Abstract
Objectives:
The purpose of this article is to review the technical and radiological aspects of MagSeed® localisation, to assess its accuracy based on post-localisation mammograms and excision specimen X-rays and to discuss the radiological experience of our institutions.
Methods:
Two-year data were collected retrospectively from three NHS boards from the West of Scotland. A total of 309 MagSeeds® were inserted under mammographic or ultrasonographic guidance in 300 women with unifocal, multifocal and/or bilateral breast lesions at the day of surgery or up to 30 days prior to it. Radiological review of post-localisation mammograms and intraoperative specimen X-rays as well as a review of the surgical outcomes were performed to assess the accuracy and efficacy of the method. Our experience relating to the technique’s strengths and downsides were also noted.
Results:
The MagSeeds® were inserted on average 7.2 days before surgery. The localisation technique was straight forward for the radiologists. In 99% of the cases, the MagSeed® was successfully deployed and 100% of the successfully localised lesions were excised at surgery. There was no difference in the accuracy of the localisation whether this was mammographically or ultrasonographically guided. On post-localisation mammograms, the MagSeed® was radiologically accurately positioned in 97.3% of the cases. No delayed MagSeed® migration was observed. On the specimen X-rays, the lesion was centrally positioned in 45.1%, eccentric within more than 1 mm from the margin in 35.7% and in 14.8% it was at the specimen’s margin. The re-excision rate was 18.3%.
Conclusion:
The MagSeed® is an accurate and reliable localisation method in breast conserving surgery with good surgical outcomes.
Advances in knowledge:
To our knowledge, the radiological aspects of MagSeed® localisation have not been widely described in peer-reviewed journals thus far.
Introduction
The current method of choice for the preoperative localisation of impalpable breast lesions in breast conserving surgery is imaging-guided wire placement. This method has been the gold standard for a considerable number of years and has been widely discussed in peer-reviewed papers. 1 Its disadvantages in the management of breast cancer patients such as wire transection and migration, patient distress and discomfort, interference with the surgical approach and even pneumothorax have been extensively described in the literature. 2 Furthermore, the necessity for radiological and surgical pairing at the day of operation can result in logistical issues and create problems in workflow and subsequent patient management. In order to improve the patient experience, optimise workflow, create more flexibility in overstrained surgical and radiological departments without compromising the high complete excision rates achieved by the guide wire method, several alternative localisation methods have been suggested, such as the ROLL (Radio-guided Occult Lesion Localisation) and Iodine-125 seed localization based on the use of radioisotopes as well as more recent non-radioisotope techniques. In the last 3 years, the SAVI-SCOUT®, based on infrared detection technology, the radiofrequency identification-based technology with the LOCaliserTM wire-free guidance system and the MagSeed® based on magnetic principles have been licensed for use in the UK and USA. 3–10 The latter appears to be a reliable, well-tolerated, uncomplicated and cost-effective method of localisation and its uptake by surgical departments in the last few years has seen a significant increase. The accuracy and efficacy of this method in terms of surgical outcomes has been assessed in several peer-reviewed journals and presentations. 11–19 It is difficult for radiology departments to accurately assess all available localisation methods and often the method of choice is dictated by equipment already available or chosen by the local surgical departments. In addition, publications regarding the radiological aspects of the method remain relatively sparse to-date. The purpose of this article is not to discuss the technical aspects and accuracy of MagSeed® surgery, but to review the technical and radiological aspects of localisation, to assess the radiological accuracy of the method comparing the position of the MagSeed® in relation to the lesion or the post-biopsy marker on post-localisation mammograms and intraoperative specimen X-Rays, to look into how this impacts the completeness of surgical excision and to discuss our radiological experience of this technique.
Methods and materials
Setting
This is a retrospective, observational study conducted at three units of the West of Scotland Cancer Network (WoSCAN). The data presented were collected over a period of 2 years, from 1 January 2018 to 31 December 2019, from the radiological Reporting Information System (RIS), the Picture Archiving and Communication System (PACS) and the clinical portals.
