Abstract
PURPOSE:
Nasopharyngeal carcinoma (NPC) is an aggressive malignant tumor that arises from the nasopharyngeal epithelial lining. Most patients with NPC present with a neck mass or cranial nerve palsy. It is infrequent for patients with NPC to present to an ophthalmologist initially with ophthalmic complaints and absence of prior diagnosis of NPC. We are reporting a series of six NPC cases that presented solely with ophthalmic complaints, to attract the attention of ophthalmologist to such a serious neoplasm.
METHODS:
A retrospective observational study of all consecutive patients diagnosed with NPC based on their initial ophthalmic presentation with no prior diagnosis of this neoplasm. Patients presented for the first time to two tertiary eye hospitals. Data were collected by the chart review for demographics, clinical presentation, radiological imaging, treatment regimen, and follow-up. Histopathological review of their tissue specimens was conducted by two pathologists.
RESULTS:
We had six patients who presented for the first time to our ophthalmic service complaining mostly of limitation of extraocular muscle motility with or without diplopia (4/6), orbital or facial pain (2/6), and disturbance in vision (2/6). The age ranged from 35 to 92 years with a mean of 58 years. A male predominance was observed with male-to-female ratio of 5:1. The cases are described along with their imaging and histopathological findings. Relevant literature review was also presented. Most of our patients (5/6) received combination of radiotherapy and chemotherapy. One patient refused treatment and 2 eventually passed away after 7 months.
CONCLUSION:
Ophthalmologists may play a major role in diagnosing such patients accurately and referring them for early management and better prognosis.
Keywords: Cranial nerve palsy, diplopia, nasopharyngeal carcinoma, orbital invasion
INTRODUCTION
Nasopharyngeal carcinoma (NPC) is an aggressive malignant tumor that arises from the nasopharyngeal epithelial lining. It is relatively uncommon, according to the World Health Organization (WHO), the estimated prevalence was said to be 0.7% of all cancers worldwide, however, in endemic areas such as Southern China and South-east Asia, the annual age-standardized incidence rates were as high as 30 cases per 100,000 population in men and 8–15 cases per 100,000 populations in women.[1] In Saudi Arabia, NPC represented 30% of all the reported head-and-neck tumors, with an age-standardized incidence rate of 1.5 per 100,000 population in male and 0.5 in female.[2] Neck mass was the most common complaint of these patient, and cranial nerve palsy being the 5th most common complaint.[2] In our literature review, we only found three case series that reported ophthalmic manifestations of NPC tumors before or in association with NPC initial presentation.[3,4,5] To the best of our knowledge, there were no local similar reports describing ophthalmic complaints as an initial presentation of NPC in our region. In this case series, we describe patients who presented to our ophthalmic practice before being diagnosed with NPC to highlight the most common possible ophthalmic manifestations of NPC tumors that should attract the attention of general ophthalmologists and ocular pathologists to this diagnosis.
METHODS
This is a retrospective, observational study of all consecutive patients diagnosed with NPC based on their clinical presentation with ophthalmic complaints for the first time to our service in two tertiary eye hospitals, in Riyadh, Saudi Arabia: King Khalid Eye Specialist Hospital (KKESH) and King Abdulaziz University Hospital during a total period of 15 years. We did not have patients who presented with ophthalmic manifestations following the diagnosis of NPC. Data were collected by reviewing the charts by the principle investigator to gather demographics, clinical presentation, radiological imaging, treatment regimen, and their latest follow-up. Histopathological review of their tissue specimens was conducted by two pathologists. This study has been conducted in compliance with the declarations of Helsinki and was approved by the Human Ethics Committee/Institutional Review Board at KKESH (RP-2062-CR). An informed written general consent was obtained from patients that included anonymous use of their information for purpose of publication.
RESULTS
Six patients were included in this study, ranging in age from 35 to 92 years of age with a mean age of 58 and a median of 57 years. A male predominance was observed with a male-to-female ratio of 5:1. None of them had a prior known history of NPC. The cases are summarized in Table 1. Most of these patients presented first with limitation of their extraocular muscle (EOM) movements with or without diplopia (4/6). Other major complaints included orbital or facial pain (2/6), disturbance in vision (2/6). Clinical presentation of these patients is summarized in Figure 1.
Table 1.
