Abstract
Objectives
To investigate the perceptions and acceptability of a home-based exercise intervention in systemic lupus erythematosus (JSLE) and juvenile idiopathic arthritis (JIA) adolescent patients during the COVID-19 pandemic, and to explore the effects of the intervention on health-related quality of life (HRQoL), sleep quality, and mental health conditions parameters.
Methods
This was a randomized controlled trial of a 12-week, home-based exercise training program conducted between October and December 2020. During this period, social distancing measures were in place in Brazil to contain the spread of COVID-19. Adolescent patients diagnosed with JSLE and JIA participated in the study. Health-related qualitative and quantitative data were collected before and after the follow-up.
Results
21 JSLE patients and 30 JIA patients were analyzed. Six themes emerged from patients’ feedback: 1) Suitability of the home-based format; 2) Appropriate trainer supervision, 3) Motivators and facilitators for the program; 4) Barriers to the program; 5) Health benefits; 6) Patients’ suggestions to improve the program. Overall, data indicated that the intervention showed good acceptability and elicited improvements in the perceived HRQoL and fatigue in JIA and JSLE patients during the pandemic. However, further quantitative analyses with validated HRQoL, sleep quality, and mental health conditions instruments did not capture these benefits (p>0.05).
Conclusion
Our main findings based on in-depth qualitative assessments suggest that a home-based exercise training program was suitable and well-accepted by adolescents with JSLE and JIA during the COVID-19 pandemic. Nonetheless, adherence was not high, particularly among JIA patients, suggesting that facilitators and barriers identified in the current study should be explored to improve the quality of new home-based exercise programs implementation, particularly in a future emerging crisis.
Keywords: pediatric rheumatic diseases, physical activity, physical training, quality of life
List of abbreviations: coronavirus 2019 (COVID-19); health-related quality of life (HRQoL); juvenile idiopathic arthritis (JIA); juvenile systemic lupus erythematosus (JSLE); Pediatric Quality of Life Inventory (PedsQL); Pittsburgh sleep quality index (PSQI); Research Electronic Data Capture (REDCap®); Strengths and Difficulties Questionnaire’ (SDQ).
Introduction
It is estimated that three million children and adolescents globally are currently living with juvenile autoimmune rheumatic diseases, such as juvenile systemic lupus erythematosus (JSLE) and juvenile idiopathic arthritis (JIA).1 JSLE is an autoimmune disease characterized by immune dysregulation, formation of autoantibodies and immune complexes, resulting in inflammation and potential damage to a variety of organs.2 JIA encompasses all forms of arthritis beginning before 16 years of age and presenting specific symptoms, such as fever, rash, uveitis, and serositis.3 JSLE and JIA patients often present with higher rates of mental health issues, and low quality of life.4
Since March, 2020, the coronavirus 2019 (COVID-19) has been spreading throughout Brazil and has been responsible for more than 23 million infected Brazilians and more than 621,000 deaths as of January, 2022.5,6 In the beginning, to prevent the spread of COVID-19, schools were closed and in-person classes were suspended, directly affecting millions of Brazilian children and adolescents.7
Consequently, important decrease in physical activity levels8–16 and higher rates of mental health issues were reported during the pandemic in this population.17,18 Adolescents with juvenile rheumatic diseases usually present with higher prevalence of mental health issues compared to healthy counterparts.17,18 Another factor that might contribute to poor mental health in this population is an inactive lifestyle.19–21
To mitigate the negative effects of home confinement, strategies focused on promoting exercise have been suggested.22 In fact, studies have shown the therapeutic utility of exercise in patients with autoimmune rheumatic diseases,23,24 and home-based exercise programs have emerged as clinically effective and cost-effective strategies to improve general health across many clinical conditions.25–27 In the present study, our main objective was to investigate the perceptions and acceptability of a home-based exercise intervention in JSLE and JIA adolescent patients during the COVID-19 pandemic. As a secondary aim, we explored the effects of the intervention on health-related quality of life (HRQoL), sleep quality and mental health conditions using self-rated questionnaires.
Methods
Study design and patients
This was a randomized controlled trial conducted between October and December 2020. During this period, social distancing measures to contain the spread of COVID-19 were in place in Brazil. This study was part of larger project aimed at exploring potential therapeutic effects of exercise during COVID-19 pandemic among adolescents with a variety of chronic diseases (clinicaltrials.gov NCT04458246). Participants were recruited from the Pediatric Rheumatology Unit and Rheumatology Division of our university and tertiary referral hospital in Sao Paulo, Brazil. Adolescents aged between 10 and 19 years with JSLE and JIA were included in this study. Patients receiving treatment and care management at our center were asked for their consent to be included in repository of patients to be contacted for future research. The research team contacted all potential patients for recruitment and screening.
Inclusion criteria were 1) JSLE and according to the American College of Rheumatology (ACR) criteria28, 2) JIA according to the International League of Associations for Rheumatology (ILAR) criteria29 3) receiving treatment or follow-up at our university hospital, and 4) aged 10–19 years. Exclusion criteria were: 1) cardiovascular involvement (e.g., arrhythmias, arterial hypertension, heart failure, conduction disturbances, myocarditis, or pericarditis), 2) undernourishment, 3) kidney or pulmonary chronic diseases, or 4) engagement in any form of exercise for at least three months prior to and during the study. All patients obtained medical clearance to participate in the intervention. On the basis of feasibility, resources, capacity of research staff and facility, and patients’ availability,30,31 we selected 21 JSLE patients and 30 JIA patients to participate in this study. After completing all questionnaires, patients were randomized to either intervention or control group.
The Research Electronic Data Capture (REDCap®) was used to send questionnaires. REDCap® is a safe web instrument planned to support data capture for research studies. It also audits trails for tracking data control and allows automated data export procedures for statistical analyses. Participants were sent the REDCap link for the surveys and asked to complete all questionnaires. If surveys were incomplete, the research team followed up with emails or messages. Approximately six emails or messages were sent per subject to improve the response rate. The questionnaires were conducted in Portuguese. The study was approved by the local ethics committee (CONEP number 4.081.961) and the patients’ parents or guardians signed the online consent prior participation.
Home-based exercise program
The home-based exercise program consisted of a 12-weeks, three times a week aerobic and bodyweight exercise training program, which is thoroughly described elsewhere.32 Training sessions were divided into two parts. Initially, the warm-up included predominantly aerobic exercises such as jumping jacks, skipping, and mobility and flexibility exercises. The second part included bodyweight exercises for the major muscle groups such as squats, lunges, push-ups, crunches, and planks. Exercise sessions occurred three times a week. One weekly session was conducted with online live supervision with the trainer, whereas the other two weekly sessions were unsupervised, but patients were instructed to provide feedback to the trainer immediately after completion of the training session. Supervision/monitoring was conducted via WhatsApp® or Google Meets® according to patients’ preference. Progression occurred every four weeks by increasing the number of sets (3 to 4), repetitions (10 to 15) and/or duration (30 to 45 s). The exercises were modified every four weeks. Sessions included 1 to 5 patients at a time and adherence to the exercise program was monitored on a session basis by a member of the research staff.
