “As with everything else that's new, (telemedicine) was also one of those things where employees would rather hit the break at first, because they say, it's more work, does it really benefit us, is it accurate enough, is it safe enough…” (Interview 3).
Both management and nursing staff believed training to be key to increase technological competence: “A general training, really basic, like how to use tablets, would be great, especially for older employees,” one manager stated (Interview 1). Nursing staff reported that the implementation process and familiarizing themselves with the videoconferencing application as a telemedical tool was rather time‐consuming and cumbersome: They advocated for a structured approach with training at the beginning to ease the implementation process, as they had experienced with the implementation of the electronic nursing documentation. Especially older colleagues and those who were not so technologically literate might profit from a more structured approach when implementing telemedicine. Through the quick implementation, some felt they had been “thrown right into the deep end” (Interview 1), meaning they did not have ample time to familiarize themselves with the new tools (Interview 1). With regards to physicians, nursing staff believed that they might also profit from training to improve their skills. However, nurses and management acknowledged the efforts made by the central office to support individual nursing homes despite the crisis and the rapid implementation, by providing training materials and responding to inquiries in a timely manner.
3.2. Person‐centred care as a guiding principle
The Zoom‐based telemedical tool also raised questions related to nurses' professional concepts and ethics, especially about the benefits of face‐to‐face communication as compared to virtual communication. Nurses and, to a lesser degree, management frequently mentioned personal encounters with the residents as an essential part of person‐centred care, which was a principle strongly supported in these nursing homes.
Nurses clearly stated that physicians' visits could not be replaced completely by telemedicine, mainly due to relational aspects. As one nurse stated, “For us, a doctor's visit of course includes that the doctor SEES the clients, but only to really TALK to them” (Interview 3). The nurse went on to explain that, in many cases, an in‐person visit was not even strictly necessary from a medical standpoint, as most of the nursing home clients were stable in their medical needs. Yet, direct contact (“talking,” not just “seeing”) between physicians and nurses was valued so highly and deemed so beneficial for the clients that they would not want to neglect in‐person visits completely.
Moreover, nurses rated telemedicine as unsuitable for residents with cognitive impairments who made up a statistically significant group in all nursing homes included in this study: For these residents, it was difficult or even impossible to follow virtual communication. This exclusion of some of the most marginalized of the residents contradicted the principles of person‐centred care in the eyes of the nurses.
Personal contact was seen as beneficial not only for the mental and emotional wellbeing of nursing home residents, but also was framed as a crucial diagnostics tool by physicians: Personal contact with the residents opened up diagnostic possibilities through comprehensive sensory impressions and thus was difficult to substitute. One doctor noted, “This may sound stupid or a bit weird, but I can actually even smell my patients, and this tells me things about their health; it gives me clues about how it changed (since the last visit). It's just something that comes with experience. You cannot do this over a tablet” (Interview 7).
Hence, telemedical communication may not only create a deficit of personal contact in a framework of person‐centred care, but could also contribute to a potential loss of quality in medical care. It thus came in conflict with professional ethics of both nurses and doctors.
Nursing staff and physicians perceived the willingness of residents to receive telemedical care as rather low. Nursing staff cited generational effects: The very elderly residents in the nursing home highly valued personal contact with physicians and have often had little experience in digital communication throughout their lives. Nurses stated that future residents would be more acquainted with the use of digital devices and thus more willing to accept virtual consultations: “What you do have to say is, I think, that especially now our clients are still at an age where this new media is not so present for them, and they miss the doctor coming to them, the PERSON of the doctor. You notice, bringing them a tablet does not create the same trust for them. In the future, this might change, because people will be more used to it” (Interview 6).
3.3. Changes in work processes and professional cooperation
Both groups, nurses and physicians, also repeatedly highlighted that they worked well together in teams in order to ensure the best possible care for residents. All interviewees agreed that trust and the willingness to cooperate were the basis for ensuring high‐quality care. As one nurse stated: “What you need, and this is beautiful, is TRUST. We (need to) trust the doctor and the doctor especially needs to trust (the nurses), that what we give him (sic), what we do, that we maybe suggest things based on our experience… This simply requires a lot of trust” (Interview 4).
