Abstract
Background
Several reports document a decrease in the rates of stroke hospital admissions during the covid-19 pandemic. There is very little information whether the admission rates will change as the infection is controlled. We report on our rates of admissions before, during and following the peak of covid-19 infections in a prospective database from Qatar.
Methods and results
The stroke admissions in the six months prior to COVID-19 pandemic averaged 229/month. There was a decrease to 157/month in March-June during the peak of the pandemic. In the 6 months following the peak, as covid-19 numbers began to decrease, the average numbers increased back to 192/month. There was an increase in severe ischemic strokes and decreased in functional recovery. The decreased admissions were mainly driven by fewer stroke mimics. Patients presenting with ischemic stroke or cerebral hemorrhage remained unchanged.
Conclusions
Fewer stroke mimics presenting to the hospital can explain the fewer admissions and poor outcome at the height of the covid-19 pandemic. The continued decrease in the number of ischemic stroke and stroke mimic admissions following the pandemic peak requires more study.
Introduction
There are a number of reports from around the world have documented a decrease in the number of stroke related admission during the peak months of the first wave of the COVID-19 pandemic [1–15]. The decrease has been most apparent with transient ischemic attacks, minor stroke and stroke mimics [4, 8, 11, 13, 14]. We have recently shown a significant decrease in stroke admissions to the Hamad General Hospital (HGH) in Qatar during the COVID-19 pandemic that was predominantly driven by a decrease in transient ischemic attacks (TIAs), minor stroke and stroke mimics [14]. The decrease has however not been universally reported, with some centers reporting no decrease in admission rates [16]. A reluctance to seek medical attention for fear of contracting the virus may be contributing to the decreased frequency in such categories. Strict instructions to stay at home during lockdowns may contribute to this trend. Social isolation, especially in the elderly may allow for a lack of detection by family members who are not able to make the diagnosis. Secondly, the emergency services may be overwhelmed by responses to the pandemic, thus neglecting the stroke patients [17]. The risk of recurrent stroke is highest following a TIA and there is considerable evidence that this is reduced significantly with appropriate assessment and treatment [18]. There is therefore an increased risk of recurrence or progression of symptoms if there is delay in the diagnosis and initiation of preventative treatment. Similar trends appear to parallel in rates of admissions of other serious conditions including cardiac and surgical emergencies [19–22].
Although, there are multiple reports documenting the decrease in stroke admission rates during the pandemic, there is little research on stroke rates once the number of COVID-19 cases begins to decrease. A study of disease trends during the months following controlling the pandemic, as the cases of COVID-19 begin to decrease in the community, may offer important information on the reasons for the decline in stroke admissions during the pandemic. We present the state-wide admission rates for stroke from the Qatar Stroke Database for the entire year and compare stroke admissions to COVID-19 cases during the same time.
Methods
The Qatar Stroke Database prospectively collects information on all acute stroke patients admitted to the Hamad General Hospital (HGH) in Qatar. The hospital is a tertiary stroke center that has a dedicated stroke ward. The hospital is the only center where stroke-specific treatments, including intravenous thrombolysis and mechanical thrombectomy are offered and where 98% of stroke patients requiring admission in Qatar are managed. The details of the database have previously been published [22, 23].
Ethical approval and Patient Consent
No patient consent was required due to the study design.
The study was approved by the Institutional Review Board, Hamad Medical Corporation at the Medical Research Centre (MRC-16016/16).
All stroke patients admitted to HGH stroke service from September 2019 to December-2020 were evaluated for this study. In addition to overall rates of admissions, we evaluated the frequency of strokes subtypes, TIAs and stroke mimics during the study period. We reviewed presumed stroke admissions in three time periods; Sept 2019 to Feb 2020 (pre-pandemic), March to June 2020 (Pandemic) and July to December 2020 (post-peak of pandemic) 2020.
Clinical information including rates of admissions, clinical presentation, NIHSS at admission and discharge, TOAST classification, ethnicity, risk factors, investigations, complications, length of stay and discharge outcomes were obtained. The modified Rankin Scale (mRS) pre-admission, at discharge, and at 90-day follow-up was also collected when available.
