Abstract
Postinfectious glomerulonephritis (PIGN) is an immune-mediated acute glomerulonephritis classically seen weeks after infection with Streptococcus pyogenes, although other infectious etiologies have emerged. While it has become increasingly rare in industrialized regions, it continues to affect children in developing countries. There has been debate as to why incidence rates are declining, including the possibility of improved initial treatment of bacterial infections. The ability of antimicrobial therapy in preventing PIGN as infectious sequelae, however, has not been comprehensively assessed. As varying evidence from published studies exists, the objective of this meta-analysis is to determine if antimicrobial therapy utilized to treat an initial infection has an effect in reducing the development of PIGN in humans. EMBASE, MEDLINE, and CENTRAL were searched using a comprehensive terminology strategy. From an initial search that returned 337 publications, 9 articles were included for analysis. Eight studies showed an incidence of PIGN after antimicrobial use ranging from 0.05% to 10% with a mean standardized difference (MSD) of 0.03 (0.01–0.06). Three studies showed an occurrence of PIGN without antibiotic use ranging from 1% to 13% with an MSD of 0.06 (−0.09–0.21). Our findings suggest that antimicrobial treatment for the initial infection may help diminish the development of PIGN. Although Streptococcus pyogenes infections are generally treated aggressively to prevent rheumatic fever, these findings may help further support the early treatment of bacterial infections to prevent postinfectious sequelae, especially as we consider other infectious etiologies of PIGN antimicrobial resistance.
Keywords: postinfectious glomerulonephritis, Streptococcus pyogenes, antimicrobial, antibiotic
1. Introduction
Postinfectious glomerulonephritis (PIGN) is an acute inflammatory disorder classified as a nephritic syndrome, resulting in hematuria, oliguria, hypertension, and edema when symptomatic [1]. This condition most frequently affects children and generally has a good prognosis [2]. It is classically seen one to two weeks following infection with Streptococcus pyogenes, although other infectious etiologies have been identified [3]. For this reason, it has historically been referred to as poststreptococcal glomerulonephritis (PSGN). While the exact mechanism is unknown, it is currently considered a type III hypersensitivity reaction that involves the accumulation of immune antigen–antibody complexes in the glomerulus, triggering an immune response and resulting in tissue damage in the kidney [4,5]. Newer theories also suggest an antibody and T-cell-mediated response to self-antigens due to molecular mimicry [6,7,8].
The majority of recent PIGN cases have affected children and occurred in low socioeconomic countries. In industrialized countries, the incidence of PIGN has become increasingly rare, with most cases occurring from nonstreptococcal bacterial infections in older individuals [9]. The mechanism behind the declining incidence rate is unknown, but it has been proposed that overall improvements in socioeconomic conditions, improved health care access, and altered susceptibility to GAS antigens plays a role. It has also been proposed that improved access to early initial treatment of bacterial infections may also contribute to this decline [10,11,12]. However, this suggestion contrasts the widely taught belief that initial treatment of bacterial infections with antimicrobials does not decrease the risk of developing PIGN [13,14]. The ability of antimicrobial therapies in preventing PIGN as infectious sequelae has not yet been comprehensively assessed, with contradictory evidence from published studies [15].
Establishing the effect of antimicrobials in preventing PIGN is important, especially as we consider new Streptococcal spp. strains with reduced susceptibility to broad-spectrum antimicrobials [16,17,18]. The objective of this meta-analysis is to determine the association between antimicrobial therapy use during an initial infection and the subsequent development of PIGN in humans.
2. Materials and Methods
2.1. Literature Search Strategy
Electronic searches of MEDLINE (all available years to May 2021), EMBASE (all available years to May 2021), and the Cochrane CENTRAL Register (all available years to May 2021) were performed. The terms used in this search were “psgn” OR “pign” OR “postinfectious glomerulonephritis” OR “post-infectious glomerulonephritis” OR “poststrep glomerulonephritis” OR “poststreptococcal glomerulonephritis” OR “post-strep glomerulonephritis” OR “post-streptococcal glomerulonephritis” AND “antibiotic” OR “antimicrobial”. Results were restricted to human studies, and no language restrictions were included. After the initial search, the study was registered in PROSPERO (Registration # CRD42021243989).
