Abstract
Background
Multilevel cervical pathology can often be addressed via anterior cervical discectomy and fusion (ACDF) or posterior cervical fusion (PCF). While posterior procedures may be technically easier for four-level pathology, there are advantages and disadvantages to both approaches that make it of interest to compare outcomes. The purpose was to compare perioperative adverse events and long-term cervical reoperation rates of four-level ACDF and PCF.
Methods
The 2010 to Q1 2020 PearlDiver MSpine database was queried. Patients undergoing isolated elective four-level ACDF or PCF were identified (excluding cases performed for trauma, neoplasm, and/or infections) and 1:1 matched based on age, sex, and comorbidities. Ninety-day adverse events were compared with univariate and multivariate analyses. Five-year incidences of subsequent cervical reoperations were also compared.
Results
A total of 3,714 patients 1:1 matched for four-level ACDF and PCF performed for degenerative pathologies were identified (1,857 for each of the study groups). On multivariate analysis controlling for age, sex, and comorbidities, PCF was found to have significantly greater odds ratios (OR) for any (OR 2.12), serious (OR 2.31), and minor (OR 1.95) adverse events, as well as for length of stay ≥3 days (OR 1.76), p<0.001 for each. However, PCF had nearly three times lower odds of dysphagia compared to ACDF (OR 0.36, p<0.001). At five years, four-level ACDF cases were found to have significantly higher reoperation rates compared to four-level PCF cases (26.3% vs 18.3%, p<0.001).
Conclusion
In evaluating four-level cervical cases, compared to anterior approach cases, posterior approach procedures were associated with approximately double the odds of any, serious, and minor adverse events, but around one third the rate of dysphagia and two thirds the rate of five-year reoperations. While the pathology may dictate surgical approach, this data suggests that the choice between four-level anterior versus posterior approach becomes a balance of risks/benefit considerations.
Keywords: Cervical myelopathy, Radiculopathy, Spinal arthrodesis, Big data, Multi-level cervical fusion, Stenosis, Dysphagia
Abbreviations: ACDF, anterior cervical discectomy and fusion; CI, confidence interval; CPT, Current Procedural Terminology; ECI, Elixhauser Comorbidity Index; ICD, International Classification of Disease; LOS, length of stay; PCF, posterior cervical fusion; OR, odds ratio; SD, standard deviation
Introduction
Cervical surgeries are commonly performed for degenerative conditions [1]. In the setting of multilevel spondylotic conditions, anterior cervical discectomy and fusion (ACDF) [2] versus posterior cervical fusion (PCF) may be considered [3,4]. While there are variables that may dictate approach, such as location of compression, cervical alignment, and surgeon preference, [5,6] there are situations where both are appropriate. The current study was developed to compare four-level cases where anterior versus posterior approaches were used.
As with any surgical decision making, the choice of anterior versus posterior cervical approaches for multi-level pathology is swayed by the relative risks and benefits. Notably, multi-level ACDF may be associated with risk of dysphagia and pseudoarthrosis [7], [8], [9]. Multi-level PCF may be associated with wound-related issues and surgical site pain [10,11]. While multi-level cases may be performed at variable levels, pathology most commonly presents at some subset of four levels (C3-C7) [11].
For ACDF, fewer level cases are the most common [12], but four-level cases account for approximately 2.4% of such cases [12]. Regarding treatment for multi-level cervical pathology, four-level ACDF and PCF have been compared with small sample sizes studies [8,10,[13], [14], [15]]. Zhai et al evaluated 19 patients that underwent four-level ACDF and 25 that underwent four-level PCF and found similar clinical and radiographical outcomes, though the small sample size limited their ability to control for confounders and obtain adequate power for outcome comparison [10]. Wang et al compared 26 patients with four-level ACDF and 32 patients with four-level PCF over two years, but similarly were limited by small sample size and short follow-up [15].
The current study attempts to address the gap in literature related to comparing outcomes of four-level anterior versus posterior cervical procedures. A large national administrative database was used to power such comparisons.
Methods
Study population
The current study used the 2010 and Q1 2020 PearlDiver MSpine national database (PearlDiver Technologies, Colorado Springs, CO, USA), which is a large administrative dataset containing records of over 1.1 million patients. Studies using the PearlDiver system and associated databases were granted exemption from our institution's Institutional Review Board.
