Abstract
Objective
Postpartum women are a vulnerable population to pandemic stressors that challenge their psychological well-being. Thus, reliable and valid instruments are necessary to measure pandemic-related stress and to identify risk and protective factors. This work aimed to assess psychometric properties of the COVID-19 Pandemic-Related Stress Scale (PSS-10-C) and associations of maternal pandemic stress with demographic, reproductive and pandemic factors of Argentinian postpartum women during the second COVID-19 wave.
Design
An online cross-sectional survey was conducted from April to June 2021.
Setting
Online recruitment of postpartum women was carried out during the second wave of COVID-19 in Argentina. This study was conducted in accordance with the Declaration of Helsinki and had the corresponding ethical approval.
Participants
This study was performed on 300 women, aged 18–49 years, up to 12 months postpartum in Argentina.
Measurements and findings
Stress was assessed with PSS-10-C, with a sociodemographic questionnaire being used to collect demographic, reproductive and pandemic variables. Statistical analysis included psychometric procedures, structural equation modeling, and multiple regressions. PSS-10-C was a reliable and structurally valid instrument with two subscales, with entire scale, Stress and Coping subscales scoring 17.31 (6.52), 9.70 (4.61) and 7.61 (2.77), respectively. History of mood disorders, pregnancy loss, and unhealthy child during the pandemic predisposed to increased stress (β > 0.10, p < 0.05), whereas having work and practicing breastfeeding promoted coping to face it (β < -0.13, p < 0.05). This situation was impaired by mood changes, loss of happiness, economic changes, fear of contracting COVID-19 -own or by a loved one- (β > 0.11, p < 0.05).
Key conclusions
The study highlighted the vulnerability of postpartum women's mental health in the pandemic context, with PSS-10-C being a useful instrument for clinicians and researchers to assess perceived stress. Targeting interventions toward women at higher risk can be highly beneficial for maternal and child health.
Keywords: COVID-19, Pandemics, Stress, Postpartum, Risk factors, Maternal medicine
Introduction
The current COVID-19 pandemic represents a public health problem due to its impact on people's physical and mental health (Kuriala, 2021). The unexpected onset of this disease has disrupted daily life, leading governments around the world to impose restrictions to contain and mitigate its spread (Ganesan et al., 2021). Since the beginning, people have been exposed to numerous stressors impacting their psychological well-being. There is evidence that the fear of contracting the virus or that a loved one will do so; uncertainties regarding the spread, the vaccination, the society reopening and the virus variants themselves; the loss of loved ones, as well as the impact of restrictions (social isolation, economic impact, school closings, teleworking) have been related to mental disorders (Saricali et al., 2020; Şimşir et al., 2021; Scotta et al., 2020).
This becomes more relevant for mentally vulnerable populations, such as pregnant and postpartum women (Perzow et al., 2021). These women have an increased risk for postpartum depression, which can be associated with the confinement duration, insomnia, and cognitive problems (Miranda et al., 2021; Perzow et al., 2021; Oskovi-Kaplan et al., 2021).
The study of stress focuses on the identification of environmental stressors, subjective perceptions, affective cognitive-behavioural reactions, and physiological responses (Lee, 2012). One of the most recognized instruments for evaluating psychological stress is the Perceived Stress Scale (PSS), which has been adapted for the current epidemiological context (Campo-Arias et al., 2021). PSS focuses on how individuals perceive stress, which reflects an imbalance between situational demands and the resources to cope with it (Chiu et al., 2016). In addition, high scores on PSS are associated with physical and mental health problems (Lu et al., 2019; Zou et al., 2020; Miranda et al., 2020a).
PSS was adapted to numerous languages and specific populations (Cohen et al., 1983; Cohen, 1988), and a recent version has been developed in Spanish language to evaluate stress related to the COVID-19 pandemic, showing good psychometric properties (Campo-Arias et al., 2021). Several investigations used PSS during the COVID-19 pandemic, which have shown a higher prevalence of psychological stress in the general population (Torales et al., 2020), in patients with COVID-19 (Gu et al., 2021), and in frontline healthcare workers (Campo-Arias et al., 2021). PSS-10-C is also useful in combination with other instruments to assess the pandemic effects on people's well-being (Eubank et al., 2021). However, it is necessary to confirm the reliability and validity of this instrument in specific populations such as postpartum women, because they may respond distinctly to online PSS adaptations to COVID-19 situation, such as adequation of each item to inquire uncertainties, feelings, among other issues, specifically derived from the pandemic (Campo-Arias et al., 2021). Thus, the objective of this study was to analyze the reliability and confirm the factorial structure of PSS-10-C for the study of pandemic-related stress in Argentinian postpartum women during the second coronavirus outbreak. In addition, this study aimed to identify factors that are associated with psychological stress.
Methods
Subjects and design
For this cross-sectional study, self-report online questionnaires were administered to 300 postpartum women from Argentina, who were recruited from April to June 2021, during the second outbreak of COVID-19. Women were recruited from public hospitals, private health clinics, and online community recruitment. Inclusion criteria were: adult (≥ 18 years-old), Argentina's inhabitant, and postpartum (first twelve months). All participants signed informed consent before being voluntarily included. This research was approved by the corresponding Research Ethics Committee (registration code REPIS-3177), following the Declaration of Helsinki and current legislation (Cordoba's Law 9694, 2009).
Instruments
The pandemic-related perceived stress was assessed using the 10-item version of PSS-C in Latin American Spanish (Campo-Arias et al., 2020). PSS-10-C is an easy-to-use self-report scale assessing the level of perceived stress during the past month related to the pandemic. Items are rated on a 5-point Likert scale (0 = never and 4 = very often). Originally, the scale showed a bidimensional structure: the first component named Stress focuses on the perceived lack of control over the situation (items 1, 2, 3, 6, 9, and 10), whereas the component Coping is defined as the set of cognitive and behavioral strategies necessary to manage stressful situations (items 4, 5, 7, and 8). As this second factor involved inverse key items, higher scores reflect low perceived ability to cope with pandemic stressors. The total score is obtained as the sum of all the items, with higher scores corresponding to higher perceived stress (Miranda et al., 2020b).
A questionnaire was used to collect data about sociodemographic variables, characteristics of social isolation and breastfeeding practices and was recorded as previously reported (Miranda et al., 2021).
