Abstract
Introduction
Several techniques and methods have been proposed to cover alveolar bone after tooth extraction when soft tissue is lacking. Some authors recommend soft tissue flap techniques, and others advocate different types of materials for socket covering. In this article, the authors use a modified buccal inversion technique for adequate coverage of the alveolar ridge to ensure its preservation and to minimize soft tissue shrinkage and loss of keratinized gingiva after tooth extraction. This local mucogingival-periosteal plastic procedure was named by the authors the “Buccal Periosteal Inversion technique” or simply BUPI.
Materials and Methods
After extraction of a fractured, endodontically compromised lower right first molar, the BUPI technique was performed to cover the alveolus. After reflecting the two-sided full-thickness flap, the periosteum was split in the cranial direction. The inverted periosteum is used to provide tension-free defect closure of the postextractional defect. Detailed technique implementation and patient postoperative healing are presented here in detail.
Results
Postoperative evaluation at six weeks was presented with photos showing adequate surgical site healing, no signs of infection or dehiscence, and no crestal shift of the keratinized gingiva.
Conclusion
The buccal periosteal inversion (BUPI) technique is a modified technique that allows full socket coverage, avoiding a keratinized gingiva shift in the crestal direction using only the periosteum as a cover material. By inverting the buccal ridge periosteum alone from its normal position, the osteoclastic effect on the buccal bony wall will be eliminated, and this procedure abolishes the need for additional alveolar coverage materials.
Keywords: Periosteum, Periosteal inversion, Periosteum inversion, Buccal ridge preservation, Alveolar protection
1. Introduction
Tooth removal certainly stimulates bone resorption and can produce significant changes in gingival contours. The consideration of three-dimensional alveolar bone will certainly influence further occlusal rehabilitation with dental implants along with their short- and long-term prognoses. Marginal alveolar bone ridge protection and the width of the keratinized gingiva are vital for achieving optimal functional, prosthetic, orthodontic, and aesthetic treatment results.
Tooth extraction is followed by marked osseous changes of the residual alveolar ridge, including severe bone alterations both in height and in width. (Covani et al., 2011)
Alveolar ridge preservation, also referred to as “socket preservation”, is defined as any technique designed to counteract, or even to eliminate, the undesirable effects of postextractional resorption. (De Tullio, et al. 2019)
Alveolar ridge preservation can be achieved with the use of different bone substitutes, which represent an effective method for diminishing the physiological resorption process after tooth extraction. (Majzoub, et al. 2019)
Two common techniques for alveolar ridge preservation after tooth extraction have been described as follows: 1) closure of the extraction wound by primary intention through a flap technique and 2) extraction socket wound healing by secondary intention as an open technique. (Aladmawy et al., 2019)
A third technique involves a group of procedures using free soft tissue grafts or matrices such as plasma rich growth factors (PRGF), plasma rich fibrin (PRF), or collagen to be used as coverage for the alveolus.
The technique described in this article is a new modified procedure of an existing similar technique described by Rosenfeld, 2014. It uses a buccal periosteal inversion to cover the exposed alveolar ridge for its preservation. It has been named by the authors the Buccal Periosteal Inversion technique or BUPI.
1.1. Purpose
The authors hypothesize that the BUPI technique combines the advantages of primary flap closure with the placement of pedicled soft tissue (periosteum) grafts to cover the socket after tooth extraction. This technique can be used for cases of ridge preservation in combination with augmentation material or for plain blood clot stabilization in sites where the width of keratinized gingiva needs to be preserved. The advantages include, but not limited to the following:
1)Prevent alveolar grafts from developing bacterial infection and secondary graft failure obtained by wound primary closure.
2)Minimize soft tissue shrinkage and loss of keratinized gingiva.
3)Reduce the need for grafting membranes, which is frequently used to stabilize the blood clot mechanically.
4)Eliminate soft tissue transplants harvested from another donor site.
5)Stamp out the osteoresorptive effect of the buccal periosteum on its ipsilateral bony ridge.
