Abstract
Fungal endophthalmitis is a potentially blinding condition. It is more often reported from Asia, including India. The incidence is lower than bacterial endophthalmitis. But it is relatively more challenging to treat than bacterial endophthalmitis. Many eyes may need therapeutic keratoplasty and/or evisceration. The current mainstays of treatment are vitrectomy irrespective of the presenting vision, intravitreal antifungal agents, and systemic therapy; additionally, the patients could require prolonged treatment with repeat vitreous surgeries and intravitreal injections. Difficulty in clinical diagnosis, delay in microbiological culture, and limited options of antifungal drugs make the treatment more difficult and less rewarding. Three common fungi causing endophthalmitis are Aspergillus, Fusarium, and Candida. The former two are molds, often identified in exogenous endophthalmitis, postoperative and traumatic; the latter is yeast and is more often identified in endogenous endophthalmitis. A faster diagnosis with newer molecular microbiological technologies might help institute treatment earlier than it is currently possible. A target trial using big data from different regions of the world might emulate a randomized clinical trial to design a definite treatment strategy. Given fewer antifungal drugs, one must be mindful of antifungal stewardship to prevent resistance to the existing drugs.
Keywords: Antifungal stewardship, endophthalmitis, fungus, microbiology, minimum fungicidal concentration, outcome, pathology, treatment
Fungi are eukaryotic organisms and are ubiquitous. Three types of fungi—molds, yeasts, and diphasic—mainly cause ocular infections. The molds are filamentous fungi and could be septate or nonseptate. There are 1.5–5 million species of fungi that can grow almost anywhere—water, soil, plants, and animals. Some fungi form spores which we inhale (e.g., Aspergillus and Fusarium sp.), and others live as human commensal organisms (e.g., Candida and Malassezia sp.). Despite these close encounters, our immune system recognizes and protects us from fungal infections. The primary pathogenic fungi usually have an environmental reservoir. Opportunistic pathogens take advantage of debilitated or immunocompromised hosts to cause infection.[1] All fungi do not have innate pathogenicity. It is acquired from the environment or may be endogenous in the few instances where they are members of the resident flora. The pathogenesis of fungal disease involves an interplay between fungal virulence factors and host immune responses.
Three key factors define the outcome of the infecting fungi: the infectivity, the pathogenicity, and the virulence. Infectivity is an organism’s ability to infect a host. Exposure may lead to carriage (colonization) or symptomatic disease, transient or chronic. Pathogenicity is the ability of an organism to cause disease that depends on the human host-pathogen interactions. Virulence is the relative capacity of the microbe to cause damage to the host, reflected by the ability of the pathogen to multiply within the host and the virulence factors.
The primary fungal pathogens can cause disease in noncompromised patients. But most pathogenic fungi are opportunistic and do not usually cause disease unless there are alternations in immune defense. Immunosuppressive drugs, the human immunodeficiency virus (HIV) infection, and excessive use of systemic antibiotics could result in such alternations. In these situations, the opportunistic pathogens produce virulence factors that allow the organisms to grow as commensals as long as the host is healthy and takes its opportunity to become pathogenic when the host’s immune system is lowered. The virulence factors allow the fungi to grow at elevated temperatures (up to 42°C), with increased ability for tissue adherence, tissue penetration, and dissemination. The innate immune system is the first line of defense against pathogens. The innate cells use genetically inherited receptors, the pattern recognition receptors (PRRs), to recognize the conserved pathogen-associated molecular patterns (PAMPs) present in nearly all microorganisms. Signaling downstream, the PRRs activate the cellular responses to the killing mechanisms and shape the adaptive immune responses.[2,3] The most important PAMPs in filamentous fungi are mannan, b-glucan, and chitin.
Infection occurs when fungi accidentally penetrate barriers (such as intact skin and mucous membrane linings) or breach the immunological defense (such as the immunocompromised state, debilitating conditions of the host). Fungi also gain access to the host tissues after penetrating trauma or inhalation. The severity of the disease depends upon the size of the inoculum, the magnitude of tissue destruction, the ability of the fungi to multiply in tissues, and the immunologic status of the host.[4] Fungal infection, including endophthalmitis of the eye, occurs more often in tropical climates, including India. It is more challenging to treat than a bacterial infection. One must understand the science of fungal endophthalmitis to recognize early and treat effectively. This review examines various related issues of fungal endophthalmitis.
Current Knowledge
Epidemiology
Common ocular fungal infections are keratitis and endophthalmitis; rarer ones are the orbital infection and dacryoadenitis [Table 1]. Fungal endophthalmitis is more challenging to treat. It is infrequently reported from Europe and North America,[5,6] than Asia.[7,8] India has reported more fungal endophthalmitis than other Asian countries (postoperative endophthalmitis 16.7%, and traumatic endophthalmitis 14.4%).[9,10] Aspergillus and Fusarium sp. are commonly isolated in exogenous fungal endophthalmitis; the patients are usually immunocompetent. The risk factors in endogenous infection include a history of recent hospitalization, diabetes mellitus, renal or liver failure, indwelling intravenous lines, catheterization, organ transplantation, intravenous drug use, and immunosuppressive (particularly corticosteroid) treatment.[11,12] Yeasts (Candida sp.) are more often isolated than molds in endogenous endophthalmitis. The common fungi identified in a large series of 723 fungal endophthalmitis collected across India were Aspergillus sp. (37.06%), Fusarium sp. (16.87%), and Candida sp. (10.65%).[13]
Table 1.
Overview of common fungi with particular reference to ocular infection.
| Organism | Morphology | Interaction with human host | Principal habitat | Major infection | Antifungal drug of choice | |||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| C | O | P | General | Eye | ||||
| Aspergillus spp. (A flavus) | Mold, Hyphae | x | x | x | Soil, Environment | Aspergillosis Lung, Paranasal sinus |
Keratitis Endophthalmitis Dacryocystitis |
Itraconazole Voriconazole Amphotericin B Posaconazole Caspofungin |
| Candida spp (C albicans) | Yeast | x | x | - | GI tract, mucosa, skin | Candidiasis Oral, Blood, Vaginal | Endophthalmitis | Amphotericin B |
| Fusarium spp (F solani) | Hyphae | x | x | - | Soil, Plant | Fusariosis Blood, Skin, Bone | Keratitis Endophthalmitis |
Amphotericin B Natamycin Voriconazole |
| Mucor Rhizopus oryzae Mucor ramosissimus | Mold, Hyphae | - | x | - | Soil, Dead decaying fruits, vegetables and plants. | Mucormycosis Brain, Stomach Lungs |
Sino-orbital | Amphotericin B Liposomal Amphotericin B Voriconazole |
C- commensal; O- opportunistic; P- pathogenic
Pathobiology
The mechanical barriers of the eye to prevent infection are the eyelids, eyelashes, the blink reflex, the tear film, the nonkeratinized squamous epithelium of the conjunctiva and cornea, and the lacrimal excretory system. A breach in these barriers either by trauma, surgery, or extension of fungal keratitis (including corneal perforation) causes exogenous endophthalmitis. The endogenous infection spreads from choroidal capillaries to the vitreous through disrupted Bruch’s membrane. In either situation, there is acute suppurative inflammation and necrosis of the vitreous. Dense infiltration of polymorphonuclear leukocytes forms microabscesses and foreign body type of multinucleated giant cell reaction with or without granuloma formation[14] [Figs. 1 and 2].
Figure 1.
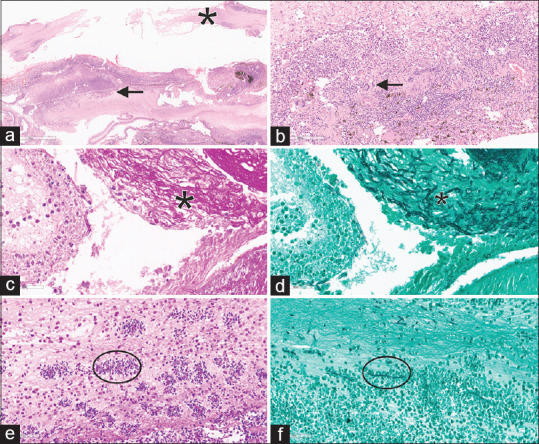
Photomicrograph of exogenous fungal endophthalmitis (a) Perforated cornea (asterix) with dense inflammation (arrow) of intraocular structure (H and E; scanner view). (b) Histiocytes and multinucleate giant cells (arrow) with dense chronic infiltrate forming microabscess and scattered uveal pigments (H and E × 300). (c and d) Fungal hyphae and chlamydospores (PAS left and GMS right, ×400). (e and f) Microabscesses in vitreous with central fungal filaments (within the circle- PAS left × 300 and GMS, right × 300)
Figure 2.