The MagSeed® is a 5 × 1 mm cylindrical bead of paramagnetic stainless steel and iron oxide that contains less than 0.23% Nickel and is readily visible on mammography and ultrasound. It is preloaded into an 18 gauge, 7 cm and 20-cm-long steel needle and is retained by a wax plug. A steel obturator is used to deploy the seed (Figure 1).
Figure 1.
MagSeed® with 18-gauge steel needle and wax plug.
In an outpatient setting, the radiologist inserted one or more seeds into the area of concern under mammographic or ultrasonographic guidance, after local anaesthesia. A small hypoallergenic plaster was then applied to the skin.
During the period covered by this study, the MagSeed® was, for the most part, licensed for placement up to 30 days prior to surgery.
Several different full-field digital mammography (MMG) and ultrasound units (US) with 12–18MHz high-frequency linear probes were used to guide the performing radiologist. Two standard 90 degree craniocaudal and mediolateral mammograms were performed to check the seed’s deployment and position within the breast. Unless operated on the day of the localisation, the patient could return home until the day of surgery. No mammograms were repeated prior to surgery.
As these were the first MagSeed® cases, they were all performed by consultant radiologists with more than 5 years of experience in breast imaging.
Breast conserving surgery was performed by eight consultant breast surgeons. During surgery, the MagSeed® was detected and excised with the use of a sensitive probe (SentiMag®), which generates an alternating magnetic field that transiently magnetises the seed and then measures the magnetic field emitted by it.
The surgical specimen was transported to the imaging department where an X-ray was performed to check for the presence of the lesion and/or the MagSeed®. The result was communicated to the operating theatre by the radiologist.
Participants
Our study included symptomatic and screening patients with one or more palpable and/or impalpable, unilateral or bilateral, breast lesions that had a pathological diagnosis of cancer or at least indeterminate pathology on 14G core needle and/or 10G vacuum-assisted core biopsies within the previous 14 days and were considered suitable for breast conserving surgery with MagSeed® localisation by the multidisciplinary team meeting. The cases of palpable lesions (n = 10) were the first few cases performed in each department as part of a learning curve. Cases of mammographically occult lesions, extensive areas of ductal carcinoma in situ (DCIS) and of cancers treated by neo-adjuvant chemotherapy (NACT) in which accurate mammographic assessment is more challenging were also included. Patients with heart pacemakers and with known Nickel allergy were excluded from this study.
Variables
The time interval between the localisation and the operation was recorded.
The position of the MagSeed® in relation to the localised lesion or the post-biopsy radiological marker was reviewed on the post-localisation mammograms. Placement was considered accurate when the MagSeed® was visible within or partly within the lesion. In cases where the MagSeed® was not within the lesion, accuracy was measured by measuring the distance of the MagSeed® from the edge of the lesion or the post-biopsy marker in mm.
Comparison of the imaging modality of choice (US v MMG) for the localisation was performed.
The intraoperative specimen X-rays were reviewed a) for the presence of the lesion and the MagSeed®, b) in terms of the position of the localised lesion in the specimen, c) in terms of the position of the MagSeed® in relation to the localised lesion.
Outcomes
Successful MagSeed® deployment was confirmed when the MagSeed® was visible on both views on the pair of 90 degree post-localisation mammograms. The localisation was considered radiologically accurate when the MagSeed® was visible in the lesion or within 5 mm from the edge of the lesion or from the post-biopsy marker.
Excision was deemed successful when the localised lesion and/or post-biopsy marker and the MagSeed® were visible in the specimen X-ray and confirmed on histopathology. In cases of mammographically occult lesions at the time of the initial diagnosis or in cases of mammographically visible lesions at initial diagnosis that became mammographically occult at the time of localisation as a result of NACT, radiologically successful excision was considered the presence of the MagSeed® in the specimen X-ray.
The number of cases that required surgical re-excision were reviewed. The re-excision rate was documented and compared to our centres’ acceptable re-excision rates. Key points in the radiological workup of these cases were noted.
Descriptive and Fisher’s exact test statistics were used to analyse data and determine statistical significance.
Results
In the 2-year period covered by our study, 309 seeds were inserted into 300 patients.
