Abstract
Access to transplant centers is a key barrier for kidney transplant evaluation and follow-up care for both the recipient and donor. Potential kidney transplant recipients and living kidney donors may face geographic, financial, and logistical challenges in engaging with a transplant center and maintaining post-transplant continuity of care. Telemedicine via synchronous video visits has the potential to overcome the access barrier to transplant centers. Transplant centers can start the evaluation process for potential recipients and donors via telemedicine, especially for those who have challenges to come for an in-person visit or when there are restrictions on clinic capacities, such as during a pandemic. Likewise, transplant centers can utilize telemedicine to sustain post-transplant follow-up care while avoiding the burden of travel and its associated costs. However, expansion to telemedicine-based kidney transplant services is substantially dependent on telemedicine infrastructure, insurer policy, and state regulations. In this review, we discuss the practice of telemedicine in kidney transplantation and its implications for expanding access to kidney transplant services and outreach from pre-transplant evaluation to post-transplant follow-up care for the recipient and donor.
Keywords: Telehealth, Access to Health Services, Kidney Transplantation, Living Donors, Evaluation and Follow-up care
INTRODUCTION
Over 100,000 patients with kidney failure in the United States await kidney transplantation (KT).1 KT is the optimal therapy for most patients with kidney failure. It is associated with superior survival, better quality of life, and cost savings for the healthcare system when compared with dialysis.2,3 However, the number of kidney transplants achieved in the US remains far below the demand. In 2019, only 11,152 and 6,858 deceased and living donor kidney transplants were performed, respectively.4,5 In addition to the long wait time on the deceased donor kidney transplant waitlist, there are substantial variations in demographic characteristics and clinical outcomes in the recipient and donor.5–18 Racial disparities exist in the receipt of live donor kidney transplantation and the donor medical conditions after living kidney donation as well. 10–18 Moreover, patients with high socioeconomic status have higher likelihood of living donor kidney transplantation and lower mortality compared with those with low socioeconomic status.19 Efforts are thus needed to reduce disparities in KT and optimize outcomes.
Access to transplant centers is a key barrier for kidney transplant evaluation and follow-up care. Patients with geographic, financial, and logistical challenges face difficulties engaging with the transplant center,20–22 and those with reduced access have an increased risk of poor post-transplant outcomes.19 Telemedicine has the potential to increase access to transplant centers and ensure post-transplant continuity of care.23–26 The accelerated adoption of telemedicine during the coronavirus disease 2019 (COVID-19) pandemic has created both opportunities and challenges in health care delivery from a distance,27–29 in light of relaxed regulatory and financial burdens due to the Public Health Emergency (PHE) as determined by the US Department of Health and Human Services.23
In this review, we define telemedicine as a healthcare delivery platform using a live-video visit that permits real-time communications between the patient and provider at a distant site. We discuss the practice of telemedicine in KT and its implications in expanding access to kidney transplant services and outreach from pre-transplant evaluation to post-transplant follow-up care for the recipient and donor.
TELEMEDICINE LIVE-VIDEO VISITS
Telemedicine via synchronous video visits involves a patient and provider interfacing remotely through computers, smartphones, or tablets using a secure videoconferencing software with a reliable internet connection. The patient can be located at a local medical facility or home (originating site), while the provider can be located at an office or a clinic (distant site). These virtual visits must comply with provider licensure regulations and Health Insurance Portability and Accountability Act (HIPPA) rules.30,31 Live-video visits from a distance could overcome the access barrier to transplant centers by offering kidney transplant services to patients who find it difficult and costly to travel to the transplant center.
TELEMEDICINE ADOPTION BY US TRANSPLANT CENTERS
Telemedicine adoption by US transplant centers was lagging prior to the COVID-19 pandemic. Cost and reimbursements are major barriers to telemedicine implementation.32 The originating sites restrictions are other hurdles limiting this practice.33 There were efforts to expand access to telemedicine in general for low-income patients, veterans, and patients residing in areas lacking access to sufficient health care.34 Additionally, the Bipartisan Budget Act of 2018 expanded telemedicine coverage for certain patient populations including home dialysis patients.35,36 Insurer reimbursements and state licensure restrictions, however, remained major barriers to telemedicine expansion.23
With the onset of the COVID-19 pandemic, there was a rapid adoption of telemedicine across US transplant centers due to relaxed regulations under the PHE and increased funding for telemedicine infrastructure through the Coronavirus Aid, Relief, and Economic Security (CARES) Act.37 A national survey assessing the early impact of the pandemic on US transplant centers found that 96.8% adopted telemedicine for care delivery, but 81% did report telemedicine challenges in a subsequent survey.27,28 Remarkably, despite the pandemic hurdles, telemedicine has allowed transplant centers to sustain pre-transplant evaluations of kidney failure patients and living kidney donor candidates and post-transplant continuity of care for both the recipient and donor.