2. Materials and methods
2.1. Technique description
The BUPI technique follows five steps conveying a scientific routine to facilitate technique reproducibility.
The first step of the BUPI technique includes full thickness flap elevation. It can be performed prior to tooth extraction, if any osteotomy is necessary, or after simple flapless extraction (Fig. 1a). The extent of the flap reflection is beyond the mucogingival line, apical to the mucogingival junction, to provide the necessary depth for further steps. The flap can be elevated beyond the mucogingival line – almost to the mucobuccal fold with one buccal extension. In the presented case, we used a two-sided triangular mucoperiosteal flap (crestal incision and one mesial-buccal extension but no distal-buccal vertical extension). If needed, the flap can be extended through a distal sulcular incision.
Fig. 1.
Schematic representation of the technique. 1a. Socket after tooth extraction. 2b. Horizontal incision of the periosteum will become the base of the periosteal flap. An elevation of a full thickness flap has already been performed. 3c. Preparation of the periosteum was performed with its detachment from the subjacent submucosa in the marginal direction. The inversion of the periosteal flap is performed. 4d. Closure of the alveolar ridge defect with the inverted periosteum to the lingual marginal gingiva. Red = marginally keratinized gingiva, yellow = soft gingiva, green = the periosteum inner layer, and blue = the periosteum outer (fibrous) layer.
The second step involves carrying out a single incision at the base of the periosteum, horizontally, made transversally to the depth of the submucosa from medial to distal aspects of the flap, as presented in Fig. 1b. Caution should be taken not to pass this incision through the soft tissue into the buccal side.
The third step is separation of the periosteum apically from its adhered mucosa towards the marginal direction. The periosteum is left attached only to the keratinized gingiva in its marginal portion as shown in Fig. 1c. In patients with thick and highly keratinized gingiva, the separation of the periosteum can be continued 1–2 mm in the coronal direction, and the marginal gingiva can be split. The minimal attachment between the inverted periosteal flap and buccal mucosal part of the flap is 2–3 mm.
In the fourth step, the prepared periosteal flap can be inverted and positioned tension-free over the alveolar crestal bone to cover the defect (alveolus) as revealed in Fig. 1d.
The fifth and last step involves suturing the inverted periosteum with a 5–0 nonresorbable suture. The outer fibrous layer of the periosteum, which is marked in blue in Fig. 1a-d, has contact with the socket and augmentation material, if used. The inner cambium layer of the periosteum, depicted in green in Fig. 1a-d, is left without contacting the alveolar bone and/or grafting material.
It is important to mention that keratinized gingiva should have the same position as prior to tooth extraction. Any crestal mobilization of the flap and keratinized gingiva will result in loss of its width after wound healing. In our experience, the fine separation of the periosteum from the underlying tissue allows complete tension-free defect closure. The proper performance of the technique eliminates the need for additional fixation of the buccal mucosal flap in the apical direction. If the periosteum is not healthy and correctly freed up from the adjacent submucosa, it has a tendency to pull the whole flap in the crestal direction, which is not beneficial because it reduces the vestibular depth.
2.2. Utilized instrumentation
All incisions for building the MPF were performed with scalpel blade No. 15. For retraction and gentle manipulation of the flaps, dental tweezers or fine surgical tweezers were used. The separation of the periosteum from the underlying tissue can be carried out with sharp dental scissors. Magnification, such as with dental loupes, microscopes and micro instruments for periodontal surgery, can be helpful, but was not used by the authors.
2.3. Case report
A 42-year-old female patient was referred to our OMFS office with fractured tooth number 46. After discussion with the patient about all possible therapeutic alternatives, removal of the tooth through osteotomy and ridge preservation under local anesthesia was accepted. The consent form for this procedure was read, understood, and signed by the patient.
According to the BUPI technique protocol described above, a full thickness flap was elevated with one buccal mesial extension along tooth number 46.
