Abstract
Background
Pain, edema, and trismus are predictable sequelae for surgical extraction of impacted mandibular third molars (M3M). The present study aimed to compare the anti-phlogistic potential of bromelain and aceclofenac in the reduction of post-surgical sequalae in the extraction of impacted M3M.
Method
A randomized controlled, triple-blinded clinical study included 72 patients scheduled for surgical removal of impacted M3M under local anesthesia. Randomization was performed and subjects were equally allocated to groups A (control) and B (study), who intended to receive aceclofenac and bromelain, respectively. The primary outcome variables were pain, edema, and trismus evaluated on postoperative days 2 and 7 and compared with baseline values. The secondary variables evaluated were the quantity of rescue analgesics required and the frequency of adverse effects in both groups for 7 postoperative (PO) days. Data were analyzed with a level of significance of P < 0.05.
Results
Group B demonstrated a significant decrease in the severity of edema and trismus compared to group A on both PO days 2 and 7 (P < 0.001). Bromelain demonstrated similar analgesic efficacy with an insignificant difference compared to aceclofenac (P > 0.05).
Conclusion
The present study showed that the efficacy of bromelain was comparable to that of aceclofenac in reducing inflammatory complications following surgical removal of impacted M3M. Bromelain can be considered a safe and potent alternative to routinely used aceclofenac when addressing inflammatory outcomes after surgery.
Keywords: Aceclofenac, Bromelain, Edema, Mandible, Pain, Third Molar, Trismus
INTRODUCTION
The probable sequelae of impacted mandibular third molar (M3M) surgery are pain, edema, and trismus arising secondary to tissue inflammation following surgical trauma to soft and bony tissue in the acute post-surgical period [1]. It adversely influences a patient’s quality of life by affecting overall comfort, limitation in daily routine activities, sleep, mastication, trismus, phonetics, and smiling [1,2]. Its management demands relevant knowledge of the anatomy of contiguous structures.
To limit these post-surgical inflammatory complications, such as edema, pain, and trismus, surgeons have improvised surgical techniques and instrumentation for precise execution and include various modalities such as Light Amplification by Stimulated Emission of Radiation (LASER), tapes, sutures, ozone gel, enzyme therapy, and cryotherapy [2,3,4].
Non-steroidal anti-inflammatory drugs (NSAIDs) are a time-honored and trusted modality to reduce the post-surgical inflammatory sequelae of impacted M3M surgery. NSAIDs act directly by inhibiting the enzyme cyclo-oxygenase. However, the therapeutic safety index of NSAIDs is narrow [5]. NSAIDs restrict the production of prostaglandins, with variable reduction of COX-1 and COX-2, which increases the risk of gastrointestinal bleeding, MI, and stroke [5]. The most common side effects include dyspepsia, gastroduodenal ulcers, hypertension, edema, electrolyte imbalance, nephrotic syndrome, and chronic kidney disease. To overcome these limitations, the quest for an equally efficacious drug is burgeoning.
Bromelain, a phytoenzyme with proteolytic action, was derived from the stem of pineapple in 1957 [6,7,8]. Bromelain has attracted special interest in the domain of maxillofacial surgery because of its anti-phlogistic, analgesic, and anti-fibrinolytic properties [8,9,10]. It acts by affecting the concentration of the cyclo-oxygenase 2 enzyme and thereby leukocyte activation [11]. Bromelain can have a variety of applications in fibrinolysis, aggregation of platelets, anticancer drugs, immune modulators, and mucolysis [12,13,14,15]. Bromelain is a drug with moderate efficacy and minimal adverse effects. Bromelain has shown significant results in limiting post-surgical inflammatory outcomes [16,17,18].
Diclofenac sodium is the most commonly prescribed NSAID among maxillofacial surgeons. A multitude of studies have demonstrated comparable efficacy of bromelain with diclofenac sodium. Aceclofenac is another drug belonging to the same class as diclofenac and demonstrates efficacy similar to that of diclofenac sodium. However, the incidence of epigastric pain, nausea, and vomiting was significantly greater with diclofenac sodium than with aceclofenac. Recently, a study compared aceclofenac and diclofenac in the removal of impacted M3M and concluded that aceclofenac is a promising analgesic that affords effective and enhanced analgesia with a faster onset and prolonged effect and better patient acceptance than diclofenac [5]. The present study was designed to highlight the efficacy of bromelain as a drug of choice to overcome the adverse effects of conventionally used NSAIDs and to reduce the frequency of postoperative complications following the removal of impacted M3M.
