Abstract
Background
The primary objective of this study is to assess the risk of thromboembolic events (TEs) in hospitalized patients with coronavirus disease 2019 (COVID-19) and study the impact of TEs on hospital course and mortality risk during the initial height of the severe acute respiratory syndrome coronavirus-2 pandemic.
Methods
A retrospective review of all adult inpatients (≥ 18 years old) with COVID-19 infection at a single academic institution from March 15, 2020 to July 1, 2020 was performed. Collected data included patient demographics, comorbidities, hospital admission type, TEs, laboratory values, use of anticoagulants/antiplatelet agents, hospital length of stay, and in-hospital mortality. A logistic regression was used to estimate associations between risk factors and TEs.
Results
A total of 826 inpatients with COVID-19 were identified. Of these, 56% were male, average age was 60.9 years, and race/ethnicity was reported as Hispanic in 51%, non-Hispanic Black in 25%, and non-Hispanic White in 18%. A total of 98 TEs were documented in 87 patients (10.5%). Hypertension, coronary artery disease, and chronic limb threatening ischemia were associated with an increased incidence of thromboembolism (P < 0.05). Hispanic patients had higher incidence of thromboembolism compared to White non-Hispanic patients (odds ratio {[OR] confidence interval [CI]}: 2.237 [1.053, 4.754], P = 0.036). As D-dimer increased, the odds of TE increased by 5.2% (OR [CI]: 1.052 [1.027, 1.077], P < 0.001). Patients with TEs had longer hospital stay (median 13 vs. 6 days, P < 0.001), higher likelihood of intensive care unit admission (63% vs. 33%, P < 0.001), and higher in-hospital mortality (28% vs. 16%, P = 0.006). Arterial TEs were associated with higher in-hospital mortality than venous TEs (37% vs. 15%, P = 0.027).
Conclusions
During the initial height of the severe acute respiratory syndrome coronavirus-2 pandemic, TEs were relatively frequent in hospitalized patients with COVID-19. Racial disparities were seen with an increased proportion of minority patients admitted with respect to percentages seen in the general population. There was also a significantly increased incidence of TEs in Hispanic patients. TEs were associated with significantly longer hospital stay and higher in-hospital mortality. Patients with arterial TEs fared worse with significantly higher mortality than those with venous events. Inconsistencies in anticoagulation management early in the pandemic may have contributed to poor outcomes and more contemporary management outcomes need to be investigated.
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). It was declared a global pandemic on March 11, 2020 by the World Health Organization. Two days later, the United States declared a national state of emergency concerning the COVID-19 outbreak. COVID-19 infection may be asymptomatic or may have a presentation ranging from mild upper respiratory symptoms to respiratory failure, requiring hospitalization and mechanical ventilation, to death. In addition, patients with COVID-19 infection often develop a hypercoagulable state and are at a risk of development of associated thromboembolic events (TE).1
Common symptoms of COVID-19 include fever, sore throat, fatigue, cough, myalgia, headache, diarrhea, multiple studies that have also reported cases of endothelial dysfunction, cardiac injury, myocardial infarction (MI), cerebrovascular attack (CVA), pulmonary embolism (PE), venous thromboembolism (VTE), disseminated intravascular coagulation (DIC), acute limb ischemia (ALI), renal artery thrombosis leading to renal failure, and other TEs.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11 A study of 184 patients with COVID-19 pneumonia in Wuhan, China found that 14% had PE.12 Another study of 81 patients with COVID-19 found that 25% had VTE.13 A single-center study from the Netherlands demonstrated that 31% of 184 critically ill COVID-19 patients had VTE.1 Moreover, extensive literature has described a prothrombotic state in COVID-19 patients with elevated D-dimer, fibrinogen, fibrin, and fibrin degradation products. When observed, the increased values seem to be associated with worse health outcomes and increased the risk of coagulopathy in patients with COVID-19 infection.1 , 4, 5, 6 , 8
Given the paucity of early publication documenting outcomes in hospitalized patients in the United States with COVID-19 and associated TEs, the purpose of this study is to review our own single-institution experience with hospitalized COVID-19 patients with attention to differences in clinical course based on race/ethnicity. Our objective is to investigate incidence of TEs, identify risk factors for their development, and evaluate their impact on hospital course including mortality. Moreover, we hypothesized that laboratory values pertaining to coagulation including D-dimer could help identify patients at an elevated risk of TEs.