Descriptive and inferential statistics were used to characterize the study sample. Descriptive results (including graphical displays) for all quantitative variables (e.g., age) are presented as the mean ± standard deviation (SD) for normally distributed data or median with interquartile range for data not normally distributed. The monthly rate of stroke admissions was compared in the six months pre-Covid-19 (Jan-Feb 2020), four months when the pandemic cases were very high (March-June 2020) and for the following 6 months (July-Dec 2022). Bivariate analysis comparing the demographic and clinical characteristics of the patients along with some discharge outcomes during the study periods were performed using Independent sample t-test, and the Mann Whitney U-test to compare the average for all quantitative variables (e.g., age) between stroke subtypes, wherever appropriate, while the Pearson Chi-Square test or Fisher Exact test were used, as appropriate, in comparing all the qualitative variables. The statistical tests were performed using IBM SPSS Statistics ver. 27 (IBM, Armonk, USA). A p-value of 0.05 or less was considered significant.
Results
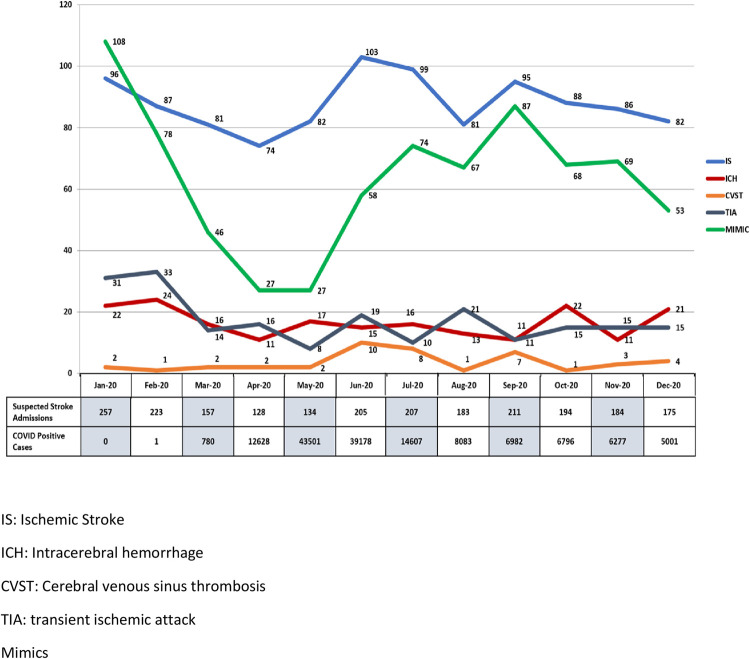
There were 3162 stroke admissions to the HGH between September 2019 and December 2020 [age: 53.3 ±14.5; male: 2306 (72.9%) (Table 1). The younger age and higher percentage of males reflects the demographics of Qatar with a predominantly young male expatriate population. The monthly rates of COVID-19 diagnosis for the state of Qatar during the pandemic are shown in Fig 1 with the peak rates during March-June months. The monthly rates of stroke admissions during the year are shown in Table 1. There was a highly significant decrease in stroke admissions during the peak months of the pandemic (Table 1 and Fig 1). The significant decrease in the number of patients with atrial fibrillation is likely due to fewer patients being offered Holter monitors during the pandemic. The young age of the patients may also account for fewer diagnosis of atrial fibrillation as we have previously reported [23]. We have no clear explanation for the significantly fewer patients with diabetes or patients who were ‘current smokers’. Perhaps the pandemic may have been a factor in fewer smokers in the pandemic and post-peak time period. The low mortality is likely related to the young age of the patient population and the very high incidence of lacunar stroke with mild symptoms as has been previously reported [21, 22]. The majority of strokes were seen in non-Qatari nationals (less than 20% patients were Qataris.
Table 1. The details of the admissions, risk factors, TOAST classification, prognosis and interventions is shown for the pre-COVID-19, during the peak of the pandemic and in the six months following the peak of the pandemic.