There is a dearth of literature comparing bromelain and aceclofenac alone in third molar surgery. In line with this, we performed a prospective, randomized, controlled, clinical study comparing the efficacy of “bromelain” against “aceclofenac” in reducing the post-operative sequelae following removal of impacted M3M with the hypothesis that bromelain is equally efficacious as aceclofenac in minimizing postoperative (PO) sequalae after surgical extraction of impacted M3M.
METHODS
The present prospective, randomized controlled, triple-blinded, parallel arm study design included 72 systemically healthy subjects belonging to ASA PS class I category with age range between 18 to 40 years with adequate mouth opening (≥ 35 mm) and a body mass index BMI score ranging from 18.5 to 24.9 (Table 1) who were scheduled for surgical removal of atleast one asymptomatic impacted M3M (class II position B, moderate to difficult) between October 2019 to June 2020 at the outpatient department of Oral and Maxillofacial Surgery. The study was initiated after the approval from the Central and Institutional Ethical Committee on Human Research (Ref. No. DMIMS [(DU])/IEC/Sept 2019/8507). The study conformed to the Helsinki Declaration and its later amendments and institutional ethical guidelines.
Table 1. Demographic details of the study population.
| N = 72 | Group A (N = 36) | Group B (N = 36) | P-Value |
|---|---|---|---|
| Age | 31.74 ± 4.12 | 30.72 ± 4.24 | 0.107, NS |
| Gender | Male: 14, Female: 22 | Male: 13, Female: 23 | 0.100, NS |
| Weight | 50 ± 3.5 | 49.8 ± 3.7 | 0.460, NS |
| Height | 159.0 ± 3.1 | 160.0 ± 4.9 | 0.242, NS |
| BMI | 21.4 ± 2.5 | 20.5 ± 3.7 | 0.06, NS |
| ASA PS class | class I: 36 | class I: 36 | 1.00, NS |
ASA PS, American Society of Anesthesiologists physical status; BMI, body mass index; NS, not significant.
The sample size required for this study was calculated at a 95% confidence interval and 80% power of the study.
where is the critical value of the normal distribution at (for a confidence level of 95%, α is 0.05, and the critical value is 1.96), Zβ is the critical value of the normal distribution at β (power of 80%, β is 0.2, and the critical value is 0.84), σ2 is the population variance, and d is the difference that can be detected.
N = 72
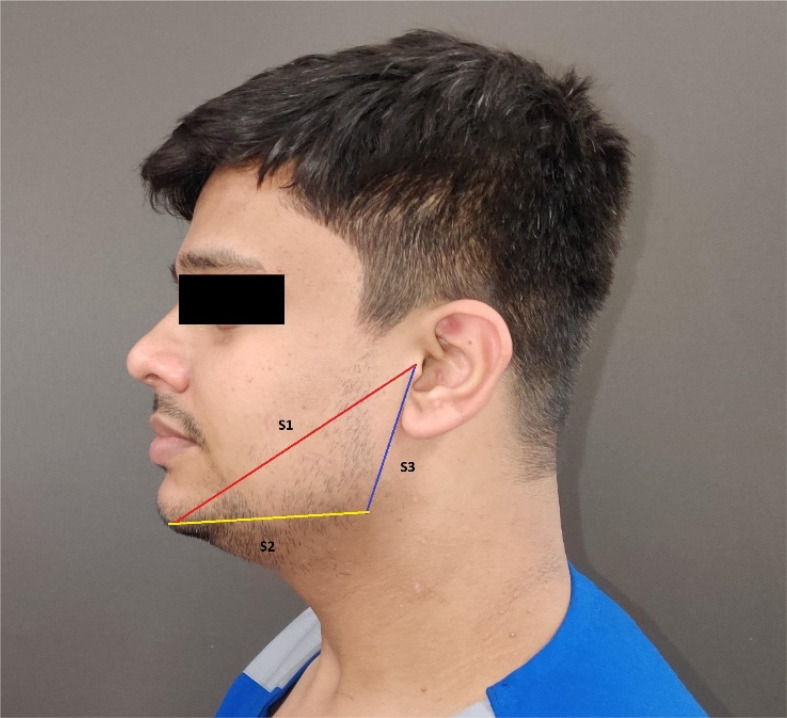
Subjects who were systemically compromised, chronic smokers, pregnant and lactating women, with periapical infection, and patients with drug allergy used in the study were excluded. Routine hematological and serological investigations (hemoglobin, clotting time, bleeding time, Random Blood Sugar (RBS), Hepatitis B surface antigen (HBsAg) and human immunodeficiency virus (HIV) were ordered for each subject and described in detail about the study policy and 10-point visual analog scale (VAS) [15]. Facial measurements were recorded using a measuring tape by taking the mean of the distance between fixed landmarks, such as tragus to menton (S1), menton to the angle of the mandible (S2), and angle of the mandible to the tragus (S3) (Fig. 1) [16]. Preoperative inter-incisal mouth opening was measured using a standard calibrated ruler. These linear measurements were compared to measurements recorded postoperatively on days 2 and 7 during the follow-up visit (Fig. 2). All nerve blocks and surgical procedures were performed by a single surgeon. All subjects were given the same standard postoperative instructions and were instructed not to consume any analgesic until the time a subject experienced a pain score ≥ 4 on the VAS.