In this respect, cooperation for nurses included their autonomy in providing hands‐on care to residents based on their daily work on site, while viewing physicians as important partners to their own work by directing treatment plans and driving diagnoses: “WE (the nurses) know our residents, and that is the most important thing,” one nursing home manager stated, describing the work nurses do on a daily basis (Interview 4).
Telemedicine, as it was implemented, changed the organization of work processes and impinged on professional cooperation in this specific respect. While some physicians stated that they saved statistically significant amounts of time during and in the preparation of patient rounds, most nurses said that the time they spent on physicians' now‐virtual visits increased. The extra time nurses spent was due to tasks such as coordinating when the virtual visit would take place, sending out Zoom invitations to the physician(s), training physicians in the use of the technology on their end, collecting residents' questions beforehand to prepare for the visit, and documenting the visit afterwards. Some of these tasks, such as the documentation work after the visit, would usually be done by the physicians themselves, but were now transferred to the nurses in some cases. The physicians, on the contrary, did not report on having to do more work through increased use of telemedicine. In fact, they saved time by not having to commute to the nursing home and not having to dress in special protective gear during the pandemic.
Differences in using telemedicine were, however, not only found in the time spent on its use, but also in the types of tasks performed. Physicians' tasks remained largely the same, minus the quality of in‐person contact with residents: They visited residents virtually, adapted medication where necessary, and decided if someone needed specialized medical care. Nurses, on the contrary, described taking on new tasks to accommodate physicians' virtual walk‐throughs in residents' rooms: They now meticulously prepared each virtual visit beforehand and documented physicians' decisions afterwards; tasks they described as highly time‐consuming and taking away from the time usually spent directly caring for nursing home residents. In turn, this compromised their principles of providing “good care.”
Besides telemedicine increasing documentation workload, nurses also had to perform an entirely new menial task: They literally carried the tablet around the nursing home to residents' beds, taking on, in their perception, the role of an assistant—a literal “hand”—to the physician. By carrying the tablet, they facilitated the physician's work, following instructions as to where to go and how to hold the tablet so as to best accommodate the physician's needs. Prior to the pandemic, nurses had sometimes accompanied physicians to provide information about individual resident's current medical concerns, but the dynamic, from the nurses' perspective, was that of two health professionals working alongside each other. With the implementation of the telemedical tool, however, nurses took a step back from their own professional role in order to allow the physicians to better, or more adequately, perform theirs.
3.4. The impact of the COVID‐19 pandemic
In many cases, nursing staff and physicians described telemedicine as a “last resort” in the time of crisis: in acute situations and when there was agreement between nursing staff and physicians that the risk of a personal contact between the physician and resident was too high. The videoconferencing application was also used when other means such as phone calls could not solve a problem as the physician needed a visual impression. Nurses and physicians both described telemedicine via the videoconferencing application as a valuable tool for a short period of time in order to secure medical care amidst a pandemic, but not for regular medical care.
Many of the nurses described themselves, or their co‐workers, as having a sceptical attitude towards new technologies, while simultaneously being eager to get residents through these challenging times safely and thus going out of their way to use new technologies. Besides these general concerns shared by all professions, both nurses and management also believed physicians to be rather hesitant about the use of telemedicine.
Management attributed part of the cautious reactions towards telemedicine to the fact that implementation had happened in the midst of a crisis and was framed as a time‐limited crisis measure by the headquarters of the nursing home. Thus, at the end of the first lockdown, medical care went back to “normal,” and physicians carried out their rounds in person again. However, nursing home management also emphasized that due to the crisis, many employees were especially willing to try out and use new technologies, such as the videoconferencing tool.
4. DISCUSSION
As is always the case for new (medical) technologies, the new tablet‐based telemedical tool was not implemented in a neutral space (Lupton, 2014; MacKenzie & Wajcman, 1995). Rather, it was added to a long line of other, previously implemented technologies used in the participating nursing homes.
