Abstract
Introduction
Despite extensive evidence of its benefits and recommendation by guidelines, cardiac rehabilitation (CR) remains highly underused with only 20%–50% of eligible patients participating. We aim to implement and evaluate the Country Heart Attack Prevention (CHAP) model of care to improve CR attendance and completion for rural and remote participants.
Methods and analysis
CHAP will apply the model for large-scale knowledge translation to develop and implement a model of care to CR in rural Australia. Partnering with patients, clinicians and health service managers, we will codevelop new approaches and refine/expand existing ones to address known barriers to CR attendance. CHAP will codesign a web-based CR programme with patients expanding their choices to CR attendance. To increase referral rates, CHAP will promote endorsement of CR among clinicians and develop an electronic system that automatises referrals of in-hospital eligible patients to CR. A business model that includes reimbursement of CR delivered in primary care by Medicare will enable sustainable access to CR. To promote CR quality improvement, professional development interventions and an accreditation programme of CR services and programmes will be developed. To evaluate 12-month CR attendance/completion (primary outcome), clinical and cost-effectiveness (secondary outcomes) between patients exposed (n=1223) and not exposed (n=3669) to CHAP, we will apply a multidesign approach that encompasses a prospective cohort study, a pre-post study and a comprehensive economic evaluation.
Ethics and dissemination
This study was approved by the Southern Adelaide Clinical Human Research Ethics Committee (HREC/20/SAC/78) and by the Department for Health and Wellbeing Human Research Ethics Committee (2021/HRE00270), which approved a waiver of informed consent. Findings and dissemination to patients and clinicians will be through a public website, online educational sessions and scientific publications. Deidentified data will be available from the corresponding author on reasonable request.
Trial registration number
ACTRN12621000222842.
Keywords: preventive medicine, cardiology, telemedicine
Strengths and limitations of this study.
The study will apply the model for large-scale knowledge translation to implement evidence-based cardiac rehabilitation into practice.
Codesign of telehealth-based cardiac rehabilitation with patients and evaluation of patient-reported outcomes and experiences demonstrate the patient-centred approach of Country Heart Attack Prevention (CHAP).
Data linkage between clinical and administrative databases will allow an accurate evaluation of the model’s clinical effectiveness.
Analysis of the cost efficiencies to health services, and the cost-benefit to rural patients and families will be performed.
The CHAP model of care is not culturally tailored to the needs of Aboriginal and Torres Strait Islander peoples living in rural South Australia.
Introduction
Cardiovascular diseases (CVD) are the number one cause of death globally, taking an estimated 17.9 million lives each year. CVDs are a group of disorders of the heart and blood vessels and include coronary heart disease, cerebrovascular disease, rheumatic heart disease and other conditions such as heart failure and arrhythmias.1 The rate of CVD secondary events globally is estimated to be between 26% and 50%.1 CVD kills one Australian every 12 min and is a major cause of mortality accounting for 43 249 deaths in 2019.2
Of particular concern are those Australians living in rural and remote areas, who have 90% higher rates of CVD-related hospitalisation and 60% higher rates of CVD death than those in metropolitan areas.3 The further a person lives from a metropolitan centre, the greater their risk of hospitalisation and death from CVD.4–6 In South Australia, a southern, central state of Australia with 1.76 million inhabitants, approximately 23% of the population live in regional areas (ie, towns, small cities and areas that lie beyond the capital city of Adelaide).7 Alarmingly, the prevalence of risk factors for heart disease in South Australia is higher than the national average8 and the age-standardised rate for hospital admissions related to heart disease was the third worst among Australian states in 2017 (120 per 10 000 persons) with some regional areas having mortality rates for coronary heart disease 18% higher than the state average.5
Cardiac rehabilitation evidence translation gap
Cardiac rehabilitation (CR) is the sum of interventions required to ensure physical, psychological and social recovery for patients after an acute cardiovascular event.9 Despite high levels of evidence supporting benefit and cost-effectiveness of risk factor modification to reduce secondary CVD events through CR,10 Australian and international statistics for the past 20 years report that only 20%–50% of eligible patients participate.10–12
Historically, CR has been delivered face to face to groups in acute hospitals or community centres.13 Alternative methods for provision of CR are effective but few have been implemented into practice.13–15 Therefore, we would argue that the evidence for strategies to modify risk factors through CR is strong but the evidence for the mode of delivery has become outdated.14 16 Research on the reasons for non-attendance has cited cost and access issues, limited models of care to accommodate patients who wish to return to work and a lack of person-centredness in service design and delivery.17 This particularly affects attendance of women, people with disabilities, rural and remote dwellers and culturally and linguistically diverse populations.17 Moreover, the COVID-19 public health emergency has amplified the barriers on accessing centre-based CR.15
Preliminary data and background of the Country Heart Attack Prevention Project
Preliminary data and background leading to the Country Heart Attack Prevention (CHAP) Project have been developed over a decade (2009–2018) through a long-standing partnership among local researchers, clinicians and health service managers. Through this partnership, our team have summarised the evidence around CR, identified local barriers and implemented and measured performance of a series of initiatives to improve CR referral, attendance and completion.4 9 12 14 17–21 Limited referrals to CR, lack of patient-centred approaches and individualised choices, lack of sustainable lifelong commitment to CR supported by primary care and heterogeneous CR quality have been identified as main barriers.17 21
Limited referrals to CR