Statistical analysis
Descriptive statistics (mean and standard deviation) were calculated for all numerical variables; the percentage of categorical variables was also described. Regarding psychometric procedures, confirmatory factor analysis (CFA) was applied using maximum-likelihood structural equation modeling techniques (Miranda et al., 2020b), previously performing a distributional analysis of PSS-10-C through histograms, q-q plots, box-plots, and Shapiro-Wilk tests. First- and second-order CFA models were assessed to test PSS-10-C structure. First-order models were: unidimensional (i.e., all items load on one latent variable) and bidimensional (i.e., items load differently on two latent variables: Stress or Coping subscales). On the other hand, the second-order CFA used was a bifactor model in which the variance of each item is explained simultaneously by a general factor, a specific factor, and a residual. Thus, it is possible to specify the direct effects of first-order factors (from the bidimensional model) and the second-order general factor (Pérez-Salas et al., 2019). Therefore, the bifactor model was tested to determine whether the measure was sufficiently unidimensional to support using a total score, while still accounting for its multidimensionality. Traditional goodness-of-fit indices were calculated. Next, reliability was assessed with alpha (α), omega (ω), inter-item, item-test, and item-rest correlations.
Finally, multiple regression models were performed to test factors associated with psychological stress. Results were expressed as regression coefficients with a standard error, adjusted betas coefficients (β), confidence interval (IC95%) and p-values. Statistical analyses were performed using the Stata software (version 15, StataCorp).
Sample size and power analysis
An a priori power analysis for multiple regression was carried out to estimate the sample size needed to detect minimal effects, taking into account the following parameters: probability level (α) = 0.05, statistical power (1 - β) = 0.95, effect size (f2) = 0.15, maximum number of predictors = 14. Given that at least 194 participants were needed to meet these criteria, the current sample (n = 300) therefore strongly supported result reliability.
Results
Sociodemographic and reproductive characteristics are summarized in Table 1 . Regarding pandemic variables, participants lived with 2.77 (1.93) people and were around on day 51.71 (11.76) of restrictions due to the second COVID-19 wave, with 27.67% being currently in quarantine. Although 11.33% had a previous diagnosis of mood disorder, 73.33% considered that pandemic impacted negatively on mood, and 63.33% answered that they were happier before the pandemic. Given it could affect economically, 42.67% showed financial worsening, whereas 14.33% improved. COVID-19 had been diagnosed in 28.33% of women and 29.67% had an infected loved one. In addition, 16.33 had a loved one who died from COVID-19. Most of the women were afraid of getting the coronavirus (82.67%) or that a loved one would get it (96.67%). Only 18.67% had received at least one dose of the anti-COVID-19 vaccine. The majority (60.33%) had been informed about COVID-19-related newborn care.
Table 1.
Sample characteristics of 300 postpartum women from Argentina during the second wave of the COVID-19 pandemic.
| N (%) | |
|---|---|
| Maternal age – M(SD) | 29.65 (5.77) |
| Partnership status | |
| In couple | 276 (92.00) |
| Single | 24 (8.00) |
| Educational level | |
| < 12 years of formal education | 17 (5.67) |
| ≥ 12 years of formal education | 283 (94.33) |
| Stable employment | |
| Yes | 152 (50.67) |
| No | 148 (49.33) |
| Work status | |
| Not working | 86 (28.67) |
| Working from home | 75 (25.00) |
| Working outside home | 139 (46.33) |
| Health insurance | |
| Yes | 252 (84.00) |
| No | 48 (16.00) |
| Postpartum (months) – M(SD) | 5.74 (3.58) |
| Gestation (weeks) – M(SD) | 38.47 (1.69) |
| Mode of delivery | |
| Vaginal | 104 (34.67) |
| Caesarean section | 196 (65.33) |
| Type of pregnancy | |
| Single | 297 (99.00) |
| Twins | 3 (1.00) |
| Parity | |
| Primiparity | 183 (61.00) |
| Multiparity | 117 (39.00) |
| History of pregnancy losses | |
| Yes | 76 (25.33) |
| No | 224 (74.67) |
| Hospitalization during the last pregnancy | |
| Yes | 41 (13.67) |
| No | 259 (86.33) |
| Hospitalization of the newborn | |
| Yes | 46 (15.33) |
| No | 254 (84.67) |
| Infant with current health problems | |
| Yes | 7 (2.33) |
| No | 293 (97.67) |
| Type of lactation | |
| Exclusive breastfeeding | 110 (36.67) |
| Mixed lactation | 143 (47.67) |
| Formula | 47 (15.67) |
Note. M = Mean, SD = Standard Deviation.
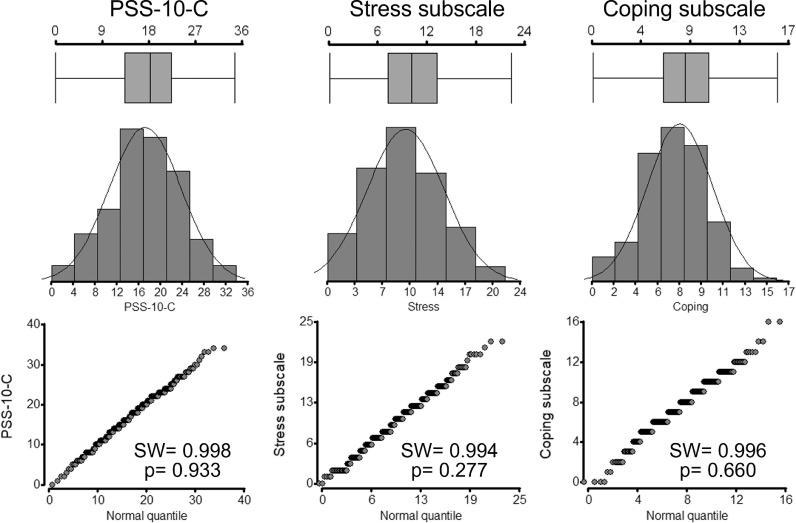
Total PSS-10-C scoring was 17.31 (6.52), while the Stress subscale showed a mean of 9.70 (4.61) and Coping subscale of 7.61 (2.77). Histograms and q-q plots of the three scores indicated normal distribution, which was confirmed with the normality test (Fig. 1 ). Internal consistency was adequate for the entire scale (> 0.80), as well as for Stress (> 0.80) and Coping (> 0.60) (Table 2 ). All item-test and item-rest correlations were < 0.30, the average inter-item correlations were around 0.30, and the items of each subscale correlated adequately. Overall, reliability decreased after item deletion.
Fig. 1.
Distributional analysis of the Perceived Stress Scale modified for COVID-19 (PSS-10-C) in a sample of 300 Argentinian postpartum women. SW = Shapiro-Wilks's normality test.
Table 2.