Cases of isolated elective four-level ACDF and PCF performed for degenerative cervical pathologies were identified using Current Procedural Terminology (CPT) codes. ACDF cases were identified with CPT code 22551 and CPT code 22552 repeated three times. PCF cases were identified with CPT code 22600 with CPT code 22614 repeated three times.
Exclusion criteria were then applied. These included: age <18 years, circumferential fusions (posterior for anterior cases and anterior for posterior cases), corpectomies, osteotomies, non-cervical procedures, and cases performed for trauma, neoplasm, and infectious etiologies. Further, any patients who did not remain in the insurance coverage dataset for at least 90 days were excluded.
Age, sex, and Elixhauser Comorbidity Index (ECI, a commonly used comorbidity index) were abstracted from the dataset. ACDF and PCF cases were matched 1:1 based on these criteria using PearlDiver's exact match function.
Postoperative outcomes
Ninety-day incidence of adverse events, dysphagia, LOS ≥3 days, and readmissions were abstracted from the dataset. Adverse events were aggregated into categories of serious, minor, and any adverse events.
Serious adverse events were noted if there was the occurrence of sepsis, cardiac arrest, shock, pulmonary embolism, deep venous thrombosis, neurologic or other organ injury, surgical site infection, or osteomyelitis. Minor adverse events were noted if there was the occurrence of acute kidney injury, hematoma and hemorrhage not leading to shock, respiratory infections, urinary tract infections, wound disruptions, or seromas. Any adverse event noted if there was the occurrence of a serious or minor adverse event.
Dysphagia rates were tabulated using ICD-9 diagnosis codes 787.20 to 787.24 and 787.29, and ICD-10 diagnosis codes R13.10 to R13.14 and R13.19. Patients with length of stay (LOS) ≥3 days following the index procedure were identified and tabulated. Readmission rates were tabulated using PearlDiver's “Admission” function that identifies inpatient ICD-9 and ICD-10 codes.
Further cervical spine surgery within five years of the index procedure were then identified based on CPT codes for ACDF, PCF, cervical laminectomy, laminotomy, and other cervical spinal procedures such as exploration and hardware removal. These cervical reoperations were then subcategorized into anterior (A), posterior (P), or concurrent anterior and posterior (A/P) procedures.
Statistical analysis
Univariate analysis was performed to compare patient characteristics and postoperative complications using independent two-tailed Student's t-test for continuous variables and the Chi Square test for categorical variables. Multivariate logistic regression adjusting for age, sex, and ECI was used to ascertain odds ratios (OR) of 90-day adverse events. ORs and 95% confidence intervals (CI) were calculated for each variable.
Kaplan-Meier survival analysis was conducted for five-year cervical reoperation rate, and a log-rank test was used to compare cumulative incidence at five years. Patients lost to follow-up or deceased were censored at last known follow-up.
An alpha of 0.05 and significance of p < 0.05 was set for both the univariate and multivariate analyses. Statistical calculations were performed in RStudio statistical software and SPSS version 28 (IBM Corp., Armonk, NY). The cumulative incidence graph was created using GraphPad Prism, version 9 (GraphPad Software, San Diego, CA).
Results
Study population
A total of 3,714 matched patients that underwent a four-level cervical procedure met inclusion criteria for this study. Patients that underwent ACDF consisted of 1,857 (50.0%) cases and patients that underwent PCF consisted of 1,857 (50.0%) cases. Patient characteristics for each of the matched cohorts are summarized in Table 1.
Table 1.
Matched patient characteristics.