A range of factors influence clinicians’ view about CR. Our preliminary work showed that clinicians lacking cardiac qualifications may have limited knowledge and awareness of CR and its benefits.21 Low agreement among clinicians on patients who are more likely to benefit from CR, clinicians’ personal lifestyle and health belief and the knowledge on the availability and quality of local CR programmes also impact on referral to CR.21 The lack of standard administrative processes of referral and of reliable systems to support clinicians with these processes has also been identified as reason for limited referrals to CR.17 21 To address this, the South Australian Department of Health’s (SA Health) Integrated Cardiovascular Clinical Network (iCCnet SA), which is a state-wide provider of clinical network support and practice of evidence-based cardiac care and continuous quality improvement servicing regional, rural and remote areas of South Australia, implemented the Country Access to Cardiac Health (CATCH) programme.18 19 This programme includes a central referral process that receives CR referrals for patients discharged from public and private hospitals and directs them to a face-to-face or telephone-based CR service depending on patient’s preferences and proximity to a CR community centre.19 In a quasiexperimental pre-post analysis conducted in 2015, regional and rural locations receiving the telephone-based CR programme showed an increase in referral rates (97.3%), a reduction in all-cause readmissions (3.4% vs 1.8%, p<0.001) and reduced length of stay for those patients readmitted (3.5 vs 2.7 days, p=0.001) after the programme implementation.19
Lack of patient-centred approaches and individualised choices
The CATCH programme also implemented a telephone-based CR service that is offered to patients living at least 50 km away from a CR service.19 The CATCH telephone programme is aligned with findings from a systematic review conducted by members of our team that showed that individualised telehealth or home-based CR programmes were effective alternative models that are comparable to the traditional hospital and community-based programmes in terms of reducing CVD risk factors.14 19 These telehealth options are particularly important to Australians living in rural and remote areas where distances and lower availability of services amplify limitations to CR access.4 6 17 20
Lack of sustainable lifelong commitment to CR supported by primary care
Access to a cardiologist is a known enabler of CR uptake.22 To address the barrier of the shortage of specialists in rural and remote areas throughout Australia,23 iCCnet has developed a model of care (GP Hybrid network) that enables CR delivery through a strong collaboration among general practitioners (GPs), practice nurses working in rural and remote areas in South Australia and CR nurses working in the CATCH telephone-based service.24 This service has been evaluated and has shown high attendance and completion rates, and enhanced clinical outcomes for patients within 12 months, such as improved lipids and diabetes control.24 All these measures of performance of the GP Hybrid network were enabled by the establishment of the CATCH database by iCCnet. This CR data set with standardised electronic data collection serves to audit and feedback purposes to all public face-to-face services and the telephone-based service in the state of South Australia.18 25
Heterogeneous CR quality
Quality improvement of CR programmes is associated with higher rates of attendance and completion.25 The Australian Cardiovascular Health and Rehabilitation Association (ACRA) recommends five core components for quality delivery and outcomes of CR services—access to services, assessment and monitoring, recovery and longer term maintenance, lifestyle or behavioural changes, medication adherence, evaluation and quality improvement.9 National quality indicators for CR were established by ACRA and the National Heart Foundation of Australia in 2019.9 However, currently, there is no standardisation of the CR services and programmes with only a few meeting minimum duration standards.26 Therefore, there is a large variation across services in terms of the content, measures, the number of sessions and length of the CR programme.
Aims and objectives
The CHAP Project aims to develop and implement evidence-based approaches to address modifiable barriers to accessing and successfully completing CR in rural and remote areas of South Australia.
We hypothesise (H1) that compared with patients not exposed to the CHAP model of care (ie, receiving standard care), patients exposed to CHAP will have higher rates of attendance and completion of CR, higher rates of risk factor modification and higher rates of adherence to evidence-based pharmacotherapy; and experience lower rates of morbidity and mortality at 30 days and 12 months and that the model will demonstrate cost-effectiveness for both services and patients.
Specific objectives of the CHAP Project are to:
Adopt a patient-centred approach by codesigning the CHAP model of care with patients’ family and clinicians and evaluate the impact on CR attendance and completion.
Evaluate the clinical effectiveness of the CHAP model.
Evaluate the cost-effectiveness of the CHAP model.
Methods and analysis
Research design
The CHAP Project is implementing a model of care within the real world. To understand and observe the various implementation activities and evaluate their different effects within this complex context of non-linear and changing processes and elements, we will apply multiple research methods.27
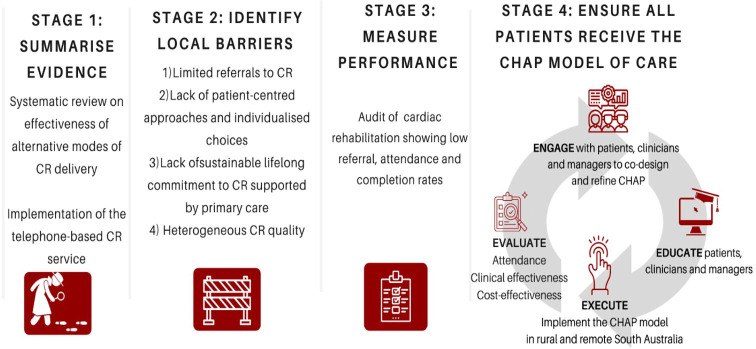
The model for large-scale knowledge translation, which is particularly useful for large-scale collaborative projects involving researchers and clinical staff, is a generalisable translation model that will be used to facilitate implementation of evidence-based interventions into practice.28 The first three of the four stages of the model for large-scale knowledge translation (1. Summarise the evidence; 2. Identify local barriers, and 3. Measure performance) have been completed in the decade (2009–2018) of preliminary work by researchers in our team and included (1) systematic review on the effectiveness of alternative modes of delivery of CR14; (2) identification of local barriers to CR attendance17; (3) the establishment of a central referral system (CATCH central referral system) and telephone-based programme (CATCH telephone programme)18 19; and (4) clinical database (CATCH database).18
The fourth stage of the model is the final and most complex one—Ensure all patients receive the intervention. The model uses a ‘four Es’ approach to improve reliability: engage, educate, execute and evaluate28 (figure 1). This is the stage that will be developed in the CHAP Project. The CHAP model of care must consider the context, local culture and resources of each hospital and health networks in the current system.
Figure 1.
Using the model for large-scale knowledge translation to develop Country Heart Attack Prevention (CHAP). CR, cardiac rehabilitation.
To complete this stage, the team will work closely with health networks and CR services addressing barriers to implementing the CHAP model of care in rural and remote areas of the state (figure 2).
Figure 2.
