Take Home Message
Rezūm is an effective surgical treatment option for bladder outflow obstruction that allows maintenance of sexual function. The retreatment rate could be further improved by ensuring adequate median lobe treatment and recognising when a simultaneous bladder-neck incision should be considered.
Keywords: Benign prostatic hyperplasia, Lower urinary tract symptoms, Minimally invasive therapy, Rezūm, Water vapour therapy, Reoperation
Abstract
Background
Rezūm water vapour ablation is an effective minimally invasive surgical therapy for the treatment of bladder outflow obstruction.
Objective
To present early outcomes and reoperation rates after Rezūm, including an analysis of retreatment rates to gain an insight into optimal patient selection and the durability of the procedure.
Design, setting, and participants
Data were prospectively collected for consecutive patients undergoing Rezūm for symptomatic benign prostatic hyperplasia between March 2017 and January 2020 at two hospital sites.
Intervention
Rezūm treatment of the prostate.
Outcome measurements and statistical analysis
Patients were reviewed at 6 wk and 3, 6, and 12 mo after their Rezūm procedure. We evaluated changes in urinary symptoms and the retreatment rate.
Results and limitations
A total of 461 patients undergoing Rezūm were analysed. The mean (±standard deviation) follow-up duration was 16.7 ± 10.4 mo. The mean patient age was 67.5 ± 7.8 yr and the mean prostate volume was 56.5 ± 24.0 ml. There was a significant improvement in mean maximum flow rate and postvoid residual volume and in International Prostate Symptom Score and quality-of-life scores (p < 0.0001). During the follow-up period, 21 patients (4.6%) required retreatment, of which 11 cases (2.4%) were within the first year. The retreatments included eight bladder neck incisions or resections, six transurethral resections of the prostate, four Greenlight laser photoselective vaporisations of the prostate, and three Rezūm procedures. The median length of time to a further operation was 11.5 mo (range 3–34). The most common findings at reoperation were an inadequately treated median lobe, an obstructing bladder neck, and in some cases asymmetry of the prostate cavity or recesses within the prostate gland.
Conclusions
This study demonstrates that the beneficial effects of Rezūm observed in the pivotal phase 2 randomised study are transferable to a real-world population with a comparable early retreatment rate. A range of procedures were used for retreatment. The factors dictating which option to select were based on patient concerns regarding side effects, gland volume, symptom profile, and cystoscopy findings.
Patient summary
We investigated outcomes for patients undergoing Rezūm, a water vapour treatment to reduce the size of the prostate in men with obstruction of the bladder outlet because of benign prostate enlargement. This technique yields significant improvements in symptoms and preserves sexual function. The proportion of men needing retreatment was 2.4% in the first year after their Rezūm procedure.
1. Introduction
Lower urinary tract symptoms (LUTS) in men are most commonly caused by bladder outflow obstruction (BOO) secondary to benign prostatic hyperplasia (BPH). The prevalence of BPH increases with age; a meta-analysis has demonstrated an increase from 14.8% among men aged 40–49 yr to 36.8% among those aged 70–79 yr [1]. For decades, transurethral resection of the prostate (TURP) was the gold standard of treatment for LUTS secondary to BPH. In recent years several new minimally invasive surgical therapies (MISTs) have been developed in an attempt to reduce surgical morbidity and enhance the patient experience.
Rezūm is a recent addition to the MIST armamentarium, which also includes procedures such as Urolift and the temporary implanted nitinol device (iTIND). Rezūm uses the convective heat energy of water vapour to ablate obstructive prostatic tissue. The pivotal Rezūm phase 2 study was a multicentre randomised controlled study including patients aged >50 yr with an International Prostate Symptom Score (IPSS) ≥13, maximum urinary flow rate (Qmax) ≤15 ml/s, and prostate volume of 30–80 ml. The study demonstrated a significant improvement in LUTS to 5 yr, with no reports of sexual dysfunction following Rezūm [2].