PRE-TRANSPLANT TELEMEDICINE SERVICES
Potential kidney transplant recipients and living kidney donors may come from different geographic areas, and it is critical to expedite their evaluation process to reduce risks of adverse outcomes for kidney failure patients. Transplant centers can start the evaluation process for potential recipients via telemedicine, especially for those who have challenges to come for an in-person visit or when there are restrictions on clinic capacities, such as during the COVID-19 pandemic. Patients who are deemed candidates during the telemedicine visit can be listed as “inactive” on the waitlist. Laboratory and imaging tests and additional consults can be completed locally, and those who pass their tests will be required to come to the transplant center for a physical examination and meeting with the transplant team in-person before being listed as “active” for KT (Figure A). This approach could help kidney transplant candidates become listed preemptively and accrue time on the waitlist. This approach could also help reduce costs to the patient and healthcare system.23,25,38 Moreover, it can help patients who seek to be listed at multiple centers. In a single-center experience at a US Veterans Affairs transplant center, telemedicine use for pre-transplant evaluation was shown to save on cost and improve timeliness to evaluation, and hence, increase access to transplant.38
Figure.
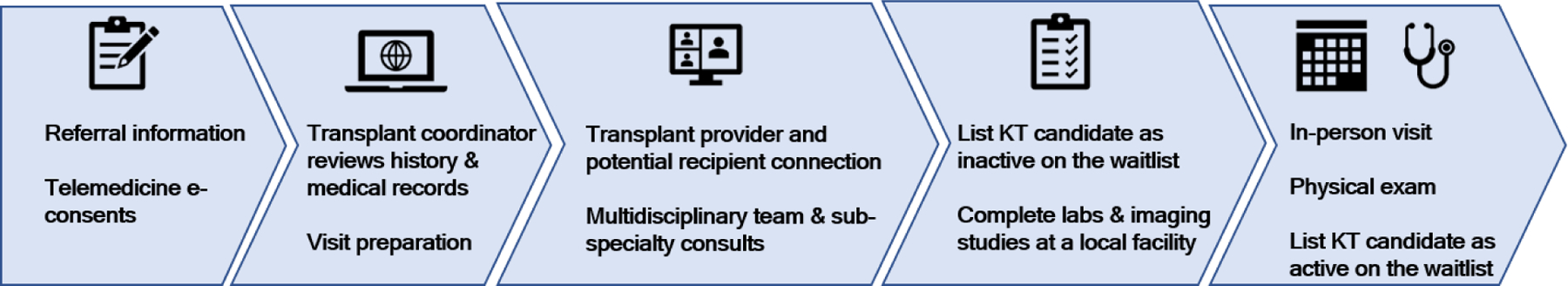
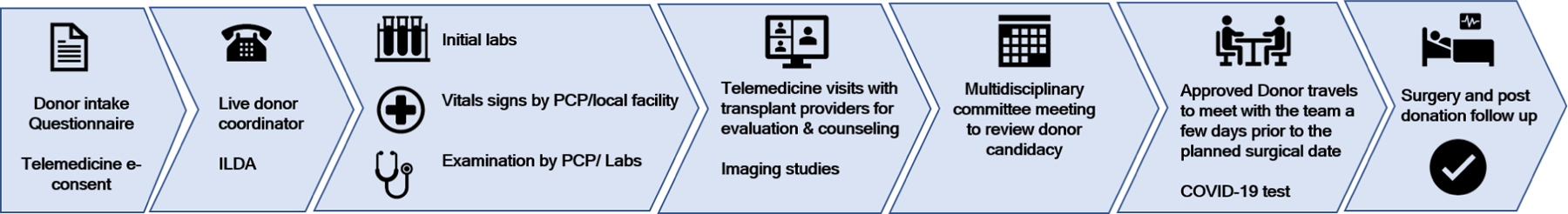
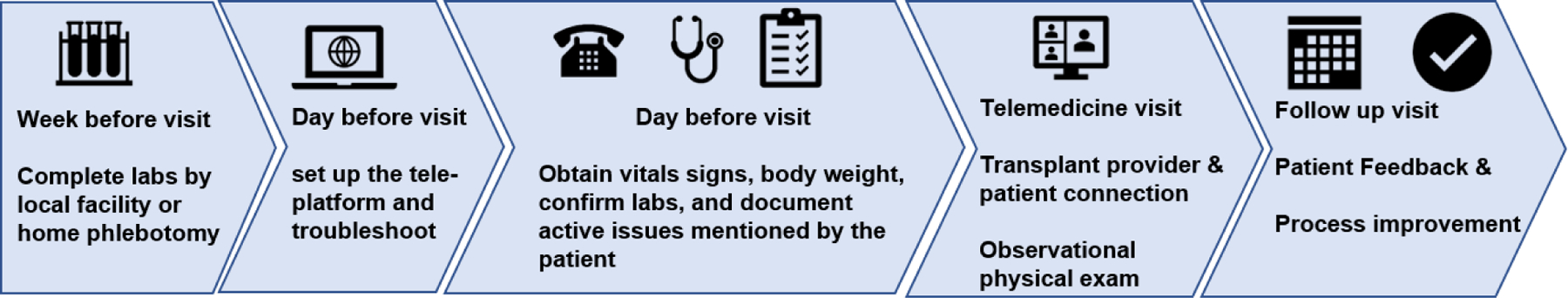
Telemedicine-based kidney transplant services*ᶧ
A. Pre-transplant evaluation of potential kidney transplant recipients via telemedicine
B. Pre-transplant evaluation of potential living kidney donors via telemedicine
C. Post-transplant follow-up care for recipients and donors via telemedicine
Abbreviations: KT, Kidney Transplantation; ILDA, Independent Live donor advocate.
*We define telemedicine as a healthcare delivery platform using a live-video visit that permits real-time communications between the patient and provider at a distant site.
ᶧInfographic by Anju Yadav, MD FASN.