2.2. Data Collection
Quality of studies was assessed using tools outlined by the National Institutes of Health [19]. These guidelines allowed consideration of different study designs and assessment of risk of bias and are a preferred tool in systematic reviews [20]. After electronic de-duplication, studies were screened by four researchers (E.B., S.M., E.O., and K.A.), who agreed on included studies and achieved consensus on data collected. This allowed for identification of data which may have been omitted by a single reviewer. Screening also allowed for deduplication that did not initially occur electronically. Case studies, reviews, abstract-only, and articles without available full text after personal correspondence were excluded from data retrieval. Additional studies were excluded for the following reasons: the study did not discuss use of antimicrobials prior to the onset of PIGN, did not discuss initial infection, did not discuss PIGN, or data were not reliably extracted or reported.
The following variables were extracted from retrieved studies and recorded in Excel (Microsoft Corp., Redmond, WA, USA): title, author, source, date of study, eligibility or reason for exclusion, study design, sampling procedure, length of follow-up, bias control, statistical methods, setting, region, age and sex of participants, prior infection, intervention with route of delivery, dosage, and length of treatment, development of glomerulonephritis and other sequelae, and participants lost to follow-up.
2.3. Statistical Analysis
Contingency tables were created for each included study to evaluate the prevalence of PIGN following an initial bacterial infection. Microsoft Excel and RStudio were then used to calculate the outcome (effect size), standard error, standardized mean difference, and confidence intervals [21]. Heterogeneity was assessed through calculating the inverse variance index (I2). The strictly standardized mean difference (SSMD), i.e., the mean divided by the standard deviation of a difference between the two values from each one of the two independent groups, was used to measure the effect size for the comparison between the two groups.
3. Results
3.1. Antimicrobial Use and Postinfectious Glomerulonephritis
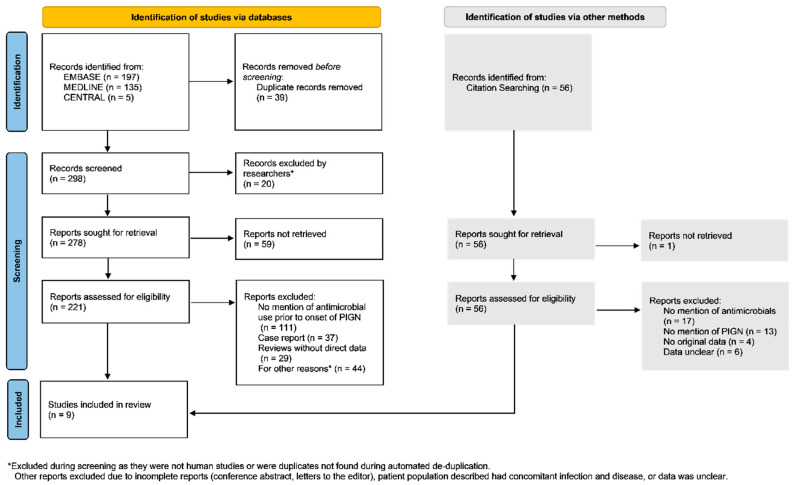
The search for studies concerning antimicrobials and PIGN in humans yielded 298 reports, which were narrowed down to 5 reports (Figure 1). An additional four reports from citation searching were assessed for inclusion eligibility, resulting in nine reports included in the review (Table 1) [22,23,24,25,26,27,28,29,30]. No studies were excluded due to quality concerns. Included studies discussed initial infection occurring at least 7 days prior to any postinfectious sequelae, mentioned the use of or withheld the use of antimicrobial therapy, and mentioned postinfectious glomerulonephritis. Three of nine studies reported incidence of PIGN without prior use of antimicrobial therapies for initial infection. These studies excluded participants who had repeat recent infections, a history of glomerulonephritis, or recent use of antimicrobial therapies. These studies also varied with regard to how initial infections were diagnosed or confirmed. The sample size of these studies ranged from 116 to 4482 patients. Five out of nine studies were conducted outside of the U.S. All nine studies evaluated use of penicillin; four studies utilized oral penicillin, four studies utilized intramuscular penicillin; and one study utilized parenteral penicillin. Two of nine studies were evaluating the efficacy of Penicillin V for group A Streptococcus (GAS) compared to another antimicrobial regimen. Each included study discussed the prevalence of PIGN following an initial infection.