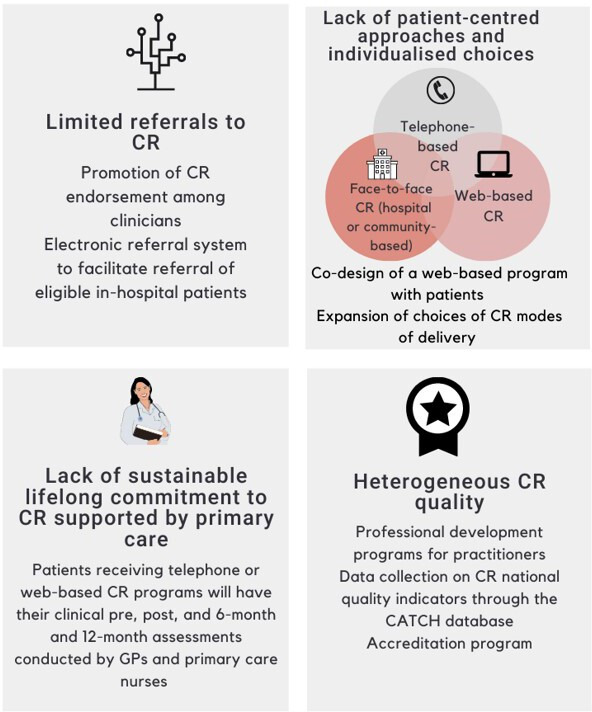
Addressing the barriers through the Country Heart Attack Prevention (CHAP) model of care (exposure) according to the fourth stage of the model for large-scale knowledge translation (‘Engage, Educate, Execute, Evaluate’). CATCH, Country Access to Cardiac Health; CR, cardiac rehabilitation; GP, general practitioner.
The evaluation of the CHAP model of care will comprise both clinical (objective 2) and cost-effectiveness (objective 3) assessments, and will involve a multimethod approach:
1. A prospective cohort study comparing attendance and clinical outcomes of patients exposed and non-exposed to CHAP—the cohort of patients eligible to CR will be followed up for 12 months from CHAP implementation and outcomes will be compared between those exposed to the CHAP model and those not exposed to the model of care. Attendance will be defined as attendance to ≥1 CR programme session. Completion was defined as attendance to at least 75% of the CR sessions.29 The exposed and non-exposed groups will be age, sex and diagnostic-related group (DRG) matched controls in a 1:3 ratio.30
2. A pre-post study design comparing outcomes before (1 January 2016 to 30 June 2021) and after CHAP implementation (1 July 2021 to 30 June 2023). A comprehensive economic analysis will be performed to evaluate the cost efficiencies to health services, and the cost-benefit to rural and remote patients and families.
Setting
The CHAP model of care will be implemented within the six local health networks in regional, rural and remote South Australia through iCCnet.18 The iCCnet is part of the Rural Support Service which is a business unit within the South Australian Health Service that provides flexible, responsive and innovative services to support the six regional local health networks. Regional health services are delivered to a population of 497 003 people with the following age group distribution: 0–4 years (5.82%), 5–18 years (17.52%), 19–64 years (56.68%) and 65 years and over (19.98%). There are 23 CR services and the CATCH telephone service.31
Participants
Eligible participants will be defined according to current international guideline criteria32 by DRGs based on the International Classification of Diseases-10 codes, and the current guidelines for those who are eligible for referral to CR include: acute myocardial infarction (I21, I21.0, I21.1, I21.2, I21.3, I21.4, I21.9), hypertensive heart disease (I11.0, I11.9, I13, I13.0, I13.2, I13.9), ischaemic heart disease (I20–I25), arrhythmias (I48, I48.0, I48.1, I48.2, I48.3, I48.4, I48.9, I49.9) and/or heart failure (I50, I50.0, I50.1, I50.9).33 Eligibility will also be defined based on DRG procedure codes for coronary artery surgery, percutaneous coronary intervention and ventricular assist device.34
All adult (≥18 years) South Australians, including Aboriginal and Torres Strait Islander peoples, discharged from hospital with a diagnosis that meets the eligibility criteria to CR (acute myocardial infarction, hypertensive heart disease, ischaemic heart disease, arrhythmias, and/or heart failure, coronary artery surgery, percutaneous coronary intervention and ventricular assist device)33 and living within the six local health networks in regional, rural and remote areas will be exposed to the CHAP model of care. The comparison group (non-exposed to CHAP) will comprise age, sex and DRG matched controls not living in these regional, rural and remote areas.
With approximately 60% of the Aboriginal and Torres Strait Islander populations of South Australia living outside major cities in regional and remote areas,35 it is likely that a number of these individuals will be exposed to the CHAP model of care. However, we acknowledge we are implementing standard guidelines that may not suit these groups. A future project to culturally adapt the CHAP model of care using appropriate Aboriginal and Torres Strait Islander translation methodology is warranted. There will be no stratification by Aboriginal/indigenous status in this study.
Exposure: the CHAP model of care
Exposure to the CHAP model of care will be defined as an individual, professional or service receiving at least one of the approaches proposed to address four different local barriers to CR attendance and completion that were previously identified by this team (figure 2).
Limited number of referrals
We will address the limited number of referrals by promoting CR endorsement among clinicians and providing them with an electronic system that facilitates referrals.
To increase CR endorsement, we will codesign education resources with clinicians including evidence-based pharmacotherapy resources, and a variety of paper-based, videos and web-based education resources. One example of this is the ‘Recommend video wall’ which was produced by the CHAP Project through collection of testimonies from patients who undertook CR and multidisciplinary teams working in hospitals and CR services who recommend CR.36 This video wall has been displayed in events with professionals and patients and websites of organisations such as ACRA and Heart Foundation as a tool to promote endorsement to CR. This will ensure that health professionals and CR patients’ needs are addressed regardless of technology literacy levels.37
We will expand the capabilities of referral introduced by the CATCH central referral system by developing an automatic electronic referral system that will streamline in-hospital referrals. A central portal for patient discharge reports will provide contact information on patients who have been discharged with applicable codes. Currently, these reports are run from several different databases and have the potential to miss patients living in rural and remote areas. We will first have automatic reports generated from information taken from the health department (SAH DataMart). This will all run on the back end of the Integrated Point of Care Clinical System (iPOCCS)38 in which an Excel document is generated daily, reporting on the previous 24 hours of discharged patients. A Uniform Resource Locator will be sent to designated users allowing them to log on to iPOCCS and download the file.
