Abstract
Objectives
To examine the effectiveness of prone positioning on COVID-19 patients with acute respiratory distress syndrome with moderating factors in both traditional prone positioning (invasive mechanical ventilation) and awake self-prone positioning patients (non-invasive ventilation).
Research methodology
A comprehensive search was conducted in CINAHL, Cochrane library, Embase, Medline-OVID, NCBI SARS-CoV-2 Resources, ProQuest, Scopus, and Web of Science without language restrictions. All studies with prospective and experimental designs evaluating the effect of prone position patients with COVID-19 related to acute respiratory distress syndrome were included. Pooled standardised mean differences were calculated after prone position for primary (PaO2/FiO2) and secondary outcomes (SpO2 and PaO2)
Results
A total of 15 articles were eligible and included in the final analysis. Prone position had a statistically significant effect in improving PaO2/FiO2 with standardised mean difference of 1.10 (95%CI 0.60–1.59), SpO2 with standardised mean difference of 3.39 (95% CI 1.30–5.48), and PaO2 with standardised mean difference of 0.77 (95% CI 0.19–1.35). Patients with higher body mass index and longer duration/day are associated with larger standardised mean difference effect sizes for prone positioning.
Conclusions
Our findings demonstrate that prone position significantly improved oxygen saturation in COVID-19 patients with acute respiratory distress syndrome in both traditional prone positioning and awake self-prone positioning patients. Prone position should be recommended for patients with higher body mass index and longer durations to obtain the maximum effect.
Keywords: Acute respiratory distress syndrome, COVID-19, Prone position, Coronavirus 2, Respiratory failure
Implications for clinical practice.
-
•
Both traditional prone positioning and awake self-prone positioning patients are effective for patients with COVID-19 ARDS.
-
•
Implementing prone position for patients with higher BMI are supported by the study’s results.
-
•
Longer durations of prone position is recommended for more benefits in traditional prone position.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has increased the number of hospitalised patients, especially with respiratory failures (Grasselli et al., 2020). Based on previous research, patients’ mortality rates were reported at 39% of 10,815 COVID-19 patients globally in all settings, while in the critical care settings, particularly in those with mechanical ventilation, the rates reached 94% (Gibson et al., 2020, Hasan et al., 2020). The SARS-CoV-2 mainly affects and causes more damage to the respiratory system than other organs (Li and Ma, 2020). The rapid onset of widespread inflammation in the lungs can result in severe hypoxemia and can develop into an acute respiratory distress syndrome (ARDS) (Bos, 2020). Examining the effectiveness of interventions and moderating factors on interventions for ARDS is essential to improve patient outcomes.
According to the World Health Organisation (WHO) guidelines, ARDS related to COVID‐19 is diagnosed when someone with confirmed COVID-19 infection meets the Berlin 2012 ARDS diagnostic criteria and there are pathological changes of diffuse alveolar damage in the lungs (Gibson et al., 2020). Based on the Berlin definition with oxygenation index, arterial oxygen partial pressure to inspired oxygen fraction (PaO2/FiO2), ARDS can be classified into: mild (200 mmHg < PaO2/FiO2 ≤ 300 mmHg), moderate (100 mmHg < PaO2/FiO2 ≤ 200 mmHg), and severe (PaO2/FiO2 ≤ 100 mmHg) (Ranieri et al., 2012). However, the National Health Commission of China developed a set of classifications for ARDS related to COVID-19 where PaO2/FiO2 less than 150 mmHg is moderate-severe (Li and Ma, 2020).
Another definition for ARDS related to COVID-19 suggested by Brown et al. (2021) is a patient receiving high-flow nasal oxygen therapy, non-invasive ventilation, or invasive mechanical ventilation for acute hypoxemic respiratory failure owing to SARS-CoV-2 pneumonia with the Kigali modification of oxygen saturation to fraction of inspired oxygen ratio (SpO2/FiO2) < 315 eliminating requirements for positive end-expiratory pressure and positive pressure ventilation. Brown and colleagues reasoned that this is consistent with the Berlin definition’s pathophysiological rationale without meaningfully altering the specificity of the resulting diagnosis or the relevance of ARDS-specific treatments (Brown et al., 2021).
The management of ARDS-related COVID-19 interventions for oxygen therapy includes high-flow nasal oxygen therapy, non-invasive ventilation, and invasive mechanical ventilation (Brown et al., 2021). Each of those interventions could be combined with prone position as a rescue therapy (Chad and Sampson, 2020). Prone positioning refers to positioning a patient face down onto their anterior chest and abdomen to take advantage of physiologic changes that can result in improved oxygenation through decreased ventilation/perfusion mismatch and, potentially, decreased lung injury (Venus et al., 2020). In the prone position, expansion of the anterior chest wall is restricted, resulting in a more homogeneous chest wall compliance (Bamford et al., 2020).
Prone positioning is generally reserved for sedated patients who are on invasive mechanical ventilation [known as traditional ICU prone positioning], but it may be beneficial for awake patients with COVID-19 with high-flow nasal oxygen therapy and non-invasive ventilation [known as awake self-prone positioning (ASPP)] (COVID-19 Treatment Guidelines Panel, 2020, Hadaya and Benharash, 2020). Prone position has been widely adopted to treat invasive mechanical ventilation patients with ARDS related to COVID-19, the majority of patients improved their oxygenation during prone position, most likely due to a better ventilation perfusion matching (Langer et al., 2021). The WHO recommends the use of 12–16 h/day prone position to improve oxygenation and patient survival under mechanical ventilation (Guérin et al., 2013, Organization, 2020).
Awake self-prone positioning in non-intubated patients with acute hypoxic respiratory failure is also feasible and safe (Jayakumar et al., 2021). There’s an increase in research evidence in treating COVID-19 patients on non-invasive ventilation with ASPP that have reported a significant improvement in oxygenation (Sodhi and Chanchalani, 2020). Moreover, the initiation of ASPP is associated with lower mortality and lower intubation rate (Kharat et al., 2022, Oliveira et al., 2022, Rahmani et al., 2020), and ASPP for COVID-19 patients has become a widespread intervention (Rahmani et al., 2020).
Previous meta-analyses have identified the effectiveness of prone position in patients with COVID-19 (Reddy et al., 2021). However, to our knowledge, no meta-analysis has yet examined whether the effectiveness of prone position will differ in regards to the demographic characteristics, duration, frequency, length of therapy, total time, time point measurement, underlying pathophysiology, and other respiratory supports used for COVID-19 patients with ARDS. As the prone position is currently used in up to 76% of invasive mechanical ventilation COVID-19 patients (Ferrando et al., 2020, Ziehr et al., 2020), it is essential to evaluate these moderating characteristics in detail. Therefore, we aimed to extend the previous knowledge base by conducting a comprehensive meta-analysis and meta-regression to (1) assess the effectiveness of prone position towards the oxygenation status in patients with ARDS related to COVID-19 and (2) examine moderating factors pertaining to the effectiveness of prone position in both traditional ICU prone positioning and awake self-prone positioning patients.
