Abstract
Purpose:
To compare the postoperative uncorrected distance visual acuity (UDVA) and refractive outcomes of cataract patients with astigmatism following implantation of Eyecryl™ and Tecnis® toric intraocular lenses (IOLs).
Methods:
We conducted a single-center, retrospective study including patients who had undergone phacoemulsification and implantation with either Eyecryl™ toric (Group 1) or Tecnis® toric (Group 2) IOL. The primary outcome measures included postoperative UDVA and residual astigmatism at 3 months. The secondary outcome measure was IOL misalignment >10° throughout the follow-up period.
Results:
One hundred and eight eyes of 76 patients (44 males and 32 females) were analyzed. Twenty-nine patients (38 eyes) received Eyecryl™ toric IOL (Group 1), and 47 patients (70 eyes) received Tecnis® toric IOL (Group 2). Groups 1 and 2 showed a mean postoperative logMAR UDVA of 0.09 ± 0.11 and 0.06 ± 0.09, respectively, at 3 months (P = 0.114). In both groups, all the eyes achieved a postoperative UDVA of ≤0.3 logMAR. The postoperative residual astigmatism of group 1 and group 2 was -0.29 ± 0.34 D and -0.16 ± 0.27 D, respectively (P = 0.038). Postoperative astigmatism was within ± 1.00 D in all the eyes. No eyes had an IOL misalignment >10° throughout the follow-up period.
Conclusion:
Both Eyecryl™ and Tecnis® toric IOLs provided significant improvement in uncorrected visual acuity and astigmatism correction postoperatively. The Tecnis® toric IOL provided statistically significant lower residual astigmatism than Eyecryl™toric IOL. However, the difference in postoperative astigmatism between the two IOLs was clinically insignificant.
Keywords: Astigmatism, cataract, Eyecryl toric, Tecnis toric, Toric IOL
Present-day cataract surgery has become a refractive procedure, and astigmatism management became an essential part of cataract surgery. Around 33% of the patients undergoing cataract surgery have preoperative corneal astigmatism of ≥1 diopter (D), with 22% having >1.5 D of astigmatism and 8% having >2.0 D of astigmatism.[1,2,3] Therefore, visual improvement is insufficient solely with a spherical intraocular lens (IOL), and patients may require spectacles, peripheral corneal relaxing incisions, or additional corneal refractive procedures, such as photorefractive keratectomy or laser in situ keratomileusis, to attain optimum visual acuity.[1] However, peripheral corneal relaxing incisions have many drawbacks, such as lack of accuracy, restricted astigmatism correction, overcorrection, regression, wound gape, and varied healing responses.[4] Furthermore, latent complications of corneal refractive procedures include dry eye, regression, undercorrection, overcorrection, and keratitis.[5]
Shimizu et al.[6] first introduced toric IOLs in the early 1990s as three-piece nonfoldable polymethyl methacrylate implants, which can be inserted through a 5.7 mm incision. Since then, implantation of toric IOLs is the most effective noninvasive procedure in correcting corneal astigmatism and decreasing postoperative spectacle dependence due to their increased predictability and safety.[7,8,9,10] Nevertheless, inaccurate or varying preoperative keratometry, inappropriate evaluation of total astigmatism, unexpected surgically induced astigmatism, errors of IOL axis position marking, or IOL instability could reduce the corrective effect of toric IOL.[11,12,13,14,15,16,17] Though the first models of toric IOL had high incidences of postoperative rotation, advances in the material and design of IOLs have resulted in improved rotational stability and precise functional outcomes.[10,18,19]
Among the different types of toric IOLs, Tecnis® and Eyecryl™ toric IOLs are the most frequently used in our hospital. The purpose of the present study was to compare the postoperative uncorrected distance visual acuity (UDVA) and refractive outcomes of cataract patients with corneal astigmatism following implantation of two types of toric IOLs and to provide a clinical basis for selecting an appropriate toric IOL.
Methods
This single-center, multisurgeon, retrospective study analyzed the data of patients who had undergone phacoemulsification and implantation with one of two toric IOLs: Tecnis® toric (Johnson and Johnson, New Brunswick, NJ) and Eyecryl™ toric (Biotech Vision Care Pvt Ltd, India), between January 2020 and January 2021. The study was performed in accordance with the principles of the Declaration of Helsinki. Institutional review board approval was obtained prior to study commencement. The confidentiality of patients was maintained throughout at all stages of the data analysis.