Lack of patient-centred approaches and individualised choices
Face-to-face and telephone services are well established as modes of CR delivery in rural South Australian regions.19 Despite variability in duration and content, these CR programmes are generally based on the National Heart Foundation of Australia32 and ACRA guidelines9 comprising 10 modules (initial assessment and goal setting, heart education and self-management, exercise training and physical activity, healthy eating and weight management, tobacco cessation and alcohol reduction, medication education and review, managing medical risk factors, psychosocial well-being, activities of daily living, reassessment and completion) which are delivered over 6–12 weeks depending on patients’ needs and decisions from services.
To expand the choices of CR modes of delivery, CHAP will codesign with patients living in rural areas a web-based programme accessed through a personal log-in. The user experience (UX) design,39 an established codesign framework, will guide the engagement with end users through workshops and the codesign process from concept design to completion. A variety of UX design methods will be used interchangeably to plan, execute and evaluate the workshops. These include cultural probes, heuristic evaluation, brainstorming, focus groups and concept testing.39 40 The content of the portal will be based on the 10 National Heart Foundation of Australia modules.9 32 Individualised programmes will be tailored according to patients’ needs. The anticipated duration of each web module completion is 30 min/week.40 Those in the web delivery mode will be required to read short texts, watch short videos (about five per module), set personal goals and self-report their dietary, physical activity, smoking and alcohol ingestion habits weekly through responding to online questionnaires on the website. The web portal will have a function to collect physical activity data from wearables and smartphone apps patients may use. Patients will be able to interact with a CR nurse through a message system embedded in the web portal. They will be asked to complete four Heart Health Risk Factor assessments (baseline, 8–12 weeks after starting CR, 6 and 12 months after completing CR). These assessments will comprise clinical and patient-reported outcome measures (PROMs) assessment using validated questionnaires that assess lifestyle habits, exercise capacity, quality of life and mental health (table 1). Six-month and 12-month follow-up will be performed by the patient’s primary care physician.
Table 1.
Primary and secondary outcomes, measurements and sources of data
| Primary outcomes | Measures/instruments |
| Attendance Completion |
Number of patients participating in at least one session Number of patients participating in at least 75% of all sessions |
| Attendance Completion |
Number of patients attending ≥1 session among the eligible ones/year Number of patients completing ≥75% of all sessions among the eligible ones/year |
| Secondary outcomes | |
| CR referral rates | Number of patients referred to CR/eligible to CR/year |
| 30-day and 12-month hospital CVD-related hospital readmission | Assessed through the linkage between the South Australian CR database and SA Health administrative databases. Each cardiac admission will be counted as a single separation, with admissions involving transfer(s) merged as one. Readmission within 24 hours will not be counted as a new event. |
| 30-day and 12-month CVD-related mortality | Assessed through the linkage between the South Australian CR database and SA Health administrative databases. CVD |
| 30-day and 12-month emergency department (ED) presentation | Assessed through the linkage between the South Australian CR database and SA Health administrative databases. Each ED presentation resulting in a separation will be considered a single hospitalisation. New ED presentation within 24 hours will not be counted as a new event. |
| Cardiovascular risk factor modification | |
| Smoking | Self-reported number of cigarettes |
| Alcohol intake | Self-reported grams of alcohol consumed/week |
| Body mass index | Self-reported weight and height |
| Nutrition | Commonwealth Scientific and Industrial Research OrganisationHealthy Diet Score58 |
| Diabetes control | HbA1c |
| Exercise, physical activity and functional capacity | 6 min walk test59
International Physical Activity Questionnaire-Short Form60 Specific Activity Questionnaire61 |
| Medication adherence | Adherence in Chronic Diseases Scale62 |
| Patient-reported outcome measures (PROMs) and patient-reported experience measures (PREMs) | |
| Anxiety | Cardiac Anxiety Questionnaire63 |
| Depression | PHQ-2, PHQ-964 |
| Quality of life* | EQ-5D-5L52
Kansas City Cardiomyopathy Questionnaire-1265 (for patients with heart failure) |
| Health literacy | Brief Health Literacy Screening Tool66 |
| Patient satisfaction | Self-reported satisfaction |
CR, cardiac rehabilitation; CVD, cardiovascular disease; EQ-5D-5L, European Quality of Life-5 Dimensions-5 Levels; PHQ-2, 2-question Patient Health Questionnaire; PHQ-9, 9-question Patient Health Questionnaire; SA Health, South Australian Department of Health.
Patient and public involvement
The CHAP model of care is underpinned by a patient-centred approach. Patient-centred care or person-centred care is based on principles that those receiving healthcare must be treated with dignity and respect and be involved in all decisions about their health.41 This approach is applied in this study through involvement of patients in the codesign of the CR web programme40 and development of a model that allows patients to choose among different CR modes of delivery (face to face, telephone or web based, or combinations of these modes—figure 2).19 41 42 We will particularly promote the participation of older CR patients and people from cultural and linguistically diverse backgrounds to ensure that groups at increased risk of low technology and health literacy are involved in the codesigning of the web-based CR programme. We anticipate this will increase patient adherence and engagement with the web-based CR programme.42
Updating the modalities of telehealth that are currently available will allow for greater flexibility of CR delivery which can improve access for patients in need. Importantly, this also provides an appropriate response to the COVID-19 pandemic when traditional CR service delivery is disrupted.15 43 44
Lack of sustainable lifelong commitment to CR supported by primary care
CHAP Project will build on the GP Hybrid model of CR delivery by creating a business model which allows primary care to support CR delivery and assessment of CR results (risk factor change) of patients undertaking telephone and web-based CR. The model will comprise a ‘Heart Health Risk Factor’ preassessment at the beginning of the programme (ie, 1–2 weeks after discharge) which will last 75 min (60 min with a practice nurse and 15 min with the GP). Reassessments will occur at 8–12 weeks after the beginning of the programme, and 6 and 12 months after completion of the CR programme. These will comprise 45–60 min consultations with the practice nurse and 15 min consultations with the GP. This has potential to enable long-term support for heart health from GPs.