Methods
Reporting standards
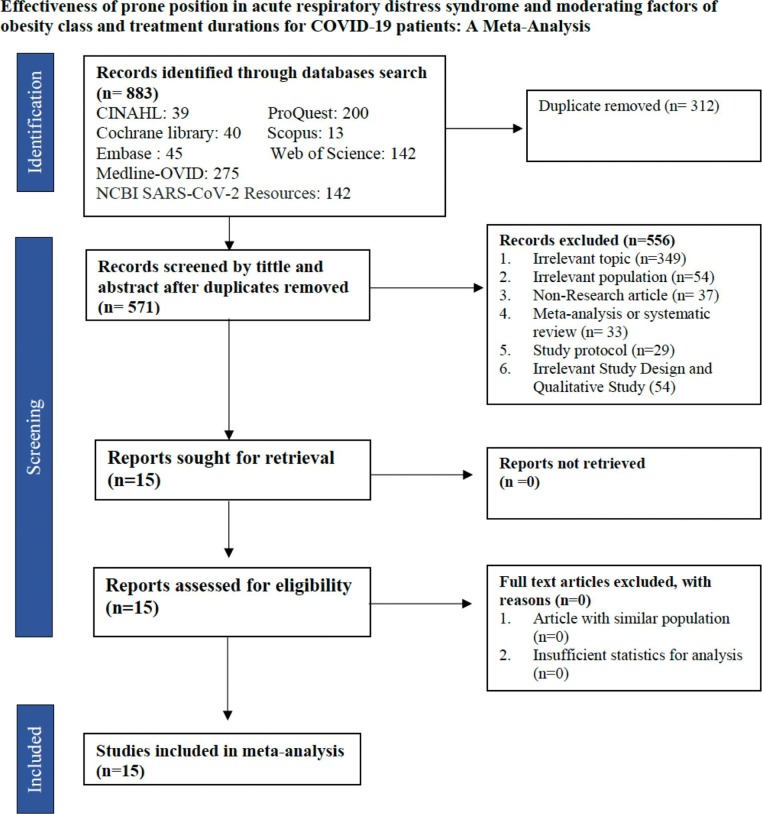
The current review is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement (Moher et al., 2009) (Fig. 1 ) and registered in PROSPERO (CRD42020225465).
Fig. 1.
Flow diagram for study selection.
Search strategy
Systematic search was conducted in the databases of CINAHL, Cochrane library, Embase, Medline-OVID, NCBI SARS-CoV-2 Resources, ProQuest, Scopus, and Web of Science. Manual searches have also been conducted on Google Scholar and reference lists of previously published studies to retrieve more relevant articles. The search was performed using combination keywords of “COVID 19” OR “Covid-19” OR “SARS-Cov 19” OR “SARS-COV 2019” OR SARS-COV-19” OR “corona virus disease” OR “corona virus 19 disease” AND “Acute respiratory syndrome” OR “ARDS” AND “Prone Positioning” OR “Proning” OR “proning position” and without date of publication and language restrictions. The last update in the search was 12th May 2021.
Eligibility criteria and screening procedures
All articles from the databases were comprehensively screened using EndNote version 9.3 software. Systematic screening was conducted by two independent reviewers to identify eligible studies according to the PICOS criteria: This study focused on patients diagnosed with COVID-19 related to ARDS that were administered in the inpatient unit and studies that evaluate the effectiveness of prone positioning were included in the analysis.
The primary outcome of this study was PaO2/FiO2 after prone position. Secondary outcomes are other respiratory physiology parameters, including SpO2 and PaO2. This study includes all analytical studies, observational and experimental, which evaluate prone position, either with or without a control group. We included prospective studies approaches as they ranked higher in the hierarchy of evidence than retrospectives design (Euser et al., 2009).
Data extraction and study outcomes
The data extracted include: study identity, study characteristics (study design, country, and setting), participant characteristics (sample, mean age, gender, mean body mass index [BMI]), intervention characteristics (frequency, duration, and, total time of prone position, time measurement and respiratory support intervention) and outcome (PaO2/FiO2, SpO2, and PaO2).
Quality assessment
Risk of bias at the individual study level was assessed using the Methodological Index for Non-randomised Studies (MINORS) (Slim et al., 2003). The MINORS is a validated instrument used to determine the methodological quality of non-randomised surgical studies, comparative and non-comparative. It consists of eight items for non-comparative studies and an additional four items for comparative studies. The maximum score is 16 for non-comparative studies which are categorised as: 0–4, very low quality; 5–8, low quality; 9–12, moderate quality; and 13–16, high quality (Öhlin et al., 2019).
Statistical analysis
This study analysed the pooled evidence using R software version 4.0.2. The effectiveness of prone position towards oxygenation status was provided in standardised mean difference (SMD) format along with 95% confidence intervals (95% CI). Interpretation of standardised mean difference values are as follows: <0.2 are considered trivial, value of ≥0.2 and <0.5 are considered small, values of ≥0.5 and <0.8 are considered medium, and values ≥0.8 are considered large (Andrade, 2020).
To assess heterogeneity of treatment effects across studies, the Q-statistic and I 2 statistics were computed. The I 2 measures the extent of inconsistency among the study’s results, and the outcome is interpreted as a percentage of total variation across studies that are due to heterogeneity rather than chance (Higgins et al., 2003). Heterogeneity was quantified as low, moderate, and high, with upper limits of 25%, 50% and 75% for I 2, respectively (Melsen et al., 2014). The fixed- and random-effect models were calculated. The random-effect model was adopted in the analysis considering variations among the included studies (Serghiou and Goodman, 2019).
Sensitivity analyses were conducted to investigate the influence of individual studies on the overall effect by eliminating one study at a time.
Moderator analysis
Subgroup analysis and meta-regression were conducted for moderator analysis among the included studies (Higgins et al., 2003). We performed subgroup analysis for several potential moderator variables including, age (adult and elderly), body mass index (normal weight, pre-obesity, obesity class I, obesity class II), comorbidities (comorbidities and no-comorbidities), unit (intensive care unit [ICU] and non ICU), frequency for prone position (1 time/day, 2 times/day, 3 times/day), duration of prone position per day (less than 12 hours and equal to or greater than 12 hours), types of ARDS (mild, moderate and severe), study design (experiment and observational) and prone position (traditional ICU Prone positioning and ASPP). Meta-regression was performed for mean duration prone position/day, mean frequency prone position/day, mean total time of therapy prone position/patient, mean time measurement and mean sample size. A result with p-value less than 0.05 indicated a significant moderator.
Results
Descriptions of studies
From the electronic databases, 883 articles were retrieved and 312 duplicate articles were identified. After screening, 556 articles were excluded based on the title and abstract for the following reasons; irrelevant topic (349 articles), irrelevant population (54 articles), irrelevant study design and qualitative study (55 articles), non-research article (37 articles), meta-analysis or systematic review (33 articles), study protocol (29 articles). Finally, based on the full-text screening, 15 articles were eligible and included in the final analysis for this study (Abou-Arab et al., 2021, Avdeev et al., 2021, Caputo et al., 2020, Clarke et al., 2021, Elharrar et al., 2020, Fazzini et al., 2021a, Gad, 2021, Mittermaier et al., 2020, Paternoster et al., 2020, Sartini et al., 2020, Taboada et al., 2021, Taboada et al., 2020, Thompson et al., 2020, Zang et al., 2020, Ziehr et al., 2020).
Study characteristics
All of the included studies were published in 2020 and 2021 as the first case of COVID-19 was identified by the end of 2019. The settings of the studies were in the intensive care unit (8 studies) and non-intensive care unit (7 studies). From these included studies, 288 participants were identified, and the range of the sample size in each study varied from 7 to 50 participants. Most participants were male (65%) with ages ranging from 38 to 87 years and body mass index ranging from 24 to 36 kg/m2. The intervention included: prone position with the frequency of the interventions ranged from 1 to 3 times/day with a duration of 0.5 to 12 hours/day. The primary outcome is oxygen saturation, which was measured by using PaO2/FiO2 (12 studies), as well as for secondary outcomes SpO2 (5 studies) and PaO2 (5 studies), see Table 1 .
Table 1.