Preservation of sexual function following Rezūm offers a significant advantage to both traditional surgical treatments, such as TURP, as well as pharmaceutical treatment. As a result we have observed an increasing number of men requesting Rezūm. However, as a relatively new procedure there is a need to better understand its durability and refine the surgical technique. The pivotal Rezūm study found a retreatment rate of 4.4% at 5 yr but did not specifically explore factors related to retreatment. In our study we report early real-world outcomes with Rezūm and an analysis of patients who required surgical retreatment.
2. Patients and methods
We performed the first Rezūm procedure in March 2017 and prospectively collected data for consecutive patients. Rezūm procedures undertaken between March 2017 and January 2020 were included in this analysis.
Patients were diagnosed with symptomatic BPH on the basis of their symptoms, validated questionnaires, uroflowmetry, and additional tests when indicated.
All procedures were performed by four consultant urologists and five supervised trainees at two neighbouring hospital sites. Treatments were delivered either under local anaesthetic with sedation or under general anaesthetic as day cases. Patients had their prostate measured via transrectal ultrasound at the start of the procedure. The technology, device, and procedure details have previously been described [3], [4]. In brief, the sites for injection are determined at cystoscopy. The total number of vapour treatments in each prostate lobe is determined according to the length of the prostatic urethra and the need to treat the median lobe. At the end of the procedure, patients were fitted with a urethral catheter that was generally removed at 3–10 d postoperatively.
Patients were typically reviewed at 6 wk and 3, 6, and 12 mo after Rezūm treatment. After 12 mo, patients had further reviews if they had ongoing urinary symptoms or were being seen in the department for an alternative problem. Data were collected for patient demographics, prostate volume, urinary flowmetry, patient-reported outcome measures (IPSS, Quality of Life [QoL] score, and International Index of Erectile Function [IIEF-5]), and need for and type of retreatment. Statistical analysis was performed using unpaired t tests, paired t tests, and Fisher’s exact test.
3. Results
Between March 2017 and January 2020, 495 patients were treated with Rezūm. Thirty-four patients (6.9%) did not attend any follow-up and were excluded, leaving 461 patients for analysis. The mean (±standard deviation) follow-up duration was 16.7 ± 10.4 mo. Procedures were performed under local anaesthetic with sedation (41.9%) or under general anaesthetic (58.1%) as day cases.
The mean patient age was 67.5 ± 7.8 yr. The mean prostate volume was 56.5 ± 24.0 ml. Eighty-three patients (18.0%) had a prostate volume ≥80 ml. Preoperatively, 32 patients (6.9%) were using intermittent catheterisation or had an indwelling catheter. Table 1 compares baseline demographics between the group that required reintervention and the group that did not; there were no significant differences in preoperative parameters between the groups.
Table 1.
Comparison of baseline patient characteristics between the groups that did and did not require reinterventiona
| Parameter | No reintervention | Reintervention | p value |
|---|---|---|---|
| (n = 440) | (n = 21) | ||
| Age (yr) | 67.6 ± 7.9 | 67.1 ± 6.4 | 0.814 |
| Prostate volume (ml) | 57.5 ± 24.4 | 53.7 ± 22.6 | 0.504 |
| Baseline maximum flow rate (ml/s) | 9.8 ± 4.3 | 8.9 ± 3.4 | 0.472 |
| Baseline postvoid residual volume (ml) | 169.4 ± 141.7 | 232.5 ± 182.6 | 0.122 |
| Baseline International Prostate Symptom Score | 20.8 ± 6.7 | 22.5 ± 5.4 | 0.296 |
| Baseline quality-of-life score | 4.5 ± 0.9 | 4.4 ± 0.9 | 0.772 |
Data are presented as the mean ± standard deviation. There were no significant differences in preoperative parameters between the groups.
There was a significant improvement in mean Qmax from baseline (9.7 ml/s) to 3 mo (15.7 ml/s) that was maintained at 12-mo follow-up (18.0 ml/s; p < 0.0001; Fig. 1). There was also a significant reduction in mean postvoid residual volume from 172.1 ml preoperatively to 91.8 ml at 3 mo and 96.7 ml at 12 mo (p < 0.0001).
Fig. 1.

Baseline and postoperative data for the maximum urinary flow rate (Qmax).
There were significant reductions in mean IPSS and QoL scores from baseline (20.9 and 4.5, respectively) that were maintained at 12-mo follow-up (4.8 and 1.2, respectively; p < 0.0001; Fig. 2, Fig. 3).