Materials And Methods
Study Design
This is a retrospective single academic institution cohort study. An institutional review board approval was obtained prior to data collection. The study sample was extracted from the electronic medical record database and included all patients aged more than 18 years who were admitted to Loyola University Medical Center from March 15, 2020 to July 1, 2020 with hospital laboratory-confirmed COVID-19 positivity. A review of the electronic medical record was performed to gather detailed data on patient demographics and clinical details.
Study Variables
Data collected included patient demographics (age, gender, race, and ethnicity), pre-existing comorbidities, smoking status, hospital admission type, diagnosis of any TEs during hospitalization, admission laboratory values, use of anticoagulants or antiplatelet agents, hospital length of stay (LOS), intensive care unit (ICU) admission rate, and in-hospital mortality. The primary outcome of interest was the diagnosis of venous TE, such as PE and deep vein thrombosis (DVT), and arterial TEs, including MI, ischemic CVA, and extremity, renal, mesenteric, splenic, carotid, and aortic thromboembolism. DIC was also included as a TE. Secondary outcomes investigated included the impact of TE on LOS, ICU admission, and in-hospital mortality.
Data Analyses
Means (standard deviation [SD]) were used to summarize normally distributed continuous variables and medians (Q1, Q3) were used to summarize non-normally distributed continuous variables; counts and frequencies were used to summarize categorical factors. Odds ratios (OR), confidence intervals (CI), and P values for associations with a TE were estimated using complete-case univariable logistic regression models. Predictors with association of P < 0.10 at the univariable level were used in multivariable regression models to estimate adjusted associations. If a variable had significant missing data (>10%), an indicator for missing data was included in the multivariable model. Standard diagnostics (variance inflation factors, linearity of continuous predictors, and Akaike information criterion) were used to assess model fit for the final multivariable model. If a continuous predictor was not linearly associated with the outcome, an ‘abnormal threshold’ was used to dichotomize the variable. If a variable had little variability, and model estimates were unstable, it was not included in the final multivariable model. In addition, TEs were correlated with outcomes of LOS, ICU admission, and mortality. Wilcoxon test was used to compare LOS between groups and Chi-squared test was used to compare ICU admission and mortality proportions between groups. Two-sided P values < 0.05 were considered statistically significant. All analyses were performed using SAS 9.4 (Cary, North Carolina).
Results
A total of 826 hospitalized COVID-19 positive patients were identified and included in the analysis. The mean (SD) age at diagnosis was 60.9 (16.7) years and 56% of patients were male with 44% female. With respect to race and ethnicity, 51% were Hispanic, 25% were non-Hispanic Black, and 18% were non-Hispanic White. The most prevalent comorbidity was hypertension (65%) followed by DM (44%), hyperlipidemia (HLD) (41%), and CAD (19%). Hospitalized patients with COVID-19 infection had a median (interquartile range [IQR]) admission D-dimer level of 948 (1,521) ng/mL, median BUN level of 16 (17) mg/dL, and median creatinine level of 1 (0.7) unit mg/dL at admission. (Table I ). TEs were diagnosed in a total of 87 patients (11%). Seventy six patients had 1 TE diagnosed, whereas 11 patients were diagnosed with 2 TEs for a total of 98 events noted during the study period (Table II ).
Table I.