Demographics and clinical characteristics of 6 NPC cases with initial ophthalmic manifestations
| # | Age/Gender | Side | Symptoms | Signs | Initial vision | Final vision | EBV result | Treatment | Follow up duration/condition |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 33/M | Right | Diplopia | Limitation of abduction, decreased sensation in the Ophthalmic and Maxillary divisions’ distribution (6th, V1, V2) | 20/20 | 20/25 | Negative | Chemotherapy & radiotherapy | 3 years Alive No recurrence |
| 2 | 41/M | Right | Diplopia | Limitation of abduction, decreased sensation in the Ophthalmic and Maxillary divisions’ distribution (6th, V1, V2) | 20/20 | 20/20 | Focally positive | Chemotherapy & radiotherapy | 7 months Disease-related mortality |
| 3 | 43/F | Left | Diplopia | Limitation of abduction | 20/22.5 | 20/22.5 | Negative | Chemotherapy & radiotherapy | 2 years Alive No recurrence |
| 4* | 92/M | Left | Decreased vision on the unaffected side, left orbital pain | Orbital swelling 3 × 3cm inferior to medial canthus | Post- anterior exenteration | Not applicable | Focally positive | Chemotherapy & Radiotherapy | 15 years Alive No recurrence |
| 5 | 73/M | Left | Decreased vision, ptosis, orbital pain and left facial pain | limitation of EOM, decreased face sensation, fixed Dilated Pupil | NLP | NLP | Negative | Chemotherapy & Radiotherapy | 5 years Alive No recurrence |
| 6 | 76/M | Left | Left eye displacement inferiorly, and loss of vision for 2 years | Proptosis, totally frozen globe and loss of vision. | NLP | NLP | Negative | Refused Treatment | 7 months Disease-related mortality |
NPC: Nasopharyngeal carcinoma, F: Female, M: Male. OD: Right eye, OS: Left eye, NLP: No light perception, CF: Counting fingers, EOM: Extraocular motility, V: Fifth cranial nerve=Trigeminal nerve, EBV: Epstein Bar virus. 8This patient is post anterior exenteration 12 years prior to his presentation for recurrent left eye conjunctival squamous cell carcinoma that is unrelated to this current presentation.
Figure 1.

A graph showing the ophthalmic clinical signs and symptoms of the 6 cases as their initial presentation of nasopharyngeal carcinoma
Case 1
A 33-year-old male presented with diplopia. Visual acuity was recorded to be 20/20 in both eyes. EOM testing showed limitation of abduction of his right eye in addition to decreased sensation along the first and second branches of the trigeminal nerve. Magnetic resonance imaging (MRI) of the orbits and brain showed a destructive mass that is originating from the right infratemporal fossa, extending to the maxillary sinus, eroding the lateral maxillary wall and extending to the right sphenoid, with erosion of the inferior and lateral sphenoid walls. Incisional biopsy for the patient was done and histopathology showed malignant epithelial tumor of nasopharyngeal origin with surrounding heavy chronic inflammation and mixed pattern consisting of keratinizing squamous carcinoma (WHO I) and nonkeratinizing differentiated carcinoma (WHO II) of the Regaud subtype [Figure 2a and b]. The patient was managed with chemotherapy and radiotherapy in another tertiary care institute. The patient has been followed up for 3 years after treatment with no evidence of recurrence.
Figure 2.

(a) Histopathological appearance of the non-keratinizing squamous area of the mixed type nasopharyngeal carcinoma in case 1 (Original magnification ×200 Hematoxylin and eosin). (b) The appearance of the keratinizing squamous area in the same case (Original magnification ×400 Hematoxylin and eosin)
Case 2
A 41-year-old male presented with diplopia and normal vision. EOM motility revealed limitation of right eye abduction and decreased sensation in the first and second branches of the trigeminal nerve. MRI of the orbits and brain showed a large aggressive nasopharyngeal tumor with orbital, intracranial, cranial nerves, and masticator space extension as well as clival and basisphenoid bone involvement suggesting late stage (T4) lesion and multiple bilateral nodal metastatic lesions (N2). Histopathological examination of the right orbital incisional biopsy showed nonkeratinizing undifferentiated NPC of the Regaud subtype. The tumor cells strongly expressed staining with epithelial markers: CK-cocktail, CK 5/6, and P63. Epstein bar virus (EBV) staining was focally positive. The patient was started on chemotherapy and radiotherapy. However, he passed away because of disseminated disease 7 months after.
Case 3
A 43-year-old female presented similarly with diplopia and left eye limitation of abduction. Her visual acuity measured 20/20 in her right eye and 20/22.5 in her left eye. MRI of the orbits and brain revealed infiltrative nasopharyngeal soft-tissue mass involving the left orbit with skull base invasion and intracranial extension [Figure 3a]. Histopathological examination of the left orbit incisional biopsy revealed epithelial tumor with characteristic features of nonkeratinizing undifferentiated NPC with surrounding numerous lymphocytic and plasma cells infiltrate [Figure 3b]. IHC tumor cells expression of Pan-CK, CK 5/6, CK HMW, and P63 was observed [Figure 3c and d]. Other IHC markers to rule out neuroendocrine tumors (synaptophysin and chromogranin) were also performed with the lack of expression by tumor cells in addition to P16 and Melan A. EBV immunostaining was negative. The patient responded well to chemotherapy and radiotherapy with no change in her vision and remained alive for 2 years after.
Figure 3.
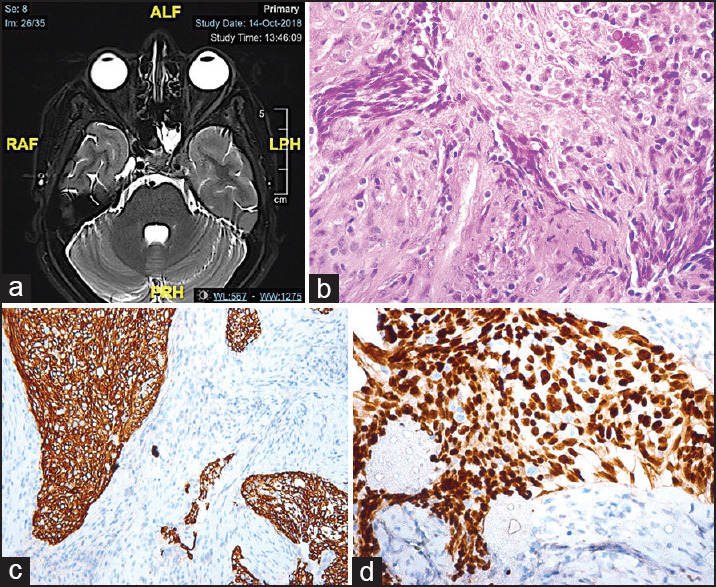
(a) Axial T2-weighted magnetic resonance imaging (in case 3) with an infiltrative nasopharyngeal soft tissue mass showing skull base invasion and intracranial extension. (b) The tumor in the same case showing areas of non-keratinizing squamous cell carcinoma with surrounding lymphocytes, plasma cells and Russel bodies (Original magnification ×400 Hematoxylin and eosin). (c) The tumor cells expressing epithelial cell marker (Original magnification ×200 CK5-6). (d) Another immunohistochemical stain showing p63 expression by the tumor cells (Original magnification ×400 p63)
Case 4
A 92-year-old one eyed patient, with a known history of left recurrent conjunctival squamous cell carcinoma, for which anterior exenteration was performed 12 years prior to his recent presentation. He presented with the complaint of decrease in vision in his right eye for 6 months duration, pain, and a growing left orbital mass over the last month. His visual acuity of the only remaining right eye measured 1/200 in his right eye. The left exenteration socket was clear. MRI of the orbits showed a large infiltrative mass involving the left maxillary sinus, nasopharynx, with expansion of the anterior and posterior ethmoidal air cells, and infiltration along the left medial orbital wall. Incisional biopsy of this left orbital extending mass was performed. The histopathological examination showed islands of nonkeratinizing squamous cell carcinoma and surrounding heavy lymphocytic infiltration and was consistent with lymphoepithelioma-like carcinoma or NPC of the Regaud subtype. The patient was referred to another institute to receive combined chemotherapy and radiotherapy, and he remained alive for 15 years after the diagnosis.
Case 5
A 73-year-old presented with decreased left eye vision, left orbital pain, and facial pain. Upon examination of the affected eye, his vision was completely lost while his visual acuity in the right eye measured 20/40. Physical examination of the patient showed 3–4 mm of left eye proptosis and moderate limitation of infra-duction and adduction with complete limitation of adduction and supra-duction on the left side. He had full EOM motility in his right eye. An afferent pupillary defect of Grade 3 was also noted in his left eye. Fundoscopy showed a healthy optic disc on the right and pale optic disc on the left eye. Computerized tomography scan of the orbits and brain showed an abnormal infiltrative lesion in the posterior-superior nasal fossa with extensive spread to the orbit, left orbital apex, superior orbital fissure, and parapharyngeal space on the left side in addition to extension into the masticator space, Meckel's cave, left cavernous sinus, and Eustachian tube. Left orbital incisional biopsy was performed and the tissue diagnosis confirmed a nonkeratinizing poorly differentiated squamous cell NPC. The patient was treated with radiotherapy and chemotherapy with follow-up of 5 years without evidence of recurrence.
Case 6
A 76-year-old male patient presented to the ER with loss of vision in the left eye, inferior displacement of the globe, disfigurement of the left palpebral fissure, and a frozen left globe. The patient was also observed to have an extensive mass in the upper fornix and no light perception in this eye. The patient was admitted for left orbital tumor biopsy and MRI of the brain and orbits. The MRI showed extensive tumor involving the dura, the left cavernous sinus, the ethmoid air cells, lateral orbital wall, orbital roof, with bone erosion effecting the ipsilateral lamina papyracea. It was extending to the left orbit with peri-optic nerve infiltration and was involving the EOMs, and the adjacent soft tissue of the upper fornix, forehead, and nasal bridge. The histologic sections of the incisional biopsy showed lobules of nonkeratinizing poorly differentiated squamous cell carcinoma heavily infiltrated by chronic inflammatory cells predominantly lymphocytes. The diagnosis was NPC of the Regaud subtype. Unfortunately, the patient refused treatment and he passed away 7 months following his diagnosis.
DISCUSSION
NPC is one of the most common malignancy of the head and neck accounting for 30%–33% of all tumors in this region.[2,6] It is more prevalent in the Asian and African population. NPC represents around 6% of all cancers reported annually in our population. In a retrospective review of 381 NPC cases by Clubb et al., found a male-to-female ratio of 3:1, with a bimodal age of distribution of 20–25 years and 45–55 years, and neck mass was the most common complaint.[2] Our patients were mostly males with a male-to-female ratio of 5:1. In their study, the most common ophthalmic presentation was cranial nerve palsy followed by ptosis, then proptosis.[2] However, all our cases presented first to our ophthalmology service without prior diagnosis of NPC. To the best of our knowledge, only three case series in the literature have shown cases with ophthalmic complaints as the initial signs of NPC.[3,4,5] The rest were all individual case reports with unique presentations.
In 2004, Hsu and Wang reported 13 patients with NPC that presented with ophthalmic complaints.[3] Their patients’ age ranged from 32 to 70 years, with a mean age of 55 years.[3] The most common presentation was proptosis, followed by diplopia, orbital pain, and lid mass.[3] Nine of their patients had a history of NPC.[3] In 2008, Lee at studied nine patients with NPC.[5] The demographic features were similar with a younger mean age of 49.2 years.[5] Their patients mostly presented with eyelid swelling and diplopia while one patient only in their study had no prior history of NPC at presentation.[5] In 2017, Wong et al., reviewed retrospective data for 354 consecutive patients who had been diagnosed with or treated for NPC.[4] They found only 13 patients with orbital involvement and the majority of these had no history of NPC.[4] The most common presentations among those with no prior history of NPC were blurred vision and facial numbness, while those with prior history of NPC complained mostly of headache and diplopia.[4] In our case series, the age ranged from 35 to 92 years with an older mean age of 58 years. Actually, half of our patients were above the mostly reported age range of NPC. In our series, EOM disturbance (mostly with diplopia) was the commonest presentation, followed by pain and loss of vision. Eyelid swelling, proptosis, atrophic optic disc, and orbital swelling were also observed less frequently [Figure 1].