Fig. 1. Pre-operative measurements for facial swelling.
Fig. 2. Preoperative measurement for interincisal mouth opening (frontal view).
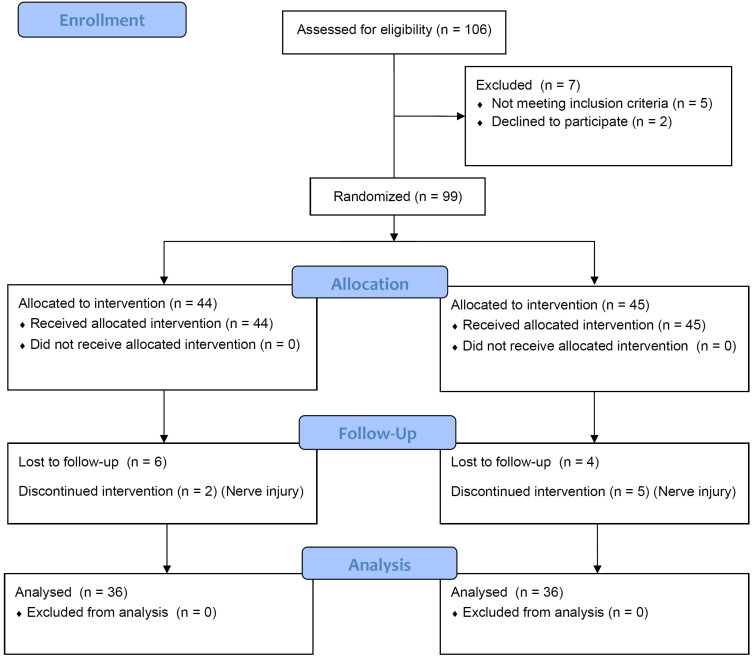
Subjects were randomized and distributed equally (n = 36) to two different groups using a computer-generated table of random numbers, irrespective of their age and sex, using a sealed opaque envelope. Group B was designated as the study group, while group A served as the control. The subjects in group B (n = 36) were selected to receive bromelain 500 mg capsules 8 hourly for 5 days (500 mg, bromelain, Simply Nutra®, India), while the subjects in group A (n = 36) received aceclofenac 100 mg (Zerodol®, ICPA) 12 hourly for 5 d. Allocation of the drugs to the group was decoded and dispensed by the pharmacist in a sealed opaque envelope in both groups and was concealed to the operating surgeon, patient, and investigator, making it a triple-blind design. The subjects were completely unaware of the composition of the prescribed drugs. The sutures were removed after 7 days. Subjects were requested to report to the clinic on postoperative days 2 and 7 as per the study protocol. The study conformed with the Consolidated Standards of Reporting Trials [19] guidelines for randomized controlled trials (Fig. 3).
Fig. 3. Consolidated Standards of Reporting Trials flow diagram.
Statistical analysis was conducted using descriptive and inferential statistics, including the chi square test, Student’s t test, repeated measures ANOVA with post hoc pairwise comparison, Statistical Package for Social Sciences (IBM SPSS Statistics 27.0, IBM Co., NY, USA). Statistical significance was set at P < 0.05.