Characteristics of the included studies (n = 15).
| No | Study ID | Study characteristics |
Participant characteristic |
Intervention characteristics |
Outcomes |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Design | Country | Setting | n | Demographic | Comorbidities |
Prone position | Respiration support intervention | Time measurements | |||
| 1 | Abou-arab et al., 2020 | Prospective cohort study |
France | ICU | 25 | Age: Mean = 62 Range = 57–64 Gender: M = 20 F = 5 Mean BMI: 30 |
Comorbidities: Hypertension Diabetes Respiratory disease |
Frequency: 1x/day Duration: 16 hour session Length of therapy: 1 day Total time: 16 hours Intervention time from admission: NA |
PEEP Ventilator |
PaO2/FiO2 | Baseline and 16 h after prone |
| 2 | Avdeev et al., 2021 | Prospective cohort study |
Russia | Non-ICU | 22 | Age: Mean = 48.5 Range = 39.8–62.8 Gender: M = 16 F = 6 Mean BMI: 28.7 |
Comorbidities: Hypertension Diabetes |
Frequency: 1x/day Duration: 3 hour/session Length of therapy: 1 day Total time: 3 hours Intervention time from admission: NA |
CPAP | PaO2/FiO2 | Baseline and 3 h after prone |
| 3 | Caputo et al., 2020 | Prospective cohort study |
United States | Non-ICU | 50 | Age: Mean = 59 Range = 50–68 Gender: M = 30 F = 20 Mean BMI: NA |
Comorbidities: NA |
Frequency: 1x/day Duration: 5 minute/session Length of therapy: 1 day Total time: 5 minutes Intervention time from admission: NA |
NRM, Nasal Cannula | PaO2/FiO2 | Baseline and 5 min after prone |
| 4 | Clarke et al., 2021 | Prospective cohort study |
Ireland | ICU | 20 | Age: Mean = 54 Range = 45–59 Gender: M = 18 F = 2 Mean BMI: 36 |
Comorbidities: NA |
Frequency: 3x/day Duration: NA Length of therapy: NA Total time: 16.2 hours Intervention time from admission: NA |
PEEP Ventilator |
PaO2/FiO2 PaO2 |
Baseline and 1 h after prone |
| 5 | Elharrar et al., 2020 | Prospective cohort study |
France | ICU | 24 | Age Mean = 66.1 Range=– Gender: M = 16 F = 8 Mean BMI: 30 |
Comorbidities: NA |
Frequency: 1x/day Duration: 3 hour/session Length of therapy: 1 day Total time: 3 hours Intervention time from admission: NA |
HFNC Nasal Cannula |
PaO2 | Baseline and 1–2 h after prone |
| 6 | Fazzini et al., 2021 | Prospective cohort study |
United Kingdom | ICU | 46 | Age: Mean = 56 Range = 30–79 Gender: M = 23 F = 11 Mean BMI: NA |
Comorbidities: NA |
Frequency: 1x/day Duration: 5 hour/session Length of therapy: day Total time: 5 hours Intervention time from admission: NA |
HFNO CPAP |
PaO2/FiO2 | Baseline and 1 h after prone |
| 7 | Gad, 2021 | Prospective randomised trial |
Egypt | ICU | 15 | Age: Mean = 49 Range = 38–62 Gender: M = 9 F = 6 Mean BMI: NA |
Comorbidities: NA |
Frequency: 5x/day Duration: 2 hour/session Length of therapy: 4 day Total time: 40 hours Intervention time from admission: NA |
HFNO CPAP HFNO |
PaO2/ | Baseline and 2 h after prone |
| 8 | Mittermaier et al., 2020 | Prospective observational study | Germany | ICU | 9 | Age: Mean = 62 Range = NA Gender: M = 6 F = 3 Mean BMI: 30.4 |
Comorbidities: Diabetes Respiratory disease Obesity |
Frequency: 1x/day Duration: 2–3 hour/session Length of therapy: 6 days Total time: 12 hours Intervention time from admission: NA |
PEEP | PaO2/FiO2 | Baseline and 12 h after prone |
| 9 | Paternoster et al., 2020 | Prospective cohort study |
Italy | ICU | 11 | Age: Mean = 62 Range = NA Gender: M = 4 F = 7 Mean BMI: NA |
Comorbidities: Hypertension Diabetes Respiratory disease |
Frequency: 1x/day Duration: 12 hour/session Length of therapy: 3 days Total time: 36 hours Intervention time from admission: NA |
CPAP | PaO2/FiO2 | Baseline and 24 h after prone |
| 10 | Sartini et al., 2020 | Quasi-experiment | Italy | Non-ICU | 15 | Age: Mean = 59 Range = NA Gender: M = 13 F = 2 Mean BMI: 24 |
Comorbidities: NA |
Frequency: 2x/day Duration: 3 hour/session Length of therapy: 1 day Total time: 6 hours Intervention time from admission: 5 hours |
Face Mask High-Oxygen | PaO2/FiO2 SpO2 |
Baseline and 1 h after prone |
| 11 | Taboada et al., 2020 (a) | Prospective cohort study |
Spain | ICU | 7 | Age: Mean = 65 Range = 49–77 Gender: M = 3 F = 4 Mean BMI: NA |
Comorbidities: Hypertension Diabetes Respiratory disease |
Frequency: 2x/day Duration: 2 hour/session Length of therapy: 3 days Total time: 12 hours Intervention time from admission: NA |
Ventilator | PaO2/FiO2 PaO2 |
Baseline and 12 h after prone |
| 12 | Taboada et al., 2020 (b) | Prospective cohort study |
Spain | Non-ICU | 29 | Age: Mean = 64 Range = NA Gender: M = 21 F = 8 Mean BMI: 29.2 |
Comorbidities: Hypertension Diabetes Respiratory disease |
Frequency: 1x/day Duration: 1 hour/session Length of therapy: 1 days Total time: 1 hour Intervention time from admission: NA |
HFNC | PaO2/FiO2 SpO2 |
Baseline and 1 h after prone |
| 13 | Thompson et al., 2020 | Prospective cohort study |
United States | Non-ICU | 25 | Age: Mean = 66.5 Range = 45–87 Gender: M = 18 F = 7 Mean BMI: 29 |
Comorbidities: Hypertension Diabetes Respiratory disease |
Frequency: 1x/day Duration: 5 hour/session Length of therapy: 2 days Total time: 10 hours Intervention time from admission: 3.25 hours |
NRM Nasal Cannula |
SpO2 | Baseline and 1 h after prone |
| 14 | Zang, et al., 2020 | Prospective cohort study |
China | ICU | 23 | Age: Mean = 59,78 Range = 48–79 Gender: M = 14 F = 9 Mean BMI: NA |
Comorbidities: NA |
Frequency: 1x/day Duration: 0.5 hour/session Length of therapy: 1 days Total time: 0.5 hours Intervention time from admission: NA |
HFNC | SpO2 | Baseline and 10 min after prone |
| 15 | Zeihr et al., 2020 | Prospective cohort study |
Israel | ICU | 31 | Age: Mean = 58 Range = 23–87 Gender: M = 20 F = 11 Mean BMI: 30 |
Comorbidities: Hypertension Diabetes Respiratory disease |
Frequency: 1x/day Duration: 18 hour/session Length of therapy: 1 days Total time: 18 hours Intervention time from admission: NA |
Ventilator | PaO2/FiO2 | Baseline and 18 h after prone |
Abbreviation: ICU: intensive care unit; Non-ICU: non-intensive care unit; BMI: body mass index; Freq: frequency; Dur: duration; CPAP: continuous positive airway pressure; HFNC: high-flow nasal cannula; HFNO: high-flow nasal oxygen; PEEP: positive end-expiratory pressure; NRM: nonrebreathing mask; PaO2/FiO2: ratio of arterial oxygen partial pressure (PaO2 in mmHg) to fractional inspired oxygen (FiO2); RR: respiratory rate; SpO2: oxygen saturation in blood; FiO2: fraction inspired oxygen; PaO2: partial pressure of oxygen.