Heterogeneous CR quality
The CHAP Project will seek adherence to the quality indicators through multiple online and offline professional development programmes targeting the practitioners, development of an accreditation programme and refinement of data collection tools on the national CR quality indicators. In particular, the project will try to integrate objective patient-generated physical activity tracking data to the CATCH CR database to enable objective monitoring of physical activity during CR and personalised feedback.
Outcomes
Primary outcomes—CR attendance rate defined as the number of patients commencing CR (≥1 session) among those eligible to CR. Completion rates defined as the number of patients attending ≥ 75% of CR sessions.
Secondary outcomes—will compare risk factor modification, clinical outcomes, PROMs and patient-reported experience measures of the CHAP and non-CHAP groups. Measurements, tools and questionnaires and data sources for the secondary outcomes are presented in table 1. The selection of validated tools and questionnaires followed extensive consultations with CR clinicians about their preferences and implications of the tools to documentation time and costs to the services.
Data sources
The South Australian CR clinical database (the CATCH database) collects data uniformly across metropolitan, rural and remote areas using a standardised electronic entry process, including electronic data capture, of patients moving through public CR services from rural and remote to a metropolitan hospital or vice versa.19 This database will be linked to the SA Health administrative database, enabling follow-up and assessment of hospital readmissions, emergency department presentations and mortality.45 This data linkage approach is similar to the one used to audit the CR services in South Australia from 2013 to 2015.12
Bias
To avoid information bias (ie, systematic differences in the completeness or the accuracy of data leading to differential misclassification of individuals regarding exposures or outcomes), we are upskilling clinicians to input data onto the CR databases as part of continuous quality improvement processes. The goal is to fill the gap of scarcity of data on CR data in Australia46 and achieve universal, uniform data entry in South Australian CR programmes.
Sample size
The average state-wide attendance of CR from 2013 to 2015 was 28.3% (pre-CHAP estimate).10 Based on a 4% improvement in attendance (ie, to 32.3%) as reported by the British Association for Cardiovascular Prevention and Rehabilitation audit,47 a total sample size of 1223 (CHAP) and 3669 (usual care, 1:3 matching) will produce a two-sided 95% CI for the difference in population proportions with a width that is equal to 0.06. Allowing for a 20% dropout, we will need to observe 1529 patients (765 per year) in the group exposed to CHAP that will be matched to 4587 patients in the group non-exposed to CHAP (usual care) from the CATCH database. From 2015 to 2019, approximately 2000 patients were entered into the CATCH CR database per year making this study highly feasible.
Data analysis
To evaluate the effectiveness of CHAP (objective 2)
Unpaired t-tests, χ2 tests and Mann-Whitney U tests for non-normal data will be used for comparisons for the pre-post analysis of the CHAP model components. Statistical significance will be inferred if two-tailed tests estimated p<0.05. Rates of referral, attendance and completion of CR per year; modification of risk factors; and adherence to evidence-based pharmacotherapy morbidity and mortality at 30 days and 12 months will be compared between CHAP and non-CHAP attendees and presented as ORs and 95% CIs. Matching will be conducted by grouping all cases and controls into relevant groupings of age, sex and DRG and analysed using the Mantel-Haenszel methods.48
Cox regression models adjusted for clinical and social factors (age, sex, the Index of Relative Socio-economic Advantage and Disadvantage from the Australian Bureau of Statistics’ Socio-Economic Indexes for Areas score,49 Accessibility and Remoteness Index of Australia,50 primary cardiac diagnosis, Charlson Index,51 in-hospital length of stay, prior heart failure, coronary disease, atrial fibrillation, revascularisation, malignancy) will be performed to understand the association between exposure to the CHAP model and attendance. For clinical outcomes (30-day and 12-month hospital CVD-related hospital readmission, 30-day and 12-month CVD-related mortality), the model will also be adjusted for CR attendance.
To evaluate the cost-effectiveness of CHAP (objective 3)
The economic evaluation of the CHAP model including the business model (explore the item numbers that can be used to cover GP-based CR and items that can be used to employ and train practice nurses to assist with assessment, monitoring, collection of outcome data and triage to maximise GP consultation time) that involves primary care in CR delivery will comprise: (1) the cost efficiencies to health services, and (2) cost-benefit to rural and remote patients and families.
The cost efficiencies to the health services
All CVD hospitalisations during the follow-up period will be included and assigned a cost, based on the diagnosis-related group category reference and length of stay. Costs of providing CR will be taken from a health system perspective and calculated over 1 year; this includes staffing, consumables, overheads and capital expenses. Quality-of-life measures will be estimated at baseline, and 6 and 12 months after CR completion, using the standard European Quality of Life-5 Dimensions-5 Levels.52 The utility is defined by the Department of Health and Ageing as a numerical value assigned by an individual to a preference for, or desirability of, a specific level of health status or a specific health outcome. Data on utilities and survival can be combined to calculate quality-adjusted life-year (QALY) by exposed and non-exposed groups using the quality-adjusted survival analysis method.53–55 Incremental cost per QALY saved will be calculated as an incremental (rehabilitation vs usual care) cost per patient divided by the incremental QALY per patient.56
Cost-benefit to rural and remote patients and families
Using an economic survey developed by the Western Australian Department of Health,57 we will quantify the economic impact of the CHAP model based on information at baseline including patient demographics such as household structure, employment status and the distances travelled to access services; the nature of the consultation, waiting time, whether the patient required time off work (and if so, how much) and the mode of transport used to travel to the hospital. The survey will include accompanying persons, and if the person required any time off work to do so. Finally, the survey will explore the patient’s treatment options; for example, did they consider having an appointment in the city essential to their care? These data will be modelled to compare two scenarios for face-to-face CR: (1) if the patient travelled to the city to attend CR, or (2) if the patient travelled to the nearest rural CR programme if this is within 60 min drive (approximately 100 km). All results will be presented unadjusted for multiple comparisons and all analyses will be done on an intention-to-treat basis. 95% CIs for the difference in QALYs will be calculated with bootstrapping.54
Time frame of the project
The original time frame comprised a 3-year project from 1 July 2019 to 30 June 2022. Due to the impact of the COVID-19 pandemic on the project implementation, the project had a 12-month extension and will now be complete by 30 June 2023. Years 1–2 will include project staff employment and training, development of resources, education materials, study protocols, additional data sets and ethics approval. Recruitment will be conducted over years 2–3 and follow-up over years 3–4.