| Characteristic or Investigation | Total Patients | Pre-COVID Time (Sep 2019-Feb 2020) | Peak COVID Time (Mar-Jun 2020) | Post-Peak COVID Time (July-Dec 2020) | P- Value |
|---|---|---|---|---|---|
| (n = 3162) | (n = 1376, average = 229.3/month) | (n = 630, average = 157.5/month) | (n = 1156, average = 192.7/month | ||
| Age- Mean, years | 53.3 ±14.5 | 52.5 ±14.0 | 54.09 ±14.6 | 53.9 ±14.9 | 0.02 |
| Sex—Males | 2306 (72.9) | 1010 (73.4) | 468 (74.3) | 828 (71.6) | 0.42 |
| Diabetes | 1536 (48.6) | 626 (45.5) | 321 (51.0) | 586 (51.0) | 0.01 |
| Hypertension | 2040 (64.5) | 904 (65.7) | 409 (64.9) | 727 (62.9) | 0.33 |
| Prior Stroke | 368 (11.6) | 153 (11.1) | 68 (10.8) | 147 (2.7) | 0.35 |
| Coronary Artery Disease | 336 (10.6) | 142 (10.3) | 77 (12.2) | 117 (10.1) | 0.34 |
| Prior Atrial Fibrillation | 292 (9.2) | 99 (7.2) | 46 (7.3) | 147 (12.7) | <0.001 |
| Current Smoker | 677 (21.4) | 331 (24.1) | 118 (18.7) | 228 (19.7) | 0.006 |
| Final Diagnosis | |||||
| Ischemic Stroke | 1433 (45.3) | 572 (41.6) | 330 (52.4) | 531 (45.9) | <0.001 |
| Transient Ischemic Attack | 299 (9.5) | 157 (11.4) | 56 (8.9) | 86 (7.4) | |
| Intracerebral Hemorrhage | 276 (8.7) | 111 (8.1) | 69 (11.0) | 96 (8.3) | |
| Cerebral Venous Sinus Thrombosis | 52 (1.6) | 13 (0.9) | 15 (2.4) | 24 (2.1) | |
| Stroke Mimic | 1102 (34.9) | 523 (38.0) | 160 (25.4) | 419 (36.2) | |
| TOAST Classification | |||||
| Small Vessel Disease | 582 (40.1) | 258 (44.1) | 115 (34.3) | 209 (39.4) | 0.005 |
| Large Vessel Disease | 279 (19.2) | 84 (14.4) | 82 (24.5) | 113 (21.3) | |
| Cardio-Embolic | 388 (26.7) | 151 (25.8) | 97 (29.0) | 140 (26.4) | |
| Stroke of Determined Origin | 72 (5.0) | 32 (5.5) | 13 (3.9) | 27 (5.1) | |
| Stroke of Undetermined Origin | 130 (9.0) | 60 (10.3) | 28 (8.4) | 42 (7.9) | |
| Prognosis–At Discharge | |||||
| Good (mRS 0–2) | 2134 (67.5) | 997 (72.5) | 368 (58.4) | 769 (66.5) | <0.001 |
| Poor (mRS 3–6) | 1028 (32.5) | 379 (27.5) | 262 (41.6) | 387 (33.5) | |
| Mortality–At Discharge | 38 (1.2) | 15 (1.1) | 11 (1.7) | 12 (1.0) | 0.37 |
| NIHSS | |||||
| NIHSS on admission (mean) | 4.1 ±6.3 | 3.6 ±5.8 | 5.3 ±7.2 | 4.1 ±6.3 | <0.001 |
| Mild Stroke (NIHSS 4 or less) | 2344 (74.1) | 1071 (77.8) | 422 (67.0) | 851 (73.6) | <0.001 |
| Moderate Stroke (NIHSS 5–10) | 415 (13.1) | 155 (11.3) | 98 (15.6) | 162 (14.0) | |
| Severe Stroke (NIHSS > 10) | 403 (12.7) | 150 (10.9) | 110 (17.5) | 143 (12.4) | |
| Intervention | |||||
| IV Thrombolysis | 138 (4.4) | 60 (4.4) | 34 (5.4) | 44 (3.8) | 0.29 |
| Door to Needle Time (minutes) | 68.4 ±31.0 | 67.7 ±34.2 | 68.8 ±32.7 | 68.9 ±32.7 | 0.97 |
| Interventional Thrombectomy | 40 (1.3) | 20 (1.5) | 10 (1.6) | 10 (0.9) | 0.30 |
Fig 1. Distribution of different discharge diagnosis per month during the pre-COVID-19, peak of the pandemic and in the six months following the peak of the COVID-19 pandemic.
The number of monthly COVID-19 cases are shown in the legend below. The “P” values are for group comparisons between the pre-pandemic, pandemic and post-pandemic time period.
The decrease in the rates of medical and functional mimics evident during the peak months of the pandemic gradually returned towards pre-pandemic levels as the rates of COVID-19 cases decreased but never quite reached the baseline.