Fig. 2.
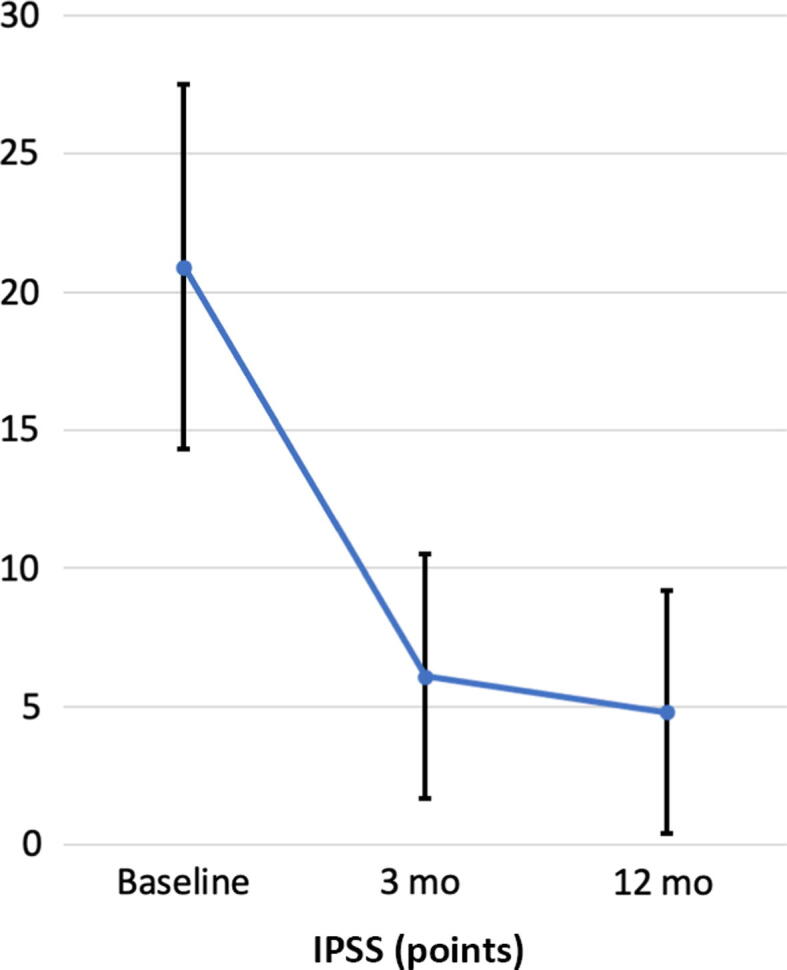
Baseline and postoperative results for the International Prostate Symptom Score (IPSS) scale.
Fig. 3.
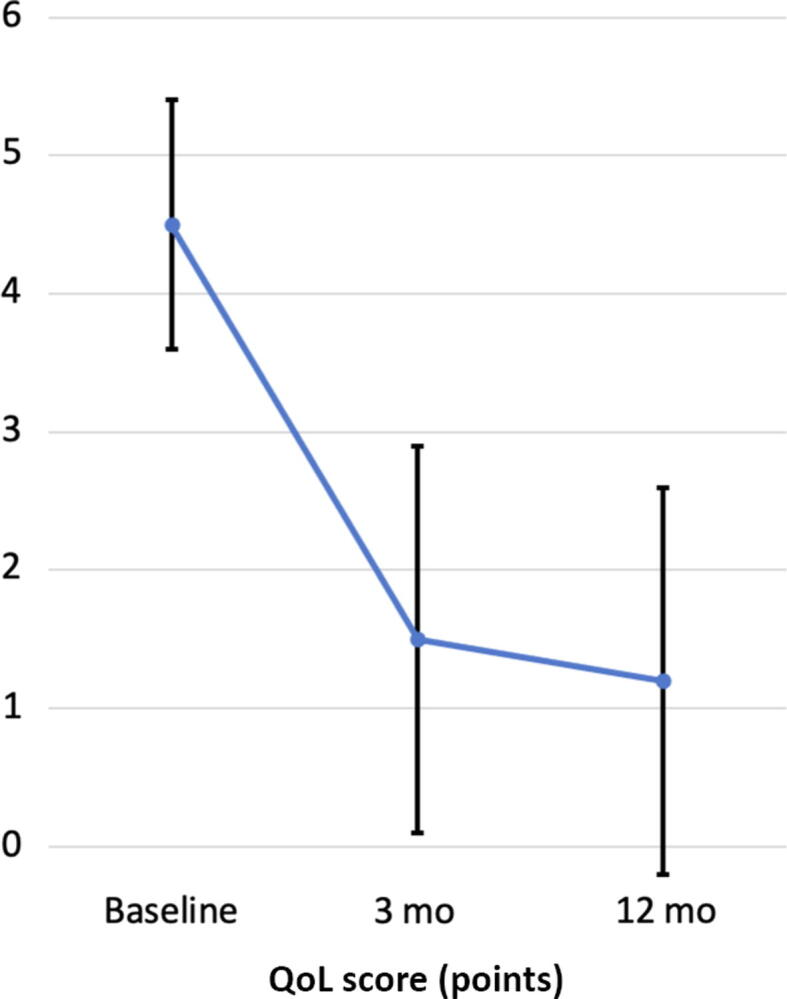
Baseline and postoperative quality of life (QoL) scores.
Of the 32 patients who were performing intermittent catheterisation or had an indwelling catheter, 25 were catheter-free after Rezūm and seven continued with intermittent catheterisation or an indwelling catheter. One of the latter patients went on to undergo TURP as further treatment and was able to discontinue intermittent catheterisation thereafter.
A total of 99 patients (21.5%) completed the IIEF-5 questionnaire before and after Rezūm treatment, which revealed a significant improvement in score from a mean of 16.5 ± 8.4 at baseline to 18 ± 8.1 (p = 0.0222).
During the follow-up period, 21 patients (4.6%) required further surgery for symptomatic BPH, of whom 11 (2.4%) underwent retreatment within the first year (Table 2). The mean initial prostate volume for those requiring retreatment was 53.6 ± 22.0 ml. Among the 33 patients with an initial gland size of ≥80 ml, three (3.6%) required retreatment, only one (1.2%) of which was in the first year of follow-up. This compares to the retreatment rate of 4.8% for patients with a prostate of <80 ml (2.7% in the first year). There was no significant difference in the retreatment rate at one year between small and large prostates (p = 0.70). In addition, there was no significant difference in the number of treatments per ml of prostate between those requiring retreatment and those who did not (0.15 ± 0.06 vs 0.14 ± 0.05; p = 0.54).