Reliability of the perceived stress scale modified for COVID-19 (PSS-10-C) in a sample of Argentinian postpartum women (n = 300).
| Item | I-T | I-R | I-I | α | α after deletion | ω | ω after deletion | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item 1 | 0.6310 | 0.5199 | 0.3286 | 0.8150 | 0.8159 | 1.00 | |||||||||||
| Item 2 | 0.7373 | 0.6504 | 0.3100 | 0.8017 | 0.8038 | 0.53 | 1.00 | ||||||||||
| Item 3 | 0.6978 | 0.6011 | 0.3169 | 0.8068 | 0.8085 | 0.55 | 0.51 | 1.00 | |||||||||
| Item 4 | 0.4896 | 0.3546 | 0.3533 | 0.8310 | 0.8328 | 0.10 | 0.24 | 0.24 | 1.00 | ||||||||
| Item 5 | 0.5843 | 0.4642 | 0.3368 | 0.8205 | 0.8236 | 0.25 | 0.34 | 0.36 | 0.29 | 1.00 | |||||||
| Item 6 | 0.5627 | 0.4389 | 0.3405 | 0.8229 | 0.8244 | 0.27 | 0.38 | 0.34 | 0.18 | 0.17 | 1.00 | ||||||
| Item 7 | 0.5723 | 0.4502 | 0.3388 | 0.8218 | 0.8260 | 0.17 | 0.28 | 0.27 | 0.27 | 0.30 | 0.27 | 1.00 | |||||
| Item 8 | 0.6173 | 0.5034 | 0.3310 | 0.8166 | 0.8217 | 0.34 | 0.31 | 0.29 | 0.23 | 0.34 | 0.23 | 0.48 | 1.00 | ||||
| Item 9 | 0.6300 | 0.5186 | 0.3288 | 0.8151 | 0.8167 | 0.31 | 0.44 | 0.32 | 0.21 | 0.27 | 0.29 | 0.23 | 0.34 | 1.00 | |||
| Item 10 | 0.7705 | 0.6924 | 0.3042 | 0.7974 | 0.7980 | 0.45 | 0.60 | 0.52 | 0.32 | 0.35 | 0.41 | 0.34 | 0.31 | 0.55 | 1.00 | ||
| Entire scale | 0.3289 | 0.8305 | 0.8324 | ||||||||||||||
| Stress subscale | 0.4312 | 0.8189 | 0.8249 | ||||||||||||||
| Coping subscale | 0.3187 | 0.6517 | 0.6566 |
Note. I-T = Item-test correlation; I-R = Item-rest correlation; I-I = Average inter-item correlation; α = Cronbach's alpha coefficient; ω = McDonald's omega coefficient. The correlations are expressed as Pearson's coefficients.
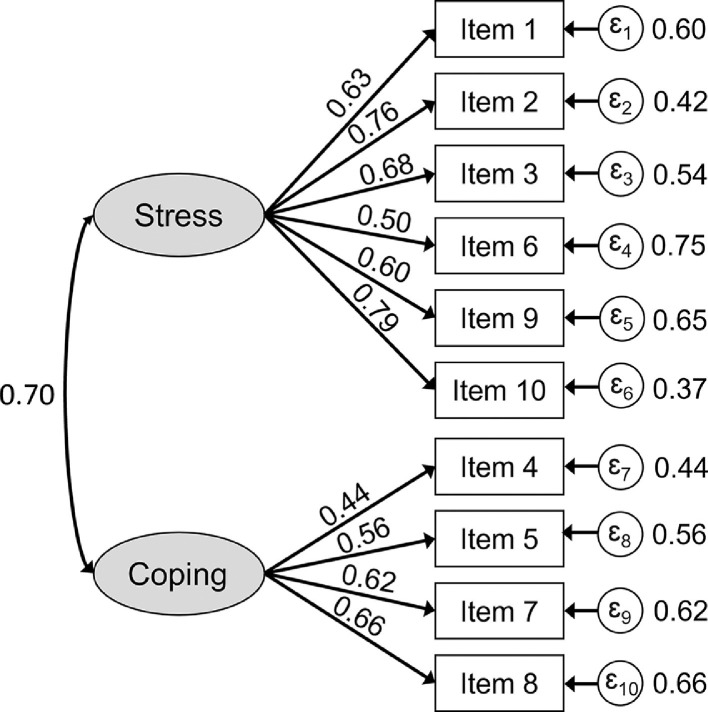
Table 3 shows goodness-of-fit measures for CFA models. The bidimensional model showed better indices than the unidimensional one, with values in accordance with cut-off criteria. Standardized coefficients were significant, ranging from 0.50 to 0.79 for Stress and from 0.44 to 0.66 for Coping (Fig. 2 ). Inter-factor correlation was 0.70. Also, the bifactor model showed adequate goodness-of-fit.
Table 3.
Fit indices for confirmatory factor analysis models.
| PSS-10-C |
||||
|---|---|---|---|---|
| Expected values | Unidimensional | Bidimensional | Bifactor | |
| χ2/df | < 3.00 | 3.95 | 2.54 | 1.54 |
| RMSEA | < 0.08 | 0.099 | 0.074 | 0.042 |
| CFI | > 0.90 | 0.879 | 0.935 | 0.985 |
| TLI | > 0.90 | 0.844 | 0.914 | 0.972 |
| SRMR | < 0.05 | 0.063 | 0.046 | 0.033 |
| CD | > 0.95 | 0.862 | 0.931 | 0.992 |
| AIC | The lower the better | 7978.25 | 7931.73 | 7899.07 |
| BIC | 8089.36 | 8046.55 | 8050.92 | |
Note. PSS-10-C = Perceived Stress Scale modified for COVID-19; χ2/df = chi-square to degree of freedom ratio; RMSEA = root mean square error of approximation; CFI = comparative fit index; TLI = Tucker–Lewis index; SRMR = standardized root mean square residual; CD = coefficient of determination; AIC = Akaike's information criterion; BIC = Bayesian information criterion. Boldface represents acceptable values.
Fig. 2.
The two-factor confirmatory factor analysis model of the Perceived Stress Scale modified for COVID-19 (PSS-10-C), showing standardized estimates fitted in a sample of 300 Argentinian postpartum women. All factor loadings were significant (T > 1.96).
After checking the structural validity, multivariate logistic regression models were performed between scores and other variables Table 4. displays the first model for women characteristics showing that a history of mood disorders had higher scores on the entire PSS-10-C (β = 0.158, p = 0.007) and on the Stress subscale (β = 0.163, p = 0.006). Workers had a lower score on the Coping subscale (β = -0.14, p = 0.035).
Table 4.