RESULTS
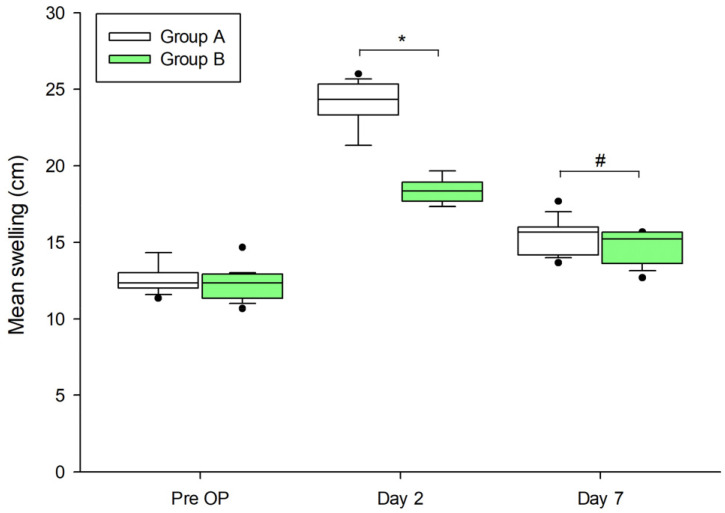
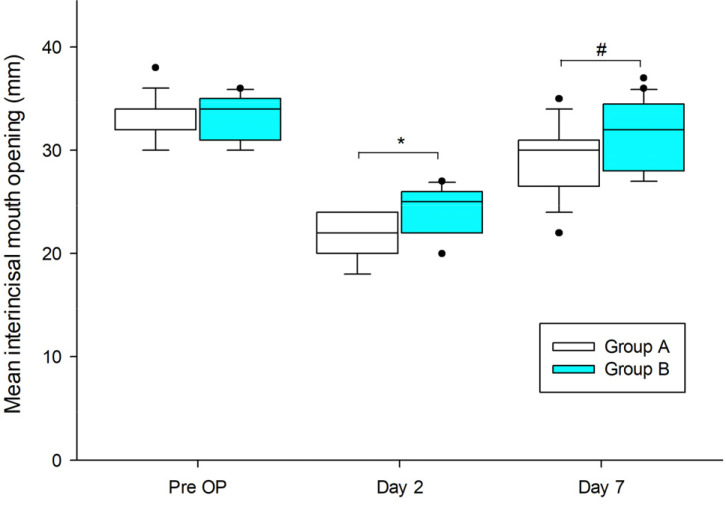
The present study included 72 subjects with a mean age of 30.72 ± 10.14 ranging 18-40 years. The study population comprised 45 women (62.50%). The mean pain score on day 2 and day 7 were 5.83 ± 0.60 and 1.55 ± 0.90, respectively, for group B, whereas 6.05 ± 0.67 and 1.22 ± 0.42, respectively, for group A. The pain was significantly reduced on PO days 2 and 7 in both groups, with insignificant differences (P > 0.05) (Table 2). The mean score of swelling in group A was found to be 24.12± 1.54 and 15.46 ± 1.14 on days 2 and 7, respectively. Whereas, the mean score of swelling was found to be 18.28 ± 0.73 and 14.74 ± 1.03 on days 2 and 7, respectively in group B (Fig. 4). The mean interincisal mouth opening (mm) on PO days 2 and 7 were found to be 24.30 ± 2.14 and 31.38 ± 3.41, respectively in group B (Fig. 5). The mean interincisal mouth opening (mm) in group A on PO days 2 and 7 were 21.44 ± 2.22 and 29.14 ± 3.58, respectively. Edema and trismus varied significantly in both the groups on PO days 2 and 7 (P < 0.001) (Fig. 4, 5). There were no significant differences (P > 0.05) in the total number of rescue analgesics consumed on days 1 through 7 in both groups, indicating comparable analgesic efficacy of both drugs. Sixty percent (n = 28) of individuals experienced varying degrees of adverse effects among subjects in group A, while there were 9% in group B (n = 4). Both groups showed significant differences between the groups (P < 0.05).
Table 2. Comparison of pain on VAS in two groups.
| Day | Group A | Group B | P-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Day 2 | 5.83 | 0.60 | 6.05 | 0.67 | P = 0.47, NS |
| Day 7 | 1.55 | 0.90 | 1.22 | 0.42 | P = 0.32, NS |
NS, not significant; SD, standard deviation; VAS, visual analogue scale.