Patients received instructional videos, photos, and “gifs” describing and illustrating the exercise program. Before the commencement of the training program, a videocall was conducted with all patients (and their parents, whenever necessary), individually, in order to provide all of the details necessary to perform the exercise training program and to collect information on patient’s health status.
Adherence to the training program was assessed by means of training log. Supervised sessions had immediate assurance of adherence by the trainer, whereas adherence to the unsupervised sessions was assessed via feedback provided by the patients immediately after completion of the training session.
Control group
Patients in the control group were asked to maintain their usual activities, and should communicate if there was any change in their routine during the time of the study.
Data collection
Qualitative data collection and analysis
Patients in the intervention group provided qualitative feedback about the program in two occasions: at the end of the first month and at the end of the third month of the program. Parents of younger patients who were actively involved in the program were also able to provide feedback. At the first qualitative data collection timepoint, a videocall with the trainer was conducted to understand patients’ initial perceptions about the program; the second one was performed via an open question using WhatsApp®. In these two time points, the following questions were asked: i) What did you like about the exercise training program? ii) What did you not like about the exercise training program? iii) How could the exercise training program be improved and what could have been done different to stimulate your engagement? iv) Did you feel any difference in your general health due to the exercise program? Patients’ feedback was transcribed verbatim in Portuguese and translated to English by trained bilingual and bicultural researchers. Content analysis was performed to identify themes.33
Strengths and Difficulties Questionnaire
The “Strengths and Difficulties Questionnaire” (SDQ) was used to evaluate symptoms of mental health disorder. It is a behavioral screening tool used to assess social, emotional, and physical aspects of behavior in young people 34 and it has been shown to be valid and reliable for completion by 11–16-year-old individuals.35 The questionnaire has 25 items which comprise five sub- scales: (i) emotional symptoms (anxiety and depressive symptoms); (ii) conduct problems; (iii) hyperactivity/inattention; (iv) peer relationship problems; and (v) prosocial behavior (positive behaviors such as being kind and helpful, scored in reverse of the other subscales). Response options are “not true, somewhat true, or certainly true” (scored 0, 1 or 2). The SDQ “Total Difficulties Score” (SDQ TDS) was generated by adding together the scores from the first four subscales and range from 0 (low difficulties) to 40 (high difficulties). The five subscales, whose scores can vary from 0 to 10, were also investigated independently. SDQ TDS provides a useful indicator of the level of symptoms of overall mental health disorder. In addition, the subscale items may be used to indicate specific clinical disorders in adolescents: depression, anxiety, hyperactivity attention deficit disorder (ADHD) and behavioral/conduct disorder. This questionnaire was translated and validated in the Portuguese language.36
Pediatric Quality of Life Inventory—PedsQL 4.0 Generic Core Scale
The PedsQL 4.037 is a tool to measure health-related quality of life (HRQOL) in healthy children and adolescents and in those with acute and chronic health conditions. This tool focuses on the following domains: physical (eight items), emotional (five items), social (five items), and school (five items) and it is administered to individuals between 2 and 25 years of age, with child self-report and parent proxy-report. All items for each of the forms are essentially identical, differing only in language. The answers are rated on a five-point scale (0=never, 1=almost never, 2=sometimes, 3=often, and 4=almost always). The items are inversely scored and transposed on a 0 to 100 scale (0=100, 1=75, 2=50, 3=25, and 4=0). Thus, the greater the score, the higher the quality of life. The total score is a sum of the scores across the four dimensions evaluated. The physical summary corresponds to the mean of the physical dimension (eight items), while the psychosocial summary (15 items) covers the emotional, social, and school domains. This tool was translated and validated in the Portuguese language.38
Pittsburgh sleep quality index (PSQI)
Sleep quality was assessed by the PSQI,39 which is a self-rated questionnaire assessing sleep quality and disturbances. The questionnaire is composed by 19 questions representing one of the seven components of sleep quality: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, sleep medication intake, and daytime dysfunction. Each component score was rated on a 3-point scale, leading to a sum of up to 21 points. A PSQI score > 5 indicate a poor sleep quality whereas a PSQI score ≤ 5 indicate good sleep quality.
Statistical analysis
The number of patients was chosen on the basis of feasibility, based on resources, capacity of research staff and facility, and available patients, in line with current recommendations.30 A linear mixed effects model was used to assess possible differences between groups, assuming fixed effects for Group and time, and random effects for participants. Significance level was d previously set at p ≤ 0.05. The lme4 package was used for linear mixed‐effects models. Data are expressed as mean ± SD, delta changes and 95% confidence interval (95%CI). Analyses were performed in RStudio version 4.02
Results
Participants’ characteristics
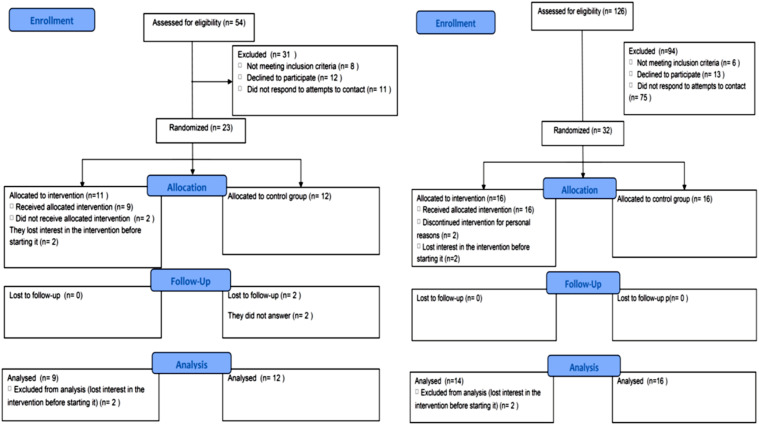
A total of 54 JSLE patients and 126 JIA patients were assessed for eligibility. Eight JSLE and 6 JIA patients were unable to participate due to physical limitations, 11 JSLE and 75 JIA patients did not respond to the recruitment contact, and 12 JSLE and 13 JIA patients declined to participate. During the follow-up period, two JSLE and 2 JIA patients lost interest in the intervention before starting it and were not analyzed as intention to treat, two JSLE in the control group did not complete the follow-up questionnaires, two JIA patients discontinued intervention for personal reasons. Therefore, 21 JSLE patients and 30 JIA patients remained and were evaluated (Figure 1). JSLE patients were 76% female; age: 15.8 ± 2.25 years; BMI: 23.1± 5.7 kg/m2; time elapsed since diagnosis: 6.45 ± 3.90 years. JIA patients were: 80% female; age: 14.5 ± 2.27 years; BMI: 24.3 ± 5.58 kg/m2; time elapsed since diagnosis: 5.20 ± 4.78 years (Table 1). Adherence to the exercise protocol was 76.7% and 44.8% for JSLE and JIA patients, respectively.
Figure 1.
Flow charts of patients with juvenile systemic lupus erythematosus and patients with juvenile idiopathic arthritis.
Table 1.