Table 2.
Retreatments performed according to time since the initial Rezūm treatment
| Retreatment | Patients (n) |
||
|---|---|---|---|
| Year 1 | Year 2 | Year 3 | |
| Bladder neck incision | 4 | 4 | 0 |
| Transurethral resection/incision of the prostate | 4 | 2 | 0 |
| Greenlight photoselective vaporisation of the prostate | 2 | 0 | 2 |
| Rezūm | 1 | 2 | 0 |
The types of retreatment performed included eight bladder neck incisions (BNIs) or resections, six TURP or transurethral incision of the prostate procedures, four Greenlight laser photoselective vaporisation of the prostate, and three Rezūm retreatments. The median time to a further operation was 11.5 mo (range 3–34). The most common findings at reoperation were an inadequately treated median lobe, an obstructing bladder neck, and in some cases gland asymmetry was noted at cystoscopy and cavities or recesses within the gland were also observed (Fig. 4).
Fig. 4.
Findings at reoperation following Rezūm treatment. (A) An inadequately treated median lobe with no significant residual lateral lobe tissue. (B) A cavity in the right lateral lobe with a high bladder neck. (C) Asymmetry in the prostate cavity. (D) An obstructed bladder neck requiring bladder neck incision. (E) A cavity just beyond the verumontanum in the left lateral lobe. (F) A cavity close to the bladder neck in the right lateral lobe.