Photomicrograph of endogenous endophthalmitis. (a) Fragments of the choroid (arrow) and retina (arrowhead) densely infiltrated with inflammatory cells, extending into the vitreous cavity (H and E, ×200). (b) Fragments of fungal hyphae (within the circle) noted in the retina (H and E, ×300). (c and d) Suppurative inflammation of vitreous (asterix) with fungal hyphae, which are hyaline, thin, septate, and branched (PAS left × 300 and GMS right, ×400)
The polymorphonuclear leukocytes can ingest and kill microorganisms by two main pathways: oxygen-dependent and oxygen-independent pathways. The oxygen-dependent pathway is based on the post-phagocytic intracellular production of oxygen radicals. The oxygen-independent pathway is based mainly on the function of an antimicrobial protein, “defensins.” Defensins are peptides that possess broad-spectrum antimicrobial activity in vitro, killing a variety of gram-positive and gram-negative bacteria and some fungi.[15]
Aspergillus flavus and Aspergillus fumigatus are the common pathogenic fungi reported from India. Aspergillosis occurs in people with chronic pulmonary diseases, organ transplants (liver, renal and bone marrow), leukemia, and drug abuse. The fungus usually gains access to the eye as it spreads from the lungs to the choroid and invades the retinal and choroidal vessel walls. Histologically, Aspergillus grows preferentially along the subretinal pigment epithelium and subretinal space; the visual outcome is invariably poor because of the preferred macular involvement.[16] Candida is an opportunistic pathogenic yeast and becomes pathogenic in various conditions. The common species infecting humans are C. albicans, C. tropicalis, C. parapsilosis, and C. glabrata. Fusarium is a filamentous fungus found in soil and on the plant. Fusarium keratitis is more common than endophthalmitis. It could occur de novo or as an extension of the nonhealing corneal ulcer; when it happens, it is destructive because it produces extracellular proteases that cause matrix degeneration.[17]
Clinical diagnosis
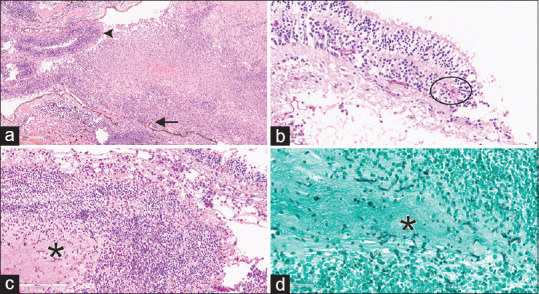
The symptoms and clinical signs of fungal endophthalmitis often mimic chronic bacterial endophthalmitis. The typical characteristics are longer time to symptoms, lower frequency of hypopyon, and indolent inflammation. A history of long-time topical corticosteroid use to reduce recurrent and persistent redness and inflammation is not uncommon. The signs of more typical fungal endophthalmitis include yellow-white infiltrates at the corneoscleral wound (in cataract surgery), nodular exudates over the iris, and crystalline/intraocular lens surface, and vitreous exudates arranged like a string of pearls and creamy white circumscribed chorioretinal lesion[18] [Fig. 3]. Time to symptoms is lesser in traumatic endophthalmitis; injury with vegetative matter and/or retained intraocular foreign body may be a pointer to the diagnosis of traumatic endophthalmitis. Hematogenous seeding from an underlying systemic disease or recent surgery/catheterization is common in patients with endogenous fungal endophthalmitis.[19]
Figure 3.
Fungal endophthalmitis. Presentation, treatment, and outcome. (a) Post cataract; (b) Traumatic; (c) Endogenous. Left-clinical and fundus view. (a) PVA: 20/100; Microbiology: Aspergillus niger. Treatment: three vitreous surgery, IOL explant, three intravitreal antifungals. FVA: 20/50. (b) PVA: FCF 2 meters. Microbiology: Aspergillus flavus. Treatment: two additional vitreous surgery, 14 intravitreal antifungal drugs. FVA: 20/60. (c) PVA: 20/500. Microbiology: Candida albicans. Treatment: Two vitreous surgery and three intravitreal antifungal drugs. FVA- final visual acuity, PVA- presenting visual acuity
Systemic investigations are essential in endogenous endophthalmitis and possibly in other forms of fungal endophthalmitis too. These investigations include complete blood count, serum urea and electrolytes, liver function tests, peripheral blood culture, sputum and urine culture, chest radiogram, liver ultrasonogram, and transthoracic echocardiogram.
Laboratory confirmation
Histopathology of formalin-fixed tissue and microbiology of ocular fluid are the two primary sources of laboratory confirmation. In histopathology, the inflammatory cells are best seen by haematoxylin and eosin (H and E) stains [Figs. 1 and 2]. The fungal hyphae appear as refractile to pale acidophilic filaments, thin or broad, septate or aseptate, and with or without branching. These hyphae are highlighted by special stains like Periodic Acid Schiff (PAS) and Gomori Methenamine Silver (GMS) [Figs. 1 and 2], and Masson Fontana stains. The latter stain helps distinguish pigmented fungi from the rest. However, the characterization of the fungus on histopathology is limited, and hence it needs further ancillary techniques or microbiological culture correlation.[20] The ancillary techniques include immunohistochemistry with antibodies (such as an anti-Aspergillus antibody), fluorescence in-situ hybridization (FISH), and real-time quantitative PCR (qPCR) on formalin fixed paraffin-embedded tissues.
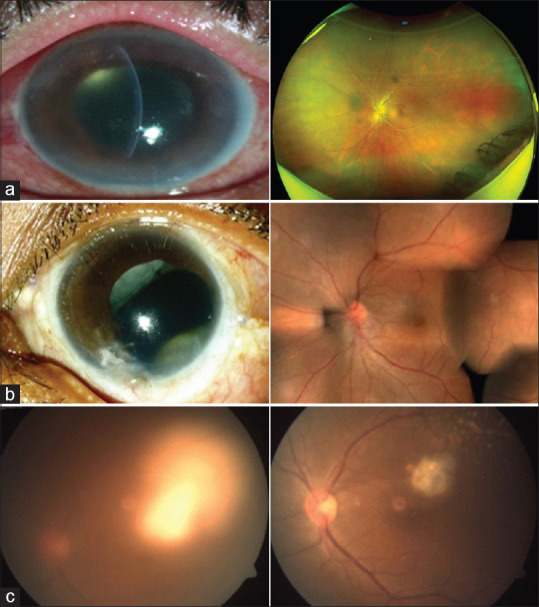
The microbiology confirmation of fungi includes direct microscopy, culture, polymerase chain reaction (PCR), and DNA sequencing. Direct microscopy of the ocular specimen is rapid and is the most commonly employed method. Sabouraud’s dextrose agar (SDA) and potato dextrose agar (PDA) are selective media for fungi, while chocolate agar/blood agar/brain heart infusion broth could also be used. SDA and PDA are incubated at 25°C for 2–4 weeks [Fig. 4].
Figure 4.
Microbiology of common fungi; left-culture and right-microscopy. (a) Aspergillus flavus-culture and microscopy (Lactophenol Cotton Blue). (b) Candida albicans-culture and microscopy (Grams). (c) Fusarium solani-culture and microscopy (Lactophenol Cotton Blue)
Molecular microbiology
The value of conventional smear and culture of intraocular fluids is never denied though it may take a longer time, sometimes 1–2 weeks, for fungi to grow in culture. The fungi may also be sequestered under the lens/capsular bag, making the detection of these organisms difficult;[21] it is not surprising that these are often reported culture negative. Advances in molecular microbiology have improved microbiological diagnosis. Some of these methods include polymerase chain reaction (PCR) and real-time PCR, matrix-assisted laser desorption/ionization–time of flight (MALDI-TOF), and peptide nucleic acid fluorescent in situ hybridization (PNA FISH).