The patients age ranged from 19 to 85 years with a mean age of 57.5 years. The size of the lesions on pathology ranged from 6 to 56 mm with a mean size of 19.5 mm. No mammography was performed on a young patient with indeterminate pre-operative pathology. The localised lesions are categorised by histopathological and radiological types in Table 1.
Table 1.
Histopathologic and mammographic classification of localised lesions. (IDC = invasive ductal carcinoma, ILC = invasive lobular carcinoma, DCIS = ductal carcinoma in situ)
| Absolute value | % value | |
|---|---|---|
| Histopathologic types of lesions | 309 | 100.0 |
| Malignant (IDC, ILC, DCIS and combinations) | 290 | 93.9 |
| Benign (papilloma, phylloides, fibroadenoma) | 19 | 6.1 |
| Mammographic types of lesions | ||
| Ill-defined mass | 208 | 67.3 |
| Calcifications | 29 | 9.4 |
| Ill-defined mass + Calcifications | 25 | 8.1 |
| Well-defined mass | 23 | 7.4 |
| Parenchymal Distortion | 11 | 3.6 |
| Mammographically occult | 6 | 1.9 |
| Parenchymal Distortion + Calcifications | 5 | 1.6 |
| Ill-defined mass + Parenchymal Distortion | 1 | 0.3 |
| Not had mammogram | 1 | 0.3 |
Time interval
Most of the cases 233/300 (77.7%) were operated on a day different to the day of localisation, whereas the remaining 67/300 (22.3%) underwent operation on the day of localisation. The time interval between the day of localisation and the day of surgery varied between 0–49 days with an average time of 7.2 days. Only one case in our dataset breached the 30-day term due to logistical issues with surgical scheduling. The lesion and the MagSeed® were successfully excised in this case.
Successful deployment
Successful deployment was achieved in 306 of the 309 cases (99%). In the remaining three cases, the MagSeed® migrated/retracted along the catheter tract and a guide-wire was used to localise the lesion. During the operation, the misplaced MagSeeds® were detected by the SentiMag® probe and removed.
In two cases, a post-localisation mammogram was not performed. One case was a young patient with a pathologically indeterminate lesion. The other case was a patient with previous mastectomy and reconstruction who was found to have a new ipsilateral cancer on computed tomography (CT).
Modality of localisation
Ultrasonography was the imaging guidance modality in 269 localisations whereas mammography was used to guide the radiologist in the remaining 40 cases. Two out of the three cases in which the MagSeed® migrated/retracted along the catheter tract were ultrasonographically guided and one was mammographically guided.
Localisation accuracy
On the post-localisation mammograms, the localisation was deemed accurate when the MagSeed® was thought to be radiologically within or partly within the lesion or within 5 mm from the lesion or the post-biopsy marker on both mammographic views. This was true in 296 out of 304 (97.3%) of the cases. In 2 cases (0.7%) the seed was visible more than 5 mm from the localised lesion or the marker. In 6 cases (2%) the lesion was considered to be mammographically occult or was not visible on both mammographic views and therefore the accuracy of the localisation was impossible to assess. Table 2 presents the analysis of the position of the MagSeed® on the post-localisation mammograms.
Table 2.
Position of the MagSeed® in relation to the target lesion on the 90 degree pair of post-localisation mammograms (n = 304)
| Position of MagSeed® in relation to lesion | Absolute value | % value |
|---|---|---|
| Satisfactory position (within/partly within lesion) | 271 | 89.1 |
| <5 mm from lesion or marker | 25 | 8.2 |
| >5 mm from lesion or marker | 2 | 0.7 |
| Not able to comment (mammographically occult/not visible on both 90 degree views) | 6 | 2.0 |
From the 298 successfully localised lesions that could be assessed on the post-localisation mammograms, the MagSeed® was in or partly within the lesion in 235 of 259 ultrasonographically guided localisations (90.7%) and in 36 of 39 mammographically guided ones (92.3%). It was visible within less than 5 mm from the edge of the lesion in 23 cases in which ultrasound was the localisation method (8.9%) and in 2 cases in which mammography was used (5.1%). In one case of ultrasonographically guided (0.4%) and in one case of mammographically guided localisations (2.6%), the MagSeed® was visible more than 5 mm from the target lesion.