Patients’ demographic characteristics and disease-related parameters in patients with juvenile systemic lupus erythematosus and juvenile idiopathic arthritis.
| Characteristics | JSLE n= (21) | JIA n= (30) |
|---|---|---|
| Age (years) | 15.8 (2.25) | 14.5 (2.27) |
| Height (m) | 1.61 (0.09) | 1.58 (0.07) |
| Bodyweight (kg) | 61.1 (18.8) | 62.2 (15.6) |
| BMI (kg/m2) | 23.1 (5.27) | 24.3 (5.58) |
| Female, n (%) | 16 (76.1) | 24 (80) |
| Disease time (years) | 6.45 (3.90) | 5.20 (4.78) |
| Age at the disease onset (years) | 9.66 (3.48) | 9.36 (3.68) |
| Prednisone, n (%) | 11 (52%) | 3 (10%) |
| Dosage mg/day | 10 (5–22.5) | 10 (10–17.5) |
| Methotrexate, n (%) | 4 (19%) | 8 (27%) |
| Dosage mg/day | 17.5 (11.2–23.7) | 25 (20–25) |
| Leflunomide, n (%) | 1 (5%) | 11 (30%) |
| Dosage mg/day | 20 | 20 (20–20) |
| HCQ, n (%) | 20 (95%) | 1 (3%) |
| Dosage mg/day | 400 (200–400) | 200 (200–200) |
| Adalimumab n (%) | 0 (0) | 3 (%) |
| Dosage mg/day | 40 (40–40) | |
| Etanercept, n (%) | 0 (0) | 3 (10%) |
| Dosage mg/day | 50 (50–50) |
Values are described in mean (SD) or median ITQ (25–75). Abbreviations: JSLE: juvenile systemic lupus erythematosus; JIA: juvenile idiopathic arthritis; BMI: body mass index; HCQ: hydroxychloroquine.
Qualitative results
Eight patients with JSLE and 11 with JIA were included in the qualitative analysis (Tables 2, 3). Only one patient in each group did not provide qualitative feedback. Six themes emerged from patients’ feedback: 1) suitability of the home-based format; 2) appropriate trainer supervision; 3) motivators and facilitators for the program; 4) barriers to the program; 5) health benefits; and 6) patients’ suggestions to improve the program.
Table 2.
Perceptions of adolescents with systemic lupus erythematosus on a home-based exercise program during COVID-19 pandemic.
| Themes | JSLE Patient’s | Quotes |
|---|---|---|
| Suitability of the home-based format | I | “I liked that the program was online, if it was in-person I think that I would had difficulties to participate because I am very shy... But doing [exercising] at home pleased me very much.” |
| II | “The online format pleased me, and I found very pleasant training with the hospital team.” | |
| III | “I liked the online format.” | |
| IV | “The online sessions were good.” | |
| V | “I liked, the internet [connection] was not a problem” | |
| Appropriate trainer supervision | II | “I liked the teacher” |
| III | “I liked the trainer” | |
| IV | “I liked the trainer” | |
| V | “I liked to exercise with the trainer “ | |
| VI | “I liked the trainer” | |
| VII | “I liked the way the patients were treated in this program, the trainer was excellent, motivated [me] a lot.” | |
| Motivators and facilitators to the program | II | “I liked the exercises” |
| III | “I liked the online sessions, they were very good. And I liked some exercises” | |
| IV | “I found the exercises "cool", I liked to train. Before I used to dance jazz, twice a week, I miss these classes.” | |
| V | “I liked the exercises” | |
| VI | “I liked the exercises” | |
| VII | “I found the exercises relatively smooth” | |
| VIII | “I liked the exercises very much and they help me a lot.” | |
| Barriers of the program | I | “I am overwhelmed with school activities, and I was not able to deal with everything. I was feeling suffocated by it all. And the fact that I have to keep sending feedbacks did not help.” |
| II | “I felt a lot of pain the day after the first session. I did not like to do exercise in general, and something I felt lazy. And that got in the way a little bit.” | |
| III | “I did not like the group sessions” | |
| IV | “The school gets in the way a little, lots of classes and homework ... And also the [unstable] internet [connection] gets in the way sometimes.” | |
| VII | “It was difficult to do the exercises during midterms and finals. Also, I felt pain and tiredness because I was sedentary” | |
| VIII | “The thing that made it most difficult was my lack of time. I worked from 9 am until 7 pm, Sunday to Sunday, for part of the program.” | |
| Health benefits | I | “I improved a lot my mental health, I started to drink more water and also felt that I improve my sleep quality.” |
| II | “I felt that my sleep quality and health improved a lot.” | |
| III | “I felt differences in my health, and I lost weight too. Also, my sleep quality improved 50% and I felt more energy during my daily activities.” | |
| IV | “I was felt more energetic [during the program” | |
| V | “I felt that [the program] improved my concentration and self-esteem” | |
| VI | “I felt that [the program] improved my concentration and self-esteem” | |
| VII | “I felt that my health and my sleep improved a lot.” | |
| VIII | “I started to sleep better, and [the program] also improved my diet, I did not feel pain as I did before. And also, I improved my self-esteem and became more focused during the program.” | |
| Patients’ suggestions to improve the program | III | “I think we could do it more times a week.” |
| V | “It would be better if it was in-person” | |
| VI | “It would be better if it was in-person” | |
| VII | “I think it would be best if the parents participate in the exercises sessions, because we are children and if our parents are not ok, they will not take care of us in the way we need.” |
Table 3.
Perceptions of adolescents with juvenile idiopathic arthritis on a home-based exercise program during COVID-19 pandemic.