Polymerase Chain Reaction is based on DNA polymerase; it is an in vitro replication of specific DNA sequences. Pan-fungal primers complementary to the 18 S rRNA sequences or the 28 S rDNA have been reported previously, but the most commonly used probes are the ITS 1 and ITS 4 (corresponding to the internal transcribed spacer region, ITS2, of the ribosomal small subunit RNA for fungus) primer sets.[22,23] These tests are highly specific and sensitive. The ITS2-gene-based PCR detects more infecting fungi than conventional culture in fungal endophthalmitis.[24] Various methods are available for species identification following the pan fungal PCR, such as DNA sequence analysis, amplification of fragment length polymorphism (AFLP), and restricted fragment length polymorphism (RFLP). The quantitative real-time PCR quantifies the fungal load in ocular fluids.[25]
MALDI-TOF is an ionization technique that uses a laser energy absorbing matrix to create ions from large molecules with minimal fragmentation. Compared to the conventional methods, the MALDI-TOF is faster and more sensitive in detecting the infecting microorganism in endophthalmitis.[26]
PNA FISH is a technique whereby DNA probes labeled with fluorophores are attached to a target DNA for identification. The FISH technique has been used for over two decades for the detection of genetic disorders. This technique has shown promising application in the detection of fungi and infectious endophthalmitis.[27,28]
Antifungal drugs
Five families of antifungals are extensively used to treat human fungal infections, but only a handful of them are used to treat ocular fungal infection due to the lack of therapeutic concentration obtained in the ocular tissues. These are: (1) polyenes represented by amphotericin B; (2) azoles with several derivatives such as imidazole (miconazole, econazole, ketoconazole), and triazoles (itraconazole, fluconazole, voriconazole, posaconazole); (3) echinocandins (such as caspofungin, micafungin, anidulafungin); (4) flucytosine, a pyrimidine analogue; and (5) allylamines (such as terbinafine). The three general mechanisms of action for the antifungal agents are cell membrane disruption, cell division inhibition, and cell wall formation.[29] All these drugs inhibit the synthesis of or directly interact with ergosterol, which is the predominant component of the fungal cell membrane.
The antifungal agents are usually fungistatic in the concentrations used in clinical practice but are fungicidal in higher concentrations; some exhibit fungicidal action against selective fungi in a dose-dependent manner. Systemic therapy with antifungal agents is also known to cause systemic adverse effects. Therefore, intravitreal injection is the primary route of administration of these agents, often supplemented with systemic (more often) and topical application of antifungal agents[30] [Table 2].
Table 2.
Antifungal agents and routes of administration in endophthalmitis
| Class | Drug | Intravitreal in 0.1 ml | Topical | Systemic | Systemic Toxicity | Susceptible fungus | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Intravenous | Oral | ||||||
| Polyene | Amphotericin B | 5-10 µg | 1.5 mg/ml (0.15%) | 0.5-1.0mg/kg | x | Renal | Fusarium Aspergillus Mucor |
| Triazole | Fluconazole | - | - | - | 200-400 mg/day | GI | |
| Triazole | Itraconazole | - | - | 200-400 mg BID | - | Liver, GI | Aspergillus |
| Imidazole | Ketoconazole | - | - | 200-800 mg/day | - | Liver | |
| Polyene | Natamycin | - | 50 mg/ml * | - | - | - | Fusarium |
| Triazole | Voriconazole | 50-200 µg | - | 6 mg/kg BID | 200 mg twice/day | Liver | Fusarium Aspergillus |
| Echinocandins | Caspofungin | 50 µg | 5 mg/ml 0.5% | 70mg/m2/day loading and 50mg/m2/day maintenance | - | Liver | Candida Aspergillus |
*Commercially available; GI- gastrointestinal
The choice of antifungal agents for intravitreal therapy is currently confined to only two molecules: amphotericin B and voriconazole. Following the intravitreal injection, the half-life (t12) of amphotericin B in the vitreous of noninflamed phakic eyes is 8.9 days and in the aphakic vitrectomized eye 1.8 days. Yeasts and filamentous fungi are susceptible to amphotericin B, but many species of Aspergillus are resistant too. The half-life of voriconazole in vitreous of noninflamed phakic eyes is 2.5–6.5 h and in aphakic vitrectomized eyes is 2.5 h; it has broad-spectrum activity against molds and yeasts.[29,31] Bioavailability following systemic treatment is superior with voriconazole than amphotericin B. Voriconazole can be used in all three routes—intracameral, intravitreal, and oral.[32,33] It is most effective against many Candida, Aspergillus, and Cryptococcus species.
Echinocandins (such as caspofungin, micafungin, and anidulafungin) have antifungal activity against Candida and Aspergillus species.[34] They exhibit their antifungal activity by inhibiting D-glucan synthase, an enzyme specifically involved in fungal cell wall synthesis. Due to the target-specific activity, echinocandins could be an ideal antifungal therapy though there are reports of both successful and unsuccessful treatment of endophthalmitis after intravitreal caspofungin.[35,36]
Treatment
Two important interventions of proven efficacy in the treatment of fungal endophthalmitis are vitrectomy and intravitreal antifungal drugs. The variation of treatment protocol of fungal endophthalmitis from bacterial endophthalmitis is early vitrectomy, more than one-time intravitreal injections, and frequent use of systemic antifungal therapy.[37] In recalcitrant cases of post cataract surgery fungal endophthalmitis, the intraocular lens explantation along with the lens capsule could benefit.[38] The visual outcome of fungal endophthalmitis is poorer than bacterial endophthalmitis.
Achieving adequate concentrations of antifungal drugs in the infected tissues is crucial to the treatment success. In refractory disease, intravitreal antifungal antibiotics may be repeated after vitrectomy. Systemic voriconazole has good intraocular bioavailability and may need a long treatment course, 6–8 weeks.[39] Topical natamycin could be used in eyes with associated keratitis.
An analysis of 730 consecutive cases of fungal endophthalmitis collected from large tertiary eye care facilities across India (doi: 10.1016/j.oret.2021.09.006) showed that: Aspergillus species was the most common infecting microorganism across the causative events, time to symptoms was longest in postoperative endophthalmitis, less than half eyes had hypopyon at presentation, nearly every eye required vitreous surgery, and each eye required multiple intravitreal injections of antifungal agents. Additionally, there was a variable need for therapeutic keratoplasty. Despite treatment, at least a third of the eyes became blind, and up to 6% of eyes required evisceration.
Maximum benefits are derived from two interventions instituted together—intravitreal therapy with antifungal agents and vitrectomy.[37,40] Systemic therapy is required in many instances and, when begun with renal and liver function tests, it must be continued for 4–6 weeks. Based on the international committee of Intraocular Inflammation Society (IOIS) recommendation, the Bristol Eye Hospital has proposed systematic antifungals alone for mild vitritis and a combination of intravitreal antifungals and vitrectomy for moderate to severe vitritis.[41]
In clinical practice, three situations arise. Situation one: bacterial endophthalmitis is suspected, but vitreous culture grows fungus; in this situation, the treating physician switches to antifungal drugs with intravitreal and systemic therapy. If not performed before, it might also call for vitrectomy and possible additional vitreous surgery (vitreous lavage) if such was done earlier. Situation two: fungal infection is suspected primarily and treated with vitrectomy and antifungal drugs from the beginning. Third situation: infective endophthalmitis is suspected clinically, treated either as bacterial or fungal endophthalmitis, but the vitreous culture does not grow any organism.