Quality assessment
Two assessors worked individually to evaluate the quality of the included studies using the MINORS. Cohen’s kappa analysis showed a value at 0.218, interpreted as a fair agreement with non-significant differences between the two assessors (p-value 0.095) see Table 2 . All included studies were evaluated using the risk of bias developed for the non-randomised study. The overall result showed 15.4% (2 studies) had high quality, and 84.6 % (11 studies) had moderate quality. Sensitivity analyses were conducted by eliminating one study each time, including studies with the lowest and highest time point measurement and the results showed the effectiveness of prone position had no significant difference with standardised mean differences ranging from 1.67 to 2.14.
Table 2.
Quality assessment using the methodological index for non-randomized studies (MINORS).
| No. |
Study |
Score |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
Total |
||
| Non-comparative studies | ||||||||||
| 1. | Abou-Arab et al., 2021 | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 2 | 13 |
| 2. | Avdeev et al., 2021 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 14 |
| 3. | Caputo et al., 2020 | 2 | 2 | 2 | 1 | 0 | 2 | 1 | 2 | 12 |
| 4. | Clarke et al., 2021 | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 1 | 10 |
| 5. | Elharr et al., 2020 | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 1 | 12 |
| 6. | Fazzini et al., 2021 | 2 | 2 | 2 | 1 | 0 | 2 | 0 | 2 | 11 |
| 7. | Gad, 2021 | 2 | 2 | 2 | 1 | 0 | 2 | 1 | 2 | 12 |
| 8 | Mittermaier et al., 2020 | 2 | 1 | 2 | 2 | 0 | 2 | 0 | 2 | 11 |
| 9. | Paternoster et al., 2020 | 2 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 13 |
| 10. | Sartini et al., 2020 | 2 | 2 | 2 | 1 | 0 | 2 | 1 | 1 | 11 |
| 11 | Taboada et al., 2020 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 12 |
| 12. | Taboada et al., 2020 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 1 | 11 |
| 13. | Thompson et al., 2020 | 2 | 2 | 2 | 1 | 0 | 0 | 1 | 1 | 9 |
| 14 | Zang, et al., 2020 | 2 | 1 | 2 | 1 | 0 | 0 | 2 | 1 | 9 |
| 15. | Ziehr et al., 2020 | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 1 | 12 |
Note: The items are scored 0 (not reported), 1 (reported but inadequate) or 2 (reported and adequate). For non-comparative studies, the scores are as follows: 0–4 very low quality, 5–8: low quality, 9–12: moderate quality, and 13–16: high quality.
Meta-analysis
Primary outcome
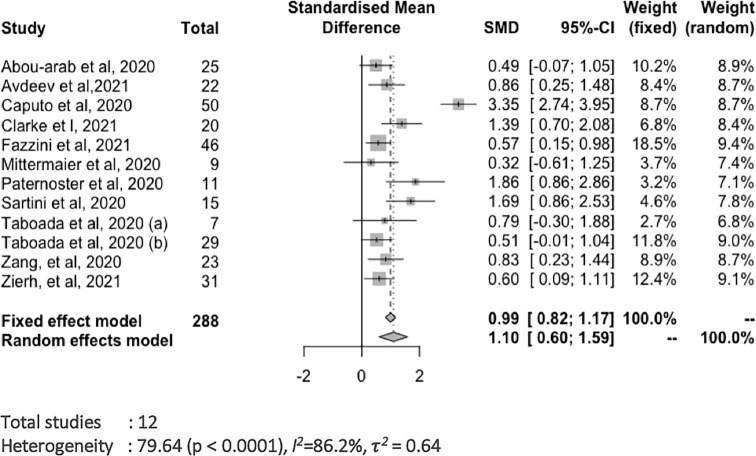
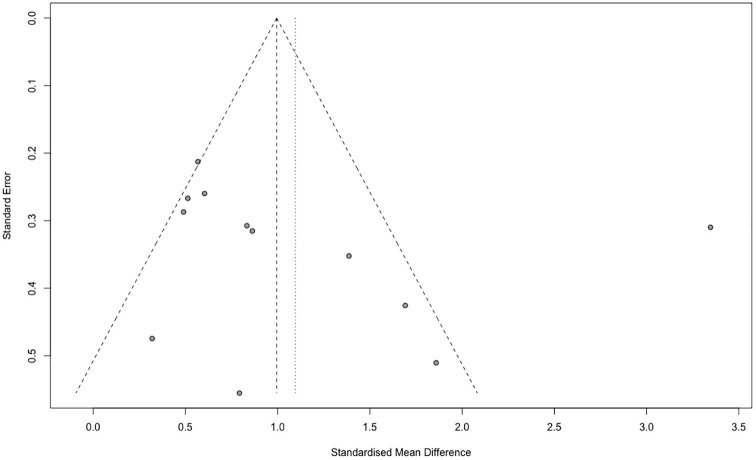
Prone position had a statistically significant effect in improving oxygen fraction PaO2/FiO2 (p < 0.0001), with a relatively large effect size of standardised mean difference 1.10 (95%CI 0.60–1.59) (Fig. 2 .). The sensitivity analysis showed pooled standardised mean difference from 1.62 to 2.16. Heterogeneity test revealed I2 = 86.2% and Q-value at 79.64 (p < 0.0001). The publication bias was analysed using Begg-Mazumdar test and found no significant result (p-value = 0.53).
Fig. 2.
Forest plot the effects of prone position towards PaO2/FiO2.
Secondary outcomes
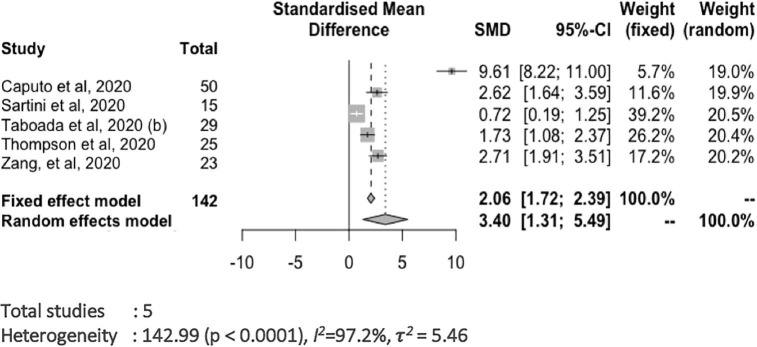
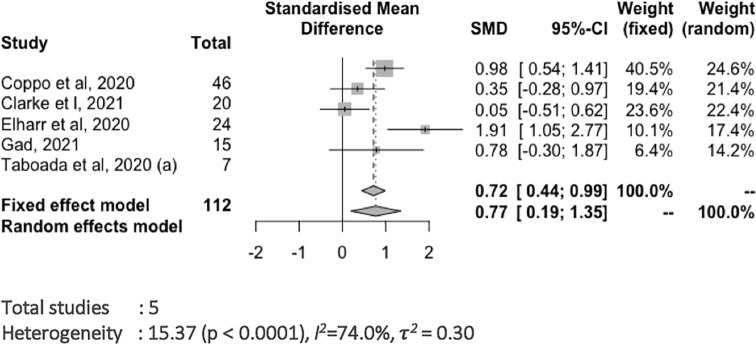
Our meta-analysis also identified a significant effect of prone position in improving SpO2 (p = 0.001), with a relatively large effect size of standardised mean difference 3.40 (95%CI 1.31–5.49) with I2 97.2% and Q-value at 142.99 (p < 0.0001) ( Fig. 3 .). Furthermore, prone position showed a significant effect in improving PaO2 (p = 0.009), with a relatively medium effect size of standardised mean difference 0.77 (95%CI 0.19–1.35) with I2 = 74% and Q-value at 15.37 (p = 0.004) (Fig. 4 .)