Summary of predictors by outcome
| Variables | All, n = 826 n (%) | No thrombotic events, n = 739 n (%) | Any thrombotic event, n = 87 n (%) |
|---|---|---|---|
| Demographics | |||
| Age, mean (SD) | 60.9 (16.7) | 60.5 (16.8) | 64.1 (15.3) |
| Male | 459 (56) | 403 (55) | 56 (64) |
| Race/Ethnicity | |||
| White non-Hispanic | 151 (18) | 140 (19) | 11 (13) |
| Black non-Hispanic | 207 (25) | 177 (24) | 30 (34) |
| Hispanic | 422 (51) | 379 (51) | 43 (49) |
| Other/not specified | 46 (6) | 43 (6) | 3 (3) |
| Comorbidities prior to COVID-19 admission | |||
| Previous or current smoker | 178 (36) | 154 (36) | 24 (39) |
| Diabetes mellitus | 351 (44) | 309 (43) | 42 (49) |
| CKD | 117 (15) | 101 (14) | 16 (19) |
| End-stage renal disease | 73 (9) | 62 (9) | 11 (13) |
| Hypertension | 527 (65) | 461 (64) | 66 (76) |
| Hyperlipidemia | 332 (41) | 293 (41) | 39 (46) |
| Coronary artery disease | 152 (19) | 128 (18) | 24 (28) |
| Myocardial infarction | 60 (7) | 49 (7) | 11 (13) |
| Congestive heart failure | 107 (13) | 96 (13) | 11 (13) |
| Peripheral artery disease | 38 (5) | 32 (4) | 6 (7) |
| Chronic limb-threatening ischemia | 12 (1) | 8 (1) | 4 (5) |
| Chronic obstructive pulmonary disease | 56 (7) | 46 (6) | 10 (11) |
| Respiratory failure | 33 (4) | 28 (4) | 5 (6) |
| Previous PE | 24 (3) | 21 (3) | 3 (3) |
| Previous DVT | 46 (6) | 37 (5) | 9 (10) |
| Ischemic stroke | 78 (10) | 67 (9) | 11 (13) |
| Hemorrhagic stroke | 12 (1) | 12 (2) | 0 (0) |
| In-hospital medication and admission laboratory values | |||
| Any antiplatelet | 246 (30) | 204 (28) | 42 (48) |
| Any anticoagulation | 748 (93) | 662 (92) | 86 (99) |
| Creatinine, median (Q1, Q3) | 1 (0.8, 1.5) | 1 (0.8, 1.4) | 1.3 (0.9, 1.8) |
| D-Dimer, median (Q1, Q3) | 948 (477, 1,998) | 856.5 (466, 1,627) | 1,842 (1,005, 7,429) |
| BUN, median (Q1, Q3) | 16 (11, 28) | 15 (11, 27) | 20 (13, 31) |
| Outcomes | |||
| Length of stay, median (Q1, Q3) | 6 (3, 12) | 6 (3, 11) | 13 (5, 30) |
| ICU Admission | 300 (37) | 245 (33) | 55 (63) |
| Death | 140 (17) | 116 (16) | 24 (28) |
Demographics, comorbidities, length-of-stay, and in-hospital mortality in the presence and absence of thromboembolic events (Missing: Gender 3, Smoking 255, DM 23, CKD 20, REN F 27, HTN 17, HLD 22, CAD 19, MI 22, HF 18, PAD 17, CLI 19, COPD 17, RESP F 18, PE 17, DVT 17, I STROKE 17, H STROKE 17, Creatinine 13, D-DIMER 435, BUN 13, LOS 225, ICU Admit 7, Death 10).
Table II.
Types of thromboembolic events noted during hospitalization
| Thromboembolic event | n = 98 (%) |
|---|---|
| Venous thromboembolism | |
| DVT (Extremity) | 15 (15) |
| DVT (Nonextremity) | 6 (6) |
| Pulmonary embolism | 26 (27) |
| Arterial thromboembolism | |
| Aortic | 1 (1) |
| Splenic artery | 1 (1) |
| Renal artery | 1 (1) |
| Superior mesenteric artery | 2 (2) |
| Extremity artery | 2 (2) |
| Ischemic stroke | 13 (13) |
| Myocardial infarction | 27 (28) |
| Disseminated intravascular coagulopathy | 4 (4) |
In univariate analyses, non-Hispanic Black patients and those with a history of HTN, CAD, and chronic limb threatening ischemia (CLTI) had significant increased odds of developing TE (P < 0.05) during their hospital stay. Use of any in hospital anticoagulant or antiplatelet agent was univariably associated with a higher likelihood of TE. Given limited information on dosing, timing, and indication of anticoagulant and antiplatelet medication usage, we were unable to establish a true association between medication use and TEs. Elevated admission laboratory values for creatinine, D-dimer, and BUN were associated with increased odds of TE (P < 0.05). Smoking status and comorbidities such as DM and hyperlipidemia had no association with development of a TE (P > 0.31) (Table III ).