Fig. 4. Comparison of swelling in two groups at days 2 and 7 (*: P < 0.001, #: P = 0.006, repeated measures ANOVA with post hoc pairwise comparison). Group A, aceclofenac; Group B, bromelain; Pre OP, Pre-operative.
Fig. 5. Comparison of interincisal mouth opening (mm) in two groups at days 2 and 7 (*: P < 0.001, #: P = 0.008, repeated measures ANOVA with post hoc pairwise comparison). Pre OP, Pre-operative.
DISCUSSION
The control of pain and post-operative inflammation in dentistry is a major concern as they are determinants of the success of the techniques employed and the procedure. Adequate control of postoperative pain and inflammation leads to greater patient comfort, satisfaction, shorter hospital stay, brief convalescence, early return to daily activities, less analgesic dependence, and overall better quality of life.
NSAIDs have been shown to be an established and reliable therapeutic strategy for analgesia and control of edema in surgical extraction of impacted M3M, albeit with side effects such as dyspepsia, gastroduodenal ulcers, hypertension, edema, electrolyte imbalance, myocardial infarction, stroke, nephrotic syndrome, and chronic kidney disease. The quest for the search for an anti-inflammatory agent with minimal side effects has led to the advent of bromelain. Bromelain, a phytoenzyme extracted from pineapple stem, is a proven drug with moderate efficacy and minimal side effects [16]. Although bromelain effectively performs fibrinolysis and restricts blood coagulation by suppressing ADP-induced platelet aggregation, it delays both prothrombin time and activated partial thromboplastin time. It limits the formation of intermediates of the clotting cascade by acting on factor X and prothrombin. It also reduces prekallikrein, thereby reducing bradykinin formation. This will lead to an increased bleeding tendency and hence should be avoided in patients with bleeding disorders [20].
The antiphlogistic efficacy of bromelain in the surgical extraction of impacted M3M is well acknowledged [5,15,16,17,18,21,22,23,24,25,26,27]. Multiple studies have postulated the plausible mode of action of bromelain [23,24,28]. It is used in diverse clinical conditions such as the management of thrombophlebitis, bronchitis, sinusitis, and angina pectoris [29]. Bromelain was found to be effective in reducing PO complications after surgical extraction of impacted M3M [5,15,16,17,18]. Aceclofenac, a relatively new class of aryl-acetic acid, exhibited efficacy comparable to that of diclofenac, with a lower frequency of adverse effects.
The present study was designed to evaluate the efficacy of bromelain vs. aceclofenac in a triple-blinded, parallel-arm, randomized controlled manner with the hypothesis that bromelain is an equally efficacious drug in minimizing postoperative inflammatory outcomes associated with the removal of impacted M3M. The primary outcome variables of the current study were to evaluate “pain,” “edema,” and “trismus” on the administration of bromelain and aceclofenac in the surgical removal of impacted M3M. The requirement for the number of rescue analgesics and the frequency of adverse effects with drug consumption were treated as secondary outcome variables.
The investigators of the current study attempted to select a standardized sample by having well-controlled determinants of post-operative inflammation in the extraction of IM3M, such as age, sex, asymptomatic impacted M3M, surgeon’s experience, and the quantity of the anesthetic agent used. The present study included 45 women and 27 men with a ratio of 1.5:1, with a mean age of 30.72 ± 10.14 ranging between 18 and 40 years were randomly assigned to groups A and B (Table 1). This can be ascertained by the resemblance assessed with respect to the surgical time required. The duration of surgery is an important factor that has been found to influence PO inflammatory sequelae following removal of impacted M3M [25,26,27,30,31]. The mean duration of the surgery was 44.64 ± 6.22 for group B and 45.97 ± 5.70 for group A respectively. The results demonstrated an insignificant difference (P = 0.92, NS) between the two groups.
The propensity for pain generated by noxious stimuli is usually biphasic in nature. It is generated not only at the time of incision placement but also occurs due to chemical mediators released by virtue of the surgical trauma and persists throughout the PO phase. The mean pain score was found to be severe on day 2 and ceased in day 7. The mean pain score on day 2 and day 7 were 5.83 ± 0.60 and 1.55 ± 0.90, respectively for group B, whereas 6.05 ± 0.67 and 1.22 ± 0.42 respectively for group A. The mean pain intensity score across both groups on days 2 and 7 varied insignificantly (P > 0.05) (Table 2). These results were in agreement with previous literature [27,30,31,32,33]. However, few studies have established the improved analgesic efficacy of bromelain [23,32]. The mean value of consumption of the number of rescue analgesics in the subjects of group B and A were found to be 0.21 ± 0.05 and 0.18 ± 0.13 but was statistically insignificant (P = 0.25). The results of the present study are consistent with that of another study [23].