| Themes | JIA Patient’s | Quotes |
|---|---|---|
| Suitability of the home-based format | I | “I thought it was great, I managed to adapt well and I even prefer [to exercise] online.” |
| II | “I thought that the online sessions were good and I even prefer [the training] to be on the computer because I don't have to leave the house.” | |
| III | “I thought it was viable.” | |
| IV | “I liked the [home-based] format.” | |
| V | “I thought the online format was good, and I didn't have to pay to commute. I can do it [exercise] anywhere.” | |
| VI | “I really liked the online format, due to the pandemic it was also the only way.” | |
| VII | “I liked everything, the form of the training and the trainer” | |
| Appropriate trainer supervision | III | “The trainers were calm and always respected our time and difficulties” |
| VI | “The trainer was very good, very patient and clarified a lot of doubts, even during the week, via audios.” | |
| VII | “The trainer was very attentive” | |
| VIII | “I liked the teacher because she explained well the exercises” | |
| Motivators and facilitators to the program | I | “In this pandemic I did not have much to do, so I put dome effort in trying to get stronger” |
| II | “I found it to be fun, I think that exercise must be good for health” | |
| III | “I liked the training and the frequency.” | |
| VI | “The training frequency was good, because I had days off and also sometimes if I couldn't do it [exercise] on a day, I had Saturday or Sunday to do it. I also liked the type of training, some exercises were heavy, but I think it is necessary for the development and to gain more strength for t” | |
| VII | “The duration of each level of difficult was good [4 weeks]” | |
| VIII | I really liked the exercises presented, the training also made us more active, and the group format was really fun | |
| IX | “The classes were well designed so that we patients could engage in the classes very carefully, if we had any questions, we could ask ... I liked it because somehow I was taking care of my health, exercising.” | |
| X | “I liked to train because it was good to use my energy ... it was interesting to have more people in the group doing the exercises together. Doing it alone is more difficult” | |
| XI | “I really enjoyed being able to exercise and move. I enjoyed the group classes, I thought it was cool ... I really liked the exercises, I thought I was in great need and I intend to go to the gym afterwards.” | |
| XII | “I found it to be fun, and it's good for health.” | |
| Barriers of the program | I | “I didn’t like to feel pain after training, as I felt a lot of pain in my knee, every time I trained, I felt that the pain was getting worse ... I didn’t like group classes, I prefer when classes are in small groups or individuals because I’m ashamed, and I'm also worried about the clothes I'm wearing. Also, I felt pain in my knees” |
| II | “In the morning I have online classes and in the afternoon I take care of the horse's stable, and because of that I come back very tired because it is a very intense activity. I'm only doing the exercises when I don't go to the farm, I don't think I can handle it if I do both ... I get really sweaty, and it bothers me a little, and when it's too hot I get very tired and I can't exercise” | |
| III | “School and church take up a lot of my time. And also I did not like to do push ups, and I was lazy sometimes. I felt pain in my knees” | |
| IV | “The school gets in the way a little, lots of classes and homework ... And also the [unstable] internet [connection] gets in the way sometimes.” | |
| VII | “It was difficult to do the exercises during midterms and finals. Also, I felt pain and tiredness because I was sedentary” | |
| IX | “I liked it a lot, and if I had another opportunity that I didn't have with the disease activity high (arthritis), I would try again. If I felt pain, it was not because of the exercises, but because of my illness, the activity increased while I was doing the program activities.” | |
| X | “I didn't like to push my knee, and sometimes I felt tired. I felt pain in the knees doing the jumps. And also, I had a lot of homework and a lack of internet access at home.” | |
| XII | “I did not like doing arm exercises and I did not like to get tired ... The school activities were overwhelming and when the night comes, I just wanted to rest” | |
| XIII | “Our [internet] connection wasn’t very good so sometimes it wasn’t possible to participate in the classes. I felt pain in my ankles, and also swelling in the knees. I felt uncoordinated, I was ashamed to train, and I was very afraid of making the pain worse ... And also, I had to take care of my cousins, and could do the exercises online at night, but I was not motivated to do the exercises. I was always tired. In addition, in my house, I did not have space to do the exercises too.” | |
| Health benefits | III | “I felt more energetic” |
| IV | “I felt better, at first I felt more tired, but now not so much.” | |
| VI | “It was very good for my sleep, since the exercises started, my sleep improved, I stopped waking up at night. My concentration improved in my studies, I was less distracted. It improved my self-esteem, general health and decreased my fatigue, I was very happy with that. I feel more comfortable with my body to go out.” | |
| VII | “I I felt my mood improve a lot, and I also felt that my agility improved.” | |
| VIII | “During the training period, I was more willing to do the daily physical activities and to play sports.” | |
| IX | “My sleep improved a little, my diet too, some days I had less energy, but others I had more energy.” | |
| XI | “My health in general improved a lot, sleep improved, concentration also” | |
| XIII | “I felt safer to do squats.” | |
| XIV | “I felt a lot of difference because before [the training] I couldn't make many movements that now I can” | |
| Patients’ suggestions to improve the program | I | “I would like more online sessions.” |
| V | “I wouldn't need online sessions, I could do it using the booklet” | |
| VI | “Could be more people in the online sessions, I liked the group interaction, I think it’s cool. | |
| X | “I wish there was less training during the week. It's a lot 3x in the week, I feel frustrated when I don't do it” | |
| XII | “I would like more online sessions.” | |
| XIII | “I am afraid to do the exercises alone. When I am in the online session with the trainer, I feel more secure, because I know she is correcting me and so I am doing it correctly. I would like more online sessions. Would be nice to have some in-person sessions” |
Suitability of the home-based format
Patients with JSLE and JIA reported the home-based exercise program to be appropriate for performing during the COVID-19 pandemic. JSLE patients reported that the online format was good, and one patient even reported that the online format made her comfortable as she considers herself as a shy person, and this format made her enjoy exercising. JIA patients also reported adapting well to the online format, they reported the ability to do it “anywhere” as a positive feature. One patient reported preferring this format over in-person training.
I liked that the program was online, if it was in-person I think that I would had difficulties to participate because I am very shy… But doing [exercising] at home pleased me very much.—Female JSLE patient, 16 years old
I really liked the online format, due to the pandemic it was also the only way [to participate in the program].—Female JIA patient, 19 years old
Appropriate trainer supervision
In general, patients reported liking the research staff that delivered the exercise training. Patients reported that the team was attentive and explained the exercises well. JSLE patients in general reported to like the trainer (six out of nine), and one patient reported that the trainer was attentive to the patients. Three JIA patients reported that the trainer was very good and explained the exercises very well.
I liked the way the patients were treated in this program, the trainer was excellent, motivated [me] a lot.—Female LESJ patient, 13 years old
The trainer was very good, very patient and clarified a lot of doubts, even during the week [on non-training days], via audios.—Female JIA patient, 19 years old
Motivators and facilitators to the program
Most patients reported that they enjoyed the exercises. A few exercises were less preferred than others such as squatting and push-ups. For JSLE patients, group classes, frequency of exercises and enjoying training were the main facilitators. In addition, some patients with JIA cited the fact that exercising is beneficial for health and a way to joyfully expend energy. One JIA patient reported that as she had no other activity to engage in during quarantine, she focused on getting stronger. JIA patients also reported that the training frequency was good, as they had some days to rest. They also mentioned the possibility of exercising during the weekend if they could not exercise on a weekday.
I liked the frequency of the exercise sessions. I also liked the exercises. And I liked the fact that even we are in a pandemic, we got to have this help. And I loved that the patients could do the sessions together.—Female JSLE patient, 13 years old
The classes were well designed so that we patients could engage in the classes very carefully, if we had any questions, we could ask … I liked it because somehow, I was taking care of my health, by exercising.—Female JIA patient, 16 years old
Barriers to the program
For patients with JSLE, the main barrier was being overwhelmed by activities (online school, helping in home and others). In addition to studying, two patients also had to work, and others stated they were overworked due to school obligations. One patient with JSLE reported the group classes as a barrier, one reported having problems with internet connection, and one patient reported that sometimes she was not motivated to engage in the sessions because she does not like to exercise. One patient with JSLE reported feeling a lot of pain, but only in the first training session. Another patient with JSLE reported pain and increased tiredness but she associated it with the fact she was sedentary. For patients with JIA, in addition to being involved in multiple activities, some patients reported not liking some of the exercises. One patient reported perceiving she was not doing the exercises the right way and that she was also afraid that exercising incorrectly could worsen her usual pain. Two patients reported having problems with the internet. One JIA patient reported many barriers, among them: taking care of cousins, tiredness, and lack of coordination. One patient reported that she had to stop exercising due to high disease activity. Five patients with JIA reported feeling pain, four in the knee and one in the knee and ankle.
I am overwhelmed with school activities, and I was not able to deal with everything. I was feeling suffocated by it all. And the fact that I had to keep sending feedbacks did not help—Female JSLE patient, 16 years old
Our [internet] connection wasn’t very good so sometimes it wasn’t possible to participate in the classes… I felt uncoordinated, I was ashamed to train, and I was very afraid of making the pain worse … And also, I had to take care of my cousins, and could do the exercises online at night, but I was not motivated to do the exercises. I was always tired. In addition, in my house, I did not have space to do the exercises too.—Female JIA patient, 13 years old.