Introducing new technologies is always inscribed with the meanings prior technologies have to those working with them (Wilson, 2002). Consequently, introducing a telemedical device into the nursing homes is strongly shaped by nurses' and physicians' previous experiences with other devices and especially by the way those devices were introduced to their work (Jennett et al., 2003). We found that nurses still felt residual unease about the way in which a nursing documentation system had been brought into their daily work routine. The same held true for the telemedical tool: It was chosen quickly by management using a top‐down approach due to pandemic time constraints, without involving nurses and using their extensive (tacit) knowledge on their own work processes (Armer et al., 2004). Hence, despite the two technologies (the nursing documentation system versus the new telemedical tool) being vastly different in both design and application, the way in which telemedicine was implemented brought up connections and associations between the two tools. This points to the need to create a better upfront analysis of the “technological space” already in place in a given setting where telemedicine is to be introduced.
Rather than merely adapting the tool itself, what will be needed is a lengthy, bottom‐up communication process involving all users in order to gain a common understanding of roles in using telemedicine, shared benefits for users and a definition of application (Ko et al., 2018; Shah and Robinson, 2006). In this context, it will also be important to accompany the implementation with appropriate training opportunities (Nicolaidou et al., 2015)—a view reinforced by our participants.
Implementing telemedicine in nursing homes showcased that existing power dynamics pre‐dated the COVID‐19 pandemic. A substantial power imbalance existed for nurses co‐using the telemedical tool with physicians. While a change in work processes was partly determined by the format of the tool itself, it made dynamics already present between the two professions more visible and related negatively to nurses valuing autonomy and professional cooperation. Hierarchies are inscribed into the telemedical tool itself, portraying nurses—whose role in nursing homes is usually that of autonomous professionals—as a de‐facto assistant to the physician. Telemedicine, therefore, is not only a neutral tool that fosters communication and care, but also mediates working relationships in the setting it is being used in, re‐scripting them.
However, we also found that power dynamics may change when new features are included in the telemedical tool, for instance, empowering nurses to perform skilled tasks, as proposed by one nursing home manager. He emphasized that a more advanced version of telemedicine, also including the monitoring of vital parameters, could increase the use of clinical nursing competencies in nursing homes. The implementation of telemedicine may then contribute to an upgrading of the nursing profession in terms of clinical skills. Thus, relationships between technology and professional roles must be considered fluid and contingent on deliberations on the use of these tools and the roles of its users (Wajcman, 2009).
A central role in the implementation process, as Cavenett et al. (2018) point out, is played by careful consideration of professionals' self‐perception, as well as professional roles as part of a complex hierarchy of decision‐making. Especially with nurses, their focus, as we have found, is clearly based on notions of person‐centred care. This, in their opinion, was not necessarily provided by using more technology, but rather, by spending time with residents and considering their individual needs (Kitson et al., 2013; Timmons, 2003).
On a societal level, as nursing is becoming an increasingly scarce resource, outsourcing nursing and care tasks to technologies seems like an efficient, feasible solution to close the resource gap via applying a “care fix” (Dowling, 2021). Based on our data, we conclude that nurses' willingness to incorporate technologies is strongly tied to them being able to continue to perform their work in the way they feel it should be performed.
5. CONCLUSIONS
As our participants noted, the pandemic was a field of experimentation exploring opportunities and problems in implementing telemedicine tools in nursing homes.
Both management and nursing staff described the implementation of telemedicine as somewhat detached from the daily practice in nursing homes. Despite ambivalent experiences with its use, the videoconferencing application was seen as the first step towards a wider telemedical solution. However, management believed that nursing homes still have a long way to go to fully implement and use telemedicine and all its functionalities.
Additionally, managers stated that telemedicine might help to decide whether a physician's in‐person visit is necessary, and suggested that virtual consultations with prospective residents might help in smoothing the transition to the nursing home, which is a stressful event for most of the residents.
Management and nursing staff both mentioned financial barriers hindering the uptake of telemedicine by physicians. There seems to be a lot of uncertainty about remuneration of consultations via telemedicine in the Austrian fee‐for‐service system, where physical presence of the physician during the consultation, although not mandated by law, is an unquestioned fact. Apart from that, physicians also mentioned costs of additional equipment in their practice as inhibiting the uptake, as well as the unclear legal situation in liability issues.