SARS-CoV2 and Endophthalmitis
Endogenous endophthalmitis is not uncommon in hospitalized patients treated for SARS-CoV2 (COVID-19) viral infection. In our analysis of 24 consecutive patients (33 eyes), time to symptoms was an average of 15 (range 6–72) days after discharge from the designated hospitals; over 90% (n = 22) patients had multiple pre-COVID-19 systemic co-morbidities, and over 66% patients were admitted to the intensive care unit (ICU). The commonest systemic disease was diabetes mellitus (87.5%). At presentation, the mean presenting vision was <20/400, and over 69% had a complete vitreous abscess. Because of poor systemic conditions, definite endophthalmitis treatment (vitrectomy and intravitreal antifungal injection) was possible in 19 of 24 patients. Fourteen of 19 vitreous biopsies (73.68%) were microbiologically positive—11 (78.6%) fungi, 2 bacteria, and 1 virus. The systemic infection focus was identified in 11 of 21 patients and included 8 fungemia (5-Candida, 2-Aspergillus, 1-Mucor) and 3 bacteremia (2-Streptococcus pneumoniae, 1 Escherichia coli). Ophthalmic interventions included primary vitrectomy in 17 patients (22 eyes), repeat vitreous surgery in 5 patients (6 eyes) including silicone oil tamponade in 5 patients (6 eyes), multiple intravitreal anti-fungal drugs in 11 patients (14 eyes), and systemic antifungal drugs in all patients. Despite treatment, 47.4% of patients only regained vision better than 20/400, and five patients died during their treatment for endophthalmitis.
Three classes of drugs used to treat the patients with COVID-19 infection increase the risk of endogenous endophthalmitis. These drugs are systemic corticosteroids, broad-spectrum antibiotics, and IL-6 inhibitors (tocilizumab). Corticosteroids are known to cause immunosuppression and increase the risk of bacterial/fungal infection.[42] Broad-spectrum antibiotics kill the bacteria and allow growth and multiplication of the commensals, including the yeasts.[43] The IL-6 inhibitors (such as tocilizumab) impair the function of neutrophil, macrophage, and T cells, thus increasing the risk of fungal infection.[44] In our cohort (doi: 10.4103/ijo.IJO_1474_21) in South India, Candida sp. was the commonest isolated fungus in endogenous endophthalmitis in people with SARS-CoV2 infection; a similar trend is recently reported in five patients (seven eyes) from North India.[45]
Knowledge Gap
Antifungal susceptibility and resistance
Minimum inhibitory concentration (MIC) is the most common test used for antibiotic susceptibility. It is defined as the lowest concentration of an antimicrobial agent that prevents the visible growth of microorganisms. It is determined by E-test or microbroth dilution method as per the Clinical and Laboratory Standards Institute (CLSI) guidelines. MIC for antifungal agents is not routinely performed. In addition, colorimetric flow cytometry and ergosterol quantitation are available to measure the MIC of anti-fungal agents. Ergosterol is the major sterol component of the fungal cell membrane and is responsible for maintaining cell integrity and function. MIC breakpoints are available for amphotericin B, fluconazole, itraconazole, voriconazole, and flucytosine against Candida and some species of filamentous fungi.[46]
Similar to MIC is the minimum fungicidal concentration (MFC). MFC is defined as the lowest drug concentration that achieves ≥ 98%–99.9% killing of particular fungi. MFC correlates better with clinical outcomes. A comparative susceptibility of three common fungi tested at Miami, USA[47] and Hyderabad, India[48] against two commonly used antifungal drugs in ocular fungal infection is shown in Table 3.
Table 3.
Susceptibility of three common fungi to two common antifungal drugs
| Location | Fungal species | Antifungal drugs | |
|---|---|---|---|
|
| |||
| Amphotericin B µg/ml | Voriconazole µg/ml | ||
| Miami, USA*[47] | Candida; n=14 | 0.125-1.0 | 0.06-0.03 |
| Aspergillus; n=8 | 1.0-8.0 | 0.125-0.25 | |
| Fusarium; n=14 | 1.0-4.0 | 2.0-8.0 | |
| Hyderabad, India**[48] | Candida; n=12 | 0.047-0.125 | 0.032-1.0 |
*endophthalmitis; **keratitis
Antifungal resistance
Resistance to antifungal drugs is not uncommon. It occurs through a variety of mechanisms and includes (1) nonsynonymous point mutations within the gene encoding the target enzyme (leading to alteration in the amino acid sequence), (2) increased expression of the target enzyme through increased transcription of the gene encoding it, (3) decreased concentrations of the drug within the fungal cells due to drug efflux, and (4) changes in the biosynthetic pathway resulting in reduced production of the target of the antifungal agents.[49]
Biofilm and antifungal resistance
Biofilm is one of the major causes of resistance to various antibiotics.[50] Structurally, a biofilm is a slimy layer of an extracellular matrix made of polymeric substances produced by microorganisms. This forms an architectural colony providing resistance not just against antibiotics but also against the human immune system. The role of biofilm has been studied in various ocular conditions, both implants-associated (such as intraocular lens, scleral buckles, punctal plugs, and lacrimal intubation devices) and nonimplant-associated pathologies (such as keratitis, chronic dacryocystitis, and endophthalmitis).[51]
The potential to form biofilms has been demonstrated in some ocular fungi (such as Aspergillus fumigatus, Candida albicans, Fusarium solani, Cladosporium sphaaerospermum, and Acremonium implicatum).[52,53,54,55] Our group has reported one corneal isolate of C. albicans resistant to three antifungal drugs as a biofilm producer; the thickness of the biofilm, measured by scanning electron microscopy (SEM), increased from a monolayer/bilayer of cells at 24 h to a more than 7-cell thickness layer at 72 h. These cells were less sensitive, up to 200 × MIC of the antifungal agents than nonbiofilm cells.[56] Similar mechanisms may act in-vivo, resulting in poor outcomes in patients with infectious endophthalmitis.
Antifungal stewardship
Antimicrobial stewardship (AMS) is a coordinated program that promotes the appropriate use of antimicrobials, improves patient outcomes, reduces microbial resistance, decreases the spread of infections caused by multidrug-resistant organisms, and finally reduces the cost of care. AMS is defined as “the optimal selection, dosage, and duration of antimicrobial therapy that results in the best clinical outcome for the treatment or prevention of infection, with minimal toxicity to the patient and minimal impact on subsequent resistance.”[57] AMS is more relevant now as fewer new antimicrobials are introduced every year, and there is a need to conserve what we have without developing resistance to these drugs. Principally, there are three goals of AMS.[58] These are (1) right treatment (4Ds[59]—right Drug, right Dose, right Directed therapy, right Duration); (2) prevent antimicrobial overuse, misuse, and abuse; and (3) minimize the development of resistance.
Life-threatening fungal diseases such as invasive Aspergillus and Candida infections are associated with high mortality.[60,61] In addition, indiscriminate use of antifungal agents and widespread agricultural antifungal exposure have resulted in the spread of resistant fungal pathogens for one or more antifungal drugs. Antifungal stewardship (AFS) is responsible for the appropriate usage and conservation of antifungal drugs. The core principles of AFS are similar to AMS; the three principal concerns are: (1) the physicians have less opportunity to switch therapy because susceptibility tests are not done routinely; (2) there is a limited choice of antifungal drugs; (3) there is no well-defined endpoint.[62,63]
Inflammatory markers
Recent studies have evaluated the use of galactomannan (GM) and 1,3 b-D-glucan (BDG) biomarkers as ancillary tests to diagnose invasive fungal endophthalmitis using commercial ELISA Kits.
1,3-BDG is a major polysaccharide cell wall component in many fungal species, including Candida and Aspergillus sp. An elevated BDG level in the vitreous fluid of patients with endogenous fungal endophthalmitis has been reported.[64] It was also suggested that testing the BDG values in the vitreous fluid could be more sensitive than the culture methods for diagnosing fungal endophthalmitis. 1,3-BDG is also released into the bloodstream in invasive fungal diseases.[65] Hence, there could be additional values of measuring serum BDG level to monitor the disease progression and prognosis in endophthalmitis.[66,67]
GM is a cell wall component of mainly Aspergillus sp. And its detection via enzyme immunoassay is part of the diagnostic criteria for invasive aspergillosis. A recent report has explored its use in the diagnosis of A. fumigatus in the vitreous sample and recommended its assay when the standard mycology is negative and if pan fungal PCR is not available.[68]
Our data (unpublished) confirms significantly higher levels of vitreous GM in patients with culture-proven fungal infections than patients with noninfectious retinal disorders. The Area under the ROC curve (AUC) value for GM was 0.81 with a sensitivity of 0.88 and a specificity of 0.73 for a cut-off value of 51.36 pg/ml, and the AUC value for BDG was 0.93 (95% CI: 0.84–0.1) with sensitivity and specificity of 0.94 and 0.82, respectively, with the cut-off value of 1.19 pg/ml. Therefore, these tests could be considered in conjunction with clinical and microbiological tests. The added advantage is that the results of these tests are available within 2–3 h compared to several days of conventional culture.