The overall accuracy of the successful ultrasonographically guided localisations that could be assessed on the pair of post-localisation mammograms was 297 of 298 (99.6%) and of the mammographically guided localisations it was 38 of 39 (97.4%). This is not a statistically significant difference (p = 0.218; Fisher’s exact test).
Specimen X-ray
The specimen X-rays were reviewed in terms of the position of the localised lesion within the specimen.
The lesion was visible centrally within the specimen in 134 of 297 X-rays (45.1%), in 106 (35.7%) it was eccentric within more than 1 mm from the margin and in 44 (14.8%) cases it was thought to be at the specimen’s margin. In all of the latter cases, the surgeon was informed about the result by the radiologist and further radial excisions were taken. It was not possible to comment in 13 (4.4%) of the excised lesions. These included radiologically occult lesions, cases of scattered microcalcifications and cases undergoing therapeutic mammoplasties before or after NACT. In six cases, no specimen X-ray was performed. (Table 3)
Table 3.
Position of localised lesion in excision specimen X-rays (n = 297). (Eccentric=>1 mm from margin). Not able to comment includes: radiologically occult at presentation or after NACT (6); scattered microcalcifications (3); therapeutic mammoplasties (4)
| Position of lesion in specimen | Absolute value | % value |
|---|---|---|
| Central | 134 | 45.1 |
| Eccentric | 106 | 35.7 |
| At margin | 44 | 14.8 |
| Not able to comment | 13 | 4.4 |
The position of the MagSeed® in relation to the lesion was deemed to have been radiologically within or partly within the lesion or within 5 mm from the lesion or the post-biopsy marker in 283 out of 300 (94.3%) of the cases. In two cases (0.7%), the seed was visible more than 5 mm from the localised lesion or the marker. In six cases (2%), the localised abnormality was not visible on mammography and therefore it was not possible to assess the position of the MagSeed® in relation to it. Interestingly, in nine cases (3%), the MagSeed® was not visible on the specimen X-ray and as it was not visible on a mammogram performed a few weeks after the operation it was assumed that it fell out during the procedure. Since excision of the target lesion was confirmed on pathology, no further action was required in these cases. (Table 4)
Table 4.
Position of the MagSeed® in relation to the target lesion in excision specimen X-rays (n = 297). Not able to comment includes: MMG occult (6); MagSeed® not visible (9)
| Position of MagSeed® in relation to lesion | Absolute value | % value |
|---|---|---|
| Satisfactory position (within/partly within lesion) | 256 | 85.3 |
| <5 mm from lesion or marker | 27 | 9.0 |
| >5 mm from lesion or marker | 2 | 0.7 |
| Not able to comment | 15 | 5.0 |
All of the localised lesions were successfully detected intraoperatively and removed with the SentiMag® probe. Two lesions that were initially undetectable were eventually successfully excised by inserting the probe closer to the lesion through the skin incision. Successful removal of their breast lesion on the first operation was possible in 245 cases (81.7%). In the remaining 55 cases (18.3%), re-excision was required for positive margins of less than 1 mm on the histopathological specimen which is the acceptable disease-free margin in our institutions.
Discussion
The MagSeed® is a new method for the preoperative localisation of impalpable breast lesions in breast conserving surgery. For the performing radiologist, the localisation technique is similar to the one used for the guide-wire with no technical caveats or additional requirements for the imaging department. The tip of the insertion needle is well visible in real-time ultrasound and the seed is clearly seen as a hyperechoic, linear artefact with minimal posterior acoustic shadowing. The seed is smoothly deployed immediately next to the tip of the insertion needle during the mammographic-guided localisations, allowing for good control by the radiologist. The tip of the insertion needle is sharp enough to penetrate with ease into the centre of hard lesions and the smooth deployment of the MagSeed® next to the tip allows for accurate prediction of its placement, particularly within strongly hypoechoic lesions with posterior acoustic shadowing. Localisation of soft lesions or calcifications within entirely fatty breasts can be slightly less accurate but is still satisfactory. Overall, MagSeed® localisation appears to be at least as fast as guide-wire localisation, probably due to the fact that the post-localisation mammogram takes less time to perform as there are no uncomfortable wires involved. Figure 2 depicts an ultrasound-guided MagSeed® localisation with post-localisation mammograms and surgical specimen X-ray.