Multivariate logistic regression between pandemic-related psychological stress and postpartum women factors during the second COVID-19 wave in Argentina.
| PSS 10-C total score |
Stress |
Coping |
|||||||
| Coef (SE) | β | p | Coef (SE) | β | p | Coef (SE) | β | p | |
| Age | 1.718 (0.976) | 0.102 | 0.079 | 1.245 (0.689) | 0.105 | 0.072 | 0.472 (0.417) | 0.066 | 0.258 |
| Couple relationship | 0.208 (1.403) | 0.009 | 0.882 | -0.127 (0.990) | -0.008 | 0.898 | 0.336 (0.599) | 0.033 | 0.576 |
| Educational level | -0.075 (1.714) | -0.003 | 0.965 | -0.205 (1.210) | -0.010 | 0.865 | 0.130 (0.732) | 0.011 | 0.859 |
| Work | -0.841 (0.950) | -0.058 | 0.377 | 0.020 (0.671) | 0.002 | 0.976 | -0.861 (0.406) | -0.140 | 0.035 |
| Telecommuting | 0.282 (0.905) | 0.019 | 0.755 | 0.298 (0.639) | 0.028 | 0.641 | -0.016 (0.386) | -0.002 | 0.968 |
| Taking virtual classes | -0.297 (0.758) | -0.023 | 0.696 | 0.053 (0.535) | 0.006 | 0.922 | -0.349 (0.323) | -0.063 | 0.281 |
| Health insurance | -1.202 (1.149) | -0.068 | 0.296 | -1.440 (0.811) | -0.115 | 0.077 | 0.238 (0.490) | 0.032 | 0.628 |
| Prior diagnosis of mood disorder | 3.244 (1.197) | 0.158 | 0.007 | 2.360 (0.845) | 0.163 | 0.006 | 0.884 (0.511) | 0.101 | 0.085 |
Note. Coef = Regression coefficient; SE = Standard error; β = Adjusted beta coefficient.
Regarding reproductive health (Table 5 ), history of pregnancy loss was related to higher scores in PSS-10-C (β = 0.150, p = 0.011), Stress subscale (β = 0.137, p = 0.019) and Coping subscale (β = 0.124, p = 0.037). In addition, mothers of an unhealthy child during the pandemic showed higher scores in PSS-10-C (β = 0.13, p = 0.037) and Stress subscale (β = 0.146, p = 0.016). Overall, although women who breastfed had lower pandemic-related stress, it was statistically significant only with Coping (β = -0.174, p = 0.043).
Table 5.
Multivariate logistic regression between pandemic-related psychological stress and reproductive variables of postpartum women during the second COVID-19 wave in Argentina.
| PSS 10-C total score |
Stress |
Coping |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Coef (SE) | β | p | Coef (SE) | β | p | Coef (SE) | β | p | |
| Number of children | 0.172 (0.548) | 0.019 | 0.753 | 0.095 (0.386) | 0.015 | 0.805 | 0.077 (0.237) | 0.019 | 0.746 |
| Prior pregnancy loss | 2.249 (0.877) | 0.150 | 0.011 | 1.455 (0.618) | 0.137 | 0.019 | 0.794 (0.380) | 0.124 | 0.037 |
| Multiple pregnancy | 0.710 (3.896) | 0.010 | 0.856 | 0.590 (2.748) | 0.013 | 0.83 | 0.119 (1.687) | 0.004 | 0.944 |
| Gestational age | -0.264 (0.253) | -0.068 | 0.298 | -0.310 (0.178) | -0.114 | 0.083 | 0.046 (0.109) | 0.028 | 0.672 |
| Postpartum months | 0.137 (0.122) | 0.075 | 0.263 | 0.114 (0.086) | 0.089 | 0.185 | 0.022 (0.053) | 0.029 | 0.671 |
| Mode of delivery | 0.498 (0.797) | 0.036 | 0.533 | 0.382 (0.562) | 0.039 | 0.497 | 0.115 (0.345) | 0.02 | 0.738 |
| Hospitalization during pregnancy | -2.124 (1.158) | -0.112 | 0.068 | -1.477 (0.817) | -0.111 | 0.072 | -0.647 (0.502) | -0.08 | 0.198 |
| Hospitalization of the newborn | -1.820 (1.172) | -0.101 | 0.121 | -1.384 (0.826) | -0.109 | 0.095 | -0.436 (0.507) | -0.057 | 0.391 |
| Newborn with health problem | 5.424 (2.592) | 0.126 | 0.037 | 4.417 (1.828) | 0.146 | 0.016 | 1.007 (1.122) | 0.055 | 0.370 |
| Mixed lactation vs. formula | -1.827 (1.092) | -0.140 | 0.095 | -0.864 (0.770) | -0.094 | 0.263 | -0.963 (0.473) | -0.174 | 0.043 |
| Exclusive lactation vs. formula | -1.511 (1.232) | -0.112 | 0.221 | -0.793 (0.869) | -0.083 | 0.362 | -0.718 (0.533) | -0.125 | 0.180 |
Note. Coef = Regression coefficient; SE = Standard error; β = Adjusted beta coefficient.
Finally, the model with pandemic-related variables indicated that women who felt mood changes triggered higher stress levels, according to scores in PSS-10-C (β = 0.205, p < 0.001) and the Stress subscale (β = 0.250, p < 0.001). In addition, those who felt unhappier scored higher on the entire scale (β = 0.215, p < 0.001) and on both subscales: Stress (β = 0.180, p = 0.001) and Coping (β = 0.207, p = 0.001). Economic impairment by the pandemic increased stress with higher scores on the three subscales. Nonetheless, participants with economic improvement also showed a higher score on the Coping subscale than ones without economic change. Also, fear of contracting COVID-19 (own or by a loved one) was associated with increments on all three measures (Table 6 ).
Table 6.