4. Discussion
Rezūm is an effective treatment option for men with LUTS secondary to BPH. Comparable to results from other studies evaluating outcomes of Rezūm, we demonstrated a significant improvement in uroflowmetry and patient-reported outcomes, with preservation of sexual function [2], [3], [5], [6], [7]. In our series there appeared to be an improvement in sexual function following Rezūm which is probably a direct result of improvement in LUTS, although this finding must be considered with caution given the low IIEF-5 completion rate preoperatively and postoperatively. Our results further demonstrate the durability of Rezūm, with a 2.4% retreatment rate at 12 mo and an overall rate of 4.6% at median follow-up of 16.7 mo. We found that some patients requiring retreatment had persistent troublesome LUTS after their first procedure, while others had an initial improvement and then a deterioration in symptoms, often 4–6 mo postoperatively.
The pivotal Rezūm study recently reported outcomes up to 5 yr, with an overall surgical retreatment rate of 4.4%. Interestingly, the majority of the retreatments occurred within the first 2 yr, and none required retreatment in years 4 and 5 of follow up [2]. In our study the retreatment rate of 4.6% up to median follow-up of 16.5 mo is slightly higher than in the pivotal study. However, we anticipate that this would remain fairly static with further time to 5 yr, as we also found that retreatment tends to be required early (within the first 2 yr) in the follow-up period. Clearly, further reporting of later retreatment rates is required to understand the long-term durability of Rezūm. Furthermore, the average gland volume was larger in our series and the exclusion criteria were less rigid, as this was a real-world prospective series rather than a randomised trial (the pivotal Rezūm study included patients aged >50 yr with IPSS ≥13, Qmax ≤15 ml/s, and prostate volume of 30–80 ml [2]). We also included catheterised patients in our analysis. However, as only one of these 32 patients required retreatment, we do not believe that has negatively impacted our retreatment rates. Furthermore, 25 of these 32 patients are now catheter-free. These encouraging early outcomes for the subgroup of patients with retention of urine should serve as a stimulus for a more comprehensive evaluation of this patient population.
The evidence so far suggests that the retreatment rate after Rezūm compares favourably to those after alternative MISTs. The 5-yr surgical retreatment rate of 4.4% after Rezūm is lower than the 13.6% after Urolift [8]. A randomised controlled trial comparing prostatic artery embolisation (PAE) and TURP found that 21% of patients undergoing PAE required surgical retreatment within the first 2 yr after their procedure [9]. iTIND is the newest MIST, with outcomes now reported to 2 yr, with a retreatment rate of 6.5% [10]. This improvement in retreatment over other MISTs is probably because Rezūm is capable of ablating median-lobe as well as lateral-lobe tissue and may possibly involve its volume-reducing effects as well.
The most common findings we identified in patients requiring retreatment were an inadequately treated median lobe, an obstructing bladder neck, and in some cases gland asymmetry (one lateral lobe more prominent than the other) or cavities or recesses within the gland (Fig. 4). This is a similar finding to results from the pivotal study, in which four of the six patients requiring surgical retreatment had an undertreated median lobe [11]. In our series, eight patients requiring retreatment underwent BNI to treat a high bladder neck causing outflow obstruction. Those requiring BNI did tend to have a smaller initial gland size (mean 45 ml). This observation has prompted us to offer Rezūm in combination with BNI for a small select group of patients with a high bladder neck and smaller gland size. This strategy will eliminate the need for early retreatment in a number of patients and should further improve the retreatment rate. A discussion with the patient before the procedure is helpful in highlighting the higher likelihood of dry ejaculation after simultaneous BNI. The early retreatments in the first year were generally related to inadequate tissue removal and were usually “resolved” via a modest second procedure to resect residual obstructing tissue or to open up cavities present within the prostate that had developed after ablation. In some cases cavities occur because of the vapour effect on the central zone. This can result in subtrigonal tissue ablation where there is not a sufficient depth of tissue underneath. A steep prostatic urethral angle may be indicative of a large median lobe and allow for safe needle placement in the median lobe. The number of patients requiring retreatment in this series was insufficient to allow evaluation of whether the presence of a median lobe was associated with a higher likelihood of a requirement for retreatment.