Figure 2.
(From top left to bottom right) a. ultrasonographic appearances of an impalpable invasive ductal carcinoma, b. lesion with introducer in situ, c. MagSeed® visible as an intensely hyperechoic, linear, metallic artefact with minimal posterior acoustic shadowing within the lesion following localisation, d. craniocaudal and e. mediolateral views post-localisation mammograms with MagSeed® visible within the lesion, f. specimen X-ray depicting MagSeed® and lesion slightly eccentrically within the excision specimen.
Importantly, there were no adverse events observed during the radiological procedure, in contrast to guide-wire localisations, where vasovagal episodes due to the patient’s heightened anxiety in combination with a fasted state on the day of surgery can occur. Anecdotal feedback by the performing radiologists highlighted that they considered this technique easy to perform and welcomed the scheduling of the procedure on a different day to surgery, as opposed to the often stressful, complicated morning theatre cases.
Successful MagSeed® deployment was observed in 99% of the cases with an accuracy of 97.3% on the post-localisation mammograms. There was no post-procedural haematoma that could potentially obscure the lesion on the post-localisation mammograms. There does not appear to be any significant difference (p > 0.05) in the accuracy of the localisation whether this was performed under ultrasonographic or mammographic guidance (99.6% US vs 97.4% MMG). This reflects good visibility, control and deployment of the seed at the tip of the needle, independent of the operator or the modality.
Since 77.7% of our cases were operated on a different day to the localisation, with a mean interval of 7.2 days, delayed seed migration was a theoretical possibility, but there were no such cases in this study. Our numbers are comparable to those from other studies evaluating the reliability of the MagSeed®. 12,14,15 The equally high percentage of satisfactory positioning of the MagSeed® in relation to the lesion on the specimen X-ray compared to the post-localisation mammogram, suggests that a second mammogram immediately prior to surgery does not offer any clinical benefits to preoperative planning. Several of the cases that had an operation on the day of localisation were amongst the first ones to be localised with a MagSeed® and reflected contingency planning, taking into account an anticipated learning curve.
The variability of the position of the localised lesion on the excision specimen X-rays probably reflects individual differences in surgical technique, different learning curves as well as differences in the degree of difficulty of the surgical procedures. Most of the cases in which the radiologist could not comment on the position of the lesion, involved oncoplastic procedures with one or more MagSeeds® in the breast, cases of mammographically occult lesions or NACT cases in which the relative position of the MagSeed® to the lesion could not be accurately established radiologically.
The mean lesion size of 19.5 mm reflects the presence of several cases of multifocal/multicentric disease that underwent therapeutic mammoplasties. The re-excision rate of 18.3% is comparable to the published re-excision rate for the WoSCAN (14.8%) and is similar to the rates published in other studies that compare the efficacy of the MagSeed® to the guide-wire bearing in mind that in our study the histopathologically acceptable disease-free margin was 1 mm. 11–22 It is beyond the scope of this study, which contains a variety of cases ranging from simpler, palpable lesions to more complex cases with multifocal/multicentric lesions and NACT cases, to comment on the surgical specimens’ features such as their size and weight or on the re-excision rates.
After careful review of the intraoperative specimen X-rays of the 55 cases that required a second operation because of involved excision margins on pathology, there were no radiological findings suggestive of margin involvement. The most common cause for re-excision was the presence of radiologically occult DCIS at the margin, followed by cases that had undergone NACT. In these cases, the specimen X-ray is usually insufficient to provide the radiologist with features suggestive of margin involvement as depending on the degree of response to NACT, the radiological features of malignancy can become very subtle or even disappear. Since all the MagSeeds® were intraoperatively detected and excised, there appears to be no correlation between the accuracy of the radiological localisation and surgical re-excision in mammographically occult lesions.
Concerns about the detection of the MagSeed® with the SentiMag® probe in cases of lesions located deep within the breast have been raised in the literature. All studies demonstrate successful lesion detection and excision albeit with different degrees of difficulty. 12,15,17,22 Interestingly, in our study, the two cases in which the surgeon was initially unable to detect the signal the MagSeed® was located more than 8 cm from the skin on mammography. That might explain the initial detection failure as the recommended depth detection range by the manufacturer is 4 cm from the skin.