After tooth root extraction was completed without complications, the periosteal flap was designed and inverted as shown in Fig. 2a and b. Socket filling was completed with b-TCP (Cerasorb M, Curasan Inc., Germany) mixed with the patient’s blood. The periosteal flap was carefully positioned to cover the whole grafted area and sutured in place with 5–0 monofil polyamide material (Seralon 5–0, Serag-Wiessner, Naila, Germany) (Fig. 3a).
Fig. 2.
The periosteal portion of the flap. 2a. The periosteal flap being released and elevated to show its extension. 2b. Inversion of the periosteum out of the buccally elevated flap. Note the periosteal attachment to the marginal gingiva.
Fig. 3.
Closure of the alveolus defect. 3a. The inverted periosteum was gently manipulated to cover the grafted alveolus and sutured with 5–0 mononylon material. 3b. Final suturing of the periosteal flap with its inner layer exposed and the vertical border of the releasing incision is sutured back to its precise initial position.
It was possible to close the wound primarily with no crestal shift of the marginal gingiva as illustrated in Fig. 3b.
Amoxicillin 1000 mg was prescribed three times daily for seven days and metamizole to control pain, as needed, after the surgery.
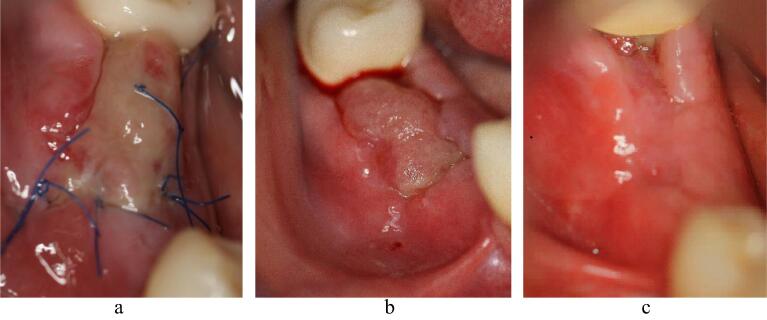
Patient postoperative examination was performed one week after surgery (Fig. 4a). The next follow-up was completed on the fourteenth day (Fig. 4b).
Fig. 4.
Postoperative healing. 4a. Initial healing process depicted after one week. 4b. Healing process on the fourteenth day after extraction. 4c. Healing six weeks after the BUPI technique.
The patient returned six weeks postoperatively, and good surgical wound healing with no signs of infection and/or dehiscence was evident. (Fig. 4c).
3. Discussion
3.1. Techniques for socket/ridge preservation
Alveolar bone ridge preservation strategies have been indicated to minimize loss of volume, which typically follows tooth extraction. (Avila-Ortiz, et al. 2014)
The benefit of socket preservation therapies is affected by the morphology of extraction sockets, type of wound closure, type of grafting materials, use of barrier membranes, use of growth factors and results in significantly less vertical and horizontal contraction of the alveolar bone crest. (Vignoletti et al., 2012, Bassir et al., 2018)
According to Aladmawy et al., 2019, there are two common techniques for alveolar ridge preservation after tooth extraction. One is primary healing of the exposed alveolus by complete flap closure. The other is the secondary healing process of the extraction socket wound when left open.
Primary closure after alveolar ridge augmentation is necessary to preserve the graft from bacterial infections and/or secondary graft failure. To avoid flap elevation, different techniques utilize placement of a free soft tissue graft or matrix (PRGF, PRF, and Collagen) as the cover and protection of the augmented socket. It has also been shown that these techniques minimize soft tissue shrinkage and optimize aesthetic results after dental implantation. (Stimmelmayr et al., 2010. Thalmair et al., 2010, Nevins and Mellonig, 1994)
The positive outcome of a flapless procedure, in terms of soft tissue preservation and improvement, is an increased keratinized gingival width compared with primary closure. (Aladmawy et al., 2019, Lee et al., 2018, Barone et al., 2014, Zhao et al., 2019)
On the other hand, a flap technique seemed to show less vertical bone resorption on the buccal aspect than flapless ridge preservation (Barone et al., 2014). Flap elevation is one of the factors associated with superior outcomes after ridge preservation (Avila-Ortiz, et al. 2014).