Figure 1.
Using PRISMA guidelines for meta-analysis, a flowchart was created to illustrate the sources, inclusion, and exclusion of identified studies from databases and citation searching.
Table 1.
Included studies for this meta-analysis, with information regarding study date, patient ages considered, confirmatory testing of initial infection (if any), type of study (Cohort vs. Randomized Controlled Trial), and number of patients treated or not treated with antibiotics and those that developed PIGN.
| Study | Year | Study Location | Type of Study | Date of Study | Population Studied | Type of Sample | Prior Use of Antimicrobials | No Prior Use of Antimicrobials | Total No. of Patients | Antimicrobial Agent Utilized | Infectious Etiology Discussed | Major Findings | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment (n = ) | Cases (n = ) | No treatment (n = ) | Cases (n = ) | |||||||||||
| Adam et al. | 2000 | Germany | RCT | 1995–1998 | Ages 1–18 | Throat Culture | 4482 | 2 | 0 | 0 | 4482 | Oral Penicillin V vs oral macrolides, cephalosporin | GAS | Efficacy of 5-day antibiotic regimen was equivalent to 10 days of penicillin V |
| Chamovitz et al. | 1954 | Wyoming, USA | RCT | 1953 | Not stated (Air Force Base) | No samples taken | 257 | 0 | 109 | 1 | 366 | Intramuscular DBED Penicillin | Exudative tonsillitis or pharyngitis | Post-streptococcal sequelae, including glomerulonephritis and rheumatic fever, occurred in control patients whereas none occurred in penicillin treated patients |
| Hovelius et al. | 1983 | Sweden | Cohort | 1976–1977 | All Ages | Throat Culture | 220 | 9 | 0 | 0 | 220 | Penicillin V (47%), Erythromycin (9%), amoxicillin or doxycycline (4%) | GAS | PSGN was diagnosed in 9 out of 220 patients, supporting the assumption that early penicillin treatment reduces incidence of PSGN |
| Schaad et al. | 2002 | Switzerland | RCT | 1996–1999 | Ages 2–12 | Throat Culture | 269 | 8 | 0 | 0 | 269 | Oral Penicillin V vs Oral Azithromycin | GAS | Clinical efficacy of 3-day azithromycin and 10-day penicillin treatments were similar, although had lower levels of bacteriologic eradication |
| Scrace & Koko et al. | 2006 | Australia | Cohort | 2005 | Ages 2–12 | No samples taken | 56 | 3 | 60 | 8 | 116 | Intramuscular Penicillin | Screening for infected scabies | Screening of children with subsequent treatment using IM penicillin may be an effective community management strategy for APSGN outbreaks |
| Stetson et al. | 1955 | Maine, USA | RCT | 1952 | Not stated (Naval Base) | No samples taken | 44 | 1 | 140 | 10 | 184 | Intramuscular Penicillin | Pharyngitis | The incidence of acute nephritis was higher among untreated patients, compared to those receiving early penicillin therapy |
| Stillerman & Bernstein | 1963 | New York, USA | RCT | 1956–1960 | Not stated (pediatric offices) | Throat Culture | 442 | 1 | 0 | 0 | 442 | Oral Phenoxymethyl Penicillin | GAS | There was a significantly higher cure rate for nontypeable Streptococcus strains when treated with larger-dose penicillin compaired to smaller-dose treatment. |
| Streeton et al. | 1995 | Austrialia | Cohort | 1995 | Ages 2–14 | No samples taken | 583 | 58 | 0 | 0 | 583 | Intramuscular Penicillin | Screening for skin infection | Epidemic of APSGN was associated with GAS skin infections. Use of penicillin may have reduced community transmission. |
| Weinstein et al. | 1968 | Massachusetts, USA | Cohort | 1948 | All Ages | Throat and Nose Cultures | 167 | 6 | 0 | 0 | 167 | Parenteral Penicillin | GAS | The treatment of scarlet fever with penicillin therapy does not prevent "late" streptococcal sequelae, including rheumatic fever or glomerulonephritis. |
Derrick & Dillon excluded in MSD analysis and forest plot creation as PIGN cases occurred within 7 days of initiating antimicrobial treatment. Sholz is a repeat of Adam….