Ethics and dissemination
Ethics approval and consent to participate
This study was approved by the Southern Adelaide Clinical Human Research Ethics Committee on 28 April 2020 (HREC/20/SAC/78). The data linkage between the South Australian CR clinical database and the Department of Health administrative databases was approved by the Department for Health and Wellbeing Human Research Ethics Committee on 26 August 2021 (2021/HRE00270). All consecutive patients who are eligible for CR according to the recommended DRG codes and referred for CR will have consent waiver to have their data used for this research.
Dissemination
Findings will be disseminated to patients and health professionals using various means and media: a public website (https://chapproject.com.au),36 online educational sessions with patients and health professionals working in CR, monthly newsletters sent to participants via email, social media (Twitter @CHAPproject, LinkedIn CHAP Project and Facebook) and scientific publications and conference presentations.
Supplementary Material
Footnotes
Twitter: @rosannatavella
Collaborators: Country Heart Attack Prevention (CHAP) Project.
Contributors: The study was conceived and designed by RAC, SJN, ABr, DPC, JB, AM, CM, VLV, JMH, PT, BK, CZ, IJP, RTa, RTi and WK. The first draft of the paper was written by AB with significant input from RAC before receiving input from the remaining authors: CA, KG, KN, HD, SC, MAPdP, IL, VP, KW, HM, AK, LG, ML and CG. All authors read and approved the final manuscript.
Funding: This study is supported by a peer-reviewed National Health and Medical Research Council (NHMRC Partnership Grant GNT1169893) between NHMRC and the following partners: Flinders University, the Integrated Cardiac Clinical Network (iCCnet SA), National Heart Foundation of Australia, Exercise and Sports Science Australia (ESSA), Australian Cardiac Rehabilitation Association (ACRA), Country Health SA, Cardiac Society of Australia and New Zealand (CSANZ), Flinders Foundation, Royal Australian College of General Practitioners (RACGP), AstraZeneca, Novartis, Health Translation SA, and the Enterprise Data and Information Department of Health and Wellbeing, SA Health. VLV is funded by the Australian Government Department of Health through the Rural Health Multidisciplinary Training (RHMT) programme. JMH is supported by a Future Leader Fellowship provided by the National Heart Foundation of Australia. CM is funded by a Medical Research Future Fund Investigator Grant (1193862).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. World Health Organization . Cardiovascular diseases - WHO, 2021. Available: https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1 [Accessed 19/05/2021].
- 2. Australian Bureau of Statistics . Causes of death ABS cat no 33030, 2020. Available: https://www.abs.gov.au/statistics/health/causes-death/causes-death-australia/latest-release
- 3. Australian Institute of Health & Welfare (AIHW) . Heart attack, stroke and cardiac arrest symptoms, 2018. Available: https://www.heart.org/en/about-us/heart-attack-and-stroke-symptoms
- 4. Clark RA, Coffee N, Turner D, et al. Application of geographic modeling techniques to quantify spatial access to health services before and after an acute cardiac event: the cardiac accessibility and remoteness index for Australia (ARIA) project. Circulation 2012;125:2006–14. 10.1161/CIRCULATIONAHA.111.083394 [DOI] [PubMed] [Google Scholar]
- 5. Australia NHFo . Interactive Australian heart maps. compare heart health indicators across Australia, 2021. Available: https://www.heartfoundation.org.au/health-professional-tools/interactive-heart-map-australia [Accessed 16 Jun 2021].
- 6. Tideman P, Taylor AW, Janus E, et al. A comparison of Australian rural and metropolitan cardiovascular risk and mortality: the greater green triangle and North West Adelaide population surveys. BMJ Open 2013;3:e003203. 10.1136/bmjopen-2013-003203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Statistics ABo . Census quick STATs. South Australia 2016, 20162021. Available: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/4?opendocument [Accessed 16/06/2021].