Health benefits
Some participants reported improvements in health after completing the program. Patients reported better sleep quality, motivation, and concentration. Some patients also reported that they felt higher self-esteem, and that they felt more confident doing some movements. Two patients (one patient with JSLE and one with JIA) also reported that they improved their diet after they started training.
I improved a lot my mental health, I started to drink more water and also felt that I improve my sleep quality.—Female JSLE patients, 16 years old.
It was very good for my sleep, since the exercises started, my sleep improved, I stopped waking up at night. My concentration improved in my studies, I was less distracted. It improved my self-esteem, general health and decreased my fatigue, I was very happy with that. I feel more comfortable with my body to go out.—Female JIA patient, 19 years old.
Patients’ suggestions to improve the program
Two JSLE patients mentioned that they would prefer the training to be in person, but acknowledged that due to the pandemic it was not a possible option. Another JSLE patient suggested that it would be good if more online sessions were offered. Another patient also thought that it would be important to have parents exercising with the patient, because in the patient's perception, if the parents are not well, they are not able to take care of their children. One patient cited his preference of doing the exercises alone, without online supervision. For JIA patients, however, some suggestions were conflicting. There were patients who would like more online sessions, and one patient suggested that it would be positive to have some face-to-face sessions. But at the same time there was a patient who wanted less training sessions during the week, and another patient preferred not to have online sessions. One patient reported that she was afraid to exercise on her own, and she preferred to have all sessions online, as she felt safer. One patient suggested that it would be nice to have more patients in the online session.
I think we could train more times a week—Female JSLE patient, 12 years old.
I wish there was less training during the week. It's a lot 3x in the week, I feel frustrated when I don't do it—Female JIA patient, 11 years old
Quantitative results
The mean (95% confidence interval) of SDQ TDS, PedsQL domains, and PSQI scores did not significantly change at baseline compared to after intervention (p>0.05) (Tables 4, 5).
Table 4.
Effects of a 12-week home-based exercise training program on Strengths and Difficulties Questionnaire (SDQ), Pediatric Quality of Live Inventory 4.0 (PedsQL 4.0), and Pittsburgh Sleep Quality Index (PSQI) in adolescents with systemic lupus erythematosus.
| Control Group | Intervention Group | p value | |||||
|---|---|---|---|---|---|---|---|
| Domains (score) | Mean Baseline (95% CI) | Mean Post (95% CI) | Mean Baseline (95% CI) | Mean Post (95% CI) | TIME | GROUP | INT |
| Strengths and Difficulties Questionnaire | |||||||
| Total difficulties score (0; 40) | 11.0 (6.7; 15.2) | 9.8 (5.49; 14.2) | 18.4 (13.5; 23.3) | 16.1 (11.2; 21.0) | 0.16 | 0.02 | 0.64 |
| Emotional problems (0; 10) | 4.2 (2.5; 5.8) | 3.40 (1.70; 5.0) | 5.9 (3.9; 7.8) | 4.8 (2.9; 6.8) | <0.01 | 0.19 | 0.69 |
| Conduct problems (0; 10) | 1.9 (1.0; 2.8) | 1.23 (0.3; 2.1) | 2.5 (1.5; 3.5) | 2.8 (1.8; 3.9) | 0.58 | 0.06 | 0.11 |
| Hyperactivity/inattention (0; 10) | 3.0 (1.3; 4.6) | 2.8 (1.1; 4.4) | 5.8 (4.0; 7.7) | 5.3 (3.4; 7.2) | 0.43 | 0.02 | 0.69 |
| Peer problems (0; 10) | 1.9 (0.9; 2.9) | 2.2 (1.3; 3.4) | 3.0 (1.8; 4.1) | 3.0 (1.8; 4.1) | 0.43 | 0.24 | 0.43 |
| Prosocial (0; 10) | 7.6 (6.42; 8.9) | 8.7 (7.5; 10.0) | 8.0 (6.5; 9.4) | 8.1 (6.6; 9.5) | 0.08 | 0.70 | 0.14 |
| Impact score (0; 10) | 0.9 (0.01; 1.8) | 1.3 (0.39; 2.2) | 1.5 (0.5; 2.6) | 1.6 (0.6; 2.7) | 0.40 | 0.42 | 0.64 |
| Pediatric Quality of Life Inventory | |||||||
| PedsQL total scale score (0; 100) | 72.3 (63.0; 81.7) | 78.5 (69.2; 87.9) | 65.9 (55.1; 76.7) | 66.6 (55.8; 77.4) | 0.24 | 0.36 | 0.36 |
| Physical health summary score (0; 100) | 71.1 (60.1; 82.1) | 81.5 970.5; 92.5) | 69.8 (56.4; 81.8) | 69.1 (56.4; 81.8) | 0.11 | 0.38 | 0.07 |
| Emotional functioning (0; 100) | 65.4 (52.4; 78.5) | 61.25 (48.2; 74.3) | 49.4 (34.4; 64.5) | 55.6(40.5; 70.6) | 0.78 | 0.24 | 0.15 |
| Social functioning (0; 100) | 87.5 (76.4; 98.6) | 88.7 9(77.6; 99.8) | 78.33 (65.5; 91.1) | 78.9 (66.1; 91.7) | 0.83 | 0.20 | 0.93 |
| School functioning (0; 100) | 67.9 (57.1; 78.7) | 76.82 (65.9; 87.4) | 57.78 (45.3;70.2) | 57.8 (45.3;70.2) | 0.33 | 0.04 | 0.33 |
| Psychosocial health summary (0; 100) | 73.6 (63.9;83.2) | 76.4 (65.9 85.2) | 61.8 (50.7; 73.0) | 64.1 (52.9; 75.2) | 0.51 | 0.08 | 0.96 |
| Pittsburgh sleep quality index | |||||||
| PSQI total score (0; 21) | 4.3 (2.4; 6.2) | 4.8 (2.9; 6.8) | 6.0 (3.8; 8.2) | 6.9 (4.6; 9.0) | 0.30 | 0.16 | 0.78 |
| Overall sleep quality (0; 3) | 1.0 (0.5; 1.5) | 0.7 (0.2; 1.2) | 1.2 (0.6; 1.7) | 1.0 (0.4; 1.5) | 0.20 | 0.57 | 0.83 |
| Sleep latency (0; 3) | 0.6 (0.1; 1.1) | 0.8(0.3; 1.4) | 0.6 (0.06; 1.2) | 1.0 (0.3; 1.6) | 0.28 | 0.87 | 0.84 |
| Sleep duration (0; 3) | 0.08 (−0.2;0.3) | 0.45 (0.1; 0.7) | 0.3 ( −0.004; 0.6) | 0.2 (−0.1;0.5) | 0.30 | 0.95 | 0.06 |
| Sleep efficiency (0; 3) | 0.1( −0.4;0.7) | 0.4 ( −0.1; 1.0) | 0.6 (−0.005; 1.3) | 1.3 (0.6;2.0) | 0.07 | 0.07 | 0.50 |
| Sleep disturbances (0; 3) | 1.3 (0.9; 1.6) | 1.1 (0.8; 1.5) | 1.22 (0.8; 1.6) | 1.1 (0.7; 1.5) | 0.44 | 0.66 | 0.89 |
| Sleep medication use (0; 3) | 0.42 (−0.3; 1.1) | 0.35 (−0.3; 1.0) | 1.33 (0.5; 2.1) | 1.0 (0.1; 1.8) | 0.34 | 0.13 | 0.51 |
| Daytime dysfunction (0; 3) | 0.5 (0.2;0.9) | 0.7 (0.4;1.1) | 0.5 (0.4; 1.1) | 1.2 (0.7; 1.6) | <0.01 | 0.40 | 0.13 |
Values are described in mean (95 confidence interval). Abbreviations: INT: interaction. JSLE: juvenile systemic lupus erythematosus
Table 5.