Multivariate logistic regression between pandemic-related psychological stress and pandemic variables of postpartum women during the second COVID-19 wave in Argentina.
| PSS 10-C total score |
Stress |
Coping |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Coef (SE) | β | p | Coef (SE) | β | p | Coef (SE) | β | p | |
| Social restriction (days) | -0.038 (0.027) | -0.068 | 0.173 | -0.018 (0.020) | -0.046 | 0.356 | -0.019 (0.013) | -0.082 | 0.130 |
| Quarantine (days) | 0.482 (0.735) | 0.033 | 0.512 | 0.418 (0.525) | 0.041 | 0.427 | 0.064 (0.342) | 0.010 | 0.851 |
| Cohabitants (number) | 0.174 (0.171) | 0.052 | 0.309 | 0.086 (0.122) | 0.036 | 0.483 | 0.088 (0.079) | 0.061 | 0.269 |
| Changes in mood | 3.014 (0.818) | 0.205 | <0.001 | 2.608 (0.585) | 0.250 | <0.001 | 0.406 (0.381) | 0.065 | 0.287 |
| Feeling of less happiness | 2.907 (0.731) | 0.215 | <0.001 | 1.721 (0.522) | 0.180 | 0.001 | 1.186 (0.340) | 0.207 | 0.001 |
| Economic impairment | 3.318 (0.714) | 0.252 | <0.001 | 2.360 (0.808) | 0.254 | <0.001 | 0.957 (0.332) | 0.171 | 0.004 |
| Economic improvement | 1.726 (0.987) |
0.093 | 0.081 | 0.808 (0.706) |
0.062 | 0.253 | 0.918 (0.460) | 0.116 | 0.047 |
| Prior COVID-19 diagnosis | 0.154 (0.727) | 0.011 | 0.832 | 0.504 (0.520) | 0.049 | 0.333 | -0.350 (0.339) | -0.057 | 0.302 |
| Loss of loved one by COVID-19 | 0.525 (0.863) | 0.030 | 0.543 | 0.262 (0.617) | 0.021 | 0.671 | 0.263 (0.402) | 0.035 | 0.513 |
| Loved one with current COVID-19 | 0.111 (0.698) | 0.008 | 0.874 | 0.072 (0.499) | 0.007 | 0.886 | 0.039 (0.325) | 0.006 | 0.905 |
| Fear of getting COVID-19 | 3.117 (0.933) | 0.181 | 0.001 | 1.978 (0.667) | 0.163 | 0.003 | 1.139 (0.434) | 0.156 | 0.009 |
| Fear that a loved one will get COVID-19 | 5.024 (1.947) | 0.139 | 0.010 | 2.985 (1.392) | 0.116 | 0.033 | 2.040 (0.907) | 0.132 | 0.025 |
| Anti-COVID-19 vaccine (at least one dose) | 0.294 (0.828) | 0.018 | 0.723 | 0.156 (0.592) | 0.013 | 0.793 | 0.138 (0.386) | 0.020 | 0.720 |
| Access to newborn care information | -0.119 (0.663) | -0.009 | 0.857 | 0.271 (0.474) | 0.029 | 0.567 | -0.391 (0.309) | -0.069 | 0.207 |
Note. Coef = Regression coefficient; SE = Standard error; β = Adjusted beta coefficient.
Discussion
The objective of this work was to study the psychometric properties of PSS-10-C to evaluate pandemic-related psychological stress in Argentinian postpartum women during the second COVID-19 outbreak and to identify modulating variables. Our hypotheses were confirmed, since the adaptation of PSS-10 proposed by Campo-Arias et al. (2020) showed good reliability and is structurally valid to study the pandemic impact on emotional well-being in a psychologically vulnerable population such as postpartum women. In addition, we were able to find that stress was related to demographic, reproductive and pandemic variables, which allowed us to identify groups of women with greater vulnerability.
The psychometric properties of PSS-10-C were similar to the original questionnaire reports. Regarding reliability, we found that the entire scale had a high level of internal consistency, like those reported for the original version in Argentina (Miranda et al., 2020b). Questionnaire adaptation for the pandemic was developed in the general population of Latin America, and it showed similar reliability to that of our findings (Pedrozo-Pupo et al., 2020). The PSS original version has been also applied to evaluate the mental health impact of pandemic with good reliability. In this regard, the study conducted in Paraguay by Torales et al. (2020) is relevant due to its cultural similarity and geographic location, which found that women had more stress during pandemic than men. Likewise, several groups have used the original version in peripartum women during the pandemic in middle- (Masjoudi et al., 2021; Suárez-Rico et al., 2021) and high- (Ceulemans et al., 2021) income countries, with good reliability indicators.
Regarding dimensionality, we proved that PSS-10-C is composed of two factors. The first component assesses the level of psychological distress associated with the pandemic and was named "Stress." Other authors have called this factor in different ways: “Perceived distress”, “Perceived helplessness”, “General distress”, “Global negative feelings of general distress”, and “Negative stress” (Makhubela, 2020). The second component, called “Coping”, assesses the ability to adapt or respond to a stimulus or event considered stressful during pandemic, and involves mental response schemes to respond to specific external or internal demands that are excessive or exceed resources of the postpartum women (Budimir et al., 2021). This factor was named “Perceived coping”, “Perceived ability to cope effectively”, “Counter-stress”, “Perceived self-efficacy”, and “Positive stress” in previous research (Makhubela, 2020). This two-dimensional model showed better indices of goodness-of-fit than the unidimensional model and managed to explain more than 90% data variability, which has been proved for the original PSS-10 (Miranda et al., 2020b). Bifactor models are superior alternatives than uni- and bidimensional ones, as PSS can be used for global scores, while it also considers both subscales (Miranda et al., 2020b; Reis et al., 2019). Furthermore, our results confirm that PSS-10-C has a bifactor structure that allows both global and subscale scoring.
Consistent with the recent literature, we found that women with a history of mood disorders had a higher level of psychological stress (Liu et al., 2021; Masters et al., 2021). Although the pandemic has impacted on the mental health of the entire population, peripartum women have shown greater vulnerability (Santabárbara et al., 2021), especially those who have a history of mental disorders. These women require psychotherapy interventions and continuous follow-up during the pandemic to maintain their mental well-being (Hermann et al., 2021).
Another factor that was associated with stress was unemployment. This finding is consistent with that of Vallejo et al. (2018) who found that unemployment negatively influences mental health, evidenced by an increase in the PSS score. Moreover, employed women report less stress and depressive symptoms in the postpartum period (Chow et al., 2019). Evidence suggests that employment is associated with better financial resources and positive psychological outcomes, which increase coping skills (Chow et al., 2019). Financial uncertainty is another factor that has a negative effect on people's mental health, for example Varma et al. (2021) found that financial distress during the pandemic was associated with psychological stress and depression. This is similar to our findings, since women who had a negative economic impact showed greater stress. Cameron et al. (2020) also found that the economic deterioration due to the pandemic was associated with mental disorders in postpartum women.