Despite the user friendliness and versatility of MagSeed® localisation, its advantages may be somewhat counterbalanced by some inherent limitations as well as high cost. Placement of the seed under MRI-guidance is not feasible because of the stainless-steel deployment needle. The sizeable 2–4 cm artefact produced by the MagSeed® on magnetic resonance imaging (MRI), which has been described in other studies and is mentioned on the product’s specifications, may limit its use in patients receiving neoadjuvant treatment whose response is monitored by breast MRI (Figure 3). 22
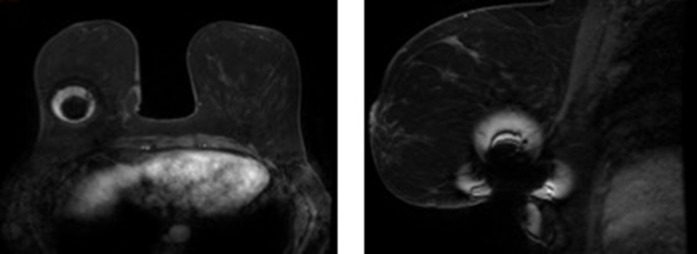
Figure 3.
a. Axial and b. Sagittal views of an inserted MagSeed® with associated artefact on dynamic, contrast enhanced breast MRI
Since the conclusion of this study the licensing for Europe and the USA increased from 30 days prior to surgery to long-term placement. The licensing extension of the time length for the use of the MagSeed® in the axilla will hopefully also allow greater flexibility in the management of axillary lymph node surgery in the future.
Patients with heart pacemakers and with known Nickel allergy were excluded from this study. According to the manufacturer’s product specifications the MagSeed® is not officially indicated for use in Nickel-allergic patients, however it contains much less Nickel compared to a stainless-steel guide-wire. Patients with pacemakers were excluded because at the time of the study it was not clear whether the magnetic field generated by the MagSeed® could affect the pacemaker. To-date there is no relevant literature to validate this.
Specialised equipment procurement and capital investment by the surgical and radiology departments are required prior to the establishment of the technique and a budget covering the ongoing operational costs should be considered. Although these are fairly significant in absolute monetary value, budget impact analysis of MagSeed® versus guide-wire localisations in breast conserving surgery has shown an advantage of the use of MagSeed® when personnel and scheduling factors are considered. 23
Ongoing research as well as randomised trials in the context of structured assessment for surgical innovation looking at the benefits of increased flexibility on surgical waiting lists and patient satisfaction related to cost may strengthen or weaken the business case for guide-wire localisation becoming a technique of the past. 19,24
Conclusion
In conclusion, the radiological experience of the use of the MagSeed® in the preoperative imaging-guided localisation of breast lesions is that it is a straight forward, accurate and reliable method. There appears to be no delayed MagSeed® migration and it can be safely inserted on a different day to surgery. This makes it logistically attractive to overstretched breast units struggling to pair-up radiological with surgical activities.
Footnotes
Conflicts of Interest: Τhe authors declare fully that there are no conflicts of interest in this manuscript.
Contributor Information
Fotios Constantinidis, Email: drfconstantinidis@gmail.com, Department of Imaging NHS Forth Valley, Larbert, UK .
Sophia Sakellariou, Email: Sophia.Sakellariou@ggc.scot.nhs.uk, Department of Imaging NHS Greater Glasgow and Clyde, Glasgow, UK .
Sau Lee Chang, Email: SauLee.Chang@ggc.scot.nhs.uk, Department of Imaging NHS Greater Glasgow and Clyde, Glasgow, UK .
Svetlana Linder, Email: Svetlanakarenga.Linder@ggc.scot.nhs.uk, Department of Imaging NHS Greater Glasgow and Clyde, Glasgow, UK .
Barbara MacPherson, Email: Barbara.macpherson@nhs.net, Department of Imaging NHS Lanarkshire, Wishaw, UK .
Subodh Seth, Email: Subodh.Seth@nhs.scot, Department of Surgery NHS Forth Valley, Larbert, UK .