Likewise, transplant centers can start the evaluation process for potential living kidney donors via telemedicine.39 Potential donors who live in different states from the transplant center, or who have difficulty traveling for their initial evaluation visit can be seen using telemedicine. During these initial remote evaluations, potential donors will be educated and counseled to make an informed decision regarding donation. Similar to the recipient approach, laboratory and imaging tests and additional consults can be completed locally. Vital signs can be obtained at a primary care physician’s office, local pharmacy, or local laboratory facility. If a potential donor is deemed a suitable donor by the transplant team, the donor candidate can then travel a few days prior to the scheduled KT date (Figure B). Telemedicine can therefore increase access to live donor kidney transplantation in a timely fashion, which is especially relevant with the limited number of available living donors. It is estimated that out of pocket cost to a living kidney donor is approximately $5000.40 Telemedicine has the potential to make the process financially neutral for donors irrespective of whether they proceed with live kidney donation or not.
POST-TRANSPLANT TELEMEDICINE SERVICES
Telemedicine has been shown to improve adherence, reduce unplanned admission rates and lengths of stay in first-year post-transplantation.41 In addition, it has also been shown to result in reduced need for travel and cost savings. In a single-center experience from Australia, 263 clinical reviews of regional post-transplant recipients were conducted through telemedicine with estimated savings of 203,202 kilometers in travel distance, 2771 hours in car travel time and AUD 31,948 in petrol expenses.42 In evaluating patient satisfaction with the appointment, most patients agreed that they received the same standard of care as they would have from an in-person visit.42 During the pandemic, telemedicine has provided a prompt and safe approach to transplant patients infected with COVID-19, which is especially important for immunosuppressed patients who may have prolonged viral shedding.24 Most transplant centers initiated and/or amplified their telemedicine platforms during the pandemic, thus ensuring continued safe care for patients.27,28 However, its use beyond the pandemic era cannot be ignored. As the transplant community navigates a new normal post-pandemic, we foresee that delivery of care through telemedicine will continue as part of a hybrid model. This hybrid model will allow transplant staff and patients to remain safe while helping off-load the burden of in-person visits. In this setting, home phlebotomy or local laboratory facilities can be utilized to provide the services required to deliver appropriate care in conjunction with telemedicine (Figure C).