3.2. Glomerulonephritis in Patients with Initial Use of Antimicrobial Therapy
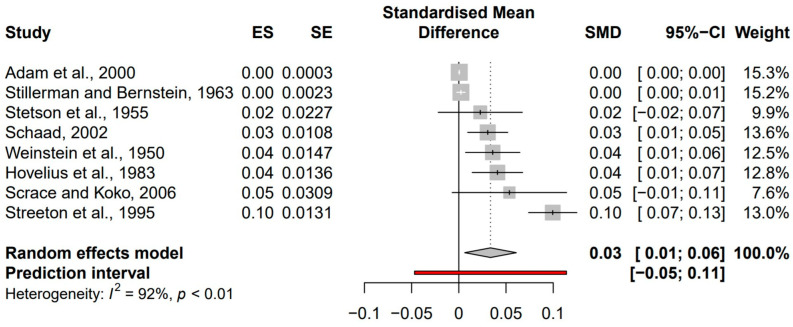
The search for studies concerning antimicrobial therapy use prior to development of PIGN yielded eight reports after applying exclusion and inclusion criteria. Studies without cases of PIGN were not considered given the overall rare incidence of PIGN. Significant heterogeneity (I2 = 92%, p < 0.01) was found in the confidence intervals (CI) of patients initially treated with antimicrobial therapies. This heterogeneity was addressed with random effects analysis. Random effects analysis was utilized based on the assumption that the studies included in this analysis represent a random sample of effect sizes, and the true effect size varies from one study to the next [31].
The overall standardized mean difference (SMD) in the CI of antimicrobial therapy prior to development of PIGN was 0.03 (95% CI, 0.01 to 0.06). Analysis of these eight studies demonstrated varying effect sizes for PIGN occurring following antimicrobial therapy for an initial infection (Figure 2).
Figure 2.
Lists the author and study year, effect size (ES), standard error (SE), standardized mean difference (SMD), and 95% confidence interval (CI) for each study. The forest plot reveals SMD for each study plotted against a random effects model.
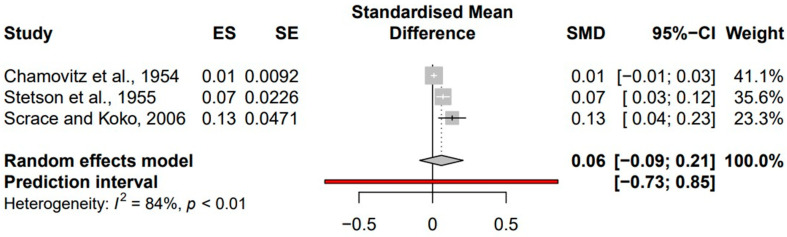
3.3. Glomerulonephritis in Patients without Initial Use of Antimicrobial Therapy
The search for studies concerning antimicrobial therapy use prior to development of PIGN yielded three reports where patients were not provided antimicrobial therapies, after applying exclusion and inclusion criteria. Studies without cases of PIGN were not considered given the overall rare incidence of PIGN. Significant heterogeneity (I2 = 84%, p < 0.01) was found in the confidence intervals (CI) of patients not initially treated with antimicrobials. This heterogeneity was addressed with random effects analysis.