3.2. The role of the periosteum
The periosteal membrane consists of an outer fibrous layer of collagen fibers and fibroblasts that maintains its mechanical stability. This layer contains blood vessels and nerves, which supply the bone. The inner osteogenic (cambium) layer, which lies adjacent to the bone, has a high cellular density, including osteoclasts. (Frey, et al., 2013, Hasuike et al., 2019)
Elevation of the periosteal flap induces active angiogenesis and increases vascular permeability, which leads to activation of osteoclasts and bone resorption. After surgery, the interstitium of the elevated mucoperiosteal vascular plexus is filled with sinusoidal new blood vessels, and bone resorption by osteoclasts is observed around those new blood vessels. This process results in an increased resorption rate of the extraction socket after flap elevation. (Fickl et al., 2008)
A study by Tiyapatanaputi et al. (2004) concluded that the absence of the periosteum on transplanted bone blocks resulted in a 75% reduction in osteoclast numbers on bone grafts, which correlated with poor remodeling activity.
Nguyen et al. (2019) showed that the inhibition of osteoclast migration from the periosteum to the bone surface can be used for alveolar ridge preservation. The authors concluded that the modeling of the extraction socket can be prevented by inhibition of osteoclasts on the outer bony surface through the insertion of a nonresorbable membrane underneath the periosteum.
Hasuike et al. 2019 described the use of the periosteum as a barrier for guided bone regeneration. The pedicle periosteum placed just above the bone defect acts more as a barrier rather than a resource of fibrous tissue in bone defects. They advocate the use of the inverted periosteum as a natural occlusal membrane with no potential for soft tissue proliferation in the defect underneath, as is intended in the BUPI technique.
In line with the BUPI technique, the inner periosteal layer, which expresses osteoresorptive properties, is left without contacting the alveolar bone or graft material. Hence, it is hypothesized that preservation of the buccal bone through elimination of osteoclasts on the buccal bone surface will occur with this procedure. Blood supply and elastic fibrous net of the outer periosteal layer is used as an autologous pedicled membrane providing graft and clot stabilization and protection for the alveolus
3.3. The socket augmentation material
In this case, the BUPI was used in combination with a b-TCP graft. The type of augmentation material and its role in the outcome are controversial. (Stumbras, et al., 2019, Faria-Almeida, et al., 2019)
3.4. Classic inverted periosteal technique
Several techniques using the inverted periosteum for defect closure have been published. The article published by Rosenfeld (2014) presented an inverted periosteum technique for defect closure after tooth extraction. The author uses two buccal extensions to elevate the trapezoid flap. The flap is retracted through two long sutures at the corners and with sutures passed only through the periosteum. Presented in this way, the technique needs more buccal space for retraction than the BUPI technique. The author described perforation of the periosteum as a possible complication and its closure with cyanoacrylate tissue adhesive. The use of only a two-sided flap and no additional sutures for retraction in the BUPI technique allows splitting the periosteum with less trauma, and additional adhesive or sutures to close possible perforations were never necessary. In Rosenfeld́s technique, the crestal defect is partially closed with the help of the crestal shift of the buccal mucosa. The BUPI eliminates this shift and the loss of vestibular depth and keratinized tissue, which are undesired complications. Both techniques also have different indications. The prime indication for BUPI is keratinized gingiva width preservation combined with bone augmentation or blood cloth stabilization. Rosenfeld’s periosteal inversion is used for oroantral communication closure.
4. Conclusion
Buccal Periosteal Inversion - BUPI - for defect closure and keratinized gingiva width preservation is a modified technique that up to now has not been described in its format as a primary technique, which applies a full horizontal incision transversally applied on the buccal mucosa flap for alveolus defects coverage after tooth extraction. With this modification proposed on the BUPI technique, the major disadvantage observed by (Rosenfeld, 2014) in his own technique, translated into a reduction of the vestibular depth, which was never observed in our series of cases because the mucosa is never elevated together with the periosteum.