Fig. 3.
Forest plot the effects of prone position towards SpO2.
Fig. 4.
Forest plot the effects of prone position towards PaO2.
Moderator analysis
Subgroup analyses were conducted for several potential moderator variables including age, body mass index (BMI), comorbidities, unit, frequency for prone position, duration of prone position per day, types of ARDS, study design, and prone position. Of the seven studies included in the analysis, prone position showed the highest effect on obesity class II body mass index with standardised mean difference 5.53 (95%CI 4.11–6.95) followed by body mass index obesity class I standardised mean difference 2.12 (95%CI 1.66–2.58), normal weight body mass index standardised mean difference 1.79 (95%CI 0.93–2.66) and body mass index pre-obesity standardised mean difference 1.19 (95%CI 0.72–1.65). Subgroup analysis for the variables of age, comorbidities, patient unit, respiratory support intervention, frequency of prone position and type of ARDS, study design, and prone position showed no significant differences. All results are provided in Table 3 .
Table 3.
Subgroup analysis.
| Variable | Subgroup analysis |
|||
|---|---|---|---|---|
| n | SMD (95% CI) |
p-value | I2 | |
| Age | ||||
| Adult (18–65 years old) | 10 | 1.00 (0.63–1.37) | 0.13 | 69.4 |
| Elderly (>65 years old) | 2 | 0.55 (0.07–1.02) | ||
| BMI | ||||
| Normal weight | 1 | 1.79 (0.93–2.66) | <0.0001 | 93.9 |
| Pre-obesity | 2 | 1.19 (0.72–1.65) | ||
| Obesity class I | 3 | 2.12 (1.66–2.58) | ||
| Obesity class II | 1 | 5.53 (4.11–6.95) | ||
| Comorbidities | ||||
| Comorbidities | 7 | 0.65 (0.39–0.91) | 0.10 | 86.2 |
| No-comorbidities | 5 | 1.53 (0.50–2.55) | ||
| Unit | ||||
| ICU | 6 | 0.97 (0.45–1.49) | 0.78 | 69.4 |
| Non-ICU | 6 | 0.88 (0.49–1.27) | ||
| Respiration Support Intervention | ||||
| Ventilator | 3 | 0.83 (0.83–1.58) | 0.53 | 74.9 |
| Non-ventilator | 5 | 1.13 (0.55–1.71) | ||
| Frequency Prone Position/day | ||||
| 1 time/day | 8 | 0.97 (1.15–1.04) | 0.85 | 86.2 |
| 2 times/day | 2 | 1.82 (1.10–2.55) | ||
| 3 times/day | 2 | 5.53 (4.11–6.95) | ||
| Duration Prone Position/day | ||||
| <12 hours | 8 | 0.93 (0.49–1.36) | 0.95 | 69.4 |
| Equal to or great 12 hours | 4 | 0.94 (0.41–1.48) | ||
| Type of ARDS | ||||
| Mild | 2 | 1.06 (−0.17 to 2.31) | 0.10 | 69.4 |
| Moderate | 7 | 0.67 (0.44–0.89) | ||
| Severe | 3 | 3.30 (−0.17 to 2.31). | ||
| Study design | ||||
| Experimental | 2 | 0.96 (0.58–1.34) | 0.66 | 69.4 |
| Observational | 10 | 0.82 (0.28–1.36) | ||
| Prone Position | ||||
| Traditional | 5 | 0.84 (0.37–1.31) | 0.64 | 69.4 |
| ASPP | 7 | 0.99 (0.54–1.45) | ||
Abbreviation: Study size (n); Confident interval (CI); Reference (ref), Significance level <0.05.
Meta-regression was performed for mean duration prone position/day, mean frequency prone position/day, mean total time of therapy prone position/patient, mean time measurement and mean sample size. Based on the results meta-regression analysis, mean duration prone position/day (1.17, 95%CI 0.59–2.02) and mean total time prone position/patients (1.30, 95%CI 0.56–1.77) showed significant relationships to the results of the current study. The variables of mean of frequency prone position/day and sample size showed no significant differences in results (see Table 4 ).
Table 4.
Meta-regression.
| Variable | Meta-regression analysis |
||||
|---|---|---|---|---|---|
| n | SE | Z-value | SMD (95% CI) |
p-value | |
| Mean duration prone position/day | 12 | 0.36 | 3.59 | 1.17 (0.59–2.02) | <0.0001 |
| Mean frequency frone position/day | 12 | 0.75 | 0.35 | 0.21 (−1.26 to 1.68) | 0.09 |
| Mean total time prone position/patient | 12 | 0.30 | 3.77 | 1.30 (0.56–1.77) | <0.0001 |
| Mean time point measurement | 12 | 0.03 | −0.55 | −0.01 (−0.08 to 0.04) | 0.58 |
| Sample size | 12 | 0.02 | −0.09 | −0.002 (−0.05 to 0.05) | 0.92 |
Abbreviation: Study size (n); Confident interval (CI); Reference (ref), Significance level <0.05.
Discussion
The effectiveness of prone positioning
This meta-analysis found that prone position significantly improved oxygenation for ARDS-related to COVID-19 for patients with invasive mechanical ventilation (traditional ICU prone positioning) and non-invasive ventilation or high-flow nasal oxygen therapy (ASPP). Based on the 15 included analytical studies of observational and experimental designs representing 288 patients with ARDS related to COVID-19, there was an increase of 50% PaO2/FiO2 before and after prone positioning. The effectiveness of prone position can also be found in the outcomes of SpO2 (pooled SMD was at 3.39) and in PaO2 (pooled SMD was at 0.77). The differences between traditional prone positioning and ASPP were not statistically significant in terms of the above-mentioned outcomes (Fig. 5 ).
Fig. 5.
Funnel plot.
Classic ARDS is commonly related to the reduction of lung compliance and severe hypoxemia. Reduction of lung compliance increases the carbon dioxide dead space calculation, meanwhile, hypoxemia occurs as a result of ventilation-to-perfusion mismatching. COVID-19-related lung injury can be managed using the same principles of lung protective ventilation strategies as those in classic ARDS (Swenson and Swenson, 2021). As a rescue therapy, the prone position significantly relieves lung compression which is squeezed by the gravity of the heart and abdominal organs in a supine position. The prone position increases the capability of the body to transfer blood and airflow more equally and improves the gas exchanges. Therefore, the dependency of the patients on supporting medical devices (i.e., ventilators) can be reduced (Hadaya and Benharash, 2020).
Moderator variables of prone positioning
Variables that moderated the pooled effect size of this meta-analysis were body mass index, duration and total time prone position. Whereas the variables of age, gender, comorbidities, patient unit, respiratory support intervention, frequency of prone position and type of ARDS showed no statistically significant differences.
There are challenges for prone position that should be considered on an individual basis, such as tolerance and lung compliance for ASPP and dislodgement of medical devices, breathing tubes, and drains for traditional ICU prone positioning (Hadaya and Benharash, 2020). Prone positioning in COVID‐19 pandemic has been adopted by healthcare professionals even for patients prior to intubation and ASPP has been included as a part of ARDS management (Guérin et al., 2020). From the subgroup analysis in this study, prone position in the group of patients with ASPP type showed a higher effect size than in the group of patients with traditional prone positioning, although the differences were not statistically significant.