Lastly, according to our interviewees, a clear and shared vision of when to use telemedicine in nursing homes in the future was missing. This was attributed to the crisis situation during implementation, leaving no time for joint planning. Both nursing management and staff advocated for exploring not only the potentials, but also the pitfalls of telemedicine in nursing homes, which also takes into account specifics of caring for elderly residents living with multimorbidity and dementia.
5.1. Limitations
Several limitations have to be mentioned: First, we were not able to involve residents and informal caregivers in our study—this was due to the tightened safety measures in the nursing homes and the evolving COVID‐19 pandemic, which made it unclear to estimate when access to residents would be possible again. Our study involved a small sample, even though we were able to include three different perspectives from nurses, physicians and nursing home management. Our study was conducted in a very specific time period during the first months of the COVID‐19 pandemic. However, we believe that our results are transferable to similar situations when a new technology is planned to be implemented. The pandemic has, in our understanding, not only simply augmented existing barriers, but also opened up a window of opportunity. Last but not least, this study involved nursing homes in Austria, and conditions might be different in other countries about nursing homes and the regulatory context.
5.2. Recommendations for nursing practice
Implementation proved to be a complex process affecting different actors at different levels: First, at the individual level nurses, physicians, and other professions using telemedicine, as well as residents and informal caregivers are involved, mainly as regards the issues of acceptance of telemedicine and competencies to use it. Second, at the organizational level, management is involved as regards commitment to start an innovation process. Third, the system level of health and social care requires attention about, for instance, reimbursement and legal issues. In this respect, the experiences we have reported here can be valuable for further development steps about the implementation of telemedicine in nursing homes.
Hurdles that made it difficult to incorporate new technologies in nursing homes in the past provide valuable insight for new implementation plans for telemedicine in nursing homes. Analysing these “technological spaces” on the individual, team and organizational level about existing technologies, and sometimes even technologies that are no longer in use, gives essential clues as to a new telemedical tool's design, features, possible applications and implementation process. Although we were not able to include residents and informal caregivers in our study, we believe that a truly collaborative development of telemedicine needs to be based also on their perspectives.
CONFLICT OF INTEREST
We have no conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
Petra Plunger, Maria Kletecka‐Pulker, Thomas Wochele‐Thoma, Elisabeth Klager and Magdalena Eitenberger: Conceptualization. Petra Plunger, Magdalena Eitenberger and Fabian Eibensteiner: instruments and interviews. Petra Plunger and Magdalena Eitenberger: data analyses and first draft preparation. Maria Kletecka‐Pulker, Thomas Wochele‐Thoma, Elisabeth Klager and Fabian Eibensteiner: data analysis and drafts. Ann Kathrin Ruf: organizational support to Petra Plunger and Magdalena Eitenberger in developing the paper.
ETHICAL STATEMENT
The study was approved by the Ethics Committee of the Vienna Medical University at the meeting on 21 April, number 1256/2020. Ethical questions also arose during the study: Due to the pandemic and necessary security measures, all participants experienced extreme stress. We responded to these conditions by keeping interviews short if need be and by conducting the interviews either in person or online, depending on interviewees' preferences.
ACKNOWLEDGEMENTS
We would like to express our gratitude to all participating nursing home managers and staff, as well as to all participating physicians, who volunteered to take part in a study during the COVID‐19 pandemic and contributed their expertise.