Table III.
Univariable and multivariable logistic regression results
| Variables | Univariable OR (CI) | P valuea | Multivariable OR (CI), n = 786 | P valueb |
|---|---|---|---|---|
| Age | 1.013 (1.00, 1.028) | 0.056 | 1.006 (0.988, 1.024) | 0.554 |
| Male | 1.492 (0.94, 2.369) | 0.090 | 1.333 (0.807, 2.201) | 0.262 |
| Race/Ethnicity | ||||
| BNH versus WNH | 2.16 (1.04, 4.46) | 0.038 | 1.940 (0.886, 4.248) | 0.097 |
| Hispanic versus WNH | 1.44 (0.72, 2.88) | 0.298 | 2.237 (1.053, 4.754) | 0.036 |
| Other versus WNH | 0.89 (0.24, 3.33) | 0.860 | 1.141 (0.293, 4.438) | 0.849 |
| Previous or current smoker | 1.154 (0.666, 2.001) | 0.610 | ||
| Diabetes | 1.26 (0.805, 1.973) | 0.311 | ||
| CKD | 1.401 (0.783, 2.509) | 0.256 | ||
| End-stage renal disease | 1.563 (0.788, 3.101) | 0.201 | ||
| Hypertension | 1.779 (1.064, 2.975) | 0.028 | 1.15 (0.609, 2.171) | 0.700 |
| Hyperlipidemia | 1.233 (0.785, 1.937) | 0.364 | ||
| Coronary artery disease | 1.762 (1.061, 2.927) | 0.029 | 0.963 (0.488, 1.900) | 0.917 |
| Myocardial infraction | 1.973 (0.984, 3.956) | 0.056 | 1.636 (0.698, 3.834) | 0.239 |
| Congestive heart failure | 0.956 (0.49, 1.866) | 0.896 | ||
| Peripheral artery disease | 1.597 (0.648, 3.936) | 0.309 | ||
| Chronic limb-threatening Ischemia | 4.289 (1.264, 14.551) | 0.020 | 2.757 (0.662, 11.48) | 0.181 |
| COPD | 1.909 (0.926, 3.934) | 0.080 | 1.401 (0.598, 3.285) | 0.487 |
| Respiratory failure | 1.509 (0.567, 4.016) | 0.410 | ||
| Previous PE | 1.192 (0.348, 4.082) | 0.780 | ||
| Previous DVT | 2.136 (0.994, 4.592) | 0.052 | 1.087 (0.426, 2.773) | 0.814 |
| Ischemic stroke | 1.415 (0.717, 2.794) | 0.317 | ||
| Any antiplatelet | 2.375 (1.513, 3.726) | <0.001 | 1.775 (1.022, 3.084) | 0.041 |
| Any anticoagulationc | 7.525 (1.03, 54.952) | 0.047 | ||
| Elevated creatinined | 1.972 (1.24, 3.14) | 0.004 | 1.455 (0.721, 2.936) | 0.354 |
| D-DIMER, per 500-unit increase | 1.055 (1.031, 1.079) | <0.0001 | 1.052 (1.027, 1.077) | <0.001 |
| BUN, per 5-unit increase | 1.053 (1.006, 1.102) | 0.028 | 0.981 (0.91, 1.058) | 0.615 |
P values < 0.10 are highlighted. BNH, Black Non-Hispanic; WNH, White Non-Hispanic.
P value calculated with a complete-case simple logistics regression model.
P value calculated in complete-case multivariable logistics regression model with all variables presented in the previous column as predictors. This model also included a missing data indicator for D-Dimer, results not presented. Pairwise comparisons between race groups not presented are not statistically significant (P > 0.05).
Any anticoagulation use was not included in the final multivariable model, despite being significant at the P < 0.10 due to a lack of variability.