The overall SMD of the CI for patients who had not undergone antimicrobial therapy prior to development of PIGN was 0.06 (95% CI, −0.09 to 0.21). Analysis of these three studies demonstrated varying effect sizes for PIGN development following initial infection without antimicrobial treatments (Figure 3).
Figure 3.
Lists the author and study year, effect size (ES), standard error (SE), standardized mean difference (SMD), and 95% confidence interval (CI) for each study. The forest plot reveals SMD for each study plotted against a random effects model.
The SMD for studies where patients were treated with antimicrobials was 0.03 at 95% CI (0.01–0.06) whereas the SMD for studies where patients were not treated with antimicrobials was 0.06 at 95% CI (−0.09 to 0.21).
To measure the effect sizes for the comparison of the two groups, we calculated the SSMD as 0.55.
4. Discussion
Overall, our findings reveal a potentially protective effect of antimicrobial therapies on the subsequent development of PIGN. Both types of studies, with and without previous use of antimicrobial therapy prior to development of PIGN, revealed a small SMD. This is likely due to the low incidence of PIGN overall, at around 470,000 cases globally per year [32]. Although PIGN is a rare postinfectious sequela, these results may still provide clinical relevance.
It is worth noting that this study did not evaluate the potential differences between age, sex, or region when calculating the incidence of PIGN as sequelae. The studies included for analysis included participants who developed PIGN at least 7 days following initiation of antimicrobial therapies. Additionally, as seen in Figure 2, Streeton et al. demonstrated a potential outlier with an effect size of 0.10. These authors note that screening can recognize clinically asymptomatic cases, which was also mentioned by Scrace and Koko. This, in combination with mass treatment and availability of penicillin treatments may have prevented the spread of nephritogenic strains of GAS, as they were studying outbreaks in three remote communities.
Potential additive biases also include different time points in treating the initial infection or different antimicrobials and pharmacotherapeutics utilized for treatment. These differences may help explain the considerable heterogeneity observed across the studies. Additionally, differences in addressing patient nonadherence to antimicrobial treatment varied across the studies with subsequent severity of PIGN not addressed.
A previous systematic review published in 2010 evaluated antimicrobials in preventing PSGN [33]. Zaffanello et al. reported that the role of antimicrobials in PIGN prevention is unproven. However, of the nine studies that were included in the review, four appear to be subsets of the same data reported by Adam et al. The study of 4482 patients had the largest dataset, and other publications included in this review of antimicrobials for prevention of PIGN appeared to be subset analyses [22,34,35]. Adam et al. and Scholz concluded that the efficacy of a 5-day antibiotic regimen was equivalent to a 10-day Penicillin V treatment regimen and treatment differences did not result in differences in streptococcal sequelae.
The exact mechanism of how streptococcal infections and subsequent immune responses damage the glomeruli is unknown. However, establishing whether antimicrobials used to treat the initial infection can effectively prevent sequelae is important [1,36,37]. Although GAS infections are generally treated aggressively to prevent the potential future development of rheumatic fever, elucidating the potential of developing other complications, such as PIGN, becomes a more pressing matter as we consider the growing rates of antimicrobial-resistant micro-organisms [38]. Studies on antibiotic efficacy and resistance should inform evidence-based treatment protocols to reduce the risk of refractory infections [39,40].
Although our analysis revealed the presence of considerable heterogeneity, data from this study have revealed potential protective effects of antimicrobial therapy in preventing PIGN. These findings may help further support early treatment of bacterial infections to prevent this type of complication. However, given the analysis of only nine studies, larger cohort studies, likely through global retrospective chart reviews, would be needed to confirm this effect.
Acknowledgments
Special thanks to the PLFSOM-TTUHSCEP Library staff for their assistance.