Effects of a 12-week home-based exercise training program on Strengths and Difficulties Questionnaire (SDQ), Pediatric Quality of Live Inventory 4.0 (PedsQL 4.0), and Pittsburgh Sleep Quality Index (PSQI) in adolescents with juvenile idiopathic arthritis.
| Control group | Intervention group | p value | |||||
|---|---|---|---|---|---|---|---|
| Domains (score) | Mean baseline (95% CI) | Mean post (95% CI) | Mean baseline (95% CI) | Mean post (95% CI) | TIME | GROUP | INT |
| Strengths and Difficulties Questionnaire | |||||||
| Total difficulties score (0; 40) | 15.0 (11.9; 18.0) | 13.8 (10.7; 16.8) | 14.6 (11.4; 17.8) | 13.2 (9.9; 16.4) | 0.33 | 0.78 | 0.93 |
| Emotional problems (0; 10) | 4.7 (3.5; 5.9) | 4.0 (2.8; 5.2) | 4.3 (3.0; 5.6) | 4.7 (3.4; 6.0) | 0.82 | 0.80 | 0.33 |
| Conduct problems (0; 10) | 2.5 (1.5; 3.4) | 2.8 (1.9; 3.7) | 3.2 (2.2; 4.2) | 2.0 (1.0; 2.9) | 0.30 | 0.88 | 0.05 |
| Hyperactivity/inattention (0; 10) | 4.7 (3.5; 5.9) | 4.0 (2.7; 5.2) | 4.8 (3.5; 6.1) | 4.2 (2.9; 5.5) | 0.26 | 0.77 | 0.88 |
| Peer problems (0; 10) | 2.6 (1.6; 3.6) | 2.8 (1.8; 3.8) | 2.2 (1.1; 3.2) | 2.1 (1.0; 3.1) | 0.89 | 0.30 | 0.76 |
| Prosocial (0; 10) | 8.1 (7.0; 9.1) | 6.9 (5.9; 7.9) | 8.1 (7.0; 9.2) | 8.5 (7.4; 9.6) | 0.46 | 0.15 | 0.12 |
| Impact score (0; 10) | 0.94 (0.1; 1.7) | 0.19 (−0.5; 0.9) | 1.9 (1.0; 2.7) | 0.7( −0.04; 1.6) | 0.01 | 0.08 | 0.58 |
| Pediatric Quality of Life Inventory | |||||||
| PedsQL total scale score (0; 100) | 72.4 (64.9; 80.0) | 78.0(70.5; 85.6) | 63.1 (55.0; 71.2) | 64.5 (56.4; 72.6) | 0.29 | 0.01 | 0.52 |
| Physical health summary score (0; 100) | 76.3 (66.0; 86.7) | 74.4(64.0; 84.7) | 65.4 (54.3; 76.4) | 64.9 (53.8; 76.0) | 0.79 | 0.10 | 0.86 |
| Emotional functioning (0; 100) | 60.0 (51.5; 68.4) | 79.0 (70.6; 87.5) | 50.7 (41.6; 59.7) | 57.8 (48.8; 66.8) | <0.01 | <0.01 | 0.14 |
| Social functioning (0; 100) | 80.6 (72.9; 88.2) | 89.0 (81.4; 96.7) | 75.0 (66.8; 83.1) | 77.1 (68.9; 85.3) | 0.18 | 0.03 | 0.42 |
| School functioning (0; 100) | 65.0 (55.6; 74.3) | 77.1(67.8; 86.4) | 57.1 (47.1; 67.0) | 57.5 (47.5; 67.4) | 0.15 | 0.01 | 0.17 |
| Psychosocial health summary (0; 100) | 68.5 (61.9; 75.0) | 81.7 (75.2; 88.3) | 60.9 (53.9; 67.9) | 64.1 (57.1; 71.1) | 0.01 | <0.01 | 0.12 |
| Pittsburgh sleep quality index | |||||||
| PSQI total score (0; 21) | 5.3 (3.8; 6.9) | 3.1 (1.5; 4.6) | 6.4 (4.7; 8.0) | 4.2 (2.6; 5.9) | <0.01 | 0.94 | 0.66 |
| Overall sleep quality (0; 3) | 1. 0 (0.6; 1.3) | 0.6 (0.3; 1.0) | 1.0 (0.72; 1.4) | 0.64 (0.2; 0.9) | <0.01 | 0.76 | 0.66 |
| Sleep latency (0; 3) | 1.0 (0.6;1.4) | 0.6 (0.2; 1.0) | 1.5 (1.0; 1.9) | 0.8 (0.4; 1.2) | 0.01 | 0.14 | 0.61 |
| Sleep duration (0; 3) | 0.3 (0.007; 0.6) | 0.06 (−0.2; 0.3) | 0.50 (0.1; 0.8) | 0.2 ( −0.04; 0.6) | 0.09 | 0.25 | 0.89 |
| Sleep efficiency (0; 3) | 0.6 (0.1; 1.0) | 0.50 (0.03; 0.9) | 0.7 (0.2; 1.2 | 0.36 (−0.1; 0.8) | 0.25 | 0.97 | 0.53 |
| Sleep disturbances (0; 3) | 1.0 (0.9; 1.1) | 0.8 (0.7; 1.0) | 1.0 (0.9; 1.2) | 1.0 (0.8; 1.1) | 0.05 | 0.33 | 0.36 |
| Sleep medication use (0; 3) | 0.6 (0.1; 1.2) | 0.1 ( −0.4; 0.6) | 0.7 (0.1; 1.2) | 0.7 (0.1; 1.2) | 0.21 | 0.34 | 0.21 |
| Daytime dysfunction (0; 3) | 0.6 (0.2; 0.9) | 0.2 (−0.09; 0.5) | 0.7 (0.4; 1.1) | 0.4 (0.06; 0.7) | 0.04 | 0.34 | 0.96 |
Values are described in mean (95 confidence interval). INT: interaction; JIA: juvenile idiopathic arthritis
Discussion
Our main findings based on in-depth qualitative assessments suggest that a home-based exercise training program was suitable to and well-accepted by adolescents with JSLE and JIA during the COVID-19 pandemic.