Postoperative edema is a common event following the removal of impacted M3M. Facial edema is a response to inadvertent trauma to the soft and bony tissues. It may adversely impact psychosocial well-being and the social and working lives of patients. The severity of facial edema score varied significantly on days 2 and 7 across both groups (P < 0.001) (Fig. 4) [16,21]. The facial edema was more severe on PO day 2 and gradually returned to the preoperative facial contours by postoperative day 7 in both groups. These results exemplify the pronounced anti-inflammatory effects in group B. The results are in agreement with those of other reported studies [31]. In contrast to the above, several authors found comparable results in the reduction of postoperative edema [30].
Trismus has a multifactorial etiology and cannot be attributed to a single cause. The causative factors of trismus include needle penetration injury to the muscle, erroneous design of the incision, inadvertent trauma to the soft and bony tissues owing to the injudicious use of instruments, overzealous stripping of muscles, and thermal injuries; however, these cannot be overlooked. Trismus is an inflammatory sequel that is directly associated with pain and edema. It is the result of the accumulation of fluid below the fascia of the masticatory muscles and adversely influences the quality of life. It is the physiological splinting of the muscles to avoid pain. It may occur due to hematoma and edema secondary to muscle injury due to injection. Trismus was evaluated as the maximal passive inter-incisal opening calculated using a calibrated ruler preoperatively and compared with values obtained on days 2 and 7 postoperatively.
Trismus varied greatly between the two groups on two consecutive follow-up days. In the present study, trismus was markedly less during the entire postoperative period in group B than in group A. Trismus worsened in the aceclofenac group as compared to the bromelain group on PO days 2 and 7. The inter-incisal opening returned earlier to its premorbid status (P < 0.001) in the bromelain group, while group A (P < 0.001) (Fig. 5) experienced trismus for a prolonged duration. This effect may be attributable to the consumption of the proteolytic enzyme bromelain in patients in group B. These observations agree with those of other trials [33]. In contrast, few studies have found bromelain to be ineffective in reducing trismus.
The present study assessed the frequency of adverse effects associated with bromelain and aceclofenac. Bromelain showed significantly better results with minimal side effects than aceclofenac (P < 0.001). In terms of reporting the frequency of adverse effects of the drugs, 9% of the subjects in group B and 70% of the subjects of group A experienced minor degrees of gastrointestinal complications in the form of epigastric pain, gastritis, nausea, and vomiting. Patients were prescribed proton pump inhibitors to alleviate gastrointestinal symptoms.
Beyond comparable variables, such as pain, edema, and trismus, may vary with individuals’ inherent response to the inflammation.
In conclusion, it was shown that bromelain exerted an enhanced anti-inflammatory action and a similar analgesic effect compared to aceclofenac with minimal side effects. Bromelain has anti-phlogistic, analgesic, anti-tumorigenic, anti-fibrotic, and anti-thrombotic properties, with minimal side effects and minimal drug interactions, making it an attractive alternative to NSAIDs in controlling inflammatory reactions in systemically healthy as well as immunocompromised subjects. Bromelain may have the potential to outweigh the conventional use of NSAIDs in the surgical extraction of impacted M3M.
Footnotes
- Aishwarya Ashok Gupta: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft.
- Rajanikanth Kambala: Conceptualization, Writing – original draft.
- Nitin Bhola: Writing – review & editing.
- Anendd Jadhav: Writing – review & editing.
DECLARATION OF INTEREST: The authors have no conflicts of interest.