Study population
Subjects were divided into two groups: those who had undergone phacoemulsification with implantation of Eyecryl™ toric IOL (Biotech Vision Care Pvt Ltd, India) were included in group 1, and those with implantation of Tecnis® toric IOL (Johnson and Johnson, New Brunswick, NJ) were included in group 2. The characteristics of the two types of toric IOLs are shown in Table 1. Patients with less than 3 months follow-up, history of corneal or retinal or optic nerve pathologies, irregular corneal astigmatism, previous corneal procedures, amblyopia, and intraoperative or postoperative complications not related to the IOL design that may have impaired visual outcomes were excluded.
Table 1.
Characteristics of Eyecryl™ and Tecnis® toric IOLs
| Characteristic | Eyecryl™ toric IOL model HFY | Tecnis® toric IOL model ZCT |
|---|---|---|
| Material | Hydrophobic acrylic containing natural chromophore | Hydrophobic acrylic UV-blocking |
| Optic type | Biconvex, anterior toric aspheric surface | Biconvex, anterior toric aspheric surface |
| Optic diameter (mm) | 6.0 | 6.0 |
| Overall diameter (mm) | 13.0 | 13.0 |
| Anterior chamber depth (mm) | 5.28 | 5.72 |
| Refractive index | 1.48 | 1.47 |
| A-constant | 118.7 (optical SRK/T) | 119.3 (optical SRK/T) |
| 118.3 (ultrasound SRK/T) | 118.8 (ultrasound SRK/T) | |
| Spherical power range (D) | +10.0-+30.0 (with 0.50 steps) | +5.0-+34.0 (with 0.50 steps) |
| Cylinder power range (D) | 1.0-6.0 (with 0.50*/0.75 steps) | 1.5-6.0 (with 0.50 steps) |
IOL: Intraocular lens, UV: Ultraviolet, SRK/T: Sanders-Retzlaff-Kraff/Theoretical, D: Diopters. *from 1.0 to 1.50
Data collection
Demographic data collected from the records of the patients included age, gender, and type of IOL used with IOL power. Preoperative clinical data included UDVA (using Snellen’s chart) and corneal astigmatism measured by optical biometer (Tomey OA-2000, Japan). Postoperative data included UDVA, residual astigmatism, and any IOL misalignment >10° throughout the follow-up period (1 week, 1 month, and 3 months).
IOL power and axis calculation
Sanders-Retzlaff-Kraff/Theoretical formula was used for IOL power calculation. The postoperative target refraction for all eyes was emmetropia with both types of IOL. The IOL cylinder power and axis placement were calculated using online calculators from the respective IOL manufacturers. The Eyecryl™ toric calculator (www.biotechcalculators.com) was used with an A-constant of 118.7 for the Eyecryl™ toric IOL. The Tecnis® toric calculator (www.tecnistoriccalc.com) was used with an A-constant of 119.3 for the Tecnis® toric IOL.
Surgical procedure and marking technique
The surgeon marked the corneal limbus of the operative eye as reference markings (3 0’ clock and 9 o’ clock positions) using a slit lamp and a marking pen, with the patient sitting erect with a straight-ahead gaze while marking the axis to avoid cyclotorsion and inadvertent errors. The reference marks were aligned with the degree gauge of the fixation ring intraoperatively. The incision and the intended axis of the lens were marked with a surgical skin marker. The surgical technique included a 2.8 mm incision in the temporal or steepest meridian, a capsulorhexis diameter of approximately 5.0 mm, hydrodissection, phacoemulsification, irrigation and aspiration of cortical matter, and IOL implantation in the capsular bag. The toric IOL was then rotated until the axis indentations of the IOL were aligned with the axis marking of the patient. The viscoelastic substance was completely removed to avoid further rotation of the IOL. The IOL was centered along the coaxially sighted corneal light reflex, as represented by the first Purkinje image when the patient was fixating on the microscope light. The side ports and main incision were hydrated and Moxifloxacin 0.5% was injected intracamerally. All patients received topical antibiotics, corticosteroids, and nonsteroidal antiinflammatory drugs postoperatively.
Outcome measures
The primary outcome measures included the postoperative UDVA and residual astigmatism at 3 months. The secondary outcome measure was misalignment of the toric IOL >10° throughout the follow-up period. The UDVA measured by Snellen’s visual acuity chart was converted to logarithm of the minimal angle of resolution (logMAR) scale for statistical analysis. The axis of implanted toric IOL was assessed postoperatively with fully dilated pupil at the slit lamp using a rotating slit and rotational gauge.