| Total |
4-Level ACDF |
4-Level PCF |
||||
|---|---|---|---|---|---|---|
| Value | % | Value | % | Value | % | |
| Total | 3,714 | 100.0% | 1,857 | 50.0% | 1,857 | 50.0% |
| Age, years, mean (SD) | 61.4 | (9.4) | 61.3 | (9.4) | 61.4 | (9.5) |
| Sex | ||||||
| Female | 1,928 | 51.9% | 964 | 51.9% | 964 | 51.9% |
| Male | 1,786 | 48.1% | 893 | 48.1% | 893 | 48.1% |
| Insurance Plan | ||||||
| Commercial | 2,443 | 65.8% | 1,219 | 65.6% | 1,224 | 65.9% |
| Medicaid | 157 | 4.2% | 82 | 4.4% | 75 | 4.0% |
| Medicare | 1,011 | 27.2% | 496 | 26.7% | 515 | 27.7% |
| Other | 103 | 2.8% | 60 | 3.2% | 43 | 2.3% |
| ECI, mean (SD) | 4.5 | (3.2) | 4.5 | (3.2) | 4.5 | (3.2) |
| Additional Diagnosis | ||||||
| Myelopathy | 1,805 | 48.6% | 904 | 48.7% | 901 | 48.5% |
| Radiculopathy | 1,134 | 30.5% | 562 | 30.3% | 572 | 30.8% |
1:1 Matching based on age, sex, and ECI Bold p-value = statistical significance at p<0.05
Abbreviations:
ACDF = Anterior Cervical Discectomy and Fusion
ECI = Elixhauser Comorbidity Index
PCF = Posterior cervical fusion
SD = Standard deviation
Ninety-day outcomes
Ninety-day outcomes are summarized in Table 2. Univariate analyses revealed significantly higher rates of 90-day aggregated any (23.4% vs 12.7%), serious (13.0% vs 6.1%), and minor (14.9% vs 8.4%) adverse events after four-level PCF cases compared to ACDF cases, p<0.001 for each. LOS ≥3 days was also noted to be significantly greater in the PCF cohort (19.5% vs 12.2%, p<0.001). However, dysphagia rate was greater in the ACDF cohort (8.7% vs 3.6%, p<0.001). No significant difference was noted for readmission rates.
Table 2.
Univariate and multivariate analyses of 90-day complications and length of stay.
| Total |
4-Level ACDF |
4-Level PCF |
Multivariate PCF relative to ACDF |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Value | % | Value | % | Value | % | p-value | ORa | 95% CI | p-value | ||
| Total | 3,714 | 100% | 1,857 | 50.0% | 1,857 | 50.0% | |||||
| Any Adverse Event | 670 | 18.0% | 236 | 12.7% | 434 | 23.4% | <0.001 | 2.12 | 1.78 | 2.53 | <0.001 |
| Serious Adverse Event | 355 | 9.6% | 113 | 6.1% | 242 | 13.0% | <0.001 | 2.31 | 1.83 | 2.93 | <0.001 |
| Sepsis | 59 | 1.6% | 13 | 0.7% | 46 | 2.5% | <0.001 | 3.56 | 1.96 | 6.91 | <0.001 |
| PE | * | * | * | * | 24 | 1.3% | 0.025 | 2.46 | 1.21 | 5.41 | 0.017 |
| DVT | 31 | 0.8% | 14 | 0.8% | 17 | 0.9% | 0.718 | 1.23 | 0.61 | 2.55 | 0.562 |
| Minor Adverse Event | 432 | 11.6% | 156 | 8.4% | 276 | 14.9% | <0.001 | 1.95 | 1.58 | 2.42 | <0.001 |
| Wound | 65 | 1.8% | 11 | 0.6% | 54 | 2.9% | <0.001 | 5.04 | 2.73 | 10.22 | <0.001 |
| Transfusion | * | * | * | * | 28 | 1.5% | 0.001 | 3.47 | 1.64 | 8.22 | 0.002 |
| AKI | 98 | 2.6% | 34 | 1.8% | 64 | 3.4% | 0.003 | 1.98 | 1.30 | 3.07 | 0.002 |
| UTI | 190 | 5.1% | 71 | 3.8% | 119 | 6.4% | 0.005 | 1.75 | 1.29 | 2.38 | <0.001 |
| Pneumonia | 121 | 3.3% | 46 | 2.5% | 75 | 4.0% | 0.010 | 1.68 | 1.16 | 2.47 | 0.007 |
| Hematoma | 49 | 1.3% | 21 | 1.1% | 28 | 1.5% | 0.388 | 1.37 | 0.78 | 2.45 | 0.281 |
| Dysphagia | 228 | 6.1% | 161 | 8.7% | 67 | 3.6% | <0.001 | 0.36 | 0.27 | 0.49 | <0.001 |
| LOS ≥3 days | 589 | 15.9% | 226 | 12.2% | 363 | 19.5% | <0.001 | 1.76 | 1.46 | 2.12 | <0.001 |
| Readmission | 378 | 10.2% | 203 | 10.9% | 175 | 9.4% | 0.143 | 0.81 | 0.65 | 1.01 | 0.064 |
Censored if one or more cohorts had <10 patients with a complication.
Odds ratio for PCF adjusted for age, sex, and ECI. Referent = ACDF Bold p-value = Statistical Significance at p<0.05.