Creatinine was not linearly associated with the outcome. Therefore, was dichotomized at value 1.4 to indicate ‘Elevated Creatinine’.
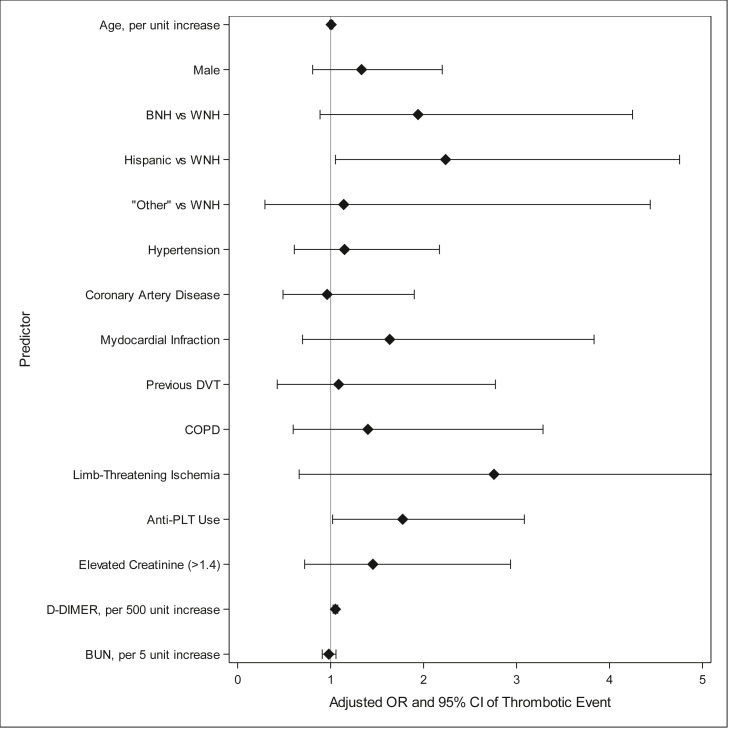
In multivariate analyses, Hispanic patients had statistically significant increased odds of TE by 2.2 times in comparison to non-Hispanic White patients (OR [CI]: 2.237 [1.053, 4.754], P = 0.036). Moreover, as admission D-dimer level increased (per 500-unit increments), the odds of developing a TE increased significantly by 5.2% (OR [CI]: 1.052 [1.027, 1.077], P < 0.001). Finally, use of any in-hospital or at-home antiplatelet agents increased odds of developing TE during hospitalization by 1.8 times in comparison to patients who did not use antiplatelet agents (OR [CI]: 1.775 [1.022, 3.084], P = 0.041) (Table III). An adjusted OR (CI) from the multivariable model is illustrated in Figure 1 .
Fig. 1.
Adjusted OR and 95% CI of thrombotic event. BNH, Black non-Hispanic; WNH, White non-Hispanic.
Patients with a TE diagnosis had higher anticoagulant/antiplatelet agent usage (P < 0.05) during hospitalization, longer hospital LOS (median: 13 vs. 6 days, P < 0.001), higher rates of ICU admission (63% vs. 33%, P < 0.001), and higher rates of in-hospital mortality (28% vs. 16%, P = 0.006) (Table III). Patients with arterial TE had a significantly higher in-hospital mortality compared to those who had venous TE (37% vs. 15%, P = 0.027).
Discussion
While the COVID-19 pandemic has had several distinct phases, perspective as to current outcomes should take into consideration those during the initial height of the SARS-CoV-2 pandemic. During this time, the incidence and impact of hypercoagulability and algorithms for anticoagulation for TE prophylaxis and treatment were not well established. Moreover, as with myriad other healthcare outcomes, we found evidence of racial disparity in hospital admissions for COVID-19 and in incidence of TE and resultant morbidity and mortality. Hispanic ethnicity was an independent predictor of TE in hospitalized COVID-19 patients in our study. While comorbidities such as HTN, CAD, and CLTI were associated with an elevated risk of TE during hospitalization, our univariate analysis demonstrated that smoking status, DM, and hyperlipidemia were not. Patients who did experience TE had longer hospital stays, higher rates of ICU admission, and higher mortality, indicating that their illness was more severe.