The current care models have poor living kidney donor follow-up care with a large proportion of donors losing follow-up as early as six months post-donation across the US,43,44 despite the requirement that transplant centers complete data collection at 6, 12, and 24 months post-donation.45 Donor financial and logistical challenges and geographic distance from the transplant center are barriers to post-donation follow-up.43,46 Telemedicine can facilitate follow-up care while avoiding the burden of donor travel and its associated costs. However, there are scarce data as to how to best use telemedicine for post-donation follow-up care.
CRITERIA FOR PATIENTS WHO ARE MORE LIKELY TO BENEFIT FROM TELEMEDICINE
To answer the question of who are the ideal patients for telemedicine, the approach should be— who are the ones to benefit the most as this virtual platform facilitates access to care for patients at their convenience efficiently? Those who live a significant distance from the transplant center;43 who have difficulty to travel due to financial burdens or caregiving responsibility;46 who have difficulty to come for in-person visits due to workload or time conflicts; who need a routine follow-up for care of a stable medical condition; or who are at risk for infection exposure during a pandemic may benefit the most from telemedicine visits. Telemedicine can therefore improve adherence to clinic visits, with considerable cost-effective post-transplant care.41 As most patients currently have access to smartphones and fast internet,47 individuals with minimal technology knowledge can presumably navigate the visit, especially if support is provided for real-time troubleshooting.
INSURER POLICY AND STATE REGULATIONS
Medicare had historically restricted services using telemedicine before the pandemic. The beneficiary was required to be in a rural area and to travel to specific types of originating sites such as a doctor’s office, skilled nursing facility, or medical center. The originating site had to be in a Health Professional Shortage Area or a county that is outside of any Metropolitan Statistical Area.23 Notably, the beneficiary could not receive telemedicine services in their home.33 In early 2019, a few exceptions were made for both geographic and originating site requirements for telemedicine which included dialysis services; thus, patients on home dialysis may elect to receive monthly kidney failure clinical assessments via telemedicine.35,36 As a result of the pandemic, the Centers for Medicare & Medicaid Services (CMS) broadened access to Medicare telemedicine services with the 1135 waiver which started on March 6, 2020.23,33,37 Patients outside rural areas and in their homes were made eligible for telemedicine services. Medicare now reimburses telemedicine visits across the states and at the same rate as if these visits were in-person regardless of patient location and prior existing relationship with the provider (new or established patient).23 Several private payors have adopted a similar policy as CMS.48 Millions of Medicare beneficiaries may lose access to telemedicine services after the expiration of the PHE.49 Legislators are taking into consideration many proposals to expand telehealth services under Medicare beyond the PHE.
State licensing restrictions are a major barrier to expanding telemedicine practice.48 Strikingly, the CMS waivers expanding telemedicine across the states do not override the individual state’s licensing requirements.48 Some states prohibit out-of-state licensed providers from practicing telemedicine for new or established patients, while others limit this practice to established patients only.23 Although many states have released waivers under the PHE, they are inconsistent across states and remain restricted and short-term.50,51 Notably, many states waivers have already expired. As such there is urgent need for legislations that allow out-of-state transplant providers to practice telemedicine across states.23
BARRIERS AND CONSIDERATIONS
While insurer reimbursement and state regulations play a substantial role in restricting the practice of telemedicine,23 other barriers merit considerations. Infrastructure and personnel staffing must be supported by healthcare systems to ensure efficiency and high quality of care. This includes investment in appropriate technology and hiring of staff that allow providers and patients to utilize telemedicine more readily. Efforts to help establish a reliable internet connection are needed for patients in rural areas or those with low income. Training is needed for providers to address virtual delivery of care and physical examination. Education tools should be provided to patients to help navigate telemedicine visits with alternative options for those who fail to connect with providers remotely. Support for real-time troubleshooting should be available to both providers and patients. Patient privacy must be protected with adherence to HIPPA rules. Special accommodations are required for patients with language barriers since non-English speakers may be disadvantaged by telemedicine visits (Table).
Table.