Investigating culture-negative endophthalmitis
A common limitation of conventional microscopy and culture is culture-negativity. This is more of a possibility in a tertiary eye care setting, where the patients are often referred after receiving intravitreal and systemic antibiotics.[69] Additionally, the classic clinical characteristics could be masked due to delayed presentation. While direct sequencing and PCR of the ITS region can be applied on clinical specimens to detect the presence of microorganisms, low pathogen loads or polymicrobial infections are usually challenging to differentiate ambiguous signals from mixed chromatograms of samples, and the sequences often remain unidentified/misidentified.
Next-generation sequencing (NGS) is a novel platform that can simultaneously detect and independently sequence virtually all the DNA sequences of the infectious agents present in a sample.[70] A culture-free platform using targeted NGS of the ITS2 region would be ideal for overcoming the divide between conventional microbiological methods and whole-genome sequencing. The NGS is less complicated than whole genome sequencing and because it is also relatively less expensive could possibly be used in diagnostic laboratories.
Targeted NGS refers to a selective capture or amplification of specific genomic regions of interest before subjecting to massive parallel sequencing. Targeted NGS provides better sensitivity and specificity in addition to the ease of downstream analysis; it also lowers the cost by allowing more samples to be tested in one run.[71] We have shown that targeted NGS is a good tool for microbial research in culture-negative endophthalmitis, with a 71.9% rate of detection of fungal pathogens in culture-negative samples. Targeted NGS is also more efficient in detecting polymicrobial infection. The NGS could be the future diagnostic tool in routine ocular microbiological laboratories when the procedures and the bioinformatics are better standardized and validated. A reduced cost will bring additional benefits.
Real-world data and evidence
Real-World Data (RWD) are “data relating to patient health status and/or the delivery of health care collected routinely from various sources.” Real-World Evidence (RWE) is the “clinical evidence about the usage and potential benefits or risks of a medical product derived from analysis of RWD.”[72] Classically, randomized controlled trials (RCTs) are considered the gold standard for demonstrating the product or procedure efficacy for regulatory approval or to create evidence for clinical care. It provides much-needed information to both treating physicians and patients to make scientific judgments and informed choices. RCTs are always a good investment; it pays back the money spent and improves the quality of life.[73] The evidence generated from observational studies of RWD is often considered inferior because of nonrandomized treatment assignment and less rigorous data collection that could compromise internal validity. But, as personalized medicine becomes increasingly common, patient recruitment into RCTs would be affected, and sometimes it is not possible to include a control arm. Efforts are made to make the observational data collected through RWD address research questions where a traditional RCT may be unfeasible or unethical.
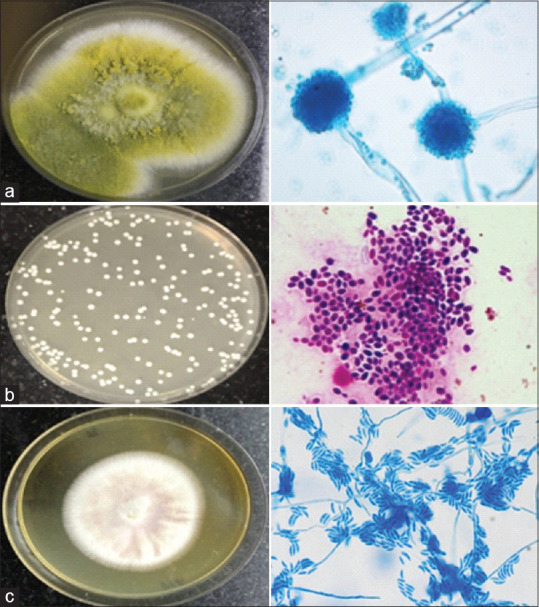
Target Trial is one such approach.[74] It closely emulates RCTs. It navigates through two steps: step 1-a causal question is asked (as is asked in RCT); step 2- the causal question is answered through a suitable RWD (instead of RCT)[75] [Fig. 5]. Target trial uses the RWD to answer the causal question to create evidence nearly similar to RCT. The most important one is to use RWD to design a fungal endophthalmitis management RCT as it is nearly impossible due to the worldwide paucity of cases, the time required to recruit an adequate number of patients, and the cost needed for such a study.
Figure 5.
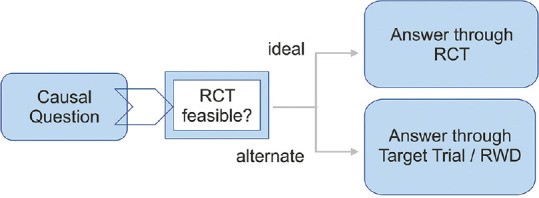
Building target trial from real-world data
RCTs and RWE generated from RWD are complementary, and each contributes valuable information about patient outcomes. Rigorously collected data is the key. Well-designed and conducted observational studies may offer valuable information that complements the evidence from clinical trials. Advances in statistical approaches to the causal estimation of treatment effects and experience using RWD and RWE may increase our confidence in observational studies of treatment effectiveness.[76]
An analysis of real-world data of 7 years (May 2014–April 2021) and 256 consecutive patients of culture-proven fungal endophthalmitis collected from our electronic medical record (EMR) has added few additional information as follows: (1) elderly age group (51–70 years) were more prone for fungal infection; (2) the age-specific principal events of fungal endophthalmitis were trauma in “younger” age up to 20 years, endogenous in the “mid-adult” age group 21–40 years, and postoperative infection in the “elderly” age group 71 and above; (3) keratitis progressed to fungal endophthalmitis in 12% to 18% instances.
Ocular surface, Mycobiome, and fungal endophthalmitis
The microbes on the ocular surface are one of the important sources of exogenous endophthalmitis. The current practice of topical 5% povidone-iodine application on the conjunctival surface aims to reduce the microbial load of the ocular surface.[77]
Many investigators have studied the ocular surface bacterial flora in health and disease. In general, more microorganisms reside on the lids than on the conjunctiva. A variation in ocular surface microbiota is expected between individuals and between people from different countries. The most common cultured microorganisms include coagulase-negative Staphylococci (S. epidermidis is most common) and Propionibacterium sp.; less common ones are Micrococcus sp. and Corynebacterium sp., and the least common are the gram-negative bacteria.[78] These bacteria cause endophthalmitis in conducive conditions.
The ocular surface fungi are not studied as much as the bacteria. Normally, fungi are not residents of the human eye but are acquired from the surrounding. Fungi usually colonize on the lid margins and conjunctiva. Aspergillus sp. is the most common fungal isolate from the conjunctiva of healthy individuals reported from India.[79] In healthy individuals, the conjunctival fungal flora has been determined using both conventional culture and culture-independent (NGS, using internal transcribed spacer 2, ITS2, sequencing as a proxy for fungi) methods.
Mycobiome refers to the diversity and abundance of fungal species in a niche. Our study (25 patients) in south India yielded 13.37 million high-quality reads (average 534,720/mycobiome); Ascomycota (mean abundance, 47.74%) and Basidiomycota (mean abundance, 26.87%) were the dominant phyla; and Aspergillus sp. (25 of 25, 100%), Fusarium sp. (21 of 25, 84%), and Candida sp. (17 of 25, 85%) were the dominant genera.[80] We also observed that the conjunctival fungal flora considerably varied with age but not with gender.