Previous studies have found that patients with COVID-19 infection and predisposing conditions of endothelial dysfunction such as CAD, HLD, DM, and HTN have worse outcomes overall.13 , 14 Our study confirms this finding. However, we did not find an increased risk of TE in patients with DM and HLD. This may be due to the small sample size in our study. Our analysis cannot establish causation but did allow for an assessment of association of TE with comorbidities studied. History of MI prior to admission did not have a significant association with the development of TEs during hospital admission, which included MI.
There is a well-established link between smoking status and increased risk of TEs in the general population.15 , 16 Multiple meta-analyses have shown that patients with current or previous smoking history had increased severity of COVID-19 symptoms.17, 18, 19 However, smoking status had no association with TE in our study. Similar negative associations were noted in a study by Meena et al. which showed no significant association between smoking status and VTE in 114 patients with COVID-19.20This finding may suggest a different pathogenesis of thromboembolism in COVID-19 patients than in the general population. We suggest further evaluation of the relationship between smoking and risk of TE in COVID-19 patients in future studies.
The results of this study demonstrated that patients of Hispanic ethnicity with active COVID-19 infection requiring hospital admission had significantly increased odds of TE. This was also found to be the case in a study by Macias Gil et al. who investigated disparities in outcomes of Hispanic COVID-19 patients in Rhode Island. They found that hospitalized Hispanic patients aged more than 65 years with COVID-19 infection were more likely to have worse outcomes compared with non-Hispanic White patients.21 Of the patients included in our study, 51% identified as Hispanic. This represents a larger proportion of Hispanic patients than in the general population and in all other studies involving patients with vascular disease at our institution. We hypothesize that this is likely multifactorial and may be related to disparities in the population affected by COVID-19. Differences in access to care, socioeconomic status, language barriers, and possible distrust in healthcare systems may have resulted in delayed access, delayed diagnosis, and substandard management. Given the study period, the impact of vaccination status did not play a role but would be of significant interest in investigating TE incidence and outcomes at a late stage of the pandemic, particularly given the potential for race/ethnic differences in vaccination patterns. Additional studies are needed to elucidate the impact of race/ethnicity on outcomes associated with COVID-19 infection.22
Our study demonstrates that as the admission D-dimer level increased by 500-unit increments, the risk of developing a TE increased by 5.2%. The median D-dimer level in our patient population overall at the time of presentation was elevated. This is in concordance with previous studies documenting elevated D-dimer levels in patients with COVID-19 infection.1 , 4 , 6 , 8 In addition, multiple studies have demonstrated that COVID-19 patients with elevated D-dimer had worse hospital course, likely related to the fact that D-dimer is a marker for TEs. Our study found that patients diagnosed with a TE during their hospital stay had an increased LOS, rate of ICU admission, and mortality.1 , 7 , 10 , 11 , 23 A D-dimer threshold level on admission could help guide early management of these patients with prophylactic anticoagulation to decrease the incidence of TEs. Unfortunately, given our small sample size, our study was not powered to calculate a numerical threshold for TE prediction.
Our univariable model indicates a higher risk of TE in patients on antiplatelet and/or anticoagulant medications, with an antiplatelet agent use associated with a higher risk of TE in our multivariable analysis. Although this is not an independent predictor of TE, it may be an indicator of other comorbidities or of treatment of TE during the hospital admission. Therefore, this highlights the importance of our multivariable model as it takes into consideration for interaction between several covariates. Currently, our dataset is limited in the ability to identify prophylactic or therapeutic anticoagulation dosing and timing of medication administration with respect to the TE diagnosis. The period of interest in this study investigates only the first wave of the pandemic in 2020. Inconsistent protocols for antiplatelet agent and anticoagulant use early in the pandemic made these data unreliable and unable to be assessed. Moreover, current anticoagulation protocols for TE prophylaxis and treatment in patients with COVID-19 are under ongoing revision processes with little consensus. We specifically limited the study period to a phase of the pandemic in which all patients were unvaccinated. We believe the impact of this study relates to documentation of the natural history of this disease process with respect to TEs in patients who cannot or choose not to undergo vaccination.