Plunger, P. , Eitenberger, M. , Kletecka‐Pulker, M. , Wochele‐Thoma, T. , Klager, E. , Ruf, A. K. , & Eibensteiner, F. (2022). Using telemedicine in nursing homes during the COVID‐19 pandemic: A multi‐perspective view on the implementation process. Nursing Open, 9, 1155–1163. 10.1002/nop2.1155
Funding information
No external funding was received for this study, as this is a self‐financed study. All authors were employed at the Ludwig Boltzmann institute during the conduct of the study
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Armer, J. M. , Harris, K. , & Dusold, J. (2004). Application of the concerns‐based adoption model to the installation of telemedicine in a rural missouri nursing home. Journal for Nurses in Staff Development (JNSD), 20(1), 42–49. 10.1097/00124645-200401000-00008 [DOI] [PubMed] [Google Scholar]
- Bali, S. (2018). Barriers to development of telemedicine in developing countries. Telehealth, Thomas F. Heston, IntechOpen. 10.5772/intechopen.81723 Available from: https://www.intechopen.com/chapters/64650 [DOI] [Google Scholar]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Cavenett, W. , Baker, S. , Waycott, J. , Carrasco, R. , Robertson, E. , Vetere, F. , & Hampson, R. (2018). Deploying new technology in residential aged care: Staff members’ perspectives. Proceedings of the 30th Australian Conference on Computer‐Human Interaction, 200–204. 10.1145/3292147.3292214 [DOI]
- Chunara, R. , Zhao, Y. , Chen, J. , Lawrence, K. , Testa, P. A. , Nov, O. , & Mann, D. M. (2021). Telemedicine and healthcare disparities: A cohort study in a large healthcare system in New York City during COVID‐19. Journal of the American Medical Informatics Association, 28(1), 33–41. 10.1093/jamia/ocaa217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Commission on Telemedicine (2008). Communication from the commission to the european parliament, the council, the European economic and social committee of the regions on telemedicine for the benefit of patients, healthcare systems and society. https://eur‐lex.europa.eu/LexUriServ/LexUriServ.do?uri=COM:2008:0689:FIN:EN:PDF
- Cormi, C. , Chrusciel, J. , Laplanche, D. , Dramé, M. , & Sanchez, S. (2020). Telemedicine in nursing homes during the COVID‐19 outbreak: A star is born (again). Geriatrics & Gerontology International, 20(6), 646–647. 10.1111/ggi.13934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doarn, C. R. (2015). Development of Telemedicine and NASA's Contribution. Aerospace Medicine and Human Performance, 86(5), 504–505. 10.3357/AMHP.4324.2015 [DOI] [PubMed] [Google Scholar]
- Dowling, E. (2021). The care crisis: What caused it and how can we end it? (First edition paperback). Verso. [Google Scholar]
- Endler, M. , Lavelanet, A. , Cleeve, A. , Ganatra, B. , Gomperts, R. , & Gemzell‐Danielsson, K. (2019). Telemedicine for medical abortion: A systematic review. BJOG: An International Journal of Obstetrics & Gynaecology, 126(9), 1094–1102. 10.1111/1471-0528.15684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groom, L. L. , McCarthy, M. M. , Stimpfel, A. W. , & Brody, A. A. (2021). Telemedicine and Telehealth in nursing homes: An integrative review. Journal of the American Medical Directors Association, 22(9), 1784–1801.e7. 10.1016/j.jamda.2021.02.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingsworth, J. D. (2018). Is there a doctor in the house: How dismantling barriers to telemedicine practice can improve healthcare access for rural residents notes & comments. Howard Law Journal, 62(2), i–686. [Google Scholar]
- Jennett, P. , Yeo, M. , Pauls, M. , & Graham, J. (2003). Organizational readiness for telemedicine: Implications for success and failure. Journal of Telemedicine and Telecare, 9(2_suppl), 27–30. 10.1258/135763303322596183 [DOI] [PubMed] [Google Scholar]
- Kahn, J. M. (2015). Virtual Visits—Confronting the Challenges of Telemedicine. New England Journal of Medicine, 372(18), 1684–1685. 10.1056/NEJMp1500533 [DOI] [PubMed] [Google Scholar]
- Kitson, A. , Marshall, A. , Bassett, K. , & Zeitz, K. (2013). What are the core elements of patient‐centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. Journal of Advanced Nursing, 69(1), 4–15. 10.1111/j.1365-2648.2012.06064.x [DOI] [PubMed] [Google Scholar]