The BUPI technique allows full socket coverage while not permitting any shift or reallocation, in any direction, of the keratinized gingiva in the crestal-marginal direction.
The BUPI technique uses only the adjacent buccal periosteum to close bone defects and does not require any additional covering materials, such as membrane, matrix, or autologous soft tissue transplants.
Detachment of the periosteum from its submucosa, a crestal pedicle attachment and its inversion, removes the buccal ridge periosteum of its normal position, possibly eliminating the osteoclast effect in its inner cambium layer on the buccal bony wall.
The outer fibrous layer of the inverted periosteum can serve as perfect coverage and protection for any type of graft (organic, inorganic or alloplastic) material placed inside the socket when necessary and recommended.
CRediT authorship contribution statement
Ivan Hristov Arabadzhiev: Conceptualization, Methodology, Investigation, Writing - original draft. Peter Maurer: Methodology, Resources, Writing - review & editing, Visualization, Supervision. Eber Luis Lima Stevao: Conceptualization, Methodology, Investigation, Writing - review & editing, Visualization.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
References
- Aladmawy M.A., et al. A Comparison between Primary and Secondary Flap Coverage in Ridge Preservation Procedures: A Pilot Randomized Controlled Clinical Trial. Biomed Res. Int. 2019;2019(7679319):20. doi: 10.1155/2019/7679319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avila-Ortiz G., et al. Effect of alveolar ridge preservation after tooth extraction: a systematic review and meta-analysis. J. Dent. Res. 2014;93(10):950–958. doi: 10.1177/0022034514541127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barone A., Toti P., Piattelli A., et al. Extraction socket healing in humans after ridge preservation techniques: comparison between flapless and flapped procedures in a randomized clinical trial. J. Periodontol. 2014;85(1):14–23. doi: 10.1902/jop.2013.120711. Epub 2013 May 20 PubMed PMID: 23688103. [DOI] [PubMed] [Google Scholar]
- Bassir SH, Alhareky M, Wangsrimongkol B, et al. Systematic Review and Meta-Analysis of Hard Tissue Outcomes of Alveolar Ridge Preservation. Int. J. Oral Maxillofac Implants. 2018 Sep/Oct;33(5):979-994. doi: 10.11607/jomi.6399. Review. PubMed PMID: 30231083. [DOI] [PubMed]
- Covani U., Ricci M., Bozzolo G., et al. Analysis of the pattern of the alveolar ridge remodelling following single tooth extraction. Clin. Oral. Implants Res. 2011;22(8):820–825. doi: 10.1111/j.1600-0501.2010.02060.x. Epub 2010 Dec 29 PubMed PMID: 21198897. [DOI] [PubMed] [Google Scholar]
- De Tullio, Ilaria et al. “A Human Clinical and Histomorphometrical Study on Different Resorbable and Non-Resorbable Bone Substitutes Used in Post-Extractive Sites. Preliminary Results.” Materials (Basel, Switzerland) vol. 12,15 2408. 28 Jul. 2019, doi:10.3390/ma12152408. [DOI] [PMC free article] [PubMed]
- Faria-Almeida, Ricardo et al. “Extraction Socket Preservation with or without Membranes, Soft Tissue Influence on Post Extraction Alveolar Ridge Preservation: a Systematic Review.” J Oral Maxillofac Res. vol. 10,3 e5. 5 Sep. 2019, doi:10.5037/jomr.2019.10305. [DOI] [PMC free article] [PubMed]