Author Contributions
Planning (E.B. and J.C.), conception and design (E.B. and J.C.), acquisition of data (E.B., S.M., E.O. and K.A.), data analysis (E.B., B.-Y.H. and J.C.), interpretation of data (E.B. and J.C.), wrote the manuscript (E.B., S.M., E.O., K.A., B.-Y.H. and J.C.). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rawla P., Padala S.A., Ludhwani D. Poststreptococcal Glomerulonephritis. StatPearls Publishing; Treasure Island, FL, USA: 2021. StatPearls. [PubMed] [Google Scholar]
- 2.Kılıc B.D., Kara M.A., Buyukcelik M., Balat A. Pediatric post-streptococcal glomerulonephritis: Clinical and laboratory data. Pediatrics Int. Off. J. Jpn. Pediatric Soc. 2018;60:645–650. doi: 10.1111/ped.13587. [DOI] [PubMed] [Google Scholar]
- 3.Satoskar A.A., Parikh S.V., Nadasdy T. Epidemiology, pathogenesis, treatment and outcomes of infection-associated glomerulonephritis. Nat. Rev. Nephrol. 2020;16:32–50. doi: 10.1038/s41581-019-0178-8. [DOI] [PubMed] [Google Scholar]
- 4.Usman N., Annamaraju P. Type III Hypersensitivity Reaction. StatPearls Publishing; Treasure Island, FL, USA: 2021. StatPearls. [PubMed] [Google Scholar]
- 5.Eison T.M., Ault B.H., Jones D.P., Chesney R.W., Wyatt R.J. Post-streptococcal acute glomerulonephritis in children: Clinical features and pathogenesis. Pediatric Nephrol. 2011;26:165–180. doi: 10.1007/s00467-010-1554-6. [DOI] [PubMed] [Google Scholar]
- 6.Couser W.G. Pathogenesis and treatment of glomerulonephritis-an update. J. Bras. De Nefrol. 2016;38:107–122. doi: 10.5935/0101-2800.20160016. [DOI] [PubMed] [Google Scholar]
- 7.Rodríguez-Iturbe B., Batsford S. Pathogenesis of poststreptococcal glomerulonephritis a century after Clemens von Pirquet. Kidney Int. 2007;71:1094–1104. doi: 10.1038/sj.ki.5002169. [DOI] [PubMed] [Google Scholar]
- 8.Luo Y.-H., Chuang W.-J., Wu J.-J., Lin M.T., Liu C.-C., Lin P.-Y., Roan J.-N., Wong T.-W., Chen Y.-L., Lin Y.-S. Molecular mimicry between streptococcal pyrogenic exotoxin B and endothelial cells. Lab Investig. 2010;90:1492–1506. doi: 10.1038/labinvest.2010.93. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez-Iturbe B., Musser J.M. The Current State of Poststreptococcal Glomerulonephritis. J. Am. Soc. Nephrol. 2008;19:1855–1864. doi: 10.1681/ASN.2008010092. [DOI] [PubMed] [Google Scholar]
- 10.Kanjanabuch T., Kittikowit W., Eiam-Ong S. An update on acute postinfectious glomerulonephritis worldwide. Nat. Rev. Nephrol. 2009;5:259–269. doi: 10.1038/nrneph.2009.44. [DOI] [PubMed] [Google Scholar]
- 11.Ilyas M., Tolaymat A. Changing epidemiology of acute post-streptococcal glomerulonephritis in Northeast Florida: A comparative study. Pediatr Nephrol. 2008;23:1101–1106. doi: 10.1007/s00467-008-0778-1. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz B., Facklam R.R., Breiman R.F. Changing epidemiology of group A streptococcal infection in the USA. Lancet. 1990;336:1167–1171. doi: 10.1016/0140-6736(90)92777-F. [DOI] [PubMed] [Google Scholar]
- 13.Glassock R.J., Alvarado A., Prosek J., Hebert C., Parikh S., Satoskar A., Nadasdy T., Forman J., Rovin B., Hebert L.A. Staphylococcus-related glomerulonephritis and poststreptococcal glomerulonephritis: Why defining “post” is important in understanding and treating infection-related glomerulonephritis. Am. J. Kidney Dis. 2015;65:826–832. doi: 10.1053/j.ajkd.2015.01.023. [DOI] [PubMed] [Google Scholar]