Nicola Gill, Email: Nicola.Gill@nhs.scot, Department of Imaging NHS Forth Valley, Larbert, UK .
Archana Seth, Email: Archana.Seth@ggc.scot.nhs.uk, Department of Imaging NHS Greater Glasgow and Clyde, Glasgow, UK .
REFERENCES
- 1. Kopans DB, DeLuca S . A modified needle-hookwire technique to simplify preoperative localization of occult breast lesions . Radiology 1980. ; 134( 3 ): 781 . doi: 10.1148/radiology.134.3.7355235 [DOI] [PubMed] [Google Scholar]
- 2. Chan BKY, Wiseberg-Firtell JA, Jois RHS, Jensen K, Audisio RA . Localization techniques for guided surgical excision of non-palpable breast lesions . Cochrane Database Syst Rev 2015. ; 12: CD009206 . doi: 10.1002/14651858.CD009206.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Luini A, Zurrida S, Galimberti V, Paganelli G . Radioguided surgery of occult breast lesions . Eur J Cancer 1998. ; 34: 204 – 5 . doi: 10.1016/s0959-8049(97)00376-6 [DOI] [PubMed] [Google Scholar]
- 4. Goudreau SH, Joseph JP, Seiler SJ . Preoperative radioactive seed localization for nonpalpable breast lesions: technique, pitfalls, and solutions . Radiographics 2015. ; 35: 1319 – 34 . doi: 10.1148/rg.2015140293 [DOI] [PubMed] [Google Scholar]
- 5. Pieri A, Milligan R, Critchley A, O’Donoghue JM, Sibal N, et al. . The introduction of radioactive seed localisation improves the oncological outcome of image guided breast conservation surgery . Breast 2017. ; 36: 49 – 53 : S0960-9776(17)30576-3 . doi: 10.1016/j.breast.2017.09.004 [DOI] [PubMed] [Google Scholar]
- 6. Sung JS, King V, Thornton CM, Brooks JD, Fry CW, et al. . Safety and efficacy of radioactive seed localization with i-125 prior to lumpectomy and/or excisional biopsy . Eur J Radiol 2013. ; 82: 1453 – 57 : S0720-048X(13)00203-9 . doi: 10.1016/j.ejrad.2013.04.008 [DOI] [PubMed] [Google Scholar]
- 7. De Cicco C, Gatti G, Luini G, Radioguided Surgery . Radioguided Occult Lesion Localization in the Breast . New York: : Springer; . 2008. . doi: 10.1007/978-0-387-38327-9 [DOI] [Google Scholar]
- 8. Cox CE, Russell S, Prowler V, Carter E, Beard A, et al. . A prospective, single arm, multi-site, clinical evaluation of a nonradioactive surgical guidance technology for the location of nonpalpable breast lesions during excision . Ann Surg Oncol 2016. ; 23: 3168 – 74 . doi: 10.1245/s10434-016-5405-y [DOI] [PubMed] [Google Scholar]
- 9. Mango VL, Wynn RT, Feldman S, Friedlander L, Desperito E, et al. . Beyond wires and seeds: reflector-guided breast lesion localization and excision . Radiology 2017. ; 284: 365 – 71 . doi: 10.1148/radiol.2017161661 [DOI] [PubMed] [Google Scholar]
- 10. Kasem I, Mokbel K . Savi scout® radar localisation of non-palpable breast lesions: systematic review and pooled analysis of 842 cases . Anticancer Res 2020. ; 40: 3633 – 43 . doi: 10.21873/anticanres.14352 [DOI] [PubMed] [Google Scholar]
- 11. Crane J, Photi E, Down S . P152. a dgh’s experience using magseed as a localisation tool for impalpable breast lesions . European Journal of Surgical Oncology 2019. ; 45: 923 – 24 . doi: 10.1016/j.ejso.2019.01.172 [DOI] [Google Scholar]
- 12. Price ER, Khoury AL, Esserman LJ, Joe BN, Alvarado MD . Initial clinical experience with an inducible magnetic seed system for preoperative breast lesion localization . AJR Am J Roentgenol 2018. ; 210: 913 – 17 . doi: 10.2214/AJR.17.18345 [DOI] [PubMed] [Google Scholar]