These resident conjunctival fungal flora could also cause exogenous fungal endophthalmitis similar to the resident bacterial flora. Conjunctival disinfection significantly impacts the occurrence of post cataract surgery endophthalmitis, and the contact kill time of currently used 5% povidone-iodine is less than 30 s for the common infecting fungi.[81]
Conclusion
Globally, over 300 million people are afflicted with a severe fungal infection, and 25 million are at high risk of dying or losing their sight. It is more frequent in South-East and South Asia.[82] Fungal keratitis is more frequent than other fungal infections of the eye, and there is no published data on the global incidence of fungal endophthalmitis. Assessment of the global burden and epidemiologic trends of fungal diseases is critical to prioritizing prevention strategies, diagnostic modalities, and therapeutic interventions. But quantifying the global burden of fungal diseases is challenging. Fungal diseases are often difficult to diagnose because they are not routinely suspected. The difficulty is further accentuated because fungi do not always grow in culture, histopathologic identification is challenging, and fungal antibody tests may cross-react.[83] In the absence of a global incidence report and randomized clinical trial, there is no universally accepted diagnosis and management protocol of fungal endophthalmitis. This opens new opportunities to test the new technologies managing this difficult disease. These new technologies include newer molecular techniques, next-generation sequencing, and real-world data. The world also needs newer antifungal drugs, avoid indiscriminate use of antibiotics, immunosuppressives, and antifungal stewardship.
Financial support and sponsorship
TD- Hyderabad Eye Research Foundation (2021).
Conflicts of interest
There are no conflicts of interest.
References
- 1. Van Burik JH, Magee PT. Aspects of fungal pathogenesis in humans. Annu Rev Microbiol. 2001;55:743–72. doi: 10.1146/annurev.micro.55.1.743. [DOI] [PubMed] [Google Scholar]
- 2. Romani L. Immunity to fungal infections. Nat Rev Immunol. 2011;11:275–88. doi: 10.1038/nri2939. [DOI] [PubMed] [Google Scholar]
- 3. Wüthrich M, Deepe G, Klein B. Adaptive immunity to fungi. Annu Rev Immunol. 2012;30:115–48. doi: 10.1146/annurev-immunol-020711-074958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kobayashi GS. Disease mechanism of fungi. Medical Microbiology. Chapter 74. 1996 [Google Scholar]
- 5. Gentile RC, Shukla S, Shah M, Ritterband DC, Engelbert M, Davis A, et al. Microbiological spectrum and antibiotic sensitivity in endophthalmitis:A 25-year review. Ophthalmology. 2014;121:1634–42. doi: 10.1016/j.ophtha.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 6. Schimel AM, Miller D, Flynn HW., Jr Endophthalmitis isolates and antibiotic susceptibilities:A 10-year review of culture-proven cases. Am J Ophthalmol. 2013;156:50–2. doi: 10.1016/j.ajo.2013.01.027. [DOI] [PubMed] [Google Scholar]
- 7. Sheng Y, Sun W, Gu Y, Lou J, Liu W. Endophthalmitis after cataract surgery in china, 1995-2009. J Cataract Refract Surg. 2011;37:1715–22. doi: 10.1016/j.jcrs.2011.06.019. [DOI] [PubMed] [Google Scholar]
- 8. Wong TY, Chee SP. The epidemiology of acute endophthalmitis after cataract surgery in an Asian population. Ophthalmology. 2004;111:699–705. doi: 10.1016/j.ophtha.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 9. Kunimoto DY, Das T, Sharma S, Jalai S, Majji AB, Gopinathan U, et al. Microbial spectrum and susceptibility of isolates. Part I. Post- operative endophthalmitis. Am J Ophthalmol. 1999;128:240–2. doi: 10.1016/s0002-9394(99)00112-9. [DOI] [PubMed] [Google Scholar]
- 10. Kunimoto DY, Das T, Sharma S, Jalai S, Majji AB, Gopinathan U, et al. Microbial spectrum and susceptibility of isolates. Part II. Post-traumatic endophthalmitis. Am J Ophthalmol. 1999;128:242–4. doi: 10.1016/s0002-9394(99)00113-0. [DOI] [PubMed] [Google Scholar]
- 11. Chee SP, Jap A. Endogenous endophthalmitis. Cur Opin Ophthalmol. 2001;12:464–70. doi: 10.1097/00055735-200112000-00012. [DOI] [PubMed] [Google Scholar]
- 12. Lingappan A, Wykoff CC, Albini TA, Miller D, Pathenagay A, Davis J, et al. Endogenous fungal endophthalmitis:Causative organisms management strategies and visual outcomes. Am J Ophthalmol. 2012;153:162–6. doi: 10.1016/j.ajo.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 13. Das T, Agarwal M, Behera U, Bhattacharjee B, Bhende M, Das AV, et al. Diagnosis and management of fungal endophthalmitis:India perspective. Expert Rev Ophthalmol. 2020;15:355–65. [Google Scholar]
- 14. Samiy N, D'Amico DJ. Endogenous fungal endophthalmitis. Int Ophthalmol Clin. 1996;36:147–62. doi: 10.1097/00004397-199603630-00014. [DOI] [PubMed] [Google Scholar]
- 15. Cullor J, Mannis MJ, Murphy CJ, Smith WL, Selsted ME, Raid T. In vitro antimicrobial activity of defensins against ocular pathogens. Arch Ophthalmol. 1990;108:861–4. doi: 10.1001/archopht.1990.01070080105044. [DOI] [PubMed] [Google Scholar]
- 16. Rao NA, Hidayat A. A comparative clinicopathologic study of endogenic mycotic endophthalmitis:Variations in clinical and histologic changes in candidiasis compared to aspergillosis. Am J Ophthalmol. 2001;132:244–5. doi: 10.1016/s0002-9394(01)00968-0. [DOI] [PubMed] [Google Scholar]
- 17. Dursun D, Fernandez V, Miller D, Alfonso EC. Advanced fusarium keratitis progressing to endophthalmitis. Cornea. 2003;22:300–3. doi: 10.1097/00003226-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 18. Vilela RC, Vilela L, Vilela P, Vilela R, Motta R, Pôssa AP, et al. Etiological agents of fungal endophthalmitis:Diagnosis and management. Int Ophthalmol. 2014;34:707–21. doi: 10.1007/s10792-013-9854-z. [DOI] [PubMed] [Google Scholar]
- 19. Durand ML. Bacterial and fungal endophthalmitis. Clin Microbiol Rev. 2017;30:597–613. doi: 10.1128/CMR.00113-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liu K, Fang F, Li H. Reliability of vitreous histological detection of pathogenic fungi in the diagnosis of fungal endophthalmitis. Eye (Lond) 2015;29:424–7. doi: 10.1038/eye.2014.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dave VP, Sharma S, Dave PJ, Joseph J, Pappuru RR. Clinical presentations, diagnostic dilemma and management outcomes of chronic postoperative endophthalmitis caused by Stephanoascus ciferrii. Retin Cases Brief Rep. 2021;15:269–74. doi: 10.1097/ICB.0000000000000782. [DOI] [PubMed] [Google Scholar]
- 22. Anand A, Madhavan H, Neelam V, Lily T. Use of polymerase chain reaction in the diagnosis of fungal endophthalmitis. Ophthalmology. 2001;108:326–30. doi: 10.1016/s0161-6420(00)00517-0. [DOI] [PubMed] [Google Scholar]
- 23. Okhravi N, Adamson P, Lightman S. Use of PCR in endophthalmitis. Ocul Immunol Inflamm. 2000;8:189–200. [PubMed] [Google Scholar]
- 24. Bagyalakshmi R, Therese LK, Madhavan HN. Application of semi-nested polymerase chain reaction targeting internal transcribed spacer region for rapid detection of pan fungal genome directly from ocular specimens. Indian J Ophthalmol. 2007;55:261–5. doi: 10.4103/0301-4738.33037. [DOI] [PubMed] [Google Scholar]
- 25. Ogawa M, Sugita S, Watanabe K, Shimizu N, Mochizuki M. Novel diagnosis of fungal endophthalmitis by broad-range real-time PCR detection of fungal 28S ribosomal DNA. Graefes Arch Clin Exp Ophthalmol. 2012;250:1877–83. doi: 10.1007/s00417-012-2015-7. [DOI] [PubMed] [Google Scholar]
- 26. Xu S, Zhou C, Zhang P, Fenf C, Zhang T, Sun Z, et al. Diagnostic performance of MALDI-TOF MS compared to conventional microbiological cultures in patients with suspected endophthalmitis. Ocul Immunol Inflamm. 2020;28:483–90. doi: 10.1080/09273948.2019.1583346. [DOI] [PubMed] [Google Scholar]
- 27. Patel N, Miller D, Relhan N, Flynn HW., Jr Peptide Nucleic Acid-Fluorescence in situ hybridization for detection of Staphylococci from endophthalmitis isolates:A proof-of-concept study. Invest Ophthalmol Vis Sci. 2017;58:4307–9. doi: 10.1167/iovs.17-21535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rigby S, Procop GW, Haase G, Wilson D, Hall G, Kurtzman C, et al. Fluorescence in situ hybridization with peptide nucleic acid probes for rapid identification of Candida albicans directly from blood culture bottles. J Clin Microbiol. 2002;40:2182–6. doi: 10.1128/JCM.40.6.2182-2186.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Myers RS.Antifungal agents. Immunizing and Antimicrobial Agents. 2006. [[Last accessed on 2021 Jun 02]]. Available from: http://www.courses.washington.edu .