- 8. National Heart Foundation of Australia . A time for action in South Australia, 2018. Available: https://www.heartfoundation.org.au/getmedia/2812a674-21f4-4889-a672-b7654e6b5015/AtimeforAction2018_20March_FINAL.pdf
- 9. Woodruffe S, Neubeck L, Clark RA, et al. Australian cardiovascular health and rehabilitation association (acrA) core components of cardiovascular disease secondary prevention and cardiac rehabilitation 2014. Heart Lung Circ 2015;24:430–41. 10.1016/j.hlc.2014.12.008 [DOI] [PubMed] [Google Scholar]
- 10. Anderson L, Thompson DR, Oldridge N. Exercise‐based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2016;2016:CD001800. 10.1002/14651858.CD001800.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Redfern J, Hyun K, Chew DP, et al. Prescription of secondary prevention medications, lifestyle advice, and referral to rehabilitation among acute coronary syndrome inpatients: results from a large prospective audit in Australia and New Zealand. Heart 2014;100:1281–8. 10.1136/heartjnl-2013-305296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Astley CM, Chew DP, Keech W, et al. The impact of cardiac rehabilitation and secondary prevention programs on 12-month clinical outcomes: a linked data analysis. Heart Lung Circ 2020;29:475–82. 10.1016/j.hlc.2019.03.015 [DOI] [PubMed] [Google Scholar]
- 13. Jelinek MV, Thompson DR, Ski C, et al. 40 years of cardiac rehabilitation and secondary prevention in post-cardiac ischaemic patients. are we still in the wilderness? Int J Cardiol 2015;179:153–9. 10.1016/j.ijcard.2014.10.154 [DOI] [PubMed] [Google Scholar]
- 14. Clark RA, Conway A, Poulsen V, et al. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol 2015;22:35–74. 10.1177/2047487313501093 [DOI] [PubMed] [Google Scholar]
- 15. Dalal HM, Doherty P, McDonagh ST, et al. Virtual and in-person cardiac rehabilitation. BMJ 2021;373:n1270. 10.1136/bmj.n1270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. West RR, Jones DA, Henderson AH. Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart 2012;98:637–44. 10.1136/heartjnl-2011-300302 [DOI] [PubMed] [Google Scholar]
- 17. Astley CM, Neubeck L, Gallagher R, et al. Cardiac rehabilitation: unraveling the complexity of referral and current models of delivery. J Cardiovasc Nurs 2017;32:236–43. 10.1097/JCN.0000000000000332 [DOI] [PubMed] [Google Scholar]
- 18. Tideman PA, Tirimacco R, Senior DP, et al. Impact of a regionalised clinical cardiac support network on mortality among rural patients with myocardial infarction. Med J Aust 2014;200:157–60. 10.5694/mja13.10645 [DOI] [PubMed] [Google Scholar]
- 19. Tideman P, Tirimacco R, Berry N, et al. Country access to cardiac health (catch) program: improving rehospitalisation rates and length of stay for cardiac rehabilitation using innovative telehealth delivery. Heart, Lung and Circulation 2015;24:S453. 10.1016/j.hlc.2015.06.790 [DOI] [Google Scholar]
- 20. Clark RA, Wilkinson D, Coffee N, et al. Mapping services to support a patient’s journey through evidence-based care pathways after a cardiac event. Heart, Lung and Circulation 2009;18:S266. 10.1016/j.hlc.2009.05.656 [DOI] [Google Scholar]
- 21. Gallagher R, Neubeck L, Du H, et al. Facilitating or getting in the way? the effect of clinicians' knowledge, values and beliefs on referral and participation. Eur J Prev Cardiol 2016;23:1141–50. 10.1177/2047487316630085 [DOI] [PubMed] [Google Scholar]
- 22. Ghisi GLM, Polyzotis P, Oh P, et al. Physician factors affecting cardiac rehabilitation referral and patient enrollment: a systematic review. Clin Cardiol 2013;36:323–35. 10.1002/clc.22126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Summit to address rural medical specialist shortage: Royal Australian College of general practitioners 2018, 2021. Available: https://www1.racgp.org.au/newsgp/professional/summit-to-address-rural-medical-specialist-shortag [Accessed 18 Jan 2021].
- 24. Clark C, Tirimacco R, Morfidis N. Delivery of outpatient cardiac rehabilitation using a GP Hybrid/Telephone program model. National rural health alliance. Tasmania: Rural Health Org, 2019. [Google Scholar]
- 25. Pack QR, Johnson LL, Barr LM, et al. Improving cardiac rehabilitation attendance and completion through quality improvement activities and a motivational program. J Cardiopulm Rehabil Prev 2013;33:153–9. 10.1097/HCR.0b013e31828db386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gallagher R, Thomas E, Astley C, et al. Cardiac rehabilitation quality in Australia: proposed National Indicators for Field-Testing. Heart, Lung and Circulation 2020;29:1273–7. 10.1016/j.hlc.2020.02.014 [DOI] [PubMed] [Google Scholar]
- 27. Peters DH, Adam T, Alonge O, et al. Implementation research: what it is and how to do it. BMJ 2013;347:f6753. 10.1136/bmj.f6753 [DOI] [PubMed] [Google Scholar]
- 28. Pronovost PJ, Berenholtz SM, Needham DM. Translating evidence into practice: a model for large scale knowledge translation. BMJ 2008;337:a1714. 10.1136/bmj.a1714 [DOI] [PubMed] [Google Scholar]
- 29. Abreu A, Frederix I, Dendale P. Standardization and quality improvement of secondary prevention through cardiovascular rehabilitation programmes in Europe: the Avenue towards EAPC accreditation programme: a position statement of the secondary prevention and rehabilitation section of the European association of preventive cardiology (EAPC). Eur J Prev Cardiol 2020;2047487320924912. 10.1177/2047487320924912 [DOI] [PubMed] [Google Scholar]
- 30. Pearce N. Analysis of matched case-control studies. BMJ 2016;352:i969. 10.1136/bmj.i969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Country SA primary health network SA health 2021, 2021. Available: https://www.countrysaphn.com.au/ [Accessed 19 May 2021].
- 32. Chew DP, Scott IA, Cullen L, et al. National heart Foundation of Australia and cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Med J Aust 2016;205:128–33. 10.5694/mja16.00368 [DOI] [PubMed] [Google Scholar]
- 33. World Health organization . International statistical classification of diseases and related health problems 10th revision, 2016. Available: https://www.who.int/classifications/icd/ICD10Volume2_en_2010.pdf
- 34. Independent Hospital Pricing Authority . International classification of diseases and related health problems, 11th revision. Australian modification (ICD-10-AM), 2019. Available: https://www.ihpa.gov.au/publications/icd-10-amachiacs-eleventh-edition
- 35. ABS . 2021 Census of Population and Housing: Reflecting Australia - Sotries form the Census, 2016. Aboriginal and Torres Strait Islander Population, 2016, 2017. Available: https://www.abs.gov.au/statistics/people/aboriginal-and-torres-strait-islander-peoples/estimates-aboriginal-and-torres-strait-islander-australians/latest-release [Accessed 16 Dec 2021].
- 36. Country heart attack prevention project 2021, 2021. Available: https://chapproject.com.au/ [Accessed 16 Dec 2021].
- 37. Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a Networked world. J Med Internet Res 2006;8:e9. 10.2196/jmir.8.2.e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Integrated point of care clinical system integrated clinical cardiovascular network (iCCnet) SA, 2021. Available: https://www.iccnetsa.org.au/ipoccs.aspx [Accessed 19 May 2021].