Due to the pandemic, home-based exercise intervention has been the only form of exercise possible to be delivered to our patients. The positive intervention’s acceptability by our patients shows that this type of exercise program can meet with the expectations of adolescents with JSLE and JIA. Home-based exercise interventions have gathered more popularity among practitioners and clinicians in the past years, and even more due to the COVID-19 pandemic. Rapid advances in mobile technologies have allowed for improvements in intervention delivery and patient supervision.40
One important theme that emerged in our assessment was the quality of the trainer supervision, with most of the patients reporting positive connection with their trainers. Bonding with healthcare workers is an important factor in maintaining a patient’s adherence. Gherman et al.41 indicated that patients who had a good and regular bond with healthcare workers were better at following medical advice and contributing to the treatment process. Aside from the trainer, patients also reported other motivators and facilitators, such as: the exercises, group classes, the belief that participating in the program would be good for their health, and the fact that the program was fun and a good way to expend energy. Emphasizing these facilitators may help increase the long-term adherence to this type of program.
Patients also reported some barriers to adherence, with the lack of time for training due to conflict with school obligations being a major one in both JIA and JSLE groups. For patients with JIA specifically, in addition to over commitment, some patients reported not liking some exercises. Also, one patient reported fear of exacerbating pre-existent pain. Pre-pandemic studies have shown similar barriers in patients with JIA.42,43 Also, a recent study conducted by Ng et al.44 conducted during the pandemic found that apparently healthy adolescents may face similar barriers to engagement in physical activity to those reported in the current study, such as: health concerns, low motivation, school closing, too much schoolwork, lack of resources, poor mental health, lack of time, and lack of routine.
Of relevance, patients in our study perceived that the program improved several aspects of their mental and physical health, despite the fact that no differences were found in the quantitative tools. Despite being somewhat inconsistent, it may suggest that the intervention achieved a practical success. According to Ayres,45 practical success refers to success achieved from the patient’s point of view, and technical success refers to a success expected from a clinical point of view.45 Within the clinical practice, the two concepts are not interchangeable. For example, it would be expected that the patients with low adherence, such as those with JIA in the present study, would not perceive benefits; however, they did report several benefits that quantitative questionnaires were not able to capture. From a clinical standpoint, therefore, practical success is of great value.
It is worth mentioning the conflicting suggestions to improve the program made by some patients. For example, there were patients who suggested more online classes, whereas others suggested reducing them. This data points out that participants have their own preferences regarding type of exercise, frequency, and intensity, which suggests that there might be no “one-size-fits-all” exercise program in this scenario. An important suggestion made by one of the patients was the parents’ engagement in the program. In fact, parental/family support in promoting physical activity during normal life and challenging health situations, such as the current pandemic, appears to be relevant to improve youth’s adherence.46 This is a point to be considered in the implementation of new exercise programs for these populations.
In this study, adherence was not high, particularly among JIA patients, suggesting that facilitators and barriers identified herein should be explored to improve the quality of new home-based exercise programs for these groups. In this regard, a new type of intervention that could suit pediatric groups is video games–based, task-oriented training, which was shown to be feasible and effective in improving physical function in JIA patients.47 Virtual reality–based programs should be compared with traditional exercise interventions in terms of adherence and efficacy for patients with pediatric rheumatic diseases.
The limitations of this study included the relatively low sample size, which is particularly problematic for the quantitative analyses; the relatively short-term follow-up; the lack of objective assessments of physical capacity, functioning, and overall clinical and laboratory status; and the biases inherent to the use of questionnaires to assess quality of life and sleep, and mental health.
In conclusion, our data indicates that a home-based exercise training program showed good acceptability and elicited improvements in the perceived quality of life and fatigue in JIA and JSLE patients during the pandemic, although quantitative analyses did not detect these benefits. Further studies should explore ways to improve exercise adherence in these populations.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Sofia Mendes Sieczkowska https://orcid.org/0000-0002-4869-318X
Lucia Maria Arruda Campos https://orcid.org/0000-0001-9653-0468
Rosa Maria Rodrigues Pereira https://orcid.org/0000-0002-3723-5028
Nadia Emi Aikawa https://orcid.org/0000-0002-7585-4348
Clovis Artur Silva https://orcid.org/0000-0001-9250-6508
References
- 1.Dave M, Rankin J, Pearce M, et al. Global prevalence estimates of three chronic musculoskeletal conditions: Club foot, juvenile idiopathic arthritis and juvenile systemic lupus erythematosus. Pediatr Rheumatol 2020; 18: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Habibi S, Saleem MA, Ramanan A V. Juvenile systemic lupus erythematosus: Review of clinical features and management. Indian Pediatr 2011; 48: 879–887. [DOI] [PubMed] [Google Scholar]
- 3.Ravelli A, Martini A. Juvenile idiopathic arthritis. Lancet 2007; 369: 767–778. [DOI] [PubMed] [Google Scholar]
- 4.Rubinstein TB, Davis AM, Rodriguez M, et al. Addressing mental health in pediatric rheumatology. Curr Treat Options Rheum 2018; 4: 55–72. [Google Scholar]
- 5.Ortega F, Orsini M. Governing COVID-19 without government in Brazil : Ignorance , neoliberal authoritarianism , and the collapse of public health leadership Governing COVID-19 without government in Brazil : Ignorance. Glob Public Health 2020; 15: 1257–1277. [DOI] [PubMed] [Google Scholar]
- 6.Saúde SE de. Updated data on coronavirus cases in Brazil, https://covid.saude.gov.br/ (2020).
- 7.Unesco . Education: From disruption to recovery, https://en.unesco.org/covid19/educationresponse (2020).