The traditional prone position in the ICU showed that the main mechanisms for prone position are oxygenation improvement, drainage of respiratory secretions, stabilisation/improvement of hemodynamic and prevention of ventilator-induced lung injury (Kharat et al., 2022). Several studies showed that the traditional ICU prone position of the patients with COVID-19 ARDS had significant improvements (Abou-Arab et al., 2021, Clarke et al., 2021, Mittermaier et al., 2020, Paternoster et al., 2020, Ziehr et al., 2020). However, traditional prone position in the ICU in patients with critical illness is not without risk because of patient condition (e.g., the need for heavier sedation, hemodynamic instability, device displacement, pressure ulcers) (Binda et al., 2021).
The physiological basis behind traditional prone position patients with COVID-19 infection also applies to patients breathing spontaneously or in ASPP (Ng et al., 2020). Previous studies found that the addition of prone positioning might have contributed to the avoidance of intubation in 11 of 20 patients and that the PaO2/FiO2 ratio was significantly higher in patients who avoided intubation (Ding et al., 2020). During the COVID-19 pandemic, the use of ASPP increased in cases of hypoxemia, and evidence on the benefit of ASPP in COVID-19 was reported (Sodhi and Chanchalani, 2020). Various studies that applied ASPP to patients with COVID-19 ARDS showed a significant improvement (Caputo et al., 2020, Ding et al., 2020, Elharrar et al., 2020, Fazzini et al., 2021a, Gad, 2021, Paternoster et al., 2020, Sartini et al., 2020, Taboada et al., 2021, Taboada et al., 2020, Thompson et al., 2020, Zang et al., 2020). Evidence show that prone positioning should be applied to all patients regardless of whether they are on invasive mechanical ventilation, high-flow nasal oxygen therapy or non-invasive ventilation, as it is a simple intervention that can be done in most circumstances, and it is compatible with all forms of basic respiratory support, and requires little or no equipment in the conscious patient (Bamford et al., 2020).
However, in ASPP, besides the risk of pressure ulcer, being unable to tolerate prone position due to discomfort may lead to anxiety in these patients, and they may require light sedation (Gürün Kaya et al., 2020). Thus, in patients with ARDS related to COVID-19, specific protocols to support decisions and limit the occurrence of complications should be applied when using prone positioning in both ICU and non-ICU settings.
In terms of patient characteristics, our analysis showed a statistically significant difference in the effect of prone positioning among body mass index, as patients in the obese class II had the highest benefits compared to other levels. Anatomic and physiological alterations are observed in obese patients, affecting the face, neck, pharynx, chest wall, and lungs. In obese patients, the reduced functional residual capacity can trigger the closure of peripheral dependent airways during tidal ventilation and decreased lung compliance and these changes result in atelectasis and ventilation-perfusion mismatch and hypoxemia (De Jong et al., 2019). These effects are being decreased in the prone position which increases the relief of pressure on the diaphragm, thereby opening small airways and the dependent parts of the lungs. Generally, prone position should not be a contraindication in patients in higher obese classes, however, turning these patients may pose more procedural challenges and require an experience team to work together (Guérin et al., 2013).
Based on our analysis, significant moderators related to intervention characteristics that need to be considered are duration of prone position/day and total time prone position/patient. Our study found that duration was a statistically significant factor in prone position’s effect on outcomes, an increase in hours correlated with a larger standardised mean difference effect. Previous studies recommended that patients with severe ARDS receive prone positioning for more than 12 hours per day (Fan et al., 2017, Rahmani et al., 2020). Our study confirmed that the application of the prone position that yielded the greatest benefit were those that were done for more than 12 hours per day. Thus, prone position appears to be more advantageous in ARDS patients, and especially when applied for a longer daily duration (Munshi et al., 2017).
As the beneficial effect is linked to the length spent in prone position, it might be more beneficial to extend the sessions rather than increase the frequency of sessions for patients with invasive mechanical ventilation, as changes in body position might dislodge medical devices, breathing tubes, and drains. Also, complications during turning manoeuvres, which are rare in experienced teams, could occur more in the smaller medical centres (Hadaya and Benharash, 2020, Jochmans et al., 2020). Most of the studies done on traditional ICU prone ventilation lasted six to eight hours per day, but some used prolonged prone position lasting 12–24 hours per day (Carsetti et al., 2020, Malhotra and Kacmarek, 2020, Parker et al., 2021, Petrone et al., 2021) and showed improvement in oxygenation. Previous study showed that patients with ARDS and severe hypoxemia (PaO2/FiO2 ratio of <150 mm Hg, with an FiO2 of ≥0.6 and a positive end-expiratory pressure of ≥5 cm of water) can benefit from prone position when it is used early and in relatively long sessions (White, 2020).
However, application for ASPP should consider the tolerance of the patient and more frequent changes in position might be better than one prolonged session (Golestani-Eraghi and Mahmoodpoor, 2020). A previous meta-analysis related to the application of ASPP showed improvement in oxygenation when applied for at least four hours of repeated sessions (Fazzini et al., 2021b). Although our study found frequency/day not to be a statistically significant factor in prone position’s effect on outcomes, there was a marked increase for greater than three times/day for prone positioning. Thus, guidelines such as those from WHO for doing prone position should be followed as the previous study has also shown that patients remaining in longer prone position sessions are associated with a decrease in mortality rates (Henderson et al., 2014).
Strengths and Limitations
The main strength of this study is its applications for the practice of critical care, as this is the first meta-analysis study to show the effectiveness of traditional ICU prone positioning and ASPP on respiratory status in all patients with ARDS related to COVID-19 with subgroup analysis and meta-regression conducted for various moderating factors. In addition, a rigorous approach was taken with systematic search to include the highest available level of evidence which was prospective and experimental designs. Typically, prospective and experimental designs are ranked higher in the hierarchy of evidence than retrospective designs. However, this study has some limitations. This review was based on data from single-arm observational case series and some cohort studies that had no comparator groups. Consequently, heterogeneity was present. However, sensitivity analyses were performed to account for the heterogeneity.
Conclusions
This meta-analysis supports the effectiveness of prone position to improve oxygenation in patients with high-flow nasal oxygen therapy or non-invasive ventilation (ASPP) and those with invasive mechanical ventilation (traditional ICU prone positioning) with ARDS related to COVID-19. In additional, knowing the differences of both of these prone positioning will help nurses to optimise oxygenation and ventilation for patients. However, according to our results, patient-centred considerations such as the BMI profile, duration, and total time prone position should be taken into account when applying prone position. Nurses play important roles in implementing and monitoring the application of prone position for COVID-19 patient with ARDS as they are the ones spending the most time with patients (Butler et al., 2018). Our study results show that knowing the moderating factors such as the body mass index, duration for prone position, and total time for prone position could benefit more patients and improve outcomes. Nurses have to be responsible for applying the prone position and monitoring patients; thus, education and training are essential for nurses in the ICU and outside the ICU.
Data Statement
As this study is a meta-analysis of previous data, no new data were generated in support of this research.
Ethical statement
Not required.
CRediT authorship contribution statement
Fauzi Ashra: Conceptualization, Methodology, Formal analysis, Data curation, Writing – original draft. Ruey Chen: Validation. Xiao Linda Kang: Validation, Writing – review & editing. Kai-Jo Chiang: Validation, Writing – review & editing. Li-Chung Pien: Validation, Writing – review & editing. Hsiu-Ju Jen: Validation, Writing – review & editing. Doresses Liu: Validation, Writing – review & editing. Shu-Tai Shen Hsiao: Validation, Writing – review & editing. Kuei-Ru Chou: Conceptualization, Validation, Writing – review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
The findings and conclusions in this document are those of the authors, who are responsible for its contents.
Role of the Funding sources
The authors did not receive any specific grant or financial support from funding agencies in the public, commercial, or not-for-profit sectors for the research, authorship, and/or publication of this article.
Registration Number
The study is registered in PROSPERO (CRD42020225465).