Statistical analysis
Statistical analysis was performed on the Statistical Package for Social Sciences version 24.0 for Windows. Data were summarized by the mean and standard deviation. Categorical variables were presented as frequency and percentage. The normality of data was tested by the Kolmogorov–Smirnov test. The Student’s t-test was applied for normally distributed values, and the Mann–Whitney U test was performed for nonnormally distributed values to evaluate the differences between the two groups. The Chi-square test was used for comparisons of categorical variables. A probability (P) value less than 0.05 is considered as significant at 95% confidence level.
Results
One hundred and eight eyes of 76 patients (44 males and 32 females) were included in this study. The demographic characteristics and preoperative clinical data of the study population are shown in Table 2. Among the 76 patients (108 eyes) included in the present study, 29 patients (38 eyes) received the Eyecryl™ toric IOL (Group 1) and 47 patients (70 eyes) received the Tecnis® toric IOL (Group 2). No significant difference in the preoperative clinical parameters was noted between the two groups.
Table 2.
Comparison of demographic characteristics and preoperative clinical data of the study population between the two groups
| Parameter | Eyecryl™ toric IOL (Group 1) (n=38) | Tecnis® toric IOL (Group 2) (n=70) | P |
|---|---|---|---|
| Age (years)* | 0.090 | ||
| Mean±SD | 66.3±8.7 | 62.5±12.0 | |
| Gender (n)† | 0.017§ | ||
| Male | 13 | 31 | |
| Female | 16 | 16 | |
| Type of astigmatism (n)† | |||
| With-the-rule | 8 (21%) | 21 (30%) | 0.435 |
| Against-the-rule | 26 (68%) | 39 (56%) | |
| Oblique | 4 (11%) | 10 (14%) | |
| UDVA (logMAR)‡ | 0.478 | ||
| Mean±SD | 0.70±0.25 | 0.73±0.26 | |
| Median (IQR) | 0.6 (0.5 to 1) | 0.8 (0.5 to 1) | |
| Corneal astigmatism (D)‡ | 0.552 | ||
| Mean±SD | - 2.03±0.77 | - 1.94±0.64 | |
| Median (IQR) | - 2.0 (-2.5 to -1.5) | - 2.0 (-2.25--1.5) | |
| IOL spherical power (D)‡ | |||
| Mean±SD | 20.76±3.32 | 20.94±2.35 | 0.533 |
SD: Standard deviation, UDVA: Uncorrected distance visual acuity, logMAR: Logarithm of the minimum angle of resolution, IQR: Interquartile range, D: Diopters, IOL: Intraocular lens, *Student’s t-test, †Chi-square test, ‡Mann-Whitney U test, §Significant
Visual acuity
Group 1 showed significant improvement in mean UDVA from 0.70 ± 0.25 logMAR preoperatively to 0.09 ± 0.11 logMAR at 3 months follow-up. Similarly, in group 2, the mean preoperative logMAR UDVA improved from 0.73 ± 0.26 to 0.06 ± 0.09 postoperatively at 3 months. There was no significant difference between the two groups in postoperative UDVA (P = 0.114). In both groups, all the eyes achieved a postoperative UDVA of ≤ 0.3 logMAR. In group 1, 22 (57.9%) eyes had a UDVA of 0 logMAR, 13 (34.2%) eyes had a UDVA of 0.2 logMAR, and 3 (7.9%) eyes had a UDVA of 0.3 logMAR at 3 months. In group 2, 50 (71.4%) eyes had a UDVA of 0 logMAR, 19 (27.1%) eyes had a UDVA of 0.2 logMAR, and 1 (1.4%) eye had a UDVA of 0.3 logMAR at 3 months follow-up.
Astigmatism
The postoperative residual astigmatism of group 1 and group 2 was -0.29 ± 0.34 D and -0.16 ± 0.27 D, respectively. There was a statistically significant difference between the two groups, with group 2 showing more reduction of astigmatism postoperatively (P = 0.038). Postoperative residual astigmatism was within ±0.50 D in 32 eyes (84.2%) in group 1 and 64 eyes (91.4%) in group 2, and within ±1.00 D in all the eyes [Fig. 1].
Figure 1.