- 14.Shulman S.T., Bisno A.L. 200-Nonsuppurative Poststreptococcal Sequelae: Rheumatic Fever and Glomerulonephritis. In: Bennett J.E., Dolin R., Blaser M.J., editors. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 8th ed. W.B. Saunders; Philadelphia, PA, USA: 2015. pp. 2300–2309. [Google Scholar]
- 15.Sainato R.J., Weisse M.E. Poststreptococcal Glomerulonephritis and Antibiotics: A Fresh Look at Old Data. Clin. Pediatrics. 2019;58:10–12. doi: 10.1177/0009922818793345. [DOI] [PubMed] [Google Scholar]
- 16.Musser J.M., Beres S.B., Zhu L., Olsen R.J., Vuopio J., Hyyryläinen H.-L., Gröndahl-Yli-Hannuksela K., Kristinsson K.G., Darenberg J., Henriques-Normark B., et al. Reduced In Vitro Susceptibility of Streptococcus pyogenes to β-Lactam Antibiotics Associated with Mutations in the pbp2x Gene Is Geographically Widespread. J. Clin. Microbiol. 2020;58:e01993-19. doi: 10.1128/JCM.01993-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaplan S.L., Mason E.O. Management of Infections Due to Antibiotic-Resistant Streptococcus pneumoniae. Clin. Microbiol. Rev. 1998;11:628–644. doi: 10.1128/CMR.11.4.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cattoir V. Mechanisms of Antibiotic Resistance. In: Ferretti J.J., Stevens D.L., Fischetti V.A., editors. Streptococcus Pyogenes: Basic Biology to Clinical Manifestations. University of Oklahoma Health Sciences Center; Oklahoma City, OK, USA: 2016. [PubMed] [Google Scholar]
- 19.National Institute of Health . Study Quality Assessment Tools|NHLBI. NIH; Bethesda, MD, USA: 2014. [(accessed on 31 January 2022)]. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. [Google Scholar]
- 20.Farrah K., Young K., Tunis M.C., Zhao L. Risk of bias tools in systematic reviews of health interventions: An analysis of PROSPERO-registered protocols. Syst. Rev. 2019;8:280. doi: 10.1186/s13643-019-1172-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neyeloff J.L., Fuchs S.C., Moreira L.B. Meta-analyses and Forest plots using a microsoft excel spreadsheet: Step-by-step guide focusing on descriptive data analysis. BMC Res. Notes. 2012;5:52. doi: 10.1186/1756-0500-5-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adam D., Scholz H., Helmerking M. Short-course antibiotic treatment of 4782 culture-proven cases of group A streptococcal tonsillopharyngitis and incidence of poststreptococcal sequelae. J. Infect. Dis. 2000;182:509–516. doi: 10.1086/315709. [DOI] [PubMed] [Google Scholar]
- 23.Hovelius B., Bygren P., Christensen P., A Mårdh P. Respiratory tract infections at a community care centre—with emphasis on group A streptococci. Scand. J. Infect. Dis. Suppl. 1983;39:59–67. [PubMed] [Google Scholar]
- 24.Scrace M., Koko K. An outbreak of acute post-streptococcal glomerulonephritis in remote Far North Queensland. Aust. J. Rural. Health. 2006;14:160–163. doi: 10.1111/j.1440-1584.2006.00795.x. [DOI] [PubMed] [Google Scholar]
- 25.Streeton C.L., Hanna J.N., Messer R.D., Merianos A. An epidemic of acute post-streptococcal glomerulonephritis among Aboriginal children. J. Paediatr. Child Health. 1995;31:245–248. doi: 10.1111/j.1440-1754.1995.tb00795.x. [DOI] [PubMed] [Google Scholar]
- 26.Chamovitz R., Catanzaro F.J., Stetson C.A., Rammelkamp C.H. Prevention of rheumatic fever by treatment of previous streptococcal infections. I. Evaluation of benzathine penicillin G. N. Engl. J. Med. 1954;251:466–471. doi: 10.1056/NEJM195409162511203. [DOI] [PubMed] [Google Scholar]