Barriers for the adoption of telemedicine and proposed mitigation strategies
| Perspective | Barriers | Mitigation Strategies |
|---|---|---|
| Patient | • Perception of incomplete care • Perception of lack of rapport with the provider or that the visit is impersonal • Lack of equipment (computer, smartphone, or tablet) • Technology limitations and language barriers • No broad-band internet |
• Education and reassurance • Provide regular feedback • Patients’ regular feedback • Resources for real-time troubleshooting and technical support • Accommodations for patients with language barriers • Government support for a reliable internet connection |
| Provider | • Licensing restrictions • Lack of physical exam to assist in decision making • Inconsistent reimbursement • Concern for patient privacy • Technology limitations |
• Institutional support for multistate licensing • Education and training • Observational physical exam training • Institutional contract agreement with insurers • Institutional support to provide appropriate equipment, technology and staff support • Venue to allow providers to provide regular feedback |
| Institutional | • Lack of infrastructure • Lack of personnel staffing • Unclear cost/benefit ratio • Lack of buy-in • Inconsistent reimbursement |
• Infrastructure investment • staffing support • Assist providers in obtaining state licensing to improve involvement and reimbursement • Advocacy for promotion of telemedicine with government agencies |
| Regulatory | • Insurer reimbursement limitations • State licensing restrictions • Regulatory limitations • Consents/prescription regulations |
• Advocacy for global licensing • Support for telemedicine by public and private insurers • Homogenize and streamline regulations • Exemption to transplant centers |
FUTURE RESEARCH
With the increasing adoption of telemedicine to deliver transplant care, it will be important to examine its effect on transplant outcomes. This includes outcomes that assess access to transplantation such as rates and times to waitlist and transplantation, and post-transplant outcomes such as acute rejection rates, rehospitalization rates, and graft and patient survival. In particular, the effect of telemedicine in disparities in outcomes among minorities and those with limited resources must be examined. Other areas of research that would be of interest include the effect of telemedicine on patient engagement and cultural differences in patient willingness to participate in virtual visits.
CONCLUSIONS
Telemedicine has the potential to have a lasting impact on the field of kidney transplantation beyond the pandemic by making kidney transplant evaluation and follow-up care more accessible, efficient, and convenient for the recipient and donor. However, expansion of telemedicine-based kidney transplant services is substantially dependent on telemedicine infrastructure, insurer policy and state regulations. Federal and state legislations are needed to support the expansion of telemedicine practice which can reduce disparities in KT. As well, research studies are needed to assess the effectiveness of telemedicine in KT. The scope of telemedicine in KT can also be generalizable to other solid-organ transplants.
ACKNOWLEDGEMENTS
We thank the telemedicine workgroup, American Society of Transplantation living donor community of practice (AST LDCOP) for their feedback in how to best adopt telemedicine in kidney transplantation.
Funding/Support:
This study was supported by the following grant from the National Institute of Diabetes and Digestive and Kidney Diseases: K23DK129820 (awarded to Dr Al Ammary).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose.
REFERENCES
- 1.Hart A, Lentine KL, Smith JM, et al. OPTN/SRTR 2019 Annual Data Report: Kidney. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons 2021;21 Suppl 2:21–137. [DOI] [PubMed] [Google Scholar]
- 2.Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. The New England journal of medicine 1999;341(23):1725–1730. [DOI] [PubMed] [Google Scholar]
- 3.Laupacis A, Keown P, Pus N, et al. A study of the quality of life and cost-utility of renal transplantation. Kidney international 1996;50(1):235–242. [DOI] [PubMed] [Google Scholar]
- 4.Organ Procurement and Transplantation Network: National Data Reports https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/#. Accessed on Mar 27, 2021.