- 30. Schere WJ, Lee K. Implication of early systemic therapy on the incidence of endogenous fungal endophthalmitis. Ophthalmology. 1997;104:1593–8. doi: 10.1016/s0161-6420(97)30091-8. [DOI] [PubMed] [Google Scholar]
- 31. Hegde MS, Pathengay A. Intravitreal antibiotics. Das T, editor. Endophthalmitis. Springer. 2018:239–51. [Google Scholar]
- 32. Chhablani J. Fungal endophthalmitis. Expert Rev Anti Infect Ther. 2011;9:1191–201. doi: 10.1586/eri.11.139. [DOI] [PubMed] [Google Scholar]
- 33. Hariprasad SM, Mieler WF, Lin TK, Sponsel WE, Graybill JR. Voriconazole in the treatment of fungal eye infections:A review of current literature. Br J Ophthalmol. 2008;92:871–8. doi: 10.1136/bjo.2007.136515. [DOI] [PubMed] [Google Scholar]
- 34. Khan FA, Slain D, Khakoo RA. Candida endophthalmitis:Focus on current and future antifungal treatment options. Pharmacotherapy. 2007;27:1711–21. doi: 10.1592/phco.27.12.1711. [DOI] [PubMed] [Google Scholar]
- 35. Gauthier GM, Nork TM, Prince R, Andes D. Subtherapeutic ocular penetration of caspofungin and associated treatment failure in Candida albicans endophthalmitis. Clin Infect Dis. 2005;41:e27–8. doi: 10.1086/431761. doi:10.1086/431761. [DOI] [PubMed] [Google Scholar]
- 36. Mora-Duarte J, Betts R, Rotstein C, Colombo AL, Thompson-Moya L, Smietana J. Comparison of caspofungin and amphotericin B for invasive candidiasis. N Engl J Med. 2002;347:2020–9. doi: 10.1056/NEJMoa021585. [DOI] [PubMed] [Google Scholar]
- 37. Behera UC, Budhwani M, Das T, Basu S, Padhi TR, Barik MR, et al. Role of early vitrectomy in the treatment of fungal endophthalmitis. Retina. 2018;38:1385–92. doi: 10.1097/IAE.0000000000001727. [DOI] [PubMed] [Google Scholar]
- 38. Dave VP, Pathengay A, Sharma S, Govindhari V, Karolia R, Pappuru RR, et al. Clinical presentations and comparative outcomes of primary versus deferred intraocular lens explantation in delayed-onset endophthalmitis. Indian J Ophthalmol. 2019;67:1101–4. doi: 10.4103/ijo.IJO_1494_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hariprasad SM, Mieler WF, Holz ER, Gao H, Kim JE, Chi J, et al. Determination of vitreous, aqueous, and plasma concentrations of orally administered voriconazole in humans. Arch Ophthalmol. 2004;122:42–7. doi: 10.1001/archopht.122.1.42. [DOI] [PubMed] [Google Scholar]
- 40. Kim DY, Moon HI, Joe SG, Kim JG, Yoon YH, Lee JY. Recent clinical manifestations and prognosis of fungal endophthalmitis:A 7-year experience at a tertiary referral center in Korea. J Korean Med Sci. 2015;30:960–4. doi: 10.3346/jkms.2015.30.7.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Narendran N, Balasubramaniam B, Johnson E, Johnson E, Dick A, Mayer E. Five-year retrospective review of guideline-based treatment of fungal endophthalmitis. Acta Ophthalmol. 2008;86:525–32. doi: 10.1111/j.1600-0420.2007.01097.x. [DOI] [PubMed] [Google Scholar]
- 42. Stuck AE, Minder CE, Frey FJ. Risk of infectious complications in patients taking glucocorticosteroids. Rev Infect Dis. 1989;11:954–63. doi: 10.1093/clinids/11.6.954. [DOI] [PubMed] [Google Scholar]
- 43. Gutierrez D, Weinstock A, Antharam VC, Gu H, Jasbi P, Shi X, et al. Antibiotic-induced gut metabolome and microbiome alterations increase the susceptibility to Candida albicans colonization in the gastrointestinal tract. FEMS Microbiol Ecol. 2020;96:fiz187. doi: 10.1093/femsec/fiz187. doi:10.1093/femsec/fiz187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Romani L, Mencacci A, Cenci E, Spaccapelo R, Toniatti C, Puccetti P, et al. Impaired neutrophil response and CD4+T helper cell 1 development in interleukin 6-deficient mice infected with Candida albicans. J Exp Med. 1996;183:1345–55. doi: 10.1084/jem.183.4.1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Shroff D, Narula R, Atri N, Chakravarti A, Gandhi A, Sapra N, et al. Endogenous fungal endophthalmitis following intensive corticosteroid therapy in severe COVID-19 disease. Indian J Ophthalmol. 2021;69:1909–14. doi: 10.4103/ijo.IJO_592_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Arikan S. Current status of antifungal susceptibility testing methods. Med Mycol. 2007;45:569–87. doi: 10.1080/13693780701436794. [DOI] [PubMed] [Google Scholar]
- 47. Silva RA, Sridhar J, Miller D, Wykoff CC, Flynn HW., Jr Exogenous fungal endophthalmitis:An analysis of isolates and susceptibilities to antifungal agents over a 20-year period (1990-2010) Am J Ophthalmol. 2015;159:257–64. doi: 10.1016/j.ajo.2014.10.027. [DOI] [PubMed] [Google Scholar]
- 48. Motukupally SR, Nanapur VR, Chathoth KN, Murthy SI, Pappuru RR, Mallick A, et al. Ocular infections caused by Candida species:Type of species, in vitro susceptibility and treatment outcome. Indian J Med Microbiol. 2015;33:538–46. doi: 10.4103/0255-0857.167331. [DOI] [PubMed] [Google Scholar]
- 49. Seyedmousavi S, Bosco S, De Hoog S, Ebel F, Elad D, Gomes RR, et al. Fungal infections in animals:A patchwork of different situations. Med Mycol. 2018;56((Supp 1)):165–87. doi: 10.1093/mmy/myx104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Costerton JW, Montanaro L, Arciola CR. Biofilm in implant infections:Its production and regulation. Int J Artif Organs. 2005;28:1062–8. doi: 10.1177/039139880502801103. [DOI] [PubMed] [Google Scholar]
- 51. Zegans ME, Becker HI, Budzik J, O'Toole G. The role of bacterial biofilms in ocular infections. DNA Cell Biol. 2002;21:415–20. doi: 10.1089/10445490260099700. [DOI] [PubMed] [Google Scholar]
- 52. Beauvais A, Schmidt C, Guadagnini S, Roux P, Perret E, Henry C, et al. An extracellular matrix glues together the aerial-grown hyphae of Aspergillus fumigatus. Cell Microbiol. 2007;9:1588–600. doi: 10.1111/j.1462-5822.2007.00895.x. [DOI] [PubMed] [Google Scholar]
- 53. M¨uller FM, Seidler M, Beauvais A. Aspergillus fumigatus biofilms in the clinical setting. Med Mycol. 2011;49((suppl 1)):S96–100. doi: 10.3109/13693786.2010.502190. [DOI] [PubMed] [Google Scholar]
- 54. Venkatesan N, Perumal G, Doble M. Bacterial resistance in biofilm-associated bacteria. Future Microbiol. 2015;10:1743–50. doi: 10.2217/fmb.15.69. [DOI] [PubMed] [Google Scholar]
- 55. Zhang X, Sun X, Wang Z, Zhang Y, Hou W. Keratitis-associated fungi form biofilms with reduced antifungal drug susceptibility. Invest Ophthalmol Vis Sci. 2012;53:7774–8. doi: 10.1167/iovs.12-10810. [DOI] [PubMed] [Google Scholar]