Using the TOAST criteria [24] for classifying the etiology, we noticed a significant decrease in the percentage of SVD in patients with confirmed ischemic stroke, decreasing from 44.1% in the pre-pandemic to 34.3% during the pandemic and 39.4% in the last six months of observation. We also noted a concomitant significant increase in the percentage of stroke due to large vessel disease, increasing from 14.4% in the pre-COVID 6 months to 24.8% in the 3 months in March-June and 21.3% in the post-peak months (see Table 1 and S1 Table). The details of the baseline, study period, diagnosis, TOAST classification, prognosis and interventions in two major ethnic groups of the study population, for the pre-COVID-19, during the peak and in the six months following the peak of the pandemic are provided in S1 Table. There were very few patients from Europe/USA, Africa and the Far East and therefore were not included in the analysis. We have previously reported on the significant differences in age, type of strokes and prognosis between Arab and South Asian patients [24, 25].
The severity of symptoms at presentation increased during the pandemic months when compared to the pre and post-peak pandemic time period. There was an increase in the average NIHSS on admission from 3.6 ±5.8 in the pre-COVID 6 months to 5.3 ±7.2 in March-June and decreasing to 4.1 ±6.3in the following 6 months. The percentage of patients with mild symptoms (NIHSS ≤ 4) decreased from 1071 (77.8%) in the pre-COVID months to 422 (67.0%) in Feb-June and increased to 851 (73.6%) in the last six months of 2020 (p = 0.001).
There was also a significant increase in the rates of patients with poor functional recovery during the four months (March-June 2020) when compared to the pre and post pandemic time. The number of patients with mRS of 0–2 at discharge decreased from 997 (72.5%) in the pre-COVID months to 368 (58.4%) in the four months post-COVID and improved again in the following 6 months to 769 (66.5%) with p = 0<0.001).
Discussion
Our study supports previous reports documenting the dramatic decline in acute stroke admissions during the COVID-19 pandemic. We also provide evidence that while there was a return towards increasing admissions as the pandemic conditions improved, it did not return to the pre-pandemic levels. Our previous report outlined the dramatic decrease in the stroke rates during the three months of the pandemic, driven predominantly by reduction in stroke mimics. The admissions for ischemic stroke and ICH had remained unchanged during the height of the pandemic [14]. This led to a relative increase in the admission of patients with severe symptoms leading to poorer functional recovery [14]. Following the height of the pandemic, as the number of COVID-19 cases began to fall, the number of suspected stroke admissions to the hospital began to increase. Once again, this was predominantly driven by the increasing number of stroke mimic admissions. Interestingly, although the number of COVID-19 cases decreased significantly in July-December 2020, the numbers remained higher than 197/month. Similarly, although stroke admissions increased, these did not reach the pre-pandemic levels.
The effects of lockdown in the recent COVID-19 pandemic have been reported on several acute emergencies [12, 19–21, 26]. In most regions the decrease in stroke and acute coronary syndromes (ACS) have been similar although in Greece, there was a decrease in acute stroke but not ACS [27]. In Finland, there was a reduction in the rates of several acute medical illnesses seen in the emergency department, including infections (28%), back or limb pain (31%) and psychiatric illness (19%). Interestingly, there was no decrease in the number of stroke or ACS admissions during the period of observation [21]. In Qatar, decline in admissions to the emergency department varied between 9% to 75% was observed for acute surgical emergencies, ACS, bone fractures and cancer whereas admissions for respiratory conditions increased [20].
Several studies noted that the severity of symptoms of stroke patients increased during the pandemic [28]. There are reports of formation of recurrent thrombi during treatment of acute stroke [28]. An enhanced thrombotic state has been reported with COVID-19 infection and this may explain the higher incidence of severe strokes [29–31]. In addition, the COVID-19 virus may directly damage the cerebral vascular endothelium, making it more thrombogenic [30, 32]. The increased severity of stroke symptoms may also be artificially increased because of the frequent observation that the majority of patients with TIAs and mild stroke are not coming to hospital as is evident from our data and the reported decline in milder cases in published reports [4,8, 11, 13, 14].
To our knowledge, there is only one other study that reported on the stroke rates following the pandemic [33]. Similar to our observations, in the report from Norway, stroke admissions following the height of the pandemic did return to the pre-pandemic levels once the COVID-19 pandemic was under better control. In Norway, the decrease was evidence for TIAs and mild stroke but not for ICH during the lockdown period [33]. Similar to our report, the severity of symptoms was higher during the lockdown and there were delays in admission to hospital [33]. The reasons for the decreased admissions following the peak COVID-19 may be persistent avoidance behavior and concerns over contracting COVID-19 even when the numbers are down or a true decrease in the stroke rates in the community. Factors that may contribute to the lower rates include social distancing, reduced other infections, decreased air pollution or other unmeasured measures that require further study.
The dramatic decline in rates of strokes and other illnesses to hospital requires further study and has been a subject of much speculation. The most prevalent hypotheses relate to a fear for coming to hospital for fear of infection. This in turn may be magnified from ‘stay-at-home’ orders, leading to deferring urgent care as a recent survey from UK [34]. In Germany, the initial early decline in stroke-related consultations in the pandemic and later increase for telemedicine paralleled the population activities during lockdowns [35]. Another study from France also reported that there appeared to be a relationship between the decrease in stroke admissions to the severity of the COVID-19 illness [36].
Several additional factors proposed to explain the decrease in emergency visits of acute illnesses and the lower rates even when the restrictions were lifted as the cases decreased. A decrease in physical activity during lockdown may also have potential protective effects. An increase in physical activity is known to increase blood pressure potentially increasing the risk of SAH [37] and ACS [38]. Several virus and bacterial infections are known to trigger plaque rupture acute heart failure, ACS and acute stroke [39]. An intriguing hypothesis suggests that the diminished cardiovascular disease during the COVID-19 pandemic may be secondary to the extreme reduction in non-COVID-19 related community-acquired infections [40]. There has been an almost 50% reduction in the diagnosis of new-onset atrial fibrillation in Denmark following the lockdown and as atrial fibrillation is an important stroke mechanism in the elderly, may also potentially contribute to the low rates of strokes [41].
In summary, the evidence from the Qatar Database shows that there is a gradual return of the rates of stroke admissions to the hospital as the COVID-19 cases began to decrease in the community. This was predominantly driven by an increase in stroke mimics. Interestingly, although the COVID-19 infections fell significantly in the months following June, 2020, the rates of stroke admissions did not return to the pre-pandemic levels. The reasons for the for the decreasing stroke numbers is unclear and the possible mechanism are discussed above.
Supporting information
(DOCX)
Acknowledgments
We acknowledge the assistance of all involved physicians, nurses, and staff of the Stroke Team in HMC. We also thank Ms. Reny Francis (HMC) and Kath McKenzie (University of Alberta) for her editorial assistance and supportive care.
Data Availability
All relevant data are in the paper and supporting information files.
Funding Statement
Dr.Naveed Akhtar received funding for the grant 16016/16 from Hamad Medical Corporation. No role of the sponsor in the study.
References
- 1.Padmanabhan N, Natarajan I, Gunston R et al. (2020) Impact of COVID-19 on stroke admissions, treatments, and outcomes at a comprehensive stroke centre in the United Kingdom. Neurol Sci. 10.1007/s10072-020-04775-x2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoyer C, Ebert A, Huttner HB, Puetz V, Kallmünzer B, Barlinn K, et al. (2020) Acute stroke in times of the COVID-19 pandemic. Stroke 51:2224–2227 3. doi: 10.1161/STROKEAHA.120.030395 [DOI] [PubMed] [Google Scholar]