- 39. Will T. User experience (UX): process and methodology, 2020. Available: https://uiuxtrend.com/user-experience-ux-process/
- 40. Nesbitt K, Beleigoli A, Du H. Web-Based Cardiac Rehabilitation: A Co-Design Workshop. Telehealth Innovations in Remote Healthcare Services Delivery. Vol 277, 2021. https://ebooks.iospress.nl/volumearticle/56656 [Google Scholar]
- 41. Australia Commission on Safety and Quality in Healthcare . Patient-Centred care improving quality and safety through partnerships with patients and consumers, 2011. Available: https://www.safetyandquality.gov.au/publications-and-resources/resource-library/patient-centred-care-improving-quality-and-safety-through-partnerships-patients-and-consumers
- 42. Australia Commission on safety and quality in healthcare . Safety and quality improvement guide standard 2: partnering with consumers. Sydney, 2012. https://www.safetyandquality.gov.au/sites/default/files/migrated/Standard2_Oct_2012_WEB.pdf [Google Scholar]
- 43. Nicholls SJ, Nelson M, Astley C, et al. Optimising secondary prevention and cardiac rehabilitation for atherosclerotic cardiovascular disease during the COVID-19 pandemic: a position statement from the cardiac Society of Australia and New Zealand (CSANZ). Heart, Lung and Circulation 2020;29:e99–104. 10.1016/j.hlc.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Arnold RH, Tideman PA, Devlin GP, et al. Rural and remote cardiology during the COVID-19 pandemic: cardiac Society of Australia and New Zealand (CSANZ) consensus statement. Heart, Lung and Circulation 2020;29:e88–93. 10.1016/j.hlc.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Admitted patient care government of South Australia SA health 2021, 2021. Available: https://www.sahealth.sa.gov.au/wps/wcm/connect/f2652cc1-996c-4c17-8115-f85beebddbab/Admitted+Patient+Care+-+Data+Elements+-+Reference+Manual+2021-2022.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-f2652cc1-996c-4c17-8115-f85beebddbab-nNJGggc [Accessed 18 Jan 2021].
- 46. Driscoll A, Hinde S, Harrison A, et al. Estimating the health loss due to poor engagement with cardiac rehabilitation in Australia. Int J Cardiol 2020;317:7–12. 10.1016/j.ijcard.2020.04.088 [DOI] [PubMed] [Google Scholar]
- 47. British heart Foundation . National audit of cardiac rehabilitation (NACR) quality and outcomes report 2018, 2018. [Google Scholar]
- 48. Altman D. Practical statistics for medical research. London: Chapman and Hall, 1991. [Google Scholar]
- 49. Australian Bureau of statistics . Census of population and housing: socio-economic indexes for areas (SEIFA) 2016, 2021. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/2033.0.55.001main+features12016 [Google Scholar]
- 50. Australian Bureau of Statistics . 2018 Australian Statistical Geography Standard: Volume 5 - Remoteness Structure, 2021. https://www.abs.gov.au/ausstats/abs@.nsf/mf/1270.0.55.005 [Google Scholar]
- 51. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 52. McCaffrey N, Kaambwa B, Currow DC, et al. Health-related quality of life measured using the EQ-5D-5L: South Australian population norms. Health Qual Life Outcomes 2016;14:133. 10.1186/s12955-016-0537-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Glasziou PP, Simes RJ, Gelber RD. Quality adjusted survival analysis. Stat Med 1990;9:1259–76. 10.1002/sim.4780091106 [DOI] [PubMed] [Google Scholar]
- 54. Glasziou PP, Cole BF, Gelber RD, et al. Quality adjusted survival analysis with repeated quality of life measures. Stat Med 1998;17:1215–29. [DOI] [PubMed] [Google Scholar]
- 55. Martin AJ, Glasziou PP, Simes RJ. A cardiovascular extension of the health measurement questionnaire. J Epidemiol Community Health 1999;53:548–57. 10.1136/jech.53.9.548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sullivan SD, Mauskopf JA, Augustovski F, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 budget impact analysis good practice II Task force. Value Health 2014;17:5–14. 10.1016/j.jval.2013.08.2291 [DOI] [PubMed] [Google Scholar]
- 57. Rankin S, House A, Heath D. The real cost of accessing specialist medical services for rural and remote communities in Western Australia. 5th national rural health conference, 1999. [Google Scholar]
- 58. Hendrie GA, Rebuli MA, Golley RK. Reliability and relative validity of a diet index score for adults derived from a self-reported short food survey. Nutr Diet 2017;74:291–7. 10.1111/1747-0080.12303 [DOI] [PubMed] [Google Scholar]
- 59. Bellet RN, Adams L, Morris NR. The 6-minute walk test in outpatient cardiac rehabilitation: validity, reliability and responsiveness--a systematic review. Physiotherapy 2012;98:277–86. 10.1016/j.physio.2011.11.003 [DOI] [PubMed] [Google Scholar]
- 60. Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381–95. 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 61. Rankin SL, Briffa TG, Morton AR, et al. A specific activity questionnaire to measure the functional capacity of cardiac patients. Am J Cardiol 1996;77:1220–3. 10.1016/s0002-9149(97)89157-6 [DOI] [PubMed] [Google Scholar]
- 62. Buszko K, Obońska K, Michalski P, et al. The adherence scale in chronic diseases (ASCD). The power of knowledge: the key to successful patient — health care provider cooperation. Medical Research Journal 2016;1:37–42. 10.5603/MRJ.2016.0006 [DOI] [Google Scholar]
- 63. Eifert GH, Thompson RN, Zvolensky MJ, et al. The cardiac anxiety questionnaire: development and preliminary validity. Behav Res Ther 2000;38:1039–53. 10.1016/s0005-7967(99)00132-1 [DOI] [PubMed] [Google Scholar]
- 64. Arroll B, Goodyear-Smith F, Crengle S, et al. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med 2010;8:348–53. 10.1370/afm.1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Spertus JA, Jones PG. Development and validation of a short version of the Kansas City cardiomyopathy questionnaire. Circ Cardiovasc Qual Outcomes 2015;8:469–76. 10.1161/CIRCOUTCOMES.115.001958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Haun J, Luther S, Dodd V, et al. Measurement variation across health literacy assessments: implications for assessment selection in research and practice. J Health Commun 2012;17 Suppl 3:141–59. 10.1080/10810730.2012.712615 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.