- 56. Konduri R, Chakravarthy SK, Adicherla H, Sharma S, Shivaji S. Temporal expression of genes in biofilm-forming ocular Candida albicans isolated from patients with keratitis and orbital cellulitis. Invest Ophthalmol Vis Sci. 2018;59:528–38. doi: 10.1167/iovs.17-22933. [DOI] [PubMed] [Google Scholar]
- 57. Gerding DN. The search for good antimicrobial stewardship. Jt Comm J Qual Improv. 2001;27:403–4. doi: 10.1016/s1070-3241(01)27034-5. [DOI] [PubMed] [Google Scholar]
- 58. Doron S, Davidson LE. Antimicrobial stewardship. Mayo Clin Proc. 2011;86:1113–23. doi: 10.4065/mcp.2011.0358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Joseph J, Rodvold KA. The role of carbapenems in the treatment of severe nosocomial respiratory tract infections. Expert Opin Pharmacother. 2008;9:561–75. doi: 10.1517/14656566.9.4.561. [DOI] [PubMed] [Google Scholar]
- 60. Bongomin F, Gago S, Oladele RO, Denning DW. Global and multi-national prevalence of fungal diseases –Estimate precision. J Fungi (Basel) 2017;3:57. doi: 10.3390/jof3040057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, White TC. Hidden Killers:Human fungal infections. Sci Transl Med. 2012;4:165rv13. doi: 10.1126/scitranslmed.3004404. doi:10.1126/scitranslmed. 3004404. [DOI] [PubMed] [Google Scholar]
- 62. Johnson MD, Lewis RE, Dodds-Ashley ES, Ostrosky-Zeichner L, Zaoutis T, Thompson GR, et al. Core Recommendations for antifungal stewardship:A statement of the Mycoses Study Group Education and Research Consortium. J Infect Dis. 2020;222((Suppl 3)):S175–98. doi: 10.1093/infdis/jiaa394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Muñoz P, Valerio M, Vena A, Bouza E. Antifungal stewardship in daily practice and health economic implications. Mycoses. 2015;58((Suppl 2)):14–25. doi: 10.1111/myc.12329. [DOI] [PubMed] [Google Scholar]
- 64. Theel ES, Doern CD. Beta-D-glucan testing is important for diagnosis of invasive fungal infections. J Clin Microbiol. 2013;51:3478–83. doi: 10.1128/JCM.01737-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Shimbo M, Ito N, Kadonosono K. [Investigation of beta-D-glucan values in the vitreous] Nippon Ganka Gakkai Zasshi. 2002;106:579–82. [Japanese] [PubMed] [Google Scholar]
- 66. Alam FF, Mustafa AS, Khan ZU. Comparative evaluation of (1, 3)-beta-D-glucan, mannan and anti-mannan antibodies, and Candida species-specific snPCR in patients with candidemia. BMC Infect Dis. 2007;7:103. doi: 10.1186/1471-2334-7-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Chen L, Tao Y, Hu X. Utility of intraocular fluid beta-D-glucan testing in fungal endophthalmitis:A series of 5 cases. Am J Case Rep. 2020;21:e921188. doi: 10.12659/AJCR.921188. doi:10.12659/AJCR.921188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Dupont D, Saison J, Mialhes P, Mouchel R, Wallon M, Persat F. Aspergillus endophthalmitis:Potential role for vitreous galactomannan testing? Int J Infect Dis. 2020;96:151–3. doi: 10.1016/j.ijid.2020.04.037. [DOI] [PubMed] [Google Scholar]
- 69. Joseph J, Sontam B, Madhuri G, Sharma S, Tyagi M, Dave V, et al. Trends in microbiological spectrum of endophthalmitis in India:A review of 25 years. Eye (Lond) 2019;33:1990–5. doi: 10.1038/s41433-019-0380-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Gandhi J, Jayasudha R, Naik P, Sharma S, Dave VP, Joseph J. Targeted high-throughput sequencing identifies predominantly fungal pathogens in patients with clinically infectious, culture-negative endophthalmitis in South India. Microorganisms. 2019;7:411. doi: 10.3390/microorganisms7100411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Deshmukh D, Joseph J, Chakrabarti M, Sharma S, Jayasudha R, Sama KC, et al. New insights into culture negative endophthalmitis by unbiased next generation sequencing. Sci Rep. 2019;9:844. doi: 10.1038/s41598-018-37502-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Framework for FDA's real-world evidence program. [[Last accessed on 2021 May 30]]. Available from://www.fda.gov .
- 73. Kupfer C. The expanded role of randomized clinical trials. Am J Ophthalmol. 1996;122:883–5. doi: 10.1016/s0002-9394(14)70386-1. [DOI] [PubMed] [Google Scholar]
- 74. Ramagopalan SV, Simpson A, Sammon C. Can real-world data really replace randomised clinical trials? BMC Med. 2020;18:13. doi: 10.1186/s12916-019-1481-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Head to head comparisons using real world data. [[Last accessed on 2021 Jun 02]]. Available from: http://www.cytel.com .
- 76. Sheffield KM, Dreyer NA, Murray JF, Faries DE, Klopchin MN. Replication of randomized clinical trial results using real-world data:Paving the way for effectiveness decisions. J Comp Eff Res. 2020;9:1043–50. doi: 10.2217/cer-2020-0161. [DOI] [PubMed] [Google Scholar]
- 77. Speaker MG, Menikoff JA. Prophylaxis of endophthalmitis with topical povidone-iodine. Ophthalmology. 1991;98:1769–75. doi: 10.1016/s0161-6420(91)32052-9. [DOI] [PubMed] [Google Scholar]
- 78. Willcox MD. Characterization of the normal microbiota of the ocular surface. Exp Eye Res. 2013;117:99–105. doi: 10.1016/j.exer.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 79. Sharma S. Diagnosis of fungal keratitis:Current options. Expert Opin Med Diagn. 2012;6:449–55. doi: 10.1517/17530059.2012.679656. [DOI] [PubMed] [Google Scholar]
- 80. Shivaji S, Jayasudha R, Sai Prashanthi G, Kalyana Chakravarthy S, Sharma S. The human ocular surface fungal microbiome. Invest Ophthalmol Vis Sci. 2019;60:451–9. doi: 10.1167/iovs.18-26076. [DOI] [PubMed] [Google Scholar]
- 81. Wu PC, Li M, Chang SJ, Teng MC, Yow SG, Shin SJ, et al. Risk of endophthalmitis after cataract surgery using different protocols for povidone- iodine preoperative disinfection. J Ocul Pharmacol Ther. 2006;22:54–61. doi: 10.1089/jop.2006.22.54. [DOI] [PubMed] [Google Scholar]
- 82.Fungal disease frequency- Global action fund. [[Last accessed on 2021 Jun 21]]. Available from: http://www.gaffi.org>why>fungal-disease-frequency .
- 83. Vallabhaneni S, Mody RK, Walker T, Chiller T. The global burden of fungal diseases. Infect Dis Clin North Am. 2016;30:1–11. doi: 10.1016/j.idc.2015.10.004. [DOI] [PubMed] [Google Scholar]