- 8.Safadi MAP, Silva CAA. The challenging and unpredictable spectrum of covid-19 in children and adolescents. Rev Paul Pediatr; 39. Epub ahead of print2020. 10.1590/1984-0462/2020/38/2020192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U. S . BMC Public Health 2020; 20: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peçanha T, Goessler KF, Roschel H, et al. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Hear Circ Physiol 2020; 318: H1441–H1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rezende DAN, Pinto AJ, Goessler KF, et al. Influence of Adherence to Social Distancing Due to the COVID-19 Pandemic on Physical Activity Level in Post-bariatric Patients. Obes Surg 2020; 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goessler KF, Nicoletti CF, Augusto D, et al. Obesity Outpatient Screening of Health Status Among Postbariatric Patients during the COVID-19 Pandemic in Sao Paulo. Obesity 2020; 28: 2263–2264. [DOI] [PubMed] [Google Scholar]
- 13.Pinto A, Rezende D, Sieczkowska S, et al. Increased prolonged sitting in rheumatoid arthritis patients during the COVID-19 pandemic: a within-subjects, accelerometer-based study. medRxiv 2020; 9: 20191395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hall Grenita, Laddu Deepika R, Phillips Shane A. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis 2020; S0033-0620: 30077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.López-Gil JF, Tremblay MS, Brazo-Sayavera J. Changes in Healthy Behaviors and Meeting 24-h Movement Guidelines in Spanish and Brazilian Preschoolers, Children and Adolescents during the COVID-19 Lockdown. Children 2021; 8: 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sá C, Pombo A, Luz C, et al. Covid-19 social isolation in Brazil : effects on the physical activity routine of families with children. Rev Paul Pediatr 2021; 39: e2020159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ravens-Sieberer U, Kaman A, Erhart M, et al. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur Child Adolesc Psychiatry 2021: 1–11. 10.1007/s00787-021-01726-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tang S, Xiang M, Cheung T, et al. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J Affect Disord 2021; 279: 353–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pinto AJ, Roschel H, Benatti FB, et al. Poor agreement of objectively measured and self-reported physical activity in juvenile dermatomyositis and juvenile systemic lupus erythematosus. Clin Rheumatol 2016; 35: 1507–1514. [DOI] [PubMed] [Google Scholar]
- 20.Pinto AJ, Miyake CNH, Benatti FB, et al. Reduced Aerobic Capacity and Quality of Life in Physically Inactive Patients With Systemic Lupus Erythematosus With Mild or Inactive Disease. Arthritis Care Res 2016; 68: 1780–1786. [DOI] [PubMed] [Google Scholar]
- 21.Fazaa A, Sellami M, Ouenniche K, et al. Physical activity assessment in children and adolescents with juvenile idiopathic arthritis compared with controls. Arch Pediatr 2021;28(1):47–52. 10.1016/j.arcped.2020.10.008. [DOI] [PubMed] [Google Scholar]
- 22.Silva CA, Queiroz LB, Fonseca CB, et al. Spotlight for healthy adolescents and adolescents with preexisting chronic diseases during the COVID-19 pandemic. Clinics 2020; 75: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gualano B, Bonfa E, Pereira RMR, et al. Physical activity for paediatric rheumatic diseases: Standing up against old paradigms. Nat Rev Rheumatol 2017; 13: 368–379. [DOI] [PubMed] [Google Scholar]
- 24.Gualano B, Sá Pinto AL, Perondi B, et al. Evidence for prescribing exercise as treatment in pediatric rheumatic diseases. Autoimmunity Reviews 2010; 9: 569–573. [DOI] [PubMed] [Google Scholar]
- 25.Sieczkowska SM, Smaira FI, Mazzolani BC, et al. Efficacy of home-based physical activity interventions in patients with autoimmune rheumatic diseases: a systematic review and meta-analysis. Semin Arthritis Rheum 2021; 51: 576–587. [DOI] [PubMed] [Google Scholar]
- 26.Thomas RJ, Beatty AL, Beckie TM, et al. Home-based cardiac rehabilitation: A scientific statement from the american association of cardiovascular and pulmonary rehabilitation, the american heart association, and the american college of cardiology. Circulation 2019; 140: e69–e89. 10.1161/CIR.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 27.Chien C-L, Lee C-M, Wu Y-W, et al. Home-based exercise improves the quality of life and physical function but not the psychological status of people with chronic heart failure: a randomised trial. J Physiother 2011; 57: 157–163. [DOI] [PubMed] [Google Scholar]
- 28.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 1997: 1725. 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 29.Petty RE, Southwood TR, Manners P, et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol 2004; 31: 390–392. [PubMed] [Google Scholar]
- 30.Bacchetti P, McCulloch CE, Segal MR. Simple, defensible sample sizes based on cost efficiency. Biometrics 2008: 577–585. 10.1111/j.1541-0420.2008.01004_1.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bacchetti P. Current sample size conventions: Flaws, harms, and alternatives. BMC Med 2010: 1–7. 10.1186/1741-7015-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marques IG, Astley C, Sieczkowska SM, et al. Lessons learned from a home-based exercise program for adolescents with pre-existing chronic diseases during the COVID-19 quarantine in Brazil. Clinics 2021;75. 10.6061/clinics/2021/e2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hsieh H, Shannon S. Three approaches to qualitative content analysis. Qual Health Res 2005; 15: 1277–1288. [DOI] [PubMed] [Google Scholar]
- 34.Muris P, Meesters C, Eijkelenboom A, et al. The self-report version of the Strengths and Difficulties Questionnaire: Its psychometric properties in 8- to 13-year-old non-clinical children. Br J Clin Psychol 2004; 43: 437–448. 10.1348/0144665042388982. [DOI] [PubMed] [Google Scholar]
- 35.Goodman A, Goodman R. Strengths and difficulties questionnaire as a dimensional measure of child mental health. J Am Acad Child Adolesc Psychiatry 2009; 48: 400–403. 10.1097/CHI.0b013e3181985068. [DOI] [PubMed] [Google Scholar]
- 36.Ferreira T, Geiser C, Cadima J, et al. The Strengths and Difficulties Questionnaire: An examination of factorial, convergent, and discriminant validity using multitrait-multirater data. Psychol Assess 2021; 33: 45–59. [DOI] [PubMed] [Google Scholar]
- 37.Varni JW, Seid M, Kurtin PS. PedsQLTM 4.0: Reliability and Validity of the Pediatric Quality of Life InventoryTM Version 4.0 Generic Core Scales in Healthy and Patient Populations. Med Care 2001; 39: 1239–1249. 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Garcia LF dos S, Manna TD, Passone C, et al. Translation and validation of Pediatric Quality of Life InventoryTM 3.0 Diabetes Module (PedsQLTM 3.0 Diabetes Module) in Brazil-Portuguese language. J Pediatr (Rio J) 2018; 94: 680–688. [DOI] [PubMed] [Google Scholar]
- 39.Buysse DJ, Reynolds CF, Monk TH, et al. The pittsburgh sleep quality index - a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28: 193–213. [DOI] [PubMed] [Google Scholar]
- 40.Peretti A, Amenta F, Tayebati SK, et al. Telerehabilitation: Review of the State-of-the-Art and Areas of Application. JMIR Rehabil Assist Technol 2017; 4: e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gherman A, Schnur J, Montgomery G, et al. How are adherent people more likely to think? A meta-analysis of health beliefs and diabetes self-care. Diabetes Educ 2011; 37: 392–408. [DOI] [PubMed] [Google Scholar]
- 42.Sims-Gould J, Race DL, Macdonald H, et al. ‘I just want to get better’: Experiences of children and youth with juvenile idiopathic arthritis in a home-based exercise intervention. Pediatr Rheumatol 2018; 16: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Favier LA, Taylor J, Rich KL, et al. Barriers to adherence in juvenile idiopathic arthritis: A multicenter collaborative experience and preliminary results. J Rheumatol 2018; 45: 690–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ng K, Cooper J, McHale F, et al. Barriers and facilitators to changes in adolescent physical activity during COVID-19. BMJ Open Sport Exerc Med 2020; 6: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ayres JRCM. CUIDADO: Trabalho e Interação nas Práticas de saúde. 1st ed.CEPESC – IMS/UERJ – ABRASCO, 2009. Rio de Janeiro. [Google Scholar]
- 46.Gilic B, Ostojic L, Corluka M, et al. Contextualizing Parental/Familial Influence on Physical Activity in Adolescents before and during COVID-19 Pandemic: A Prospective Analysis. Children 2020; 7: 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arman N, Tarakci E, Tarakci D, et al. Effects of video games-based task-oriented activity training (xbox 360 kinect) on activity performance and participation in patients with juvenile idiopathic arthritis: A randomized clinical trial. Am J Phys Med Rehabil 2019; 98: 174–181. [DOI] [PubMed] [Google Scholar]