In this study, COVID-19 patients with TE had significantly longer hospital stays, increased transfer to ICU care, and higher mortality. Other published reports have found similar results.23 , 24 In addition, patients with arterial TE had a significantly higher in-hospital mortality in comparison to those who had only venous TE as would be expected. Additional research in identifying the mechanisms of TE in COVID-19 patients is warranted.
There are several limitations in this study. First, it is a retrospective study intended to describe in-hospital events and outcomes. The study was not designed to include long-term follow-up. Second, we had a small sample size with relatively few TEs, which can lead to selection bias. Third, this study only evaluated outcomes in patients hospitalized with COVID-19 and thus sicker than their outpatient counterparts. It is likely that minimally symptomatic patients with venous TEs may have been managed as outpatients and thus this study would not have captured all TEs. This patient cohort likely carries more comorbidities inherently which could lead to an increased mortality risk. Therefore, we cannot draw conclusions on COVID-19 patients with TE who did not meet hospital admission criteria. In addition, only patients with a high clinical suspicion of TE underwent diagnostic testing in an effort to protect staff, such as vascular technologists, from COVID-19 exposure. Patients who were too ill to undergo diagnostic testing may have been treated empirically with therapeutic anticoagulation or treatment may have been deferred in patients who were not expected to survive and therefore they were not captured in this analysis. The incidence of TE diagnosis may have been higher, if more frequent diagnostic imaging was performed. Moreover, data from the initial stage of the SARS-CoV-2 pandemic may not be applicable in the current era where vaccination is available, anticoagulant use is more standardized, and variants of the virus have developed. As of January 2022, the National Institutes of Health recommends usage of therapeutic-dose of anticoagulation for hospitalized, non-ICU level patients who require low-flow oxygen, have an abnormal D-dimer level, and do not have an increased bleeding risk.25
Conclusion
In summary, patients admitted to the hospital with COVID-19 infection during the initial height of the SARS-CoV pandemic were more likely to develop a TE if they were of Hispanic ethnicity or had elevated D-dimer on admission. The presence of TEs portended worse outcomes, including longer length of hospital stay and in-hospital mortality. Utilization of comorbidity risk factors and laboratory values to identify patients early in their hospitalization at a risk of TE may lead to earlier institution of therapeutic anticoagulation, cardiovascular specialty consultation, and perhaps overall improved survival in this patient cohort. Additional studies are needed to account for changes in outcomes given the availability of vaccination, improved understanding of the course of the COVID-19 infection, and established but evolving protocols in treatment.
The diamond marker represents the adjusted OR of a TE in the presence of each categorical risk factor compared to none (or other reference group) or adjusted OR per relevant unit increase for each continuous variable. Accompanying lower and upper bars represent the 95% CI. If the lower bound extends past and includes 1, the risk factor was not significantly associated with an increased risk of TE.