Furthermore, our study showed that women with a history of pregnancy loss had more psychological stress. These results reflect those of Preis et al. (2020) who found that pregnant women with a history of prior pregnancy loss had increased perinatal COVID-19 stress. Up to now, far too little attention has been paid to this issue. Reardon and Craver (2021) reported that a history of mental health disorders and previous pregnancy loss are risk factors for psychotherapy treatment during postpartum, especially when both are present. Moreover, our study supports evidence from previous studies (e.g., Nguyen et al., 2016; Clout and Brown, 2015; Yağmur and Ulukoca, 2010) that showed that having an infant with health problems increases the risk of maternal stress and depression. Some studies have reported increased maternal stress in women who delivered newborn infants with health problems during the COVID-19 pandemic (Bin-Nun et al., 2021; Molgora and Accordini, 2020). A possible explanation for this might be that women perceive their children as more susceptible to complications of COVID-19, leading to greater fear, anxiety and stress; besides that, these women struggle with increased childcare demands (Vescovi et al., 2021; Ren et al., 2020).
In accordance with our results, previous studies have demonstrated that peripartum women experiencing fear of contracting COVID-19 or that a loved one would become infected was associated with higher stress (Kumari et al., 2021; Puertas-Gonzalez et al., 2021). Currently, the construct "fear of COVID-19" has been introduced in the study of mental health, being related to various psychological outcomes such as stress and negative well-being (Lathabhavan and Vispute, 2021). Furthermore, we found that negative change in mood and happiness were associated with increased stress. Fear of the pandemic has the potential to affect subjective happiness (i.e., the balance of positive and negative feelings and satisfaction in one's life) and therefore negatively impact people's mental health (Satici et al., 2020). These negative emotions and stress symptoms have shown temporary variations throughout the pandemic, being higher during the acute stages and at the peak of the waves (Yarrington et al., 2021). Another significant aspect of postpartum mental health is that it is a predictor of parenting quality. It is known that those mothers who experience stress, depression and anxiety show alteration in maternal-infant affective attachment, dissatisfaction with maternal self-efficacy, and negative impacts on child development and health. Our results show that women who do not breastfeed have higher levels of perceived stress, which is consistent with that reported by Mayopoulos et al. (2021). The authors found that stress in women who gave birth during the pandemic was associated with more symptoms of stress-related disorders and less attachment, including breastfeeding problems. Breastfeeding is known to have positive effects on the mother's physical and mental health, improving sleep and moderating psychological stress. Furthermore, although stress itself does not affect milk production, women with stress may have difficulty because it can inhibit the milk ejection reflex (Brown and Shenker, 2021). Perry et al. (2021) proposes the design of interventions with informational and psychoeducational approaches that help postpartum women to cope with pandemic stressors with resilience. The authors highlight the importance of providing adequate information at the current moment since it is essential for women to be able to initiate and maintain breastfeeding. This is particularly important because in our work almost 40% of women indicated that they did not receive information on how to care for their babies in the current pandemic.
The current data highlight the importance of addressing the mental health of postpartum women in the current pandemic scenario. The uncertainties, fears, and emotions related to COVID-19 put the mental health of women in the reproductive stages at risk. It is necessary for the health system to be prepared to comprehensively address women's health, and to provide strategies that allow women to face the demands in atypical epidemic moments. In this framework, health professionals and researchers need valid instruments to measure aspects of well-being, such as the level of psychological stress that postpartum women are facing. Here we encourage the use of PSS-10-C, adapted from a widely known instrument, which has been shown to be reliable and structurally valid for the assessment of perceived stress related to a pandemic. Consequently, its applicability extends beyond the current COVID-19 pandemic and enables its use for future epidemiological situations.
There were some limitations to this study. For example, as it is a cross-sectional study, it does not allow the evaluation of directionality over time. Thus, we recommend that future research design longitudinal studies in larger samples. Another potential problem is that other stress moderators were not analyzed such as consumption of psychostimulants, lifestyle changes, or intimate partner violence. Finally, further research should be undertaken to investigate other validity aspects of PSS-10-C, such as convergent and discriminant validity. Notwithstanding these limitations, our findings contribute to the available evidence and open new questions for future research in other populations, using different methodological designs and variables.
Funding
Funding was provided by Secretaría de Ciencia y Tecnología, Universidad Nacional de Córdoba (grant number SECYT-UNC 273/2020).
Availability of data and material
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Ethics approval
This research was approved by the Research Ethics Committee of the National Clinics Hospital, National University of Cordoba (registration code REPIS-3177), in accordance with the Declaration of Helsinki and current legislation.
CRediT authorship contribution statement
Agustín R. Miranda: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. Mariela V. Cortez: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. Ana V. Scotta: Conceptualization, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. Elio A. Soria: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships. That could have appeared to influence the work reported in this paper.
Acknowledgments
ARM and AVS were supported by Ph.D. fellowships (Universidad Nacional de Córdoba) and MVC was supported by a postdoctoral fellowship (Consejo Nacional de Investigaciones Científicas y Técnicas). The authors gratefully acknowledge the participating women.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.midw.2022.103290.
Appendix. Supplementary materials
References
- Bin-Nun A., Palmor-Haspal S., Mimouni F.B., Kasirer Y., Hammerman C., Tuval-Moshiach R. Infant delivery and maternal stress during the COVID-19 pandemic: a comparison of the well-baby versus neonatal intensive care environments. J. Perinatol. Off. 2021:1–7. doi: 10.1038/s41372-021-01016-7. Journal of the California Perinatal Association. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown A., Shenker N. Experiences of breastfeeding during COVID-19: lessons for future practical and emotional support. Matern. Child Nutr. 2021;17(1):e13088. doi: 10.1111/mcn.13088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budimir S., Probst T., Pieh C. Coping strategies and mental health during COVID-19 lockdown. J. Mental Health. 2021;30(2):156–163. doi: 10.1080/09638237.2021.1875412. (Abingdon, England) [DOI] [PubMed] [Google Scholar]