References
- 1.Savin J, Ogden GR. Third molar surgery--a preliminary report on aspects affecting quality of life in the early postoperative period. Br J Oral Maxillofac Surg. 1997;35:246–253. doi: 10.1016/s0266-4356(97)90042-5. [DOI] [PubMed] [Google Scholar]
- 2.Antunes AA, Avelar RL, Martins Neto EC, Frota R, Dias E. Effect of two routes of administration of dexamethasone on pain, edema, and trismus in impacted lower third molar surgery. Oral Maxillofac Surg. 2011;15:217–223. doi: 10.1007/s10006-011-0290-9. [DOI] [PubMed] [Google Scholar]
- 3.Genc A, Cakarer S, Yalcin BK, Kilic BB, Isler SC, Keskin C. A comparative study of surgical drain placement and the use of kinesiologic tape to reduce postoperative morbidity after third molar surgery. Clin Oral Investig. 2019;23:345–350. doi: 10.1007/s00784-018-2442-x. [DOI] [PubMed] [Google Scholar]
- 4.Carrillo JS, Calatayud J, Manso FJ, Barberia E, Martinez JM, Donado M. A randomized double-blind clinical trial on the effectiveness of helium-neon laser in the prevention of pain, swelling and trismus after removal of impacted third molars. Int Dent J. 1990;40:31–36. [PubMed] [Google Scholar]
- 5.Chunduri N, Kollu T, Goteki VR, Mallela KK, Madasu K. Efficacy of aceclofenac and diclofenac sodium for relief of postoperative pain after third molar surgery: a randomised open label comparative study. J Pharmacol Pharmacother. 2013;4:144–145. doi: 10.4103/0976-500X.110910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.da Silva FRP, Vasconcelos ACCG, Alves EHP, de Oliveira Junior PV, de Oliveira JS, Vasconcelos DFP. Bromelain: a potential strategy for the adjuvant treatment of periodontitis. Dent Hypotheses. 2016;7:88–93. [Google Scholar]
- 7.Orsini RA Plastic Surgery Educational Foundation Technology Assessment Committee. Bromelain. Plast Reconstr Surg. 2006;118:1640–1644. doi: 10.1097/01.prs.0000242503.50548.ee. [DOI] [PubMed] [Google Scholar]
- 8.Rachmawati H, Sulastri E, Iwo MI, Safitri D, Rahma A. Bromelain encapsulated in self assembly nanoemulsion exhibits better debridement effect in animal model of burned skin. J Nano Res. 2016;40:158–166. [Google Scholar]
- 9.Maurer HR. Bromelain: biochemistry, pharmacology and medical use. Cell Mol Life Sci CMLS. 2001;58:1234–1245. doi: 10.1007/PL00000936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bormann KH, Weber K, Kloppenburg H, Staude P, Koch A, Meiser P, et al. Perioperative bromelain therapy after wisdom teeth extraction - a Randomized, placebo-controlled, double-blinded, three-armed, cross-over dose-finding study. Phytother Res. 2016;30:2012–2019. doi: 10.1002/ptr.5707. [DOI] [PubMed] [Google Scholar]
- 11.Bala M, Ismail NA, Mel M, Jami MS, Salleh HM, Amid A. Bromelain production: current trends and perspective. Arch Sci. 2012;65:369–399. [Google Scholar]
- 12.Bhattacharyya BK. Bromelain: an overview. Indian J Nat Prod Resour. 2008;7:359–363. [Google Scholar]
- 13.de Souza GM, Fernandes IA, Dos Santos CRR, Falci SGM. Is bromelain effective in controlling the inflammatory parameters of pain, edema, and trismus after lower third molar surgery? A systematic review and meta-analysis. Phytother Res. 2019;33:473–481. doi: 10.1002/ptr.6244. [DOI] [PubMed] [Google Scholar]
- 14.Scocca J, Lee YC. The Composition and Structure of the Carbohydrate of Pineapple Stem Bromelain. J Biol Chem. 1969;244:4852–4863. [PubMed] [Google Scholar]
- 15.Berge TI. Visual analogue scale assessment of postoperative swelling: a study of clinical inflammatory variables subsequent to third-molar surgery. Acta Odontol Scand. 1988;46:233–240. doi: 10.3109/00016358809004772. [DOI] [PubMed] [Google Scholar]
- 16.Inchingolo F, Tatullo M, Marrelli M, Inchingolo AM, Picciariello V, Inchingolo AD, et al. Clinical trial with bromelain in third molar exodontia. Eur Rev Med Pharmacol Sci. 2010;14:771–774. [PubMed] [Google Scholar]