- Fickl S., Zuhr O., Wachtel H., et al. Tissue alterations after tooth extraction with and without surgical trauma: a volumetric study in the beagle dog. J. Clin. Periodontol. 2008;35(4):356–363. doi: 10.1111/j.1600-051X.2008.01209.x. PubMed PMID: 31209434. [DOI] [PubMed] [Google Scholar]
- Frey, Sönke Percy et al. “Immunohistochemical and molecular characterization of the human periosteum.” Sci. World J. vol. 2013 341078. 2 May. 2013, doi:10.1155/2013/341078. [DOI] [PMC free article] [PubMed]
- Hasuike A., Ujiie H., Senoo M., et al. Pedicle Periosteum as a Barrier for Guided Bone Regeneration in the Rabbit Frontal Bone. Vivo. 2019;33(3):717–722. doi: 10.21873/invivo.11530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J, Lee JB, Koo KT, et al. Flap Management in Alveolar Ridge Preservation: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2018 May/Jun;33(3):613-621. doi: 10.11607/jomi.6368. Review. PubMed PMID: 29763499. [DOI] [PubMed]
- Majzoub, Jad et al. “The Influence of Different Grafting Materials on Alveolar Ridge Preservation: a Systematic Review.” J Oral Maxillofac Res. vol. 10,3 e6. 5 Sep. 2019, doi:10.5037/jomr.2019.10306. [DOI] [PMC free article] [PubMed]
- Nevins M., Mellonig J.T. The advantages of localized ridge augmentation prior to implant placement: a staged event. Int J Periodontics Restorative Dent. 1994;14(2):96–111. PubMed PMID: 7928133. [PubMed] [Google Scholar]
- Nguyen V., von Krockow N., Pouchet J., et al. Periosteal Inhibition Technique for Alveolar Ridge Preservation as It Applies to Implant Therapy. Int J Periodontics Restorative Dent. 2019;39(5):737–744. doi: 10.11607/prd.4178. [DOI] [PubMed] [Google Scholar]
- Rosenfeld E.A. Inverted periosteal flap: an alternative to the buccal advancement flap for tension-free, watertight closure. J. Oral Maxillofac. Surg. 2014;72(7):1244–1250. doi: 10.1016/j.joms.2014.03.006.Epub. 2014 Mar 20, PMID:24768423. [DOI] [PubMed] [Google Scholar]
- Stimmelmayr M., Allen E.P., Reichert T.E., et al. Use of a combination epithelized-subepithelial connective tissue graft for closure and soft tissue augmentation of an extraction site following ridge preservation or implant placement: description of a technique. Int J Periodontics Restorative Dent. 2010;30(4):375–381. PubMed PMID: 20664839. [PubMed] [Google Scholar]
- Stumbras, Arturas et al. “Alveolar Ridge Preservation after Tooth Extraction Using Different Bone Graft Materials and Autologous Platelet Concentrates: a Systematic Review.” J Oral Maxillofac Res.vol. 10,1 e2. 31 Mar. 2019, doi:10.5037/jomr.2019.10102 [DOI] [PMC free article] [PubMed]
- Thalmair T., Hinze M., Bolz W., et al. The Healing of Free Gingival Autografts for Socket-seal Surgery: a Case Report. Eur. J Esthet Dent. 2010;5(4):358–368. PubMed PMID: 21069107. [PubMed] [Google Scholar]
- Tiyapatanaputi P., Rubery P.T., Carmouche J., et al. A novel murine segmental femoral graft model. J. Orthop. Res. 2004;22(6):1254–1260. doi: 10.1016/j.orthres.2004.03.017. PubMed PMID: 15475206. [DOI] [PubMed] [Google Scholar]
- Vignoletti F., Matesanz P., Rodrigo D., et al. Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin Oral Implants Res. 2012;23(Suppl 5):22–38. doi: 10.1111/j.1600-0501.2011.02331.x. PubMed PMID: 22211304. [DOI] [PubMed] [Google Scholar]
- Zhao LP, Hu WJ, Xu T,et al. [Two procedures for ridge preservation of molar extraction sites affected by severe bone defect due to advanced periodontitis]. Beijing Da Xue Xue Bao Yi Xue Ban. 2019 Jun 18;51(3):579. [DOI] [PMC free article] [PubMed]