Footnotes
Funding sources: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Bikdeli B., Madhavan M.V., Jimenez D., et al. COVID-19 and thrombotic or thromboembolic disease: implications for Prevention, Antithrombotic Therapy, and follow-up. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang X., Yu Y., Xu J., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhai P., Ding Y., Wu X., et al. The epidemiology, diagnosis and treatment of COVID-19. Int J Antimicrob Agents. 2020;55:105955. doi: 10.1016/j.ijantimicag.2020.105955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Connors J.M., Levy J.H. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135:2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang N., Bai H., Chen X., et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Violi F., Pastori D., Cangemi R., et al. Hypercoagulation and antithrombotic treatment in coronavirus 2019: a new challenge. Thromb Haemost. 2020;120:949–956. doi: 10.1055/s-0040-1710317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang D., Yin Y., Hu C., et al. Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS-CoV-2, discharged from two hospitals in Wuhan, China. Crit Care. 2020;24:188. doi: 10.1186/s13054-020-02895-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iba T., Levy J.H., Levi M., et al. Coagulopathy of Coronavirus disease 2019. Crit Care Med. 2020;48:1358–1364. doi: 10.1097/CCM.0000000000004458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bellosta R., Luzzani L., Natalini G., et al. Acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg. 2020;72:1864–1872. doi: 10.1016/j.jvs.2020.04.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mestres G., Puigmacià R., Blanco C., et al. Risk of peripheral arterial thrombosis in COVID-19. J Vasc Surg. 2020;72:756–757. doi: 10.1016/j.jvs.2020.04.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wright F.L., Vogler T.O., Moore E.E., et al. Fibrinolysis shutdown correlates to thromboembolic events in severe COVID-19 infection. J Am Coll Surg. 2020;231:193–203.e1. doi: 10.1016/j.jamcollsurg.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klok F.A., Kruip M., van der Meer N., et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Center for Health Statistics (US). Health, United States . National Center for Health Statistics (US); 2019; Hyattsville (MD): 2018. . Table 21, Selected Health Conditions and Risk Factors, by Age: United States, Selected Years 1988-1994 Through 2015-2016. [Google Scholar]
- 14.Villarroel M.A., Blackwell D.L., Jen A. National Health Interview Survey; 2018. Tables of Summary Health Statistics for U.S. Adults: 2018 National Health Interview Survey. National Center for Health Statistics. 2019.http://www.cdc.gov/nchs/nhis/SHS/tables.htm Available from. [Google Scholar]
- 15.Zhang G., Xu X., Su W., et al. Smoking and risk of venous thromboembolism: a systematic review. Southeast Asian J Trop Med Public Health. 2014;45:736–745. [PubMed] [Google Scholar]
- 16.Severinsen M.T., Kristensen S.R., Johnsen S.P., et al. Smoking and venous thromboembolism: a Danish follow-up study. J Thromb Haemost. 2009;7:1297–1303. doi: 10.1111/j.1538-7836.2009.03490.x. [DOI] [PubMed] [Google Scholar]
- 17.Reddy R.K., Charles W.N., Sklavounos A., et al. The effect of smoking on COVID-19 severity: a systematic review and meta-analysis. J Med Virol. 2021;93:1045–1056. doi: 10.1002/jmv.26389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gülsen A., Yigitbas B.A., Uslu B., et al. The effect of smoking on COVID-19 symptom severity: systematic review and meta-analysis. Pulm Med. 2020;2020:7590207. doi: 10.1155/2020/7590207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patanavanich R., Glantz S.A. Smoking is associated with COVID-19 progression: a meta-analysis. Nicotine Tob Res. 2020;22:1653–1656. doi: 10.1093/ntr/ntaa082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meena R.A., Sharifpour M., Gaddh M., et al. COVID-19-associated venous thromboembolism portends worse survival. Semin Vasc Surg. 2021;34:117–124. doi: 10.1053/j.semvascsurg.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Macias Gil R., Touzard-Romo F., Sanchez M.C., et al. Characteristics and outcomes of Hispanic/Latinx patients with coronavirus disease 19 (COVID-19) requiring hospitalization in Rhode Island: a retrospective cohort study. Ann Epidemiol. 2021;58:64–68. doi: 10.1016/j.annepidem.2021.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tai D.B.G., Shah A., Doubeni C.A., et al. The disproportionate impact of COVID-19 on racial and ethnic Minorities in the United States. Clin Infect Dis. 2021;72:703–706. doi: 10.1093/cid/ciaa815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cohen S.L., Gianos E., Barish M.A., et al. Prevalence and predictors of venous thromboembolism or mortality in hospitalized COVID-19 patients. Thromb Haemost. 2021;121:1043–1053. doi: 10.1055/a-1366-9656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Azevedo R.B., Botelho B.G., Hollanda J.V.G., et al. Covid-19 and the cardiovascular system: a comprehensive review. J Hum Hypertens. 2021;35:4–11. doi: 10.1038/s41371-020-0387-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Institutes of Health, US The COVID-19 treatment guidelines Panel's statement on anticoagulation in hospitalized patients with COVID-19. 2022. https://www.covid19treatmentguidelines.nih.gov/therapies/statement-on-anticoagulation-in-hospitalized-patients/ Available from: