Abstract
This case report documents treatment of a 32-year-old male patient after being extricated from an extensively damaged motor vehicle after a collision. On first presentation, the patient had a Glascow Coma Score of 14 and a pan-scan revealed a severely comminuted fracture of the proximal left femoral shaft, a fracture of the left patella, and multiple rib fractures. A neurological exam on a later evaluation showed global aphasia and sharp decline in movements of the right upper and lower extremities even with painful stimuli. A CT Angiography of the head and neck was obtained and revealed evidence of occlusion in the upper cervical segment and proximal petrous segment of the left internal carotid artery (ICA). Two 6x40mm precise stents were placed restoring normal intracranial flow to the patient's left ICA. The patient was discharged having sensation and motor function in all extremities and with resolved aphasia and no neurologic deficits.
Keywords: Blunt cerebrovascular injury, Neurologic deficits
Introduction
Blunt cerebrovascular injury (BCVI) is an injury to the carotid or vertebral arteries secondary to non-penetrating trauma. While it was previously presumed that BVCI was a rare occurrence, the most recent literature indicates an occurrence of 1–2% in the hospitalized trauma population, with an incidence of up to 9% in trauma patients with severe head injury [1]. A common screening tool is the expanded modifications of the Denver criteria for BCVI screening initiated in 2011 [2]. Expansion of the criteria was ultimately explored subsequent to recognizing that the original criteria resulted in a 20% BCVI diagnosis deficit [3], [4]. We present the case of a 32-year old male presenting to our hospital with polytrauma following a motor vehicle collision with an occlusion in the upper cervical segment and proximal petrous segment of the left internal carotid artery. The following is the care and treatment of this rare event.
Case report
A 32-year-old male patient who presented to our hospital via Medflight air critical care transportation with polytrauma subsequent to a motor vehicle accident. The patient did have a prolonged extrication time of approximately 15 min secondary to extensive vehicle damage. While loss of consciousness was denied, patient did present with a Glascow Coma Score of 14 (E-4, V-4, M-6), due to confusion on arrival. The patient's emergent trauma pan-scan was remarkable for a severely comminuted fracture of the proximal left femoral shaft and an old dorsal endplate compression fracture of T12 with stable pedicle screw fixation. Further x-rays of the extremities also indicated a right-sided nondisplaced fracture of inferior aspect of the patella, multiple fractures of the second, third, and fourth digits on the left foot. Pulmonary contusions were identified as well as right-sided fractures of ribs 4, 5, 6, and 7 with a left-sided fracture of rib 5.
On repeat evaluation, approximately 2 h later, the patient's neurologic exam declined with significant movement deficits to the right upper extremity, minimal movement to painful stimuli in the right lower extremity, and global aphasia. CTA of the head and neck was obtained with evidence of occlusion in the upper cervical segment and proximal petrous segment of the left internal carotid artery. An unremarkable CT of the head was obtained, and a CT cerebral perfusion analysis was obtained with evidence of hypoperfusion in the territory of the left middle cerebral artery (MCA) and the anterior cerebral artery (ACA). A cerebral angiogram revealed very poor collateral flow with occlusive left ICA dissection at the petrous segment of the carotid (Fig. 1). The decision was made to proceed with placement of two 6x40mm precise stents. Post treatment angiography demonstrated normal intracranial flow with patient left ICA (Fig. 2). The patient was subsequently initiated on eptifibatide, a platelet aggregate inhibitor, in addition to dual antiplatelet therapy with aspirin and clopidogrel.
Fig. 1.
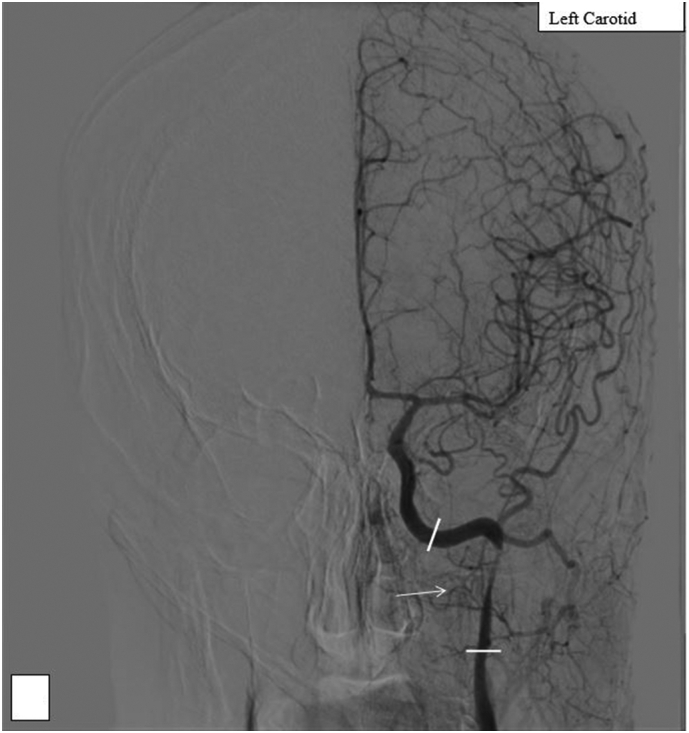
A: Type IV vessel occlusion; white blocks indicate the approximate boundaries of the petrous segment of carotid, white arrow points to area of occlusion.
Fig. 2.
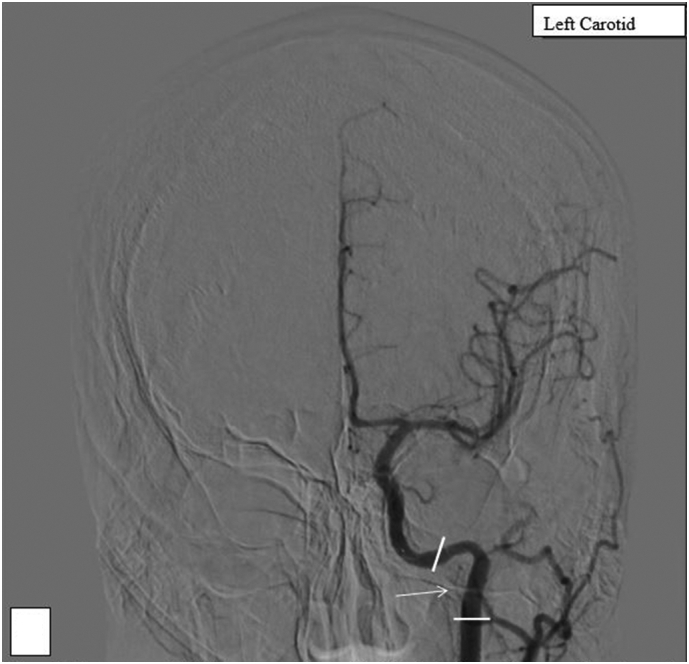
B: patency of L ICA post-stenting; white blocks indicate the approximate boundaries of the petrous segment of carotid, white arrow points to area of occlusion, resolved.
Immediate post intervention assessment did reveal persistent aphasia and right-sided weakness prompting an MRI brain evaluation. This revealed innumerable bilateral small infarcts, with the left greater than the right and concern for right-sided vascular injury. Upon negative embolic work up, the patient was taken for repair of the orthopedic injuries. This included an intramedullary nail of the left femur and irrigation/debridement of the right patella. Neurology evaluation recommended continued dual antiplatelet therapy, and cardiac evaluation where transthoracic and transesophageal echocardiograms were both unremarkable for cardiac abnormalities and intracardiac thrombus. The patient was transferred out of the ICU on post-trauma day 4.