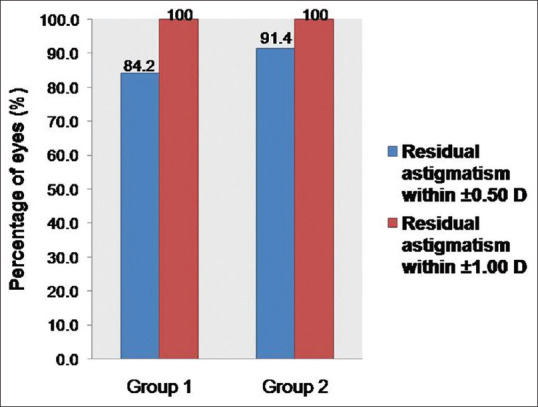
Percentage of eyes with postoperative astigmatism within ±0.50 and ±1.00 D in both groups
Table 3 shows the comparison of mean postoperative UDVA and residual astigmatism between the two groups at 3 months. No eyes had an IOL misalignment >10° throughout the follow-up period, and no resurgery or rerotation was needed in both the groups.
Table 3.
Comparison of primary outcome measures between the two groups at 3 months follow-up
| Outcome measures | Eyecryl™ toric IOL (Group 1) (n=38) | Tecnis® toric IOL (Group 2) (n=70) | P |
|---|---|---|---|
| UDVA (logMAR) | 0.114 | ||
| Mean±SD | 0.09±0.11 | 0.06±0.09 | |
| Median (IQR) | 0 (0 to 0.2) | 0 (0 to 0.2) | |
| Residual astigmatism (D) | 0.038* | ||
| Mean±SD | - 0.29±0.34 | -0.16±0.27 | |
| Median (IQR) | 0 (-0.5-0) | 0 (-0.5-0) |
UDVA: Uncorrected distance visual acuity, logMAR: Logarithm of the minimum angle of resolution, SD: Standard deviation, IQR: Interquartile range, D: Diopters, IOL: Intraocular lens, *Significant (P<0.05), Mann-Whitney U test
Discussion
The present study showed that patients with mild to high corneal astigmatism who had undergone phacoemulsification with Eyecryl™, and Tecnis® toric IOLs achieved desirable visual outcomes and astigmatism correction. Previous studies have reported the functional and anatomical outcomes of different types of toric IOLs, including Tecnis® toric IOL.[1,8,10,18,19,20,21,22,23,24,25,26,27,28,29,30,32] However, this is one of the first studies to analyze the outcomes of Indian-made Eyecryl™ toric IOL and compare it with an already established global toric IOL in the real-world setting.
No statistically significant difference was observed between the two toric IOLs in postoperative UDVA. The Eyecryl™ and Tecnis® toric groups showed a mean postoperative logMAR UDVA of 0.09 ± 0.11 and 0.06 ± 0.09, respectively, at 3 months. These results are consistent with those previously reported for several monofocal toric IOLs, including Tecnis® toric, AcrySof toric, Precizon toric, AT TORBI, and T-flex.[1,8,10,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32] Studies involving Tecnis® toric IOL showed a mean postoperative logMAR UDVA ranging from 0.02 to 0.36.[8,18,23,27,28,29,30,31] The Eyecryl™ toric group observed a UDVA of 20/20 in 57.9%, and the Tecnis® toric group noted a UDVA of 20/20 in 71.4% eyes at 3 months follow-up. Though there is no statistically significant difference, most of the patients who had undergone Tecnis® toric IOL implantation achieved more spectacle independence than those who had Eyecryl™ toric implanted.
Patients in both Tecnis® and Eyecryl™ groups achieved a significant reduction of astigmatism after surgery. The mean difference in postoperative residual astigmatism between the Tecnis® and Eyecryl™ groups was -0.13 D, which was statistically significant (P = 0.038). However, this minor difference in residual astigmatism may not be clinically significant. In both the groups, six eyes had postoperative astigmatism >0.50 D. Nevertheless, all the eyes had residual astigmatism within ± 1.00 D. This is in comparison with the outcomes of other studies involving monofocal toric IOLs such as Tecnis® toric, AcrySof toric, Precizon toric, and AT TORBI.[1,8,10,18,20,21,22,23,24,25,26,27,28,29,30,31] Different studies of Tecnis® toric IOL showed mean postoperative astigmatism ranging between -0.32 and -1.42 D, which is comparatively higher than the residual astigmatism of -0.16 D obtained in the present study.[8,18,23,27,28,29,30,31] This difference in astigmatism could be to variation in the demographic characteristics of the patients between the studies.