- 5.Al Ammary F, Yu Y, Ferzola A, et al. The first increase in live kidney donation in the United States in 15 years. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons 2020;20(12):3590–3598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Axelrod DA, Guidinger MK, Finlayson S, et al. Rates of solid-organ wait-listing, transplantation, and survival among residents of rural and urban areas. JAMA : the journal of the American Medical Association 2008;299(2):202–207. [DOI] [PubMed] [Google Scholar]
- 7.Epstein AM, Ayanian JZ, Keogh JH, et al. Racial disparities in access to renal transplantation--clinically appropriate or due to underuse or overuse? The New England journal of medicine 2000;343(21):1537–1544, 1532 p preceding 1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O’Hare AM, Johansen KL, Rodriguez RA. Dialysis and kidney transplantation among patients living in rural areas of the United States. Kidney international 2006;69(2):343–349. [DOI] [PubMed] [Google Scholar]
- 9.Joshi S, Gaynor JJ, Bayers S, et al. Disparities among Blacks, Hispanics, and Whites in time from starting dialysis to kidney transplant waitlisting. Transplantation 2013;95(2):309–318. [DOI] [PubMed] [Google Scholar]
- 10.Gore JL, Danovitch GM, Litwin MS, Pham PT, Singer JS. Disparities in the utilization of live donor renal transplantation. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons 2009;9(5):1124–1133. [DOI] [PubMed] [Google Scholar]
- 11.Purnell TS, Luo X, Cooper LA, et al. Association of Race and Ethnicity With Live Donor Kidney Transplantation in the United States From 1995 to 2014. JAMA : the journal of the American Medical Association 2018;319(1):49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Waterman AD, Peipert JD, Hyland SS, McCabe MS, Schenk EA, Liu J. Modifiable patient characteristics and racial disparities in evaluation completion and living donor transplant. Clinical journal of the American Society of Nephrology : CJASN 2013;8(6):995–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar K, Tonascia JM, Muzaale AD, et al. Racial differences in completion of the living kidney donor evaluation process. Clin Transplant 2018;32(7):e13291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al Ammary F, Bowring MG, Massie AB, et al. The changing landscape of live kidney donation in the United States from 2005 to 2017. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons 2019;19(9):2614–2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reed RD, Sawinski D, Shelton BA, et al. Population Health, Ethnicity, and Rate of Living Donor Kidney Transplantation. Transplantation 2018;102(12):2080–2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al Ammary F, Luo X, Muzaale AD, et al. Risk of ESKD in Older Live Kidney Donors with Hypertension. Clinical journal of the American Society of Nephrology : CJASN 2019;14(7):1048–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muzaale AD, Massie AB, Al Ammary F, et al. Donor-Recipient Relationship and Risk of ESKD in Live Kidney Donors of Varied Racial Groups. American journal of kidney diseases : the official journal of the National Kidney Foundation 2020;75(3):333–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lentine KL, Schnitzler MA, Xiao H, et al. Racial variation in medical outcomes among living kidney donors. The New England journal of medicine 2010;363(8):724–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Axelrod DA, Dzebisashvili N, Schnitzler MA, et al. The interplay of socioeconomic status, distance to center, and interdonor service area travel on kidney transplant access and outcomes. Clinical journal of the American Society of Nephrology : CJASN 2010;5(12):2276–2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lynch RJ, Patzer RE. Geographic inequity in transplant access. Curr Opin Organ Transplant 2019;24(3):337–342. [DOI] [PubMed] [Google Scholar]
- 21.Purnell TS, Luo X, Crews DC, et al. Neighborhood Poverty and Sex Differences in Live Donor Kidney Transplant Outcomes in the United States. Transplantation 2019. [DOI] [PubMed]
- 22.Hamoda RE, McPherson LJ, Lipford K, et al. Association of sociocultural factors with initiation of the kidney transplant evaluation process. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons 2020;20(1):190–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al Ammary F, Sidoti C, Segev DL, Henderson ML. Health Care Policy and Regulatory Challenges for Adoption of Telemedicine in Kidney Transplantation. American journal of kidney diseases : the official journal of the National Kidney Foundation 2021;77(5):773–776. [DOI] [PubMed] [Google Scholar]
- 24.Abuzeineh M, Muzaale AD, Crews DC, et al. Telemedicine in the Care of Kidney Transplant Recipients With Coronavirus Disease 2019: Case Reports. Transplantation proceedings 2020;52(9):2620–2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Concepcion BP, Forbes RC. The Role of Telemedicine in Kidney Transplantation: Opportunities and Challenges. Kidney360 2020;1(5):420–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yadav A, Caldararo K, Singh P. Optimising the use of telemedicine in a kidney transplant programme during the coronavirus disease 2019 pandemic. J Telemed Telecare 2020:1357633×20942632. [DOI] [PMC free article] [PubMed]
- 27.Boyarsky BJ, Po-Yu Chiang T, Werbel WA, et al. Early impact of COVID-19 on transplant center practices and policies in the United States. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons 2020;20(7):1809–1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boyarsky BJ, Ruck JM, Chiang TP, et al. Evolving Impact of COVID-19 on Transplant Center Practices and Policies in the United States. Clin Transplant 2020;34(12):e14086. [DOI] [PubMed] [Google Scholar]
- 29.Lentine KL, Vest LS, Schnitzler MA, et al. Survey of US Living Kidney Donation and Transplantation Practices in the COVID-19 Era. Kidney international reports 2020;5(11):1894–1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.State Telehealth Laws and Reimbursement Policies Report. Center for Connected Health Policy https://www.cchpca.org/telehealth-policy/state-telehealth-laws-and-reimbursement-policies-report. Accessed on May 27, 2021.