- 13. Lake B, Wilson M, Williams S, Metelko M, Thomas G, et al. . 25. magseed for localisation of impalpable breast cancers is associated with high patient satisfaction and lower re-excision rates . European Journal of Surgical Oncology 2018. ; 44: 1839 . doi: 10.1016/j.ejso.2018.10.030 [DOI] [Google Scholar]
- 14. Zacharioudakis K, Down S, Maxwell A, Howe M, Harvey J . P037. magseed localisation of non palpable breast cancer. is the future magnetic? European Journal of Surgical Oncology 2019. ; 45: 895 – 96 . doi: 10.1016/j.ejso.2019.01.059 [DOI] [PubMed] [Google Scholar]
- 15. Harvey JR, Lim Y, Murphy J, Howe M, Morris J, et al. . Safety and feasibility of breast lesion localization using magnetic seeds (magseed): a multi-centre, open-label cohort study . Breast Cancer Res Treat 2018. ; 169: 531 – 36 . doi: 10.1007/s10549-018-4709-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Thekkinkattil D, Kaushik M, Hoosein MM, Al-Attar M, Pilgrim S, et al. . A prospective, single-arm, multicentre clinical evaluation of a new localisation technique using non-radioactive magseeds for surgery of clinically occult breast lesions . Clin Radiol 2019. ; 74: 974 . S0009-9260(19)30533-1 . doi: 10.1016/j.crad.2019.08.018 [DOI] [PubMed] [Google Scholar]
- 17. Gera R, Tayeh S, Al-Reefy S, Mokbel K . Evolving role of magseed in wireless localization of breast lesions: systematic review and pooled analysis of 1,559 procedures . Anticancer Res 2020. ; 40: 1809 – 15 . doi: 10.21873/anticanres.14135 [DOI] [PubMed] [Google Scholar]
- 18. Lamb LR, Bahl M, Specht MC, D’Alessandro HA, Lehman CD . Evaluation of a nonradioactive magnetic marker wireless localization program . AJR Am J Roentgenol 2018. ; 211: 940 – 45 . doi: 10.2214/AJR.18.19637 [DOI] [PubMed] [Google Scholar]
- 19. Lake B, Wilson M, Thomas G, Williams S, Usman T . P006: the triple effect of the magseed for localisation of impalpable breast cancer: significant reduction in re-excision rate, cost saving by reducing further surgery and high patient satisfaction . European Journal of Surgical Oncology 2020. ; 46: e12 . doi: 10.1016/j.ejso.2020.03.045 [DOI] [Google Scholar]
- 20. Harvey J, Barnes N, Maxwell A, Lim Y . Magseed for wide local excision surgery . European Journal of Surgical Oncology 2018. ; 44: 918 . doi: 10.1016/j.ejso.2018.02.241 [DOI] [Google Scholar]
- 21. West of Scotland Cancer Network . Final Published Breast Cancer MCN Audit Report v1.0. West of Scotland Cancer Network, UK . 2020. . Available from : https://www.woscan.scot.nhs.uk/wp-content/uploads/Final_Published_QPI-Audit-Report-v0.1_140120.pdf ( accessed 14 Jan 2020 )
- 22. McCamley C, Ruyssers N, To H, Tsao S, Keane H, et al. . Multicentre evaluation of magnetic technology for localisation of non-palpable breast lesions and targeted axillary nodes . ANZ J Surg 2021. ; 91: 2411 – 17 . doi: 10.1111/ans.17108 [DOI] [PubMed] [Google Scholar]
- 23. Lindenberg M, van Beek A, Retèl V, van Duijnhoven F, van Harten W . Early budget impact analysis on magnetic seed localization for non-palpable breast cancer surgery . PLoS One 2020. ; 15( 5 ): e0232690 . doi: 10.1371/journal.pone.0232690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ahmed M . The bottom line for lesion localization in breast cancer . Breast Cancer Res Treat 2020. ; 182: 523 – 25 . doi: 10.1007/s10549-020-05735-x [DOI] [PubMed] [Google Scholar]