- 3.Rudilosso S, Laredo C, Vera V, Vargas M, Renú A, Llull L, et al. (2020) Acute stroke care is at risk in the era of COVID-19. Stroke 51:1991–1995 doi: 10.1161/STROKEAHA.120.030329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kristoffersen ES, Jahr SH, Thommessen B, Rønning OM (2020) Effect of COVID-19 pandemic on stroke admission rates in a Norwegian population. Acta Neurol Scand 2020; 142:632–636. doi: 10.1111/ane.13307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meza HT, Lambea Gil Á, Saldaña AS, et al. on behalf of the NORDICTUS Investigators (2020) Impact of COVID-19 outbreak on ischemic stroke admissions and in-hospital mortality in north-west Spain. Int J Stroke 15:755–762 8. doi: 10.1177/1747493020938301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sacco S, Ricci S, Ornello R, et al. (2020) Reduced admissions for cerebrovascular events during COVID-19 outbreak in Italy. Stroke 51:3746–3737 doi: 10.1161/STROKEAHA.120.031293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Y, Chen F, Wang Z, Feng W, Liu Y, Wang Y, et al. (2020) Reductions in hospital admissions and delays in acute stroke care during the pandemic of COVID-19. Front Neurol 11:584734 12. doi: 10.3389/fneur.2020.584734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diegoli H, Magalhães PSC, Martins SCO, Moro CHC, França PHC, Safanelli J, et al. (2020) Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke 51:2315–2321 13. doi: 10.1161/STROKEAHA.120.030481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uchino K, Kolikonda MK, Brown D, Kovi S, Collins D, Khawaja Z, et al. (2020) Decline in stroke presentations during COVID-19 surge. Stroke 51:2544–2547. doi: 10.1161/STROKEAHA.120.030331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pasarikovski CR, da Costa L. The impact of COVID-19 pandemic on stroke volume. Can J Neurol Sciences 2021; 47: 847–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dowlatshahi D, Scott G, Bourgoin A et al. Decreased stroke presentation rates at a comprehensive stroke center during COVID-19. Can j Neurol Sciences. 2020; doi: 10.1017/cjn.2020.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwarz V, Mahfoud F, Lauder L et al. Decline of emergency admissions for cardiovascular and cerebrovascular events after the outbreak of COVID-19. Clinical Res Cardiology 2020; 109: 1500–1506. doi: 10.1007/s00392-020-01688-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perry R, Banaras A, Werring DJ, Simister R. What caused the fall in stroke admissions during the COVID-19 pandemic? J Neurol 2020; 267: 3457–3458. doi: 10.1007/s00415-020-10030-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akhtar Naveed, Salman Al Jerdi Ziyad Mahfoud, Imam Yahia, Kamran Saadat, Saqqur Maher, et al. The impact of the COVID-19 pandemic on Stroke Admissions in Qatar. BMJ Neurol Open; 2021. 3:e000084. doi: 10.1136/bmjno-2020-000084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehrpour M, Shuaib A, Farahani M et al. Coronavirus disease 2019 and stroke in Iran: a case series and effects on stroke admissions. International J Stroke 2020. Accepted 5 June 2020. doi: 10.1177/1747493020937397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bullrich MB, Fridman S, Mandzia J et al. COVID-19: Stroke admissions, emergency department visits, and prevention clinic referrals. Can J Neurol Sci 2020; 46: 693–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Sousa DA, Sandset EC, Elkind MSV. The curious case of the missing strokes during the COVID-19 pandemic. Stroke 2020; 51: 1921–1923. doi: 10.1161/STROKEAHA.120.030792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Powers WJ, Rabinstein AA, Ackerson T et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2019; 50 ([published correction appears in Stroke. 2019. Dec;50(12): e440–e441]): e344-e418 doi: 10.1161/STR.0000000000000215 [DOI] [PubMed] [Google Scholar]
- 19.Butt AA, Kartha AB, Masoodi NA et al. Hospital admission rates, length of stay and in-hospital mortality for common acute care conditions in COVID-19 vs pre-COVID-19 era. Public Health. 2020; 189: 6–12. doi: 10.1016/j.puhe.2020.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuitunen I, Ponkilainen VT, Launonen AP, Reito A, Hevonkorpi TP. The effect of national lockdown due to COVID-19 on emergency department visits. Scan J Trauma, Resuscitation and Emergency Med. 2020; 28: 114. doi: 10.1186/s13049-020-00810-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akhtar N, Kamran S, Singh R et al. Beneficial effects of implementing stroke protocols require establishment of a geographically distinct unit. Stroke 2015; 46:3494–3501; doi: 10.1161/STROKEAHA.115.010552 [DOI] [PubMed] [Google Scholar]