- Ko, M. , Wagner, L. , & Spetz, J. (2018). Nursing home implementation of health information technology: Review of the literature finds inadequate investment in preparation, infrastructure, and training. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 55, 004695801877890. 10.1177/0046958018778902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodukula, S. , & Nazvia, M. (2011). Evaluation of critical success factors for telemedicine implementation. International Journal of Computer Applications, 12(10), 29–36. 10.5120/1718-2304 [DOI] [Google Scholar]
- Lupton, D. (2014). Beyond techno‐utopia: Critical approaches to digital health technologies. Societies, 4(4), 706–711. 10.3390/soc4040706 [DOI] [Google Scholar]
- MacKenzie, D. , & Wajcman, J. (Eds.) (1995). The Social Shaping of Technology. Open University Press. [Google Scholar]
- McGee, M. , Potter, C. , & Kane, J. (2020). Are UK care homes ready for the telemedicine revolution? BJPsych Bulletin, 44(5), 222. 10.1192/bjb.2020.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore, M. (1999). The evolution of telemedicine. Future Generation Computer Systems, 15(2), 245–254. 10.1016/S0167-739X(98)00067-3 [DOI] [Google Scholar]
- Nathan, S. , Newman, C. , & Lancaster, K. (2019). Qualitative Interviewing. In Liamputtong P. (Ed.), Handbook of Research Methods in Health Social Sciences. Springer. 10.1007/978-981-10-5251-4_77 [DOI] [Google Scholar]
- Nesbitt, T. S. (2012). The Evolution of Telehealth: Where Have We Been and Where Are We Going? In Board on Health Care Services , Institute of Medicine , eds. The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary. National Academies Press (US). 1–8. https://www.ncbi.nlm.nih.gov/books/NBK207141/ [PubMed] [Google Scholar]
- Nicolaidou, I. , Antoniades, A. , Constantinou, R. , Marangos, C. , Kyriacou, E. , Bamidis, P. , Dafli, E. , & Pattichis, C. S. (2015). A Virtual emergency telemedicine serious game in medical training: A quantitative, professional feedback‐informed evaluation study. Journal of Medical Internet Research, 17(6), e3667. 10.2196/jmir.3667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton, M. Q. (2015). Qualitative research & evaluation methods: Integrating theory and practice (Fourth edition). SAGE Publications Inc. [Google Scholar]
- Rutledge, C. M. , & Gustin, T. (2021). Preparing Nurses for Roles in Telehealth: Now is the Time! OJIN: The Online Journal of Issues in Nursing, 26(1). 10.3912/OJIN.Vol26No01Man03 [DOI] [Google Scholar]
- Senanayake, B. , Wickramasinghe, S. I. , Eriksson, L. , Smith, A. C. , & Edirippulige, S. (2018). Telemedicine in the correctional setting: A scoping review. Journal of Telemedicine and Telecare, 24(10), 669–675. 10.1177/1357633X18800858 [DOI] [PubMed] [Google Scholar]
- Shah, G. S. S. , & Robinson, I. (2006). User involvement in healthcare technology development and assessment: Structured literature review. International Journal of Health Care Quality Assurance, 19(6), 500–515. 10.1108/09526860610687619 [DOI] [PubMed] [Google Scholar]
- Timmons, S. (2003). Nurses resisting information technology. Nursing Inquiry, 10, 257–269. 10.1046/j.1440-1800.2003.00177.x [DOI] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32‐item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Uscher‐Pines, L. , Fischer, S. , Tong, I. , Mehrotra, A. , Malsberger, R. , & Ray, K. (2018). Virtual first responders: The role of direct‐to‐consumer telemedicine in caring for people impacted by natural disasters. Journal of General Internal Medicine, 33(8), 1242–1244. 10.1007/s11606-018-4440-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidal‐Alaball, J. , Acosta‐Roja, R. , Pastor Hernández, N. , Sanchez Luque, U. , Morrison, D. , Narejos Pérez, S. , Perez‐Llano, J. , Salvador Vèrges, A. , & López Seguí, F. (2020). Telemedicine in the face of the COVID‐19 pandemic. Atencion Primaria, 52(6), 418–422. 10.1016/j.aprim.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wajcman, J. (2009). Feminist theories of technology. Cambridge Journal of Economics, 34(1), 143–152. 10.1093/cje/ben057 [DOI] [Google Scholar]
- Wilson, M. (2002). Making nursing visible? Gender, technology and the care plan as script. Information Technology & People, 15(2), 139–158. 10.1108/09593840210430570 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