Abbreviation:
ACDF = Anterior Cervical Discectomy and Fusion AKI = Acute kidney injury CI = Confidence interval DVT = Deep vein thrombosis ECI = Elixhauser Comorbidity Index LOS = Length of stay OR = Odds Ratio PCF = Posterior cervical fusion PE = Pulmonary embolism UTI = Urinary tract infection.
Multivariate logistic regression adjusting for potential residual differences in demographic and comorbidity profiles are summarized in Table 2 (right columns) and Fig. 1. Compared to ACDF, PCF was found to have significantly greater odds ratio for any (OR 2.12), serious (OR 2.31), and minor (OR 1.95) adverse events, as well as for length of stay ≥3 days (OR 1.76), p<0.001 for each. However, PCF had nearly three times lower odds of dysphagia compared to ACDF (OR 0.36, p<0.001). No significant difference was noted for readmission rates on multivariate analysis.
Fig. 1.
Forest plot of 90-day complications and length of stay adjusted odds ratios for posterior cervical fusion (PCF), with anterior cervical discectomy and fusion (ACDF) as the reference population. Select serious and minor adverse events shown.
Five-year reoperations
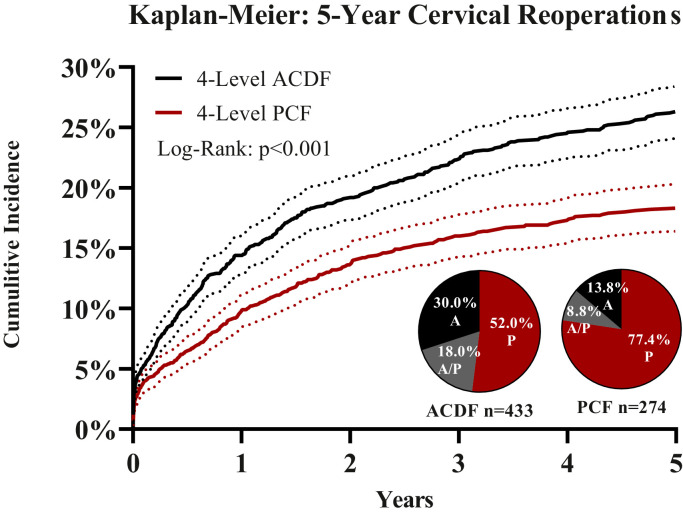
Over five years, ACDF cases had a mean follow-up +/- standard deviation (SD) of 4.1 +/- 1.4 years whereas PCF cases had a mean follow-up +/- SD of 3.9 +/- 1.5 years (Fig. 2). For five-year cervical reoperations, the cumulative incidence after ACDF cases was significantly greater than after PCF cases (26.3% vs 18.3%, p<0.001).
Fig. 2.
Five-year Kaplan-Meier survival plot of cervical reoperations for anterior cervical discectomy and fusion (ACDF) and posterior cervical fusion (PCF) that were actively covered under their insurance plan for up to five years. Log-rank test, p < 0.001. Pie charts demonstrate the type of subsequent cervical reoperation – anterior (A), posterior (P), or both (A/P).
For revision of index ACDF cases, posterior-only approaches were used in 52.0%, anterior-only approaches in 30.0%, and both anterior and posterior approaches in 18.0%. For revision of PCF cases, posterior-only approaches were used in 77.4%, anterior-only approaches in 13.8%, and both anterior and posterior approaches in 8.8%.
Discussion
The optimal surgical approach for multi-level degenerative cervical pathology, particularly for four-level disease, remains controversial. Options include anterior or posterior techniques, with four-level ACDF and four-level PCF available as treatment options [1,3,4]. The current study is the largest to date comparing short-term adverse events and long-term reoperation rates following four-level ACDF and PCF.
For four-level cases performed for degenerative cervical pathology, the current study found PCF to have approximately two-fold greater odds of aggregated 90-day any adverse event, serious adverse event, and minor adverse event compared to ACDF. This is in line with recent evidence from 2018-2021 that offers support to the notion that four-level ACDF may be safer and more efficacious than traditionally thought in appropriately selected patients [10,13,16]. Zhai et al. compared anterior (n=19) and posterior (n=25) approaches for management of four-level cervical degenerative diseases, and found that while postoperative patient reported and radiographical outcomes were similar, there were five patients with persistent axial symptoms or C5 palsy following posterior surgery that were not present following anterior surgery [10]. This supports our finding of aggregated 90-day adverse events being greater in the PCF cohort compared to the ACDF cohort, as persistent axial symptoms include pain, stiffness, and soreness.