Studies have shown that including posterior corneal astigmatism while calculating total corneal astigmatism helps to avoid errors in IOL power calculation. The posterior cornea acts as a minus lens, and the astigmatism is generally against-the-rule and constant over time.[13,33] Depending solely on the anterior corneal curvature measurements could result in residual astigmatism after toric IOL implantation, overcorrecting by a factor of 1.38 in eyes having with-the-rule astigmatism and under correcting by a factor of 0.65 in the eyes with against-the-rule astigmatism.[33] In our study, we have used toric IOL online calculators provided by the respective manufacturers for cylinder power and axis calculation. The Tecnis® toric calculator incorporates the anterior chamber depth based on the axial length and keratometry values and includes the posterior corneal astigmatism for IOL power calculation. However, the Eyecryl™ toric calculator does not include posterior corneal astigmatism. This could be one reason for better refractive outcomes with Tecnis® toric IOL compared to Eyecryl™ toric IOL in the present study. Nevertheless, the Barrett toric calculator, which incorporates the effective lens position and the posterior corneal astigmatism, is found to have better predictability than the other calculators and nomograms.[34,35]
Different methods have been described to place the axis marks, including manual techniques, image-guided systems, intraoperative aberrometry, and iris-detection methods.[36] Variation in the accuracy of corneal axis marking has been shown between different marking methods.[37] In a study by Mayer et al.,[38] better IOL alignment and lower deviation from the target induced astigmatism was observed in the image-guided CALLISTO Eye group than the manual marking group. They also found the preoperative procedure and IOL alignment to be faster in the image-guided group. Intraoperative aberrometry-based methods are two times more likely to have ≤0.50 D residual astigmatism compared with other conventional marking methods.[39] However, the high costs of these devices limit their use. In our study, the preoperative manual marking method was used using a rotational thin slit beam and marking pen for all patients. As the same marking technique was used in both toric IOL groups, this might not have affected the outcomes. However, an intersurgeon variability may exist in the accuracy and reproducibility of manual corneal axis markings.
In the present study, postoperative IOL rotation of >10° did not occur in any of the eyes throughout the follow-up period. Other studies with Tecnis® toric IOL implanted cases also showed an IOL misalignment of >10° in only 0–3% of eyes.[8,18,23,27,28,29,30,31] Different studies, including AcrySof toric and Precizon toric, found a postoperative IOL rotation of >10° in 0–7% of eyes and maximum rotation occurred within the initial 10 days in the postoperative period in patients with high axial length.[18,20,21,22,23,24,25,26] Other monofocal toric IOLs such as AT TORBI and T-flex toric IOLs showed a misalignment >10° in 0–5 and 0–9% eyes, respectively.[10,19,20,32]
The rotational stability of the IOL differs with design and material, and better stability has been observed with hydrophobic acrylic lenses. The development of strong adhesions between the IOL and lens capsule in the early postoperative period leads to greater rotational stability. Early IOL rotation can be caused by retained OVDs, large capsular bag, small diameter of the haptic, and high axial length. The axis of IOL implantation is also associated with postoperative rotation, and a greater incidence of IOL rotation has been observed in with-rule-astigmatism cases with a vertical axis of IOL implantation. Capsulorhexis extension or fibrosis can also cause postoperative rotation.[36] IOL rotation <10° usually does not warrant any resurgery, as in our study.
Haripriya et al.,[40] in their study, assessed the rotational stability and the repositioning rates of Indian-made Auroflex hydrophilic acrylic toric IOL with AcrySof hydrophobic acrylic toric IOL. They found a surgical repositioning rate of 2.5 and 1.9% with Auroflex and AcrySof toric IOLs, respectively. However, the difference was no statistically significant. They attributed the higher rate of IOL repositioning to younger age, higher presurgical astigmatism, and with-the-rule astigmatism.
The provision of customized IOLs to correct high astigmatism, the low cost compared to the imported IOLs, and the reasonable effective functional and anatomical outcomes make Eyecryl™ toric IOL a good cost-effective alternative for those patients with cataract and astigmatism who want spectacle independence and cannot afford the imported IOLs.
The major limitation of the study is its retrospective design. Also, the clinical data were collected from patients who underwent phacoemulsification with toric IOL implantation by different surgeons at the hospital. Moreover, vector analysis of residual astigmatism to evaluate changes in refractive astigmatism was not performed, and the mean deviation of IOL from the target position was not assessed. A questionnaire on subjective visual quality, including spectacle independence, postoperative optical, or visual disturbances to evaluate the patient satisfaction, would have given more significant results. Prospective, randomized controlled trials with longer follow-up are needed, which can provide more valuable information. Despite the limitations, our study is one of the first studies to assess the outcomes of Eyecryl™ toric IOL, and certain conclusions may be drawn based on the analysis of the available real-world data.
Conclusion
Patients with cataract and mild to high corneal astigmatism achieved significant improvement in uncorrected visual acuity and astigmatism reduction following Eyecryl™ and Tecnis® toric IOL implantation. The Tecnis® toric IOL provided statistically significant lower postoperative astigmatism than Eyecryl™ toric IOL. However, the difference in residual astigmatism between the two IOLs was clinically insignificant. Thus, the decision to select one IOL over the other may depend on patient and surgeon preferences rather than merely visual acuity and refractive outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors thank Dr. Jagadeesh Kumar Reddy, Dr. Prabhu Shankar M, Dr. Siddharthan KS, Dr. Geetha G, and Dr. Rajesh Prabu (Sankara Eye Hospital, Coimbatore, Tamil Nadu, India) for their patient data contribution.
References
- 1. Holland E, Lane S, Horn JD, Ernest P, Arleo R, Miller KM. The AcrySof toric intraocular lens in subjects with cataracts and corneal astigmatism;a randomized, subject-masked, parallelgroup, 1-year study. Ophthalmology. 2010;117:2104–11. doi: 10.1016/j.ophtha.2010.07.033. [DOI] [PubMed] [Google Scholar]
- 2. Hoffmann PC, Hütz WW. Analysis of biometry and prevalence data for corneal astigmatism in 23,239 eyes. J Cataract Refract Surg. 2010;36:1479–85. doi: 10.1016/j.jcrs.2010.02.025. [DOI] [PubMed] [Google Scholar]
- 3. Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, González-Méijome JM, Cerviño A. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35:70–5. doi: 10.1016/j.jcrs.2008.09.027. [DOI] [PubMed] [Google Scholar]
- 4. Horn JD. Status of toric intraocular lenses. Curr Opin Ophthalmol. 2007;18:58–61. doi: 10.1097/ICU.0b013e328011f9bf. [DOI] [PubMed] [Google Scholar]
- 5. Netto MV, Mohan RR, Ambrosio R, Jr, Hutcheon AE, Zieske JD, Wilson SE. Wound healing in the cornea:A review of refractive surgery complications and new prospects for therapy. Cornea. 2005;4:509–22. doi: 10.1097/01.ico.0000151544.23360.17. [DOI] [PubMed] [Google Scholar]
- 6. Shimizu K, Misawa A, Suzuki Y. Toric intraocular lenses:Correcting astigmatism while controlling axis shift. J Cataract Refract Surg. 1994;20:523–6. doi: 10.1016/s0886-3350(13)80232-5. [DOI] [PubMed] [Google Scholar]
- 7. Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal L. Toric intraocular lenses in the correction of astigmatism during cataract surgery:A systematic review and meta-analysis. Ophthalmology. 2016;123:275–86. doi: 10.1016/j.ophtha.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 8. Waltz KL, Featherstone K, Tsai L, Trentacost D. Clinical outcomes of TECNIS toric intraocular lens implantation after cataract removal in patients with corneal astigmatism. Ophthalmology. 2015;122:39–47. doi: 10.1016/j.ophtha.2014.06.027. [DOI] [PubMed] [Google Scholar]
- 9. Sun XY, Vicary D, Montgomery P, Griffiths M. Toric intraocular lenses for correcting astigmatism in 130 eyes. Ophthalmology. 2000;107:1776–81. doi: 10.1016/s0161-6420(00)00266-9. [DOI] [PubMed] [Google Scholar]
- 10. Kim YJ, Wee WR, Kim MK. Efficacy of 4-haptic Bitoric intraocular Lens implantation in Asian patients with cataract and astigmatism. Korean J Ophthalmol. 2019;33:36–45. doi: 10.3341/kjo.2018.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kobashi H, Kamiya K, Igarashi A, Ishii R, Sato N, Wang G, et al. Comparison of corneal power, corneal astigmatism, and axis location in normal eyes obtained from an autokeratometer and a corneal topographer. J Cataract Refract Surg. 2012;38:648–54. doi: 10.1016/j.jcrs.2011.11.026. [DOI] [PubMed] [Google Scholar]
- 12. Goggin M, Moore S, Esterman A. Outcome of toric intraocular lens implantation after adjusting for anterior chamber depth and intraocular lens sphere equivalent power effects. Arch Ophthalmol. 2011;129:998–1003. doi: 10.1001/archophthalmol.2011.188. [DOI] [PubMed] [Google Scholar]