Near the end of the patient's nine-day hospital course, the patient did have sensation and motor function in all extremities, his aphasia had resolved, and he was tolerating an oral diet. The patient was treated with dual antiplatelet therapy, physical therapy, and occupational therapy during his hospital course. The patient did struggle with balance secondary to his orthopedic injuries, however, but did not demonstrate any neurologic deficits.
Discussion
Several guidelines exist regarding BCVI screening – including the Memphis criteria [5] and the Boston guidelines [6]; the modified Denver criteria is the most studied in the literature, and the most commonly utilized [2]. Interestingly, this patient did not meet initial screening criteria until he developed aphasia and lateralizing symptoms. The modified Denver criteria recommend screening investigation with CTA as described in Table 1. and upon the result of this CTA, this patient received swift neurologic intervention [7].
Table 1.
Extended Denver criteria [2].
| Extended Denver criteria for screening investigation of BCVI |
|---|
|
BCVI, over half of which are caused by motor vehicle accidents [8], are classified based on the Biffl grading system developed in 1999 as described in Table 2 [9]. General management guidelines based on the Biffl scale have been developed; guidelines suggest an initial treatment with antiplatelet therapy for grades I–IV, with long term suggestions for antiplatelets therapy until healing or intervention for grades I–III and life-long antiplatelet therapy for grade IV. A Biffl grade V is treated entirely differently with immediate pressure on oozing sites, with the need for emergent intervention and no data regarding long term treatment [10].
Table 2.
Biffl classification of cerebrovascular injuries [14].
| Grade of injury | Description |
|---|---|
| Type I | Luminal irregularity or dissection with <25% narrowing |
| Type II | Dissection or intramural hematoma with ≥25% luminal narrowing |
| Type III | Pseudoaneurysm |
| Type IV | Vessel occlusion |
| Type V | Vessel transection with free extravasation |
His Biffl grade IV lesion was treated with endovascular intervention with stenting of the internal carotid due to stroke symptoms, hypoperfusion in the territory of the left MCA, hypoperfusion in the territory of the left ACA, and poor collateral flow. His treatment restored neurologic function with no immediate complications, which is promising for potential future treatments. The ideal strategy for endovascular therapy for patients with acute ICA occlusions is still being investigated (Table 3). Currently, both anterograde and retrograde approaches exist, which vary in stenting sequence. However, the current literature and this case report a favorable outcome with neurointervention in patients with acute ICA occlusions [11], [12], [13].
Table 3.
Stent indications [15].
| Indications for endovascular stent placement |
|---|
|
| Additional Biffl et al. recommendations: |
|---|
|
Conclusion
BCVIs are an important consideration with significant quality of life consequences for patients in the trauma setting. While guidelines for screening investigations may continue to be evaluated and improved, we would like to emphasize the consideration of BCVI in patients with high-energy injuries with acute mental status changes and the potential need for urgent neurointervention.
Declaration of competing interest
No conflicts of interest to disclose by any of the authors, either financial or personal.
Contributor Information
Leva Gorji, Email: leva.gorji@ketteringhealth.org.
Ragavan Narayanan, Email: Ragavan.narayanan@ketteringhealth.org.
Christa Siebenburgen, Email: christa.siebenburgen@ketteringhealth.org.
References
- 1.Brommeland T., Helseth E., Aarhus M., et al. Best practice guidelines for blunt cerebrovascular injury (BCVI) Scand. J. Trauma Resusc. Emerg. Med. 2018;26:90. doi: 10.1186/s13049-018-0559-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geddes A.E., Burlew C.C., Wagenaar A.E., Biffl W.L., Johnson J.L., Pieracci F.M., Campion E.M., Moore E.E. Expanded screening criteria for blunt cerebrovascular injury: a bigger impact than anticipated. Am. J. Surg. 2016;212(6):1167–1174. doi: 10.1016/j.amjsurg.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 3.Emmett K.P., Fabian T.C., DiCocco J.M., Zarzaur B.L., Croce M.A. Improving the screening criteria for blunt cerebrovascular injury: the appropriate role for computed tomography angiography. J Trauma. 2011;70(5):1058–1063. doi: 10.1097/TA.0b013e318213f849. discussion 1063-5. [DOI] [PubMed] [Google Scholar]
- 4.Nagpal P., Policeni B.A., Bathla G., Khandelwal A., Derdeyn C., Skeete D. Blunt cerebrovascular injuries: advances in screening, imaging, and management trends. AJNR Am. J. Neuroradiol. 2017;39(3):406–414. doi: 10.3174/ajnr.A5412. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagpal P., Policeni B.A., Bathla G., Khandelwal A., Derdeyn C., Skeete D. Blunt cerebrovascular injuries: advances in screening, imaging, and management trends. AJNR Am J Neuroradiol. 2017;39(3):406–414. doi: 10.3174/ajnr.A5412. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bajkó Z., Maier S., Moţăţăianu A., et al. Stroke secondary to traumatic carotid artery injury - a case report. J. Crit. Care Med. (Targu Mures) 2018;4(1):23–28. doi: 10.1515/jccm-2018-0003. Published 2018 Feb 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buch K., Nguyen T., Mahoney E., et al. Association between cervical spine and skull-base fractures and blunt cerebrovascular injury. Eur. Radiol. 2016;26:524–531. doi: 10.1007/s00330-015-3858-1. [DOI] [PubMed] [Google Scholar]
- 8.Cogbill T.H., Moore E.E., Meissner M., Fischer R.P., Hoyt D.B., Morris J.A., Shackford S.R., Wallace J.R., Ross S.E., Ochsner M.G., et al. The spectrum of blunt injury to the carotid artery: a multicenter perspective. J. Trauma. 1994;37(3):473–479. doi: 10.1097/00005373-199409000-00024. [DOI] [PubMed] [Google Scholar]
- 9.Biffl W.L., Moore E.E., Offner P.J., Brega K.E., Franciose R.J., Burch J.M. Blunt carotid arterial injuries: implications of a new grading scale. J. Trauma. 1999;47:845–853. doi: 10.1097/00005373-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Foreman P.M., Griessenauer C.J., Kicielinski K.P., et al. Reliability assessment of the Biffl Scale for blunt traumatic cerebrovascular injury as detected on computer tomography angiography [published correction appears in J Neurosurg. 2017 Sep;127(3):702] J. Neurosurg. 2017;127(1):32–35. doi: 10.3171/2016.7.JNS16849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller Preston R., Fabian Timothy C., Croce Martin A., Cagiannos Catherine, Williams J.Scott, Vang Meng, Qaisi Waleed G., Felker Richard E., Timmons Shelly D. Prospective screening for blunt cerebrovascular injuries: analysis of diagnostic modalities and outcomes. Ann. Surg. 2002;236(3):386–395. doi: 10.1097/01.SLA.0000027174.01008.A0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li W., Yin Q., Xu G., Liu X. Treatment strategies for acute ischemic stroke caused by carotid artery occlusion. Interv Neurol. 2016;5(3–4):148–156. doi: 10.1159/000445304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foreman P.M., Griessenauer C.J., Kicielinski K.P., et al. Reliability assessment of the Biffl Scale for blunt traumatic cerebrovascular injury as detected on computer tomography angiography [published correction appears in J Neurosurg. 2017 Sep;127(3):702] J. Neurosurg. 2017;127(1):32–35. doi: 10.3171/2016.7.JNS16849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biffl W.L., Moore E.E., Offner P.J., Brega K.E., Franciose R.J., Burch J.M. Blunt carotid arterial injuries: implications of a new grading scale. J. Trauma. 1999;47(5):845–853. doi: 10.1097/00005373-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Lee T.S., Ducic Y., Gordin E., Stroman D. Management of carotid artery trauma. Craniomaxillofac. Trauma Reconstr. 2014;7(3):175–189. doi: 10.1055/s-0034-1372521. [DOI] [PMC free article] [PubMed] [Google Scholar]