Of the individual adverse events evaluated, dysphagia was notable in that it showed independent significance, with nearly three-fold greater odds for four-level ACDF than for four-level PCF. In the literature, multi-level anterior cervical fusions are known to be associated with a high incidence of dysphagia [10,17]. Jack et al. examined differences in clinical outcomes from baseline to minimum one-year follow up in patients that underwent four-level ACDF with or without concurrent posterior cervical fusion. While 18.3% reported early perioperative dysphagia – higher than what was found in this present study of 8.7% - this was transient and resolved for all but two patients [8].
When comparing long-term cervical reoperation rates, patients with ACDF had greater than 1.4-fold higher rate of 5-year cervical reoperations compared to those that underwent PCF (26.3% vs. 18.3%, p<0.001). Literature on long-term outcomes following four-level ACDF corroborates our findings that reoperation rates may be higher for four-level ACDF compared to PCF. The majority of revisions following ACDF are related to either adjacent segment disease or pseudoarthrosis [18]. Wang et al. compared ACDF to laminectomy with fusion (LF) to treat four-level cervical spondylotic myelopathy in 58 patients, and showed that while cervical lordosis and fused segment lordosis were improved in both groups after one week, after 24 months there was significantly greater loss of lordosis and a higher non-union rate in patients that underwent ACDF [15].
The current study does have limitations. As with other administrative database studies, it is reliant on the accuracy of administrative coding and the degree and details of the cervical pathology cannot be assessed. Thus, relevant factors such as severity of preoperative stenosis, degenerative instability, patient reported outcomes and pain/functional improvement should be evaluated in future prospective studies. Further, the specifics of the reoperations were limited based on the coding available. Notably, to keep the study cohorts and comparisons simple, other treatment options such as anterior hybrid discectomy/corpectomy cases and other posterior options such as laminoplasty were not assessed. Last, the study subjects were largely covered by commercial plans. As most patients on commercial plans are assumed to be of a higher socioeconomic status compared to those on Medicaid, the outcomes results of this study should be interpreted with this in mind. Despite these limitations, the large cohorts assessed in the current study have not been otherwise accessible in prior studies, allowing the current study to be powered for assessments not previously possible.
Conclusion
Overall, compared to four-level anterior approach cases, four-level posterior approach cases were associated with approximately double the odds of any, serious, and minor adverse events, but around one third the rate of dysphagia and two thirds the rate of five-year reoperations. While the pathology may dictate surgical approach, the cohorts studied here are much greater than previously reported for such studies and suggest that (if both are appropriately indicated options) the choice between four-level anterior versus posterior approach becomes a balance of risks/benefit considerations.
Declaration of Competing Interest
One or more authors declare potential competing financial interests or personal relationships as specified on required ICMJE Disclosure Forms.
Source of funding
No funding or financial support was provided for this study.
Footnotes
Given his role as Editor in Chief, Jonathan Grauer, MD had no involvement in the peer-review of this article and has no access to information regarding its peer-review. Full responsibility for the editorial process for this article was delegated to Tobias Mattei, MD.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.xnsj.2022.100115.