The most common pathway for the NPC to spread by is through the pterygopalatine fossa and inferior orbital fissure in which they can form a direct communication between the infratemporal fossa and the orbit.[7] This was evident in our first case. The second most common pathway is through paranasal sinuses invasion either through the ethmoid and/or the sphenoid sinuses which erode the lamina papyracia to the retrobulbar area or the medial orbit, or through the maxillary sinus where the tumor may erode via the thin orbital floor, as seen in our patients (Cases 4,5 and 6).[7]
WHO defines NPCS as “A carcinoma arising in the nasopharyngeal mucosa that shows light microscopic or ultrastructural evidence of squamous differentiation” Historically, NPC has been classified in 1978 into WHO 1, WHO 2, and WHO 3, then was modified in 1991. Based on the histopathological features, NPC has been classified by WHO into different classifications, the most recent was in 2005, which has included three categories: Keratinizing squamous cell carcinoma, nonkeratinizing carcinoma with differentiated and undifferentiated subtypes, and basaloid squamous cell carcinoma.[8] In their recent classification, well-defined epithelial islands were termed “Regaud pattern,” while individual cells in ill-defined sheets are called “Schmincke pattern.” The term “lymphoepithelioma” refers to when the lymphoid component is predominant. Most of our patients (5/6) were of nonkeratinizing type (poorly or undifferentiated), the sixth case had a mixed keratinizing and nonkeratinizing type, four were of the Regaud subtype and two showed the typical predominant “lymphoepithelioma” appearance, It was also found that EBV staining is mostly found in nonkeratinizing NPC.[8] In our case series, only three showed positive staining for EBV.
Radiotherapy is the standard treatment; however, NPC is also chemotherapy sensitive. Therefore, radiotherapy is best used when there is a localized NPC. However, whenever there are metastases or the NPC is not localized, it is best to include chemotherapy in the management.[9] Surgery for NPC is reserved whenever the tumor seems to be resistant to the standard treatment or whenever there is recurrence.[9] Most of our patients (5/6) received combination of radiotherapy and chemotherapy. None of the patients underwent surgery. One patient refused treatment and 2 eventually passed away.
CONCLUSION
In conclusion, NPC is not an uncommon malignancy among our population. Patients might present initially to the ophthalmologist. Therefore, ophthalmic/oculoplastic surgeons and ocular pathologists should be aware of the unique presentation of NPC. Early tissue diagnosis with histopathological confirmation and staging will allow earlier treatment and better outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.WHO. 2014 Review of Cancer Medicines on the WHO List of Essential Medicines Nasopharyngeal Carcinoma. [Last accessed on 1 Aug 2021];Union Int Cancer Control. 2014 :1–9. Available at https://www.who.int/selection_medicines/committees/expert/20/applications/NasopharyngealCarcinoma.pdf . doi: 10.1016/B978-0-12-374984-0.01018-4. [Google Scholar]
- 2.Clubb B, Quick C, Amer M, Ali A, Greer W, De Vol EB, et al. Nasopharyngeal carcinoma in saudi arabia: Selected clinical and epidemiological aspects. Ann. Saudi Med. 1990;10:171–5. [Google Scholar]
- 3.Hsu WM, Wang AG. Nasopharyngeal carcinoma with orbital invasion. Eye (Lond) 2004;18:833–8. doi: 10.1038/sj.eye.6701358. [DOI] [PubMed] [Google Scholar]
- 4.Wong WM, Young SM, Amrith S. Ophthalmic involvement in nasopharyngeal carcinoma. Orbit. 2017;36:84–90. doi: 10.1080/01676830.2017.1279658. [DOI] [PubMed] [Google Scholar]
- 5.Lee KY, Seah LL, Tow S, Cullen JF, Fong KS. Nasopharyngeal carcinoma with orbital involvement. Ophthalmic Plast Reconstr Surg. 2008;24:185–9. doi: 10.1097/IOP.0b013e318171a629. [DOI] [PubMed] [Google Scholar]
- 6.Al-Shahrani ZS, Al-Rawaji AI, Al-Madouj AN, Hayder MS, Al-Zahrani AS, Al-Mutlaq HM, et al. Vol. 108. Saudi Arabia: Saudi Health Council; 2014. [Last accessed on 01 Aug 2021]. Cancer incidence report. In: Kingdom Saudi Arab. Minist. Heal. Saudi Cancer Regist. Available from: https://nhic.gov.sa/eServices/Documents/2014.pdf . [Google Scholar]
- 7.Luo CB, Teng MM, Chen SS, Lirng JF, Guo WY, Chang T. Orbital invasion in nasopharyngeal carcinoma: Evaluation with computed tomography and magnetic resonance imaging. Zhonghua Yi Xue Za Zhi (Taipei) 1998;61:382–8. [PubMed] [Google Scholar]
- 8.Thompson LD. Update on nasopharyngeal carcinoma. Head Neck Pathol. 2007;1:81–6. doi: 10.1007/s12105-007-0012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wei WI, Kwong DL. Current management strategy of nasopharyngeal carcinoma. Clin Exp Otorhinolaryngol. 2010;3:1–12. doi: 10.3342/ceo.2010.3.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