- 17.Howat RC, Lewis GD. The effect of bromelain therapy on episiotomy wounds--a double blind controlled clinical trial. J Obstet Gynaecol Br Commonw. 1972;79:951–953. doi: 10.1111/j.1471-0528.1972.tb12194.x. [DOI] [PubMed] [Google Scholar]
- 18.Taussig SJ, Batkin S. Bromelain, the enzyme complex of pineapple (Ananas comosus) and its clinical application. An update. J Ethnopharmacol. 1988;22:191–203. doi: 10.1016/0378-8741(88)90127-4. [DOI] [PubMed] [Google Scholar]
- 19.Schulz KF, Altman DG, Moher D CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Errasti ME, Prospitti A, Viana CA, Gonzalez MM, Ramos MV, Rotelli AE, et al. Effects on fibrinogen, fibrin, and blood coagulation of proteolytic extracts from fruits of Pseudananas macrodontes, Bromelia balansae, and B. hieronymi (Bromeliaceae) in comparison with bromelain. Blood Coagul Fibrinolysis. 2016;27:441–449. doi: 10.1097/MBC.0000000000000531. [DOI] [PubMed] [Google Scholar]
- 21.Hotz G, Frank T, Zöller J, Wiebelt H. Antiphlogistic effect of bromelain following third molar removal. Dtsch Zahnarztl Z. 1989;44:830–832. [PubMed] [Google Scholar]
- 22.Lotz-Winter H. On the pharmacology of bromelain: an update with special regard to animal studies on dose-dependent effects. Planta Med. 1990;56:249–253. doi: 10.1055/s-2006-960949. [DOI] [PubMed] [Google Scholar]
- 23.Kamenícek V, Holán P, Franĕk P. Systemic enzyme therapy in the treatment and prevention of post-traumatic and postoperative swelling. Acta Chir Orthop Traumatol Cech. 2001;68:45–49. [PubMed] [Google Scholar]
- 24.Gaspani L, Limiroli E, Ferrario P, Bianchi M. In vivo and in vitro effects of bromelain on PGE(2) and SP concentrations in the inflammatory exudate in rats. Pharmacology. 2002;65:83–86. doi: 10.1159/000056191. [DOI] [PubMed] [Google Scholar]
- 25.Walker AF, Bundy R, Hicks SM, Middleton RW. Bromelain reduces mild acute knee pain and improves well-being in a dose-dependent fashion in an open study of otherwise healthy adults. Phytomedicine. 2002;9:681–686. doi: 10.1078/094471102321621269. [DOI] [PubMed] [Google Scholar]
- 26.Ogden GR. Third molar surgery and postoperative pain relief. Br Dent J. 2003;194:261 [Google Scholar]
- 27.Báez R, Lopes MT, Salas CE, Hernández M. In vivo antitumoral activity of stem pineapple (Ananas comosus) bromelain. Planta Med. 2007;73:1377–1383. doi: 10.1055/s-2007-990221. [DOI] [PubMed] [Google Scholar]
- 28.Banihashemrad SA, Nasrabadi N, Rajabi O, Kanafi AR, Taher M. Impact of bromelain on wound healing and complications after periodontal surgery. Arch Pharm Pract. 2020;11:38–41. [Google Scholar]
- 29.Ordesi P, Pisoni L, Nannei P, Macchi M, Borloni R, Siervo S. Therapeutic efficacy of bromelain in impacted third molar surgery: a randomized controlled clinical study. Quintessence Int. 2014;45:679–684. doi: 10.3290/j.qi.a32237. [DOI] [PubMed] [Google Scholar]
- 30.Kumakura S, Yamashita M, Tsurufuji S. Effect of bromelain on kaolin-induced inflammation in rats. Eur J Pharmacol. 1988;150:295–301. doi: 10.1016/0014-2999(88)90010-6. [DOI] [PubMed] [Google Scholar]
- 31.Singh T, More V, Fatima U, Karpe T, Aleem MA, Prameela J. Effect of proteolytic enzyme bromelain on pain and swelling after removal of third molars. J Int Soc Prev Community Dent. 2016;6:S197–S204. doi: 10.4103/2231-0762.197192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fitzhugh DJ, Shan S, Dewhirst MW, Hale LP. Bromelain treatment decreases neutrophil migration to sites of inflammation. Clin Immunol. 2008;128:66–74. doi: 10.1016/j.clim.2008.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bhoobalakrishnan MS, Rattan V, Rai S, Jolly SS, Malhotra S. Comparison of efficacy and safety of bromelain with diclofenac sodium in the management of postoperative pain and swelling following mandibular third molar surgery. Adv Oral Maxillofac Surg. 2021;3:100112 [Google Scholar]