- 27.Stetson C.A., Rammelkamp C.H., Krause R.M., Kohen R.J., Perry W.D. Epidemic acute nephritis: Studies on etiology, natural history and prevention. Medicine. 1955;34:431–450. doi: 10.1097/00005792-195512000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Weinstein L., Bachrach L., Boyer N.H. Observations on the Development of Rheumatic Fever and Glomerulonephritis in Cases of Scarlet Fever Treated with Penicillin. N. Engl. J. Med. 1950;242:1002–1010. doi: 10.1056/NEJM195006292422602. [DOI] [PubMed] [Google Scholar]
- 29.Stillerman M., Bernstein S.H. Streptococcal Pharyngitis Therapy. Am. J. Dis. Child. 1964;107:35–46. doi: 10.1001/archpedi.1964.02080060037006. [DOI] [PubMed] [Google Scholar]
- 30.Schaad U.B., Kellerhals P., Altwegg M. Azithromycin versus penicillin V for treatment of acute group A streptococcal pharyngitis. Pediatric Infect. Dis. J. 2002;21:304–308. doi: 10.1097/00006454-200204000-00009. [DOI] [PubMed] [Google Scholar]
- 31.Borenstein M., Hedges L.V., Higgins J., Rothstein H.R. Introduction to Meta-Analysis. John Wiley & Sons; Hoboken, NJ, USA: 2009. [Google Scholar]
- 32.Carapetis J.R., Steer A.C., Mulholland E.K., Weber M. The global burden of group A streptococcal diseases. Lancet Infect. Dis. 2005;5:685–694. doi: 10.1016/S1473-3099(05)70267-X. [DOI] [PubMed] [Google Scholar]
- 33.Zaffanello M., Cataldi L., Franchini M., Fanos V. Evidence-based treatment limitations prevent any therapeutic recommendation for acute poststreptococcal glomerulonephritis in children. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2010;16:RA79–RA84. [PubMed] [Google Scholar]
- 34.Adam D., Scholz H., Helmerking M. Comparison of short-course (5 day) cefuroxime axetil with a standard 10 day oral penicillin V regimen in the treatment of tonsillopharyngitis. J. Antimicrob. Chemother. 2000;45:23–30. doi: 10.1093/jac/45.suppl_1.23. [DOI] [PubMed] [Google Scholar]
- 35.Scholz H. Streptococcal-A tonsillopharyngitis: A 5-day course of cefuroxime axetil versus a 10-day course of penicillin V. results depending on the children’s age. Chemotherapy. 2004;50:51–54. doi: 10.1159/000077286. [DOI] [PubMed] [Google Scholar]
- 36.Balasubramanian R., Marks S.D. Post-infectious glomerulonephritis. Paediatr. Int. Child Health. 2017;37:240–247. doi: 10.1080/20469047.2017.1369642. [DOI] [PubMed] [Google Scholar]
- 37.Van De Voorde R.G. Acute poststreptococcal glomerulonephritis: The most common acute glomerulonephritis. Pediatrics Rev. 2015;36:3–12. doi: 10.1542/pir.36.1.3. [DOI] [PubMed] [Google Scholar]
- 38.Kim S., Lee S., Park H., Kim S. Predominance of emm4 and antibiotic resistance of Streptococcus pyogenes in acute pharyngitis in a southern region of Korea. J. Med. Microbiol. 2019;68:1053–1058. doi: 10.1099/jmm.0.001005. [DOI] [PubMed] [Google Scholar]
- 39.Tyrstrup M., Melander E., Hedin K., Beckman A., Mölstad S. Children with respiratory tract infections in Swedish primary care; prevalence of antibiotic resistance in common respiratory tract pathogens and relation to antibiotic consumption. BMC Infect. Dis. 2017;17:603. doi: 10.1186/s12879-017-2703-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Septimus E.J. Antimicrobial Resistance: An Antimicrobial/Diagnostic Stewardship and Infection Prevention Approach. Med. Clin. N. Am. 2018;102:819–829. doi: 10.1016/j.mcna.2018.04.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.