- 22.Akhtar N, Salam A, Kamran S et al. Ethnic variation in acute cerebrovascular disease: Analyses from the Qatar stroke registry. European Stroke Journal 2016; 1:231–241. doi: 10.1177/2396987316663776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Imam Y, Kamran S, Akhtar N et al. Incidence, clinical features and outcomes of atrial fibrillation and stroke in Qatar. International J Stroke 2019; 15: 85–89 doi: 10.1177/1747493019830577 [DOI] [PubMed] [Google Scholar]
- 24.Adam HP, Bendixen BH, Kappelle LJ et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute stroke treatment. Stroke 1993; 24: 35–41. doi: 10.1161/01.str.24.1.35 [DOI] [PubMed] [Google Scholar]
- 25.Clerkin KJ, Fried JA, Raikhelkar J et al. COVID-19 and cardiovascular disease. Circulation. 2020; 141: 1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941 [DOI] [PubMed] [Google Scholar]
- 26.Mahham MM, Spata E, Goldacre R et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in Endland. Lancet 2020; 396: 381–389. doi: 10.1016/S0140-6736(20)31356-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Katsouras C, Karapanayiotides T, Papafaklis M et al. Greater decline in acute stroke admissions compared with acute coronary artery syndromes during COVID-19 outbreak in Greece: Cerebro/cardiovascular implications amidst a second wave surge. Eur J Neurol. 2020; doi: 10.1111/eme.14666 [DOI] [PubMed] [Google Scholar]
- 28.Oxley TJ, Mocco J, Majidi S et al. Large-vessel stroke as a presenting feature of COVID_19 in the young. New Eng J Med 2020; published on-line April 28. doi: 10.1056/NEJMc2009787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lodigiani C, Iapichino I, Carenzo L et al. Venous and arterial thrombotic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thrombosis Research. 2020; 191: 9–14 doi: 10.1016/j.thromres.2020.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Solomon IH, Normindin E, Bhattacharyya S et al. Neuropathological features of COVID-19. New Eng Medical J. 2020; 383: 989–992. doi: 10.1056/NEJMc2019373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wichmann D, Sperhake J-P, Lutgehetmann M et al. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann Internal Medicine. 2020; doi: 10.7326/M20-2003 [DOI] [PubMed] [Google Scholar]
- 32.Matschke J, Lutgehetmann M, Hagel C et al. Nuropathology of patients with COVID-19 in Germany. Lancet Neurol. 2020; 19: 919–929. doi: 10.1016/S1474-4422(20)30308-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kristoffersen ES, Jahr SH, Faiz KW, Thommessen B, Ronning OM. Stroke admission rates before, during and after the first phase of the COVID-19 pandemic. Neurol Sci 2020. Doi.org/10.1007/s10072-021-05039-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.British Heart Foundation. https://www.bhf.org.uk/what-we-do/news-from-the-bhf/news-archive/2020/april/drop-in-heart-attack-patients-amidst-coronavirus-outbreak (12 August 2020.
- 35.Schlachetzki F, Wilfling S, Hubert ND et al. Decline and recurrence of stroke consultations during the COVID-19 pandemic lockdown parallels population activity levels. Cerebrovascular diseases. 2021; doi: 10.1159/000514154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mariet A-A, Giroud M, Benzenine E et al. Hospitalizations for stroke in France during COVID-19 pandemic before, during and after the national lockdown. Stroke 2021; 52: 00–00. doi: 10.1161/STROKEAHA.120.032312 [DOI] [PubMed] [Google Scholar]
- 37.Qian Z, Kang H, Tang K et al. Assessment of risk of aneurysmal rupture in patients with normotensive and uncontrolled hypertension. J Stroke and CVD. 2016; 25:1746–52. [DOI] [PubMed] [Google Scholar]
- 38.Kato A, Minami Y, Katsura A et al. Physical exersion as a trigger of acute coronary artery syndrome caused by plaque erosion. J Thromb Thrombolysis. 2020; 49: 377–85. doi: 10.1007/s11239-020-02074-y [DOI] [PubMed] [Google Scholar]
- 39.Grau AJ, Urbanek C, Palm F. Common infections and the risk of stroke. Nat Rev Neurol. 2010, 12: 681–94. doi: 10.1038/nrneurol.2010.163 [DOI] [PubMed] [Google Scholar]
- 40.Hall ME, Vaduganathan M Khan et al. Reductions in heart failure hospitalizations during COVID-19 pandemic. J Card Failure 2020; 26: 462–63. doi: 10.1016/j.cardfail.2020.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Holt A, Gislason GH, Schou M et al. New onset atrial fibrillation: incidence, characteristics, and related events following a national COVID-19 related lockdown. Eur Heart 2020; 41: 3072–79. [DOI] [PMC free article] [PubMed] [Google Scholar]