- Cameron E.E., Joyce K.M., Delaquis C.P., Reynolds K., Protudjer J., Roos L.E. Maternal psychological distress & mental health service use during the COVID-19 pandemic. J. Affect. Disord. 2020;276:765–774. doi: 10.1016/j.jad.2020.07.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campo-Arias A., Jiménez-Villamizar M.P., Caballero-Domínguez C.C. Healthcare workers' distress and perceived discrimination related to COVID-19 in Colombia. Nurs. Health Sci. 2021;23(3):763–767. doi: 10.1111/nhs.12854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campo-Arias A., Pedrozo-Cortés M.J., Pedrozo-Pupo J.C. Pandemic-related perceived stress scale of COVID-19: an exploration of online psychometric performance. Rev. Colomb. Psiquiatr. 2020;49(4):229–230. doi: 10.1016/j.rcp.2020.05.005. (English ed.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceulemans M., Foulon V., Ngo E., Panchaud A., Winterfeld U., Pomar L., Lambelet V., Cleary B., O'Shaughnessy F., Passier A., Richardson J.L., Hompes T., Nordeng H. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic-a multinational cross-sectional study. Acta Obstet. Gynecol. Scand. 2021;100(7):1219–1229. doi: 10.1111/aogs.14092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu Y.H., Lu F.J., Lin J.H., Nien C.L., Hsu Y.W., Liu H.Y. Psychometric properties of the Perceived Stress Scale (PSS): measurement invariance between athletes and non-athletes and construct validity. PeerJ. 2016;4:e2790. doi: 10.7717/peerj.2790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow A., Dharma C., Chen E., Mandhane P.J., Turvey S.E., Elliott S.J., Becker A.B., Subbarao P., Sears M.R., Kozyrskyj A.L. Trajectories of depressive symptoms and perceived stress from pregnancy to the postnatal period among Canadian women: impact of employment and immigration. Am. J. Public Health. 2019;109(S3):S197–S204. doi: 10.2105/AJPH.2018.304624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clout D., Brown R. Sociodemographic, pregnancy, obstetric, and postnatal predictors of postpartum stress, anxiety and depression in new mothers. J. Affect. Disord. 2015;188:60–67. doi: 10.1016/j.jad.2015.08.054. [DOI] [PubMed] [Google Scholar]
- Cohen S., Spacapan S., Oskamp S. The Social Psychology of Health. Sage Publications, Inc; 1988. Perceived stress in a probability sample of the United States; pp. 31–67. [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cordoba's Law 9694 . Official Bulletin. Córdoba; 2009. System of evaluation, registration and control of health researches [Spanish] Year XCVII -Volume DXXXVIII - N° 209(Argentina.). Tuesday, November 10, 2009. [Google Scholar]
- Eubank J.M., Burt K.G., Orazem J. Examining the psychometric properties of a refined perceived stress scale during the COVID-19 pandemic. J. Prev. Interv. Community. 2021;49(2):179–192. doi: 10.1080/10852352.2021.1908873. [DOI] [PubMed] [Google Scholar]
- Ganesan B., Al-Jumaily A., Fong K., Prasad P., Meena S.K., Tong R.K. Impact of coronavirus disease 2019 (COVID-19) outbreak quarantine, isolation, and lockdown policies on mental health and suicide. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.565190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu Y., Zhu Y., Xu F., Xi J., Xu G. Factors associated with mental health outcomes among patients with COVID-19 treated in the Fangcang shelter hospital in China. Asia Pac. Psychiatry. 2021;13(2):e12443. doi: 10.1111/appy.12443. Official Journal of the Pacific Rim College of Psychiatrists. [DOI] [PubMed] [Google Scholar]
- Hermann A., Fitelson E.M., Bergink V. Meeting maternal mental health needs during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(2):123–124. doi: 10.1001/jamapsychiatry.2020.1947. [DOI] [PubMed] [Google Scholar]
- Kumari A., Rajasekaran K., Ranjan P., Upadhyay A.D., Singh A., Kumar Chadda R., Bhatla N. Development of a questionnaire to assess the psychosocial effects of COVID-19 on peripartum women. Cureus. 2021;13(4):e14270. doi: 10.7759/cureus.14270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuriala G.K. COVID-19 and its impact on global mental health. Sens. Int. 2021;2 doi: 10.1016/j.sintl.2021.100108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lathabhavan R., Vispute S. Examining the mediating effects of stress on fear of COVID-19 and well-being using structural equation modeling. Int. J. Ment. Health Addict. 2021:1–9. doi: 10.1007/s11469-021-00541-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee E.H. Review of the psychometric evidence of the perceived stress scale. Asian Nurs. Res. 2012;6(4):121–127. doi: 10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Liu C.H., Erdei C., Mittal L. Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 Pandemic. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu X., Juon H.S., He X., Dallal C.M., Wang M.Q., Lee S. The Association Between Perceived Stress and Hypertension Among Asian Americans: Does Social Support and Social Network Make a Difference? J. Community Health. 2019;44(3):451–462. doi: 10.1007/s10900-018-00612-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makhubela M. Assessing psychological stress in south african university students: measurement validity of the perceived stress scale (pss-10) in diverse populations. Curr. Psychol. 2020 doi: 10.1007/s12144-020-00784-3. A Journal for Diverse Perspectives on Diverse Psychological Issues. [DOI] [Google Scholar]
- Masjoudi M., Aslani A., Seifi M., Khazaeian S., Fathnezhad-Kazemi A. Association between perceived stress, fear and anxiety of COVID 19 with self-care in pregnant women: a cross-sectional study. Psychol. Health Med. 2021:1–12. doi: 10.1080/13548506.2021.1894344. [DOI] [PubMed] [Google Scholar]
- Masters G.A., Asipenko E., Bergman A.L., Person S.D., Brenckle L., Moore Simas T.A., Ko J.Y., Robbins C.L., Byatt N. Impact of the COVID-19 pandemic on mental health, access to care, and health disparities in the perinatal period. J. Psychiatr. Res. 2021;137:126–130. doi: 10.1016/j.jpsychires.2021.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayopoulos G.A., Ein-Dor T., Dishy G.A., Nandru R., Chan S.J., Hanley L.E., Kaimal A.J., Dekel S. COVID-19 is associated with traumatic childbirth and subsequent mother-infant bonding problems. J. Affect. Disord. 2021;282:122–125. doi: 10.1016/j.jad.2020.12.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda A.R., Rivadero L., Bruera J.Á., Villarreal V., Bernio L.Y., de Los Ángeles Baydas L., Brizuela M.L., Serra S.V. Examining the Relationship Between Engagement and Perceived Stress-Related Cognitive Complaints in the Argentinian Working Population. Eur. J. Psychol. 2020;16(1):12–31. doi: 10.5964/ejop.v16i1.1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda A.R., Scotta A.V., Méndez A.L., Serra S.V., Soria E.A. Public sector workers' mental health in Argentina: comparative psychometrics of the perceived stress scale. J. Prev. Med. Public Health. 2020;53(6):429–438. doi: 10.3961/jpmph.20.