Rezūm is still relatively novel and the EAU guidelines state that it remains a technique under investigation and do not recommend under which circumstances it is most suitable [12]. However, with results from the pivotal study and increasing evidence demonstrating both its efficacy and durability, the technique has now been approved by the UK National Institute of Clinical Excellence (NICE). The NICE guidelines suggest that Rezūm can be considered for patients with moderate to severe LUTS (IPSS ≥13) and a moderately enlarged prostate (between 30 and 80 ml) [13]. There is still a lack of evidence on the use of Rezūm for large prostates (≥80 ml), with two recent studies reporting outcomes [14], [15]. Bole et al [14] found no significant difference in early outcomes between patients with small and large prostates but were unable to comment on retreatment given that the outcomes reported were only up to 3 mo. Garden et al [15] found a significantly higher retreatment rate of 8.33% for large prostates (≥80 ml) compared to 4.76% for small prostates at 1 yr. In our study we found no significant difference in the retreatment rate at 1 year between small and large prostates and a lower retreatment rate at 1 yr of 1.2% compared to the 8.33% reported by Garden et al. However, we had a larger number of patients with prostates of ≥80 ml (83 vs 36 ml) which may partly explain the differences, and further studies are required to evaluate Rezūm in patients with large prostates.
The strengths of our study lie in its prospective data collection and the large number of cases. To the best of our knowledge, this is the first study on Rezūm to further explore possible factors that may influence the need for retreatment. The main limitation of our study is that 6.9% of patients did not attend any follow-up visits. As we are a tertiary referral centre for Rezūm, it is possible that some of these patients had retreatment at their local hospital. Unfortunately, only 21.5% of patients completed IIEF-5 questionnaires preoperatively and postoperatively. In these patients there was an improvement in IIEF-5 score and the pivotal Rezūm study has already demonstrated that the procedure preserves sexual function. However, we acknowledge that this has not been fully evaluated in our study. In addition, the mean follow-up of 16.7 mo means that we are unable to comment on the longer-term durability of Rezūm treatment.
5. Conclusions
Rezūm is an effective volume-reducing surgical treatment option for BOO and allows maintenance of sexual function for the majority of patients. This study demonstrated that the beneficial effects of Rezūm observed in the pivotal Rezūm II study are transferable to a real-world population. This approach offers a competitive retreatment rate in comparison to other MISTs and does not appear to have a higher retreatment rate for larger prostates. The retreatment rate could be further improved by ensuring adequate treatment of the median lobe and recognising when simultaneous BNI could be considered. Further studies are required to assess these issues in greater detail and to determine whether certain gland characteristics may predict a less favourable outcome. It is possible that refinements with regard to the optimal placement of water vapour injections and the delivery device itself may lead to better outcomes and in doing so further reduce the retreatment rate.
Author contributions: Danielle Whiting had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Emara, Hindley.
Acquisition of data: Whiting, Noureldin, Abdelmotagly, Johnston, Rajkumar, Emara, Hindley.
Analysis and interpretation of data: Whiting.
Drafting of the manuscript: Whiting.
Critical revision of the manuscript for important intellectual content: Whiting, Noureldin, Abdelmotagly, Johnston, Brittain, Rajkumar, Emara, Hindley.
Statistical analysis: Whiting.
Obtaining funding: None.
Administrative, technical, or material support: None.
Supervision: Emara, Hindley.
Other: None.
Financial disclosures: Danielle Whiting certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: Amr Emara is a proctor for Boston Scientific. Richard Hindley is a proctor/medical advisor for Boston Scientific. The remaining authors have nothing to disclose.
Funding/Support and role of the sponsor: None.