References
- Abou-Arab O., Haye G., Beyls C., Huette P., Roger P.-A., Guilbart M., Bernasinski M., Besserve P., Trojette F., Dupont H., Jounieaux V., Mahjoub Y. Hypoxemia and prone position in mechanically ventilated COVID-19 patients: a prospective cohort study. Can. J. Anaesth. 2021;68:262–263. doi: 10.1007/s12630-020-01844-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade C. Mean difference, standardized mean difference (SMD), and their use in meta-analysis: as simple as it gets. J. Clin. Psychiatry. 2020;81:81. doi: 10.4088/JCP.20f13681. [DOI] [PubMed] [Google Scholar]
- Avdeev S.N., Nekludova G.V., Trushenko N.V., Tsareva N.A., Yaroshetskiy A.I., Kosanovic D. Lung ultrasound can predict response to the prone position in awake non-intubated patients with COVID-19 associated acute respiratory distress syndrome. Crit. Care. 2021;25:35. doi: 10.1186/s13054-021-03472-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamford P., Bentley A., Dean J., Whitmore D., Wilson-Baig N. ICS guidance for prone positioning of the conscious COVID patient 2020. Intensive Care Soc. 2020 [Google Scholar]
- Binda F., Marelli F., Galazzi A., Pascuzzo R., Adamini I., Laquintana D. Nursing management of prone positioning in patients with COVID-19. Crit. Care Nurse. 2021;41:27–35. doi: 10.4037/ccn2020222. [DOI] [PubMed] [Google Scholar]
- Bos L.D.J. COVID-19-related acute respiratory distress syndrome: Not so atypical. Am. J. Respir. Crit. Care Med. 2020;202:622–624. doi: 10.1164/rccm.202004-1423LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown S.M., Peltan I.D., Barkauskas C., Rogers A.J., Kan V., Gelijns A., Thompson B.T. What does acute respiratory distress syndrome mean during the COVID-19 pandemic? Ann. Am. Thorac. Soc. 2021;18:1948–1950. doi: 10.1513/AnnalsATS.202105-534PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler R., Monsalve M., Thomas G.W., Herman T., Segre A.M., Polgreen P.M., Suneja M. Estimating time physicians and other health care workers spend with patients in an intensive care unit using a sensor network. Am. J. Med. 2018;131:972.e9–972.e15. doi: 10.1016/j.amjmed.2018.03.015. [DOI] [PubMed] [Google Scholar]
- Caputo N.D., Strayer R.J., Levitan R., Kline J. Early self-proning in awake, non-intubated patients in the emergency department: a single ED's experience during the COVID-19 pandemic. Acad. Emerg. Med. 2020;27:375–378. doi: 10.1111/acem.13994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carsetti A., Paciarini A.D., Marini B., Pantanetti S., Adrario E., Donati A. Prolonged prone position ventilation for SARS-CoV-2 patients is feasible and effective. Crit. Care. 2020;24:1–3. doi: 10.1186/s13054-020-02956-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chad T., Sampson C. Prone positioning in conscious patients on medical wards: A review of the evidence and its relevance to patients with COVID-19 infection. Clin. Med. 2020;20:e97–e103. doi: 10.7861/clinmed.2020-0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke J., Geoghegan P., McEvoy N., Boylan M., Ní Choileáin O., Mulligan M., Hogan G., Keogh A., McElvaney O.J., McElvaney O.F., Bourke J., McNicholas B., Laffey J.G., McElvaney N.G., Curley G.F. Prone positioning improves oxygenation and lung recruitment in patients with SARS-CoV-2 acute respiratory distress syndrome; a single centre cohort study of 20 consecutive patients. BMC Res. Notes. 2021;14:20. doi: 10.1186/s13104-020-05426-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health 2020. [PubMed]
- De Jong A., Verzilli D., Jaber S. ARDS in obese patients: specificities and management. Crit. Care. 2019;23:74. doi: 10.1186/s13054-019-2374-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding L., Wang L., Ma W., He H. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Crit. Care. 2020;24:28. doi: 10.1186/s13054-020-2738-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elharrar X., Trigui Y., Dols A.-M., Touchon F., Martinez S., Prud’homme E., Papazian L. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA. 2020;323:2336–2338. doi: 10.1001/jama.2020.8255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Euser A.M., Zoccali C., Jager K.J., Dekker F.W. Cohort studies: prospective versus retrospective. Nephron. Clin. Pract. 2009;113:c214–c217. doi: 10.1159/000235241. [DOI] [PubMed] [Google Scholar]
- Fan E., Del Sorbo L., Goligher E.C., Hodgson C.L., Munshi L., Walkey A.J., Adhikari N.K.J., Amato M.B.P., Branson R., Brower R.G., Ferguson N.D., Gajic O., Gattinoni L., Hess D., Mancebo J., Meade M.O., McAuley D.F., Pesenti A., Ranieri V.M., Rubenfeld G.D., Rubin E., Seckel M., Slutsky A.S., Talmor D., Thompson B.T., Wunsch H., Uleryk E., Brozek J., Brochard L.J. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2017;195:1253–1263. doi: 10.1164/rccm.201703-0548ST. [DOI] [PubMed] [Google Scholar]
- Fazzini, B., Fowler, A.J., Zolfaghari, P. 2021a. Effectiveness of prone position in spontaneously breathing patients with COVID-19: A prospective cohort study. J. Intensive Care Soc. 1751143721996542. [DOI] [PMC free article] [PubMed]
- Fazzini B., Page A., Pearse R., Puthucheary Z. Prone position for non-intubated spontaneously breathing patients with hypoxic respiratory failure: a systematic review and meta-analysis. Br. J. Anaesth. 2021 doi: 10.1016/j.bja.2021.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrando C., Suarez-Sipmann F., Mellado-Artigas R., Hernández M., Gea A., Arruti E. Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive Care Med. 2020;46:2200–2211. doi: 10.1007/s00134-020-06192-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gad G.S. Awake prone positioning versus non invasive ventilation for COVID-19 patients with acute hypoxemic respiratory failure. Egypt. J. Anaesth. 2021;37:85–90. [Google Scholar]
- Gibson P.G., Qin L., Puah S.H. COVID-19 acute respiratory distress syndrome (ARDS): clinical features and differences from typical pre-COVID-19 ARDS. Med. J. Aust. 2020;213:54–56.e1. doi: 10.5694/mja2.50674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golestani-Eraghi M., Mahmoodpoor A. Early application of prone position for management of Covid-19 patients. J. Clin. Anesth. 2020;66:109917. doi: 10.1016/j.jclinane.2020.109917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A., et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guérin C., Albert R.K., Beitler J., Gattinoni L., Jaber S., Marini J.J., et al. Prone position in ARDS patients: why, when, how and for whom. Intensive Care Med. 2020;46:2385–2396. doi: 10.1007/s00134-020-06306-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guérin C., Reignier J., Richard J.-C., Beuret P., Gacouin A., Boulain T., et al. Prone positioning in severe acute respiratory distress syndrome. N. Engl. J. Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- Gürün Kaya A., Öz M., Erol S., Çiftçi F., Çiledağ A., Kaya A. Prone positioning in non-intubated patients with COVID-19. Tuberk Toraks. 2020;68:331–336. doi: 10.5578/tt.70164. [DOI] [PubMed] [Google Scholar]
- Hadaya J., Benharash P. Prone positioning for acute respiratory distress syndrome (ARDS) JAMA. 2020;324:1361. doi: 10.1001/jama.2020.14901. [DOI] [PubMed] [Google Scholar]
- Hasan S.S., Capstick T., Ahmed R., Kow C.S., Mazhar F., Merchant H., Zaidi S.T.R. Mortality in COVID-19 patients with acute respiratory distress syndrome and corticosteroids use: a systematic review and meta-analysis. Expert. Rev. Respir. Med. 2020;14:1149–1163. doi: 10.1080/17476348.2020.1804365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson W.R., Griesdale D.EG., Dominelli P., Ronco J.J. Does prone positioning improve oxygenation and reduce mortality in patients with acute respiratory distress syndrome? Can. Respir. J. 2014;21:213–215. doi: 10.1155/2014/472136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayakumar, D., Ramachandran, P., Rabindrarajan, E., Tirupakuzhi Vijayaraghavan, B.K., Ramakrishnan, N., Venkataraman, R. 2021. Standard care vs. awake prone position in adult non-intubated patients with acute hypoxaemic respiratory failure secondary to COVID-19 infection – A multi-centre feasibility randomized controlled trial. medRxiv. 2021.03.13.21253499.
- Jochmans S., Mazerand S., Chelly J., Pourcine F., Sy O., Thieulot-Rolin N., et al. Duration of prone position sessions: a prospective cohort study. Ann. Intensive Care. 2020;10:66. doi: 10.1186/s13613-020-00683-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kharat A., Simon M., Guérin C. Prone position in COVID 19-associated acute respiratory failure. Curr. Opin. Crit. Care. 2022;28:57–65. doi: 10.1097/MCC.0000000000000900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer T., Brioni M., Guzzardella A., Carlesso E., Cabrini L., Castelli G., et al. Prone position in intubated, mechanically ventilated patients with COVID-19: a multi-centric study of more than 1000 patients. Crit. Care. 2021;25:128. doi: 10.1186/s13054-021-03552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Ma X. Acute respiratory failure in COVID-19: is it “typical” ARDS? Crit. Care. 2020;24:198. doi: 10.1186/s13054-020-02911-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhotra, A., Kacmarek, R.M. 2020. Prone ventilation for adult patients with acute respiratory distress syndrome and Finlay G, deputy editor: UpToDate® Wolters Kluwers.
- Melsen W.G., Bootsma M.C.J., Rovers M.M., Bonten M.J.M. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin. Microbiol. Infect. 2014;20:123–129. doi: 10.1111/1469-0691.12494. [DOI] [PubMed] [Google Scholar]
- Mittermaier M., Pickerodt P., Kurth F., de Jarcy L.B., Uhrig A., Garcia C., Machleidt F., Pergantis P., Weber S., Li Y., Breitbart A., Bremer F., Knape P., Dewey M., Doellinger F., Weber-Carstens S., Slutsky A.S., Kuebler W.M., Suttorp N., Müller-Redetzky H. Evaluation of PEEP and prone positioning in early COVID-19 ARDS. EClinicalMedicine. 2020;28:100579. doi: 10.1016/j.eclinm.2020.100579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munshi L., Del Sorbo L., Adhikari N.K.J., Hodgson C.L., Wunsch H., Meade M.O., Uleryk E., Mancebo J., Pesenti A., Ranieri V.M., Fan E. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann. Am. Thorac. Soc. 2017;14(Suppl. 4):S280–S288. doi: 10.1513/AnnalsATS.201704-343OT. [DOI] [PubMed] [Google Scholar]
- Ng Z., Tay W.C., Ho C.H.B. Awake prone positioning for non-intubated oxygen dependent COVID-19 pneumonia patients. Eur. Respir. J. 2020;56(1):2001198. doi: 10.1183/13993003.01198-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öhlin A., Karlsson L., Senorski E.H., Jónasson P., Ahldén M., Baranto A., et al. Quality assessment of prospective cohort studies evaluating arthroscopic treatment for femoroacetabular impingement syndrome: a systematic review. Orthop. J. Sports Med. 2019;7 doi: 10.1177/2325967119838533. 2325967119838533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira V.M., Barcellos R.A., Piekala D.M., Moretti M.MS., Welter D.I., Candaten A.E., Cioato S.G., Machado K.C., Deponti G.N. Response to awake prone position in nonintubated individuals with COVID-19. Respiratory Care. 2022;67:48–55. doi: 10.4187/respcare.08982. [DOI] [PubMed] [Google Scholar]
- Organization W.H. World Health Organization; 2020. Clinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease is Suspected: Interim Guidance, 13 March 2020. [Google Scholar]
- Parker E.M., Bittner E.A., Berra L., Pino R.M. Efficiency of prolonged prone positioning for mechanically ventilated patients infected with COVID-19. J. Clin. Med. 2021;10:2969. doi: 10.3390/jcm10132969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paternoster G., Sartini C., Pennacchio E., Lisanti F., Landoni G., Cabrini L. Awake pronation with helmet continuous positive airway pressure for COVID-19 acute respiratory distress syndrome patients outside the ICU: A case series. Med. Intensiva (Engl. Ed.) 2020 doi: 10.1016/j.medin.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrone P., Brathwaite C.E.M., Joseph D.K. Prone ventilation as treatment of acute respiratory distress syndrome related to COVID-19. Eur. J. Trauma Emerg. Surg. 2021;47:1017–1022. doi: 10.1007/s00068-020-01542-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahmani F., Salmasi S., Rezaeifar P. Prone position effects in the treatment of Covid-19 patients. Caspian J. Intern Med. 2020;11:580–582. doi: 10.22088/cjim.11.0.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranieri V.M., Rubenfeld G.D., Thompson B.T., Ferguson N.D., Caldwell E., Fan E., et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- Reddy M.P., Subramaniam A., Afroz A., Billah B., Lim Z.J., Zubarev A., et al. Prone positioning of nonintubated patients with coronavirus disease 2019-A systematic review and meta-analysis. Crit. Care Med. 2021;49:e1001–e1014. doi: 10.1097/CCM.0000000000005086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sartini C., Tresoldi M., Scarpellini P., Tettamanti A., Carcò F., Landoni G., Zangrillo A. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA. 2020;323:2338. doi: 10.1001/jama.2020.7861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serghiou S., Goodman S.N. Random-effects meta-analysis: summarizing evidence with caveats. JAMA. 2019;321:301–302. doi: 10.1001/jama.2018.19684. [DOI] [PubMed] [Google Scholar]
- Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J. Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- Sodhi K., Chanchalani G. Awake proning: current evidence and practical considerations. Indian J. Crit. Care Med. 2020;24:1236–1241. doi: 10.5005/jp-journals-10071-23684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swenson K.E., Swenson E.R. Pathophysiology of acute respiratory distress syndrome and COVID-19 lung injury. Crit. Care Clin. 2021;37(4):749–776. doi: 10.1016/j.ccc.2021.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taboada M., González M., Álvarez A., González I., García J., Eiras M., et al. Effectiveness of prone positioning in nonintubated intensive care unit patients with moderate to severe acute respiratory distress syndrome by coronavirus disease 2019. Anesth. Analg. 2021;132:25–30. doi: 10.1213/ANE.0000000000005239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taboada M., Rodríguez N., Riveiro V., Baluja A., Atanassoff P.G. Prone positioning in awake non-ICU patients with ARDS caused by COVID-19. Anaesth. Crit. Care Pain Med. 2020;39:581–583. doi: 10.1016/j.accpm.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson A.E., Ranard B.L., Wei Y., Jelic S. Prone positioning in awake, nonintubated patients with COVID-19 hypoxemic respiratory failure. JAMA Intern. Med. 2020;180:1537–1539. doi: 10.1001/jamainternmed.2020.3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venus K., Munshi L., Fralick M. Prone positioning for patients with hypoxic respiratory failure related to COVID-19. CMAJ. 2020;192:E1532–E1537. doi: 10.1503/cmaj.201201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White M. Proning for ARDS makes a comeback. Nursing. 2020;35:32cc1–32cc2. [Google Scholar]
- Zang X., Wang Q., Zhou H., Liu S