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda A.R., Scotta A.V., Cortez M.V., Soria E.A. Triggering of postpartum depression and insomnia with cognitive impairment in Argentinian women during the pandemic COVID-19 social isolation in relation to reproductive and health factors. Midwifery. 2021;102 doi: 10.1016/j.midw.2021.103072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molgora S., Accordini M. Motherhood in the time of coronavirus: the impact of the pandemic emergency on expectant and postpartum women's psychological well-being. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.567155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen A.J., Haroz E.E., Mendelson T., Bass J. Symptom endorsement and sociodemographic correlates of postnatal distress in three low income countries. Depress. Res. Treat. 2016;2016 doi: 10.1155/2016/1823836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oskovi-Kaplan Z.A., Buyuk G.N., Ozgu-Erdinc A.S., Keskin H.L., Ozbas A., Moraloglu Tekin O. The effect of COVID-19 pandemic and social restrictions on depression rates and maternal attachment in immediate postpartum women: a preliminary study. Psychiatr. Q. 2021;92(2):675–682. doi: 10.1007/s11126-020-09843-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrozo-Pupo J.C., Pedrozo-Cortés M.J., Campo-Arias A. Perceived stress associated with COVID-19 epidemic in Colombia: an online survey. Cad. Saude Publica. 2020;36(5) doi: 10.1590/0102-311x00090520. [DOI] [PubMed] [Google Scholar]
- Pérez-Salas C.P., Sirlopú D., Cobo R., Awad A. Análisis bifactorial de la escala de participación escolar en una muestra de estudiantes chilenos. Rev. Iberoam. Diagn. Eval. Aval. Psicol. 2019;3(52):27–39. [Google Scholar]
- Perry C.P.B., da Cunha A.C.B., de Albuquerque K.A., et al. Motherhood and COVID-19: a digital psychoeducational booklet for the coping with the pandemic stressors. Trends Psychol. 2021;29:436–455. doi: 10.1007/s43076-021-00072-4. [DOI] [Google Scholar]
- Perzow S., Hennessey E.P., Hoffman M.C., Grote N.K., Davis E.P., Hankin B.L. Mental health of pregnant and postpartum women in response to the COVID-19 pandemic. J. Affect. Disord. Rep. 2021;4 doi: 10.1016/j.jadr.2021.100123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preis H., Mahaffey B., Heiselman C., Lobel M. Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Soc. Sci. Med. 2020;266(1982) doi: 10.1016/j.socscimed.2020.113348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puertas-Gonzalez J.A., Mariño-Narvaez C., Peralta-Ramirez M.I., Romero-Gonzalez B. The psychological impact of the COVID-19 pandemic on pregnant women. Psychiatry Res. 2021;301 doi: 10.1016/j.psychres.2021.113978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon D.C., Craver C. Effects of pregnancy loss on subsequent postpartum mental health: a prospective longitudinal cohort study. Int. J. Environ. Res. Public Health. 2021;18(4):2179. doi: 10.3390/ijerph18042179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis D., Lehr D., Heber E., Ebert D.D. The German version of the perceived stress scale (PSS-10): evaluation of dimensionality, validity, and measurement invariance with exploratory and confirmatory bifactor modeling. Assessment. 2019;26(7):1246–1259. doi: 10.1177/1073191117715731. [DOI] [PubMed] [Google Scholar]
- Ren J., Li X., Chen S., Chen S., Nie Y. The influence of factors such as parenting stress and social support on the state anxiety in parents of special needs children during the COVID-19 epidemic. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.565393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabárbara J., Lasheras I., Lipnicki D.M., Bueno-Notivol J., Pérez-Moreno M., López-Antón R., De la Cámara C., Lobo A., Gracia-García P. Prevalence of anxiety in the COVID-19 pandemic: an updated meta-analysis of community-based studies. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021;109 doi: 10.1016/j.pnpbp.2020.110207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saricali M., Satici S.A., Satici B., Gocet-Tekin E., Griffiths M.D. Fear of COVID-19, mindfulness, humor, and hopelessness: a multiple mediation analysis. Int. J. Ment. Health Addict. 2020:1–14. doi: 10.1007/s11469-020-00419-5. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satici S.A., Kayis A.R., Satici B., Griffiths M.D., Can G. Resilience, hope, and subjective happiness among the turkish population: fear of COVID-19 as a mediator. Int. J. Ment. Health Addict. 2020:1–16. doi: 10.1007/s11469-020-00443-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scotta A.V., Cortez M.V., Miranda A.R. Insomnia is associated with worry, cognitive avoidance and low academic engagement in Argentinian university students during the COVID-19 social isolation. Psychol. Health Med. 2020:1–16. doi: 10.1080/13548506.2020.1869796. [DOI] [PubMed] [Google Scholar]
- Şimşir Z., Koç H., Seki T., Griffiths M.D. The relationship between fear of COVID-19 and mental health problems: a meta-analysis. Death Stud. 2021:1–9. doi: 10.1080/07481187.2021.1889097. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Suárez-Rico B.V., Estrada-Gutierrez G., Sánchez-Martínez M., Perichart-Perera O., Rodríguez-Hernández C., González-Leyva C., et al. Prevalence of depression, anxiety, and perceived stress in postpartum Mexican women during the COVID-19 lockdown. Int. J. Environ. Res. Public Health. 2021;18(9):4627. doi: 10.3390/ijerph18094627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torales J., Ríos-González C., Barrios I., O'Higgins M., González I., García O., Castaldelli-Maia J.M., Ventriglio A. Self-perceived stress during the quarantine of COVID-19 pandemic in paraguay: an exploratory survey. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.558691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallejo M.A., Vallejo-Slocker L., Fernández-Abascal E.G., Mañanes G. Determining factors for stress perception assessed with the perceived stress scale (PSS-4) in Spanish and other European samples. Front. Psychol. 2018;9:37. doi: 10.3389/fpsyg.2018.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varma P., Junge M., Meaklim H., Jackson M.L. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: a global cross-sectional survey. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021;109 doi: 10.1016/j.pnpbp.2020.110236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vescovi G., Riter H.D.S., Azevedo E.C., Pedrotti B.G., Frizzo G.B. Parenting, mental health, and Covid-19: a rapid systematic review. Psicol. Teor. Prát. 2021;23(1):01–28. 10.5935/1980-6906/ePTPC1913554. [Google Scholar]
- Yağmur Y., Ulukoca N. Social support and postpartum depression in low-socioeconomic level postpartum women in Eastern Turkey. Int. J. Public Health. 2010;55(6):543–549. doi: 10.1007/s00038-010-0182-z. [DOI] [PubMed] [Google Scholar]
- Yarrington J.S., Lasser J., Garcia D., Vargas J.H., Couto D.D., Marafon T., Craske M.G., Niles A.N. Impact of the COVID-19 pandemic on mental health among 157,213 Americans. J. Affect. Disord. 2021;286:64–70. doi: 10.1016/j.jad.2021.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou B., Miao C., Chen J. Depression and perceived stress, but not anxiety, are associated with elevated inflammation in an obese adult population. Risk Manag. Healthc. Policy. 2020;13:1489–1497. doi: 10.2147/RMHP.S270359. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.