Appendix. Supplementary materials
References
- 1.Kato S, Fehlings M. Degenerative cervical myelopathy. Curr Rev Musculoskelet Med. 2016;9(3):263–271. doi: 10.1007/s12178-016-9348-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xiao SW, Jiang H, Yang LJ, Xiao ZM. Anterior cervical discectomy versus corpectomy for multilevel cervical spondylotic myelopathy: a meta-analysis. Eur Spine J. 2015;24(1):31–39. doi: 10.1007/s00586-014-3607-1. [DOI] [PubMed] [Google Scholar]
- 3.Neifert SN, Martini ML, Yuk F, et al. Predicting trends in cervical spinal surgery in the United States from 2020 to 2040. World Neurosurg. 2020;141:e175–ee81. doi: 10.1016/j.wneu.2020.05.055. [DOI] [PubMed] [Google Scholar]
- 4.Yang X, Gharooni AA, Dhillon RS, et al. The relative merits of posterior surgical treatments for multi-level degenerative cervical myelopathy remain uncertain: findings from a systematic review. J Clin Med. 2021;10(16) doi: 10.3390/jcm10163653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirabayashi K, Bohlman HH. Multilevel cervical spondylosis. Laminoplasty versus anterior decompression. Spine (Phila Pa 1976) 1995;20(15):1732–1734. doi: 10.1097/00007632-199508000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Jiang L, Tan M, Dong L, et al. Comparison of anterior decompression and fusion with posterior laminoplasty for multilevel cervical compressive myelopathy: a systematic review and meta-analysis. J Spinal Disord Tech. 2015;28(8):282–290. doi: 10.1097/BSD.0000000000000317. [DOI] [PubMed] [Google Scholar]
- 7.Wewel JT, Kasliwal MK, Adogwa O, Deutsch H, O’Toole JE, Traynelis VC. Fusion rate following three- and four-level ACDF using allograft and segmental instrumentation: a radiographic study. J Clin Neurosci. 2019;62:142–146. doi: 10.1016/j.jocn.2018.11.040. [DOI] [PubMed] [Google Scholar]
- 8.Jack MM, Lundy P, Reeves AR, Arnold PM. Four-level anterior cervical discectomy and fusions: results following multilevel cervical fusion with a minimum 1-year follow-up. Clin Spine Surg. 2021;34(4):E243–E2E7. doi: 10.1097/BSD.0000000000001116. [DOI] [PubMed] [Google Scholar]
- 9.Montano N, Ricciardi L, Olivi A. Comparison of anterior cervical decompression and fusion versus laminoplasty in the treatment of multilevel cervical spondylotic myelopathy: a meta-analysis of clinical and radiological outcomes. World Neurosurg. 2019;130:530–536. doi: 10.1016/j.wneu.2019.06.144. e2. [DOI] [PubMed] [Google Scholar]
- 10.Zhai JL, Guo SG, Nie L, Hu JH. Comparison of the anterior and posterior approach in treating four-level cervical spondylotic myelopathy. Chin Med J (Engl) 2020;133(23):2816–2821. doi: 10.1097/CM9.0000000000001146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Youssef JA, Heiner AD, Montgomery JR, et al. Outcomes of posterior cervical fusion and decompression: a systematic review and meta-analysis. Spine J. 2019;19(10):1714–1729. doi: 10.1016/j.spinee.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 12.Joo PY, Zhu JR, Kammien AJ, Gouzoulis MJ, Arnold PM, Grauer JN. Clinical outcomes following one-, two-, three-, and four-level anterior cervical discectomy and fusion: a national database study. Spine J. 2021 doi: 10.1016/j.spinee.2021.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Kreitz TM, Hollern DA, Padegimas EM, et al. Clinical outcomes after four-level anterior cervical discectomy and fusion. Global Spine J. 2018;8(8):776–783. doi: 10.1177/2192568218770763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McClure JJ, Desai BD, Shabo LM, et al. A single-center retrospective analysis of 3- or 4-level anterior cervical discectomy and fusion: surgical outcomes in 66 patients. J Neurosurg Spine. 2020:1–7. doi: 10.3171/2020.6.SPINE20171. [DOI] [PubMed] [Google Scholar]
- 15.Wang B, Lu G, Kuang L. Anterior cervical discectomy and fusion with stand-alone anchored cages versus posterior laminectomy and fusion for four-level cervical spondylotic myelopathy: a retrospective study with 2-year follow-up. BMC Musculoskelet Disord. 2018;19(1):216. doi: 10.1186/s12891-018-2136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basques BA, Louie PK, Mormol J, et al. Multi- versus single-level anterior cervical discectomy and fusion: comparing sagittal alignment, early adjacent segment degeneration, and clinical outcomes. Eur Spine J. 2018;27(11):2745–2753. doi: 10.1007/s00586-018-5677-y. [DOI] [PubMed] [Google Scholar]
- 17.Lu DC, Tumialan LM, Chou D. Multilevel anterior cervical discectomy and fusion with and without rhBMP-2: a comparison of dysphagia rates and outcomes in 150 patients. J Neurosurg Spine. 2013;18(1):43–49. doi: 10.3171/2012.10.SPINE10231. [DOI] [PubMed] [Google Scholar]
- 18.Laratta JL, Reddy HP, Bratcher KR, McGraw KE, Carreon LY, Owens RK., 2nd. Outcomes and revision rates following multilevel anterior cervical discectomy and fusion. J Spine Surg. 2018;4(3):496–500. doi: 10.21037/jss.2018.06.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.