Associate Editor: Véronique Phé
References
- 1.Lee S.W.H., Chan E.M.C., Lai Y.K. The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a systematic review and meta-analysis. Sci Rep. 2017;7:7984. doi: 10.1038/s41598-017-06628-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McVary K.T., Gittelman M.C., Goldberg K.A., et al. Final 5-year outcomes of the multicenter randomized sham-controlled trial of Rezūm water vapor thermal therapy for treatment of moderate-to-severe lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2021;206:715–724. doi: 10.1097/JU.0000000000001778. [DOI] [PubMed] [Google Scholar]
- 3.Darson M.F., Alexander E.E., Schiffman Z.J., et al. Procedural techniques and multicenter postmarket experience using minimally invasive convective radiofrequency thermal therapy with Rezūm system for treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Res Rep Urol. 2017;9:159–168. doi: 10.2147/RRU.S143679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McVary K.T., Gange S.N., Gittelman M.C., et al. Minimally invasive prostate convective water vapour energy ablation: a multicenter, randomized, controlled study for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2016;195:1529–1538. doi: 10.1016/j.juro.2015.10.181. [DOI] [PubMed] [Google Scholar]
- 5.Dixon C.M., Cedano E.R., Pacik D., et al. Two-year results after convective radiofrequency water vapor thermal therapy of symptomatic benign prostatic hyperplasia. Res Rep Urol. 2016;8:207–216. doi: 10.2147/RRU.S119596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mollengarden D., Goldberg K., Wong D., Roehrborn C. Convective radiofrequency water vapor thermal therapy for benign prostatic hyperplasia: a single office experience. Prostate Cancer Prostat Dis. 2018;21:379–385. doi: 10.1038/s41391-017-0022-9. [DOI] [PubMed] [Google Scholar]
- 7.Alegorides C., Fourmarier M., Eghazarian C., Lebdai S., Chevrot A., Droupy S. Treatment of benign prostate hyperplasia using the Rezum® water vapor therapy system: results at one year. Prog Urol. 2020;30:624–631. doi: 10.1016/j.purol.2020.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Roehrborn C.G., Barkin J., Gange S.N., et al. Five year results of the prospective randomised controlled prostatic urethral L.I.F.T. study. Can J Urol. 2017;24:8802–8813. [PubMed] [Google Scholar]
- 9.Abt D., Müllhaupt G., Hechelhammer L., et al. Prostatic artery embolisation versus transurethral resection of the prostate for benign prostatic hyperplasia: 2-yr outcomes of a randomised, open-label, single-centre trial. Eur Urol. 2021;80:34–42. doi: 10.1016/j.eururo.2021.02.008. [DOI] [PubMed] [Google Scholar]
- 10.Kadner G., Valerio M., Giannakis I., et al. Second generation of temporary implantable nitinol device (iTIND) in men with LUTS: 2 year results of the MT-02-study. World J Urol. 2020;38:3235–3244. doi: 10.1007/s00345-020-03140-z. [DOI] [PubMed] [Google Scholar]
- 11.McVary K.T., Roehrborn C.G. Three-year outcomes of the prospective, randomized controlled Rezūm system study: convective radiofrequency thermal therapy for treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Urology. 2018;111:1–9. doi: 10.1016/j.urology.2017.10.023. [DOI] [PubMed] [Google Scholar]
- 12.Gravas S., Cornu J.N., Gacci M., et al. European Association of Urology; Arnhem (The Netherlands): 2021. Male lower urinary tract symptoms (LUTS), incl. benign prostatic obstruction (BPO)https://uroweb.org/wp-content/uploads/EAU-Guidelines-on-Management-of-Non-Neurogenic-Male-LUTS-2021.pdf [Google Scholar]
- 13.National Institute of Health and Care Excellence . NICE; London (UK): 2020. Rezūm for treating lower urinary tract symptoms secondary to benign prostatic hyperplasia. Medical technologies guidance MTG49.www.nice.org.uk/guidance/mtg49/resources/rezum-for-treating-lower-urinary-tract-symptoms-secondary-to-benign-prostatic-hyperplasia-pdf-64372064176069 [Google Scholar]
- 14.Bole R., Gopalakrishna A., Kuang R., et al. Comparative postoperative outcomes of Rezūm prostate ablation in patients with large versus small glands. J Endourol. 2020;34:778–781. doi: 10.1089/end.2020.0177. [DOI] [PubMed] [Google Scholar]
- 15.Garden E.B., Shukla D., Ravivarapi, et al. Rezum therapy for patients with large prostates (≥80 g): initial clinical experience and postoperative outcomes. World J Urol. 2021;39:3041–3048. doi: 10.1007/s00345-020-03548-7. [DOI] [PMC free article] [PubMed] [Google Scholar]