- 13. Koch DD, Ali SF, Weikert MP, Shirayama M, Jenkins R, Wang L. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38:2080–7. doi: 10.1016/j.jcrs.2012.08.036. [DOI] [PubMed] [Google Scholar]
- 14. Visser N, Bauer NJ, Nuijts RM. Residual astigmatism following toric intraocular lens implantation related to pupil size. J Refract Surg. 2012;28:729–32. doi: 10.3928/1081597X-20120911-02. [DOI] [PubMed] [Google Scholar]
- 15. Berdahl JP, Hardten DR. Residual astigmatism after toric intraocular lens implantation. J Cataract Refract Surg. 2012;38:730–2. doi: 10.1016/j.jcrs.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 16. Jin H, Limberger IJ, Ehmer A, Guo H, Auffarth GU. Impact of axis misalignment of toric intraocular lenses on refractive outcomes after cataract surgery. J Cataract Refract Surg. 2010;36:2061–72. doi: 10.1016/j.jcrs.2010.06.066. [DOI] [PubMed] [Google Scholar]
- 17. Chang DF. Comparative rotational stability of single-piece open-loop acrylic and plate-haptic silicone toric intraocular lenses. J Cataract Refract Surg. 2008;34:1842–7. doi: 10.1016/j.jcrs.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 18. Jung NY, Lim DH, Hwang SS, Hyun J, Chung TY. Comparison of clinical outcomes of toric intraocular lens, Precizon vs Tecnis:A single center randomized controlled trial. BMC Ophthalmol. 2018;18:292. doi: 10.1186/s12886-018-0955-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nanavaty MA, Bedi KK, Ali S, Holmes M, Rajak S. Toric intraocular lenses versus peripheral corneal relaxing incisions for astigmatism between 0.75 and 2.5 diopters during cataract surgery. Am J Ophthalmol. 2017;180:165–77. doi: 10.1016/j.ajo.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 20. Seth SA, Bansal RK, Ichhpujani P, Seth NG. Comparative evaluation of two toric intraocular lenses for correcting astigmatism in patients undergoing phacoemulsification. Indian J Ophthalmol. 2018;66:1423–8. doi: 10.4103/ijo.IJO_73_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ram J, Singh R, Gupta R, Bhutani G, Gupta PC, Sukhija J. Toric intraocular lens implantation in children with developmental cataract and preexisting corneal astigmatism. Acta Ophthalmol. 2017;95:e95–100. doi: 10.1111/aos.13220. [DOI] [PubMed] [Google Scholar]
- 22. Miyake T, Kamiya K, Amano R, Iida Y, Tsunehiro S, Shimizu K. Long-term clinical outcomes of toric intraocular lens implantation in cataract cases with preexisting astigmatism. J Cataract Refract Surg. 2014;40:1654–60. doi: 10.1016/j.jcrs.2014.01.044. [DOI] [PubMed] [Google Scholar]
- 23. Ferreira TB, Almeida A. Comparison of the visual outcomes and OPD-scan results of AMO Tecnis toric and Alcon Acrysof IQ toric intraocular lenses. J Refract Surg. 2012;28:551–5. doi: 10.3928/1081597X-20120703-03. [DOI] [PubMed] [Google Scholar]
- 24. Visser N, Ruíz-Mesa R, Pastor F, Bauer NJ, Nuijts RM, Montés-Micó R. Cataract surgery with toric intraocular lens implantation in patients with high corneal astigmatism. J Cataract Refract Surg. 2011;37:1403–10. doi: 10.1016/j.jcrs.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 25. Dardzhikova A, Shah CR, Gimbel HV. Early experience with the AcrySof toric IOL for the correction of astigmatism in cataract surgery. Can J Ophthalmol. 2009;44:269–73. doi: 10.3129/i09-048. [DOI] [PubMed] [Google Scholar]
- 26. Thomas BC, Khoramnia R, Auffarth GU, Holzer MP. Clinical outcomes after implantation of a toric intraocular lens with a transitional conic toric surface. Br J Ophthalmol. 2018;102:313–6. doi: 10.1136/bjophthalmol-2017-310386. [DOI] [PubMed] [Google Scholar]
- 27. Lubiński W, Kaźmierczak B, Gronkowska-Serafin J, Podborączyńska-Jodko K. Clinical outcomes after uncomplicated cataract surgery with implantation of the tecnis toric intraocular lens. J Ophthalmol. 2016;2016:3257217. doi: 10.1155/2016/3257217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lam DK, Chow VW, Ye C, Ng PK, Wang Z, Jhanji V. Comparative evaluation of aspheric toric intraocular lens implantation and limbal relaxing incisions in eyes with cataracts and ≤3 dioptres of astigmatism. Br J Ophthalmol. 2016;100:258–62. doi: 10.1136/bjophthalmol-2014-306587. [DOI] [PubMed] [Google Scholar]
- 29. Hirnschall N, Maedel S, Weber M, Findl O. Rotational stability of a single-piece toric acrylic intraocular lens:A pilot study. Am J Ophthalmol. 2014;157:405–11. doi: 10.1016/j.ajo.2013.09.032. [DOI] [PubMed] [Google Scholar]
- 30. Mazzini C. Visual and refractive outcomes after cataract surgery with implantation of a new toric intraocular lens. Case Rep Ophthalmol. 2013;4:48–56. doi: 10.1159/000353389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sheppard AL, Wolffsohn JS, Bhatt U, Hoffmann PC, Scheider A, Hütz WW, et al. Clinical outcomes after implantation of a new hydrophobic acrylic toric IOL during routine cataract surgery. J Cataract Refract Surg. 2013;39:41–7. doi: 10.1016/j.jcrs.2012.08.055. [DOI] [PubMed] [Google Scholar]
- 32. Entabi M, Harman F, Lee N, Bloom PA. Injectable 1-piece hydrophilic acrylic toric intraocular lens for cataract surgery:Efficacy and stability. J Cataract Refract Surg. 2011;37:235–40. doi: 10.1016/j.jcrs.2010.08.040. [DOI] [PubMed] [Google Scholar]
- 33. Goggin M, Zamora-Alejo K, Esterman A, van Zyl L. Adjustment of anterior corneal astigmatism values to incorporate the likely effect of posterior corneal curvature for toric intraocular lens calculation. J Refract Surg. 2015;31:98–102. doi: 10.3928/1081597X-20150122-04. [DOI] [PubMed] [Google Scholar]
- 34. Abulafia A, Barrett GD, Kleinmann G, Ofir S, Levy A, Marcovich AL, et al. Prediction of refractive outcomes with toric intraocular lens implantation. J Cataract Refract Surg. 2015;41:936–44. doi: 10.1016/j.jcrs.2014.08.036. [DOI] [PubMed] [Google Scholar]
- 35. Skrzypecki J, Sanghvi PM, Suh LH. Performance of the barrett toric calculator with and without measurements of posterior corneal curvature. Eye. 2019;33:1762–7. doi: 10.1038/s41433-019-0489-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kaur M, Shaikh F, Falera R, Titiyal JS. Optimizing outcomes with toric intraocular lenses. Indian J Ophthalmol. 2017;65:1301–13. doi: 10.4103/ijo.IJO_810_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lee BS, Onishi AC, Chang DF. Comparison of rotational stability and repositioning rates of two presbyopia-correcting and two monofocal toric intraocular lenses. J Cataract Refract Surg. 2021;47:622–6. doi: 10.1097/j.jcrs.0000000000000497. [DOI] [PubMed] [Google Scholar]
- 38. Mayer WJ, Kreutzer T, Dirisamer M, Kern C, Kortuem K, Vounotrypidis E, et al. Comparison of visual outcomes, alignment accuracy, and surgical time between 2 methods of corneal marking for toric intraocular lens implantation. J Cataract Refract Surg. 2017;43:1281–6. doi: 10.1016/j.jcrs.2017.07.030. [DOI] [PubMed] [Google Scholar]
- 39. Woodcock MG, Lehmann R, Cionni RJ, Breen M, Scott MC. Intraoperative aberrometry versus standard preoperative biometry and a toric IOL calculator for bilateral toric IOL implantation with a femtosecond laser:One-month results. J Cataract Refract Surg. 2016;42:817–25. doi: 10.1016/j.jcrs.2016.02.048. [DOI] [PubMed] [Google Scholar]
- 40. Haripriya A, Gk S, Mani I, Chang DF. Comparison of surgical repositioning rates and outcomes for hydrophilic vs hydrophobic single-piece acrylic toric IOLs. J Cataract Refract Surg. 2021;47:178–83. doi: 10.1097/j.jcrs.0000000000000415. [DOI] [PubMed] [Google Scholar]