- 31.Shachar C, Engel J, Elwyn G. Implications for Telehealth in a Postpandemic Future: Regulatory and Privacy Issues. JAMA : the journal of the American Medical Association 2020. [DOI] [PubMed]
- 32.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare 2018;24(1):4–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Medicare Telemedicine Health Care Provider Fact Sheet. Expansion of Telehealth With 1135 Waiver, March 6. 2020 https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed on Aug 15, 2021.
- 34.Promoting Telehealth for Low-Income Consumers. Federal Communications Commission (FCC) https://www.fcc.gov/document/fcc-proposes-100-million-connected-care-pilot-telehealth-program-0. Accessed May 19, 2020.
- 35.H.R.1892 - Bipartisan Budget Act of 2018 https://www.congress.gov/bill/115th-congress/house-bill/1892/text. Accessed on Jul 19, 2020.
- 36.Lew SQ, Sikka N. Operationalizing Telehealth for Home Dialysis Patients in the United States. American journal of kidney diseases : the official journal of the National Kidney Foundation 2019;74(1):95–100. [DOI] [PubMed] [Google Scholar]
- 37.Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020 https://www.congress.gov/116/plaws/publ123/PLAW-116publ123.pdf. Accessed on May 17, 2020.
- 38.Forbes RC, Rybacki DB, Johnson TB, Hannah-Gillis A, Shaffer D, Hale DA. A Cost Comparison for Telehealth Utilization in the Kidney Transplant Waitlist Evaluation Process. Transplantation 2018;102(2):279–283. [DOI] [PubMed] [Google Scholar]
- 39.Yadav Anju MMP, Singh Pooja Telehealth: A novel tool to make living donation simple and financially neutral American Transplant Congress,. 2020
- 40.Przech S, Garg AX, Arnold JB, et al. Financial Costs Incurred by Living Kidney Donors: A Prospective Cohort Study. Journal of the American Society of Nephrology 2018;29(12):2847–2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schmid A, Hils S, Kramer-Zucker A, et al. Telemedically Supported Case Management of Living-Donor Renal Transplant Recipients to Optimize Routine Evidence-Based Aftercare: A Single-Center Randomized Controlled Trial. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons 2017;17(6):1594–1605. [DOI] [PubMed] [Google Scholar]
- 42.Andrew N, Barraclough KA, Long K, et al. Telehealth model of care for routine follow up of renal transplant recipients in a tertiary centre: A case study. J Telemed Telecare 2020;26(4):232–238. [DOI] [PubMed] [Google Scholar]
- 43.Henderson ML, Thomas AG, Shaffer A, et al. The National Landscape of Living Kidney Donor Follow-Up in the United States. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons 2017;17(12):3131–3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Al Ammary F, Thomas AG, Massie AB, et al. The landscape of international living kidney donation in the United States. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons 2019;19(7):2009–2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Organ Procurement and Transplantation Network (OPTN) Policies https://optn.transplant.hrsa.gov/media/1200/optn_policies.pdf. Accessed on June 17, 2021.
- 46.Waterman AD, Dew MA, Davis CL, et al. Living-donor follow-up attitudes and practices in U.S. kidney and liver donor programs. Transplantation 2013;95(6):883–888. [DOI] [PubMed] [Google Scholar]
- 47.Mobile Fact Sheet. Pew Research Center. Internet & Technology Available at https://www.pewresearch.org/internet/fact-sheet/mobile/. Accessed on May 24, 2021.
- 48.Telehealth Coverage Policies in The Time Of COVID-19. The Center for Connected Health Policy https://www.cchpca.org/resources/covid-19-telehealth-coverage-policies. Accessed on May 17, 2021.
- 49.Public Health Emergency Declarations https://www.phe.gov/emergency/news/healthactions/phe/Pages/default.aspx. Accessed on Aug 19, 2021.
- 50.Policy changes during the COVID-19 Public Health Emergency https://www.telehealth.hhs.gov/providers/policy-changes-during-the-covid-19-public-health-emergency/. Accessed on May 21, 2021.
- 51.States Waiving Telehealth Licensure Requirements http://www.fsmb.org/advocacy/covid-19/. Accessed on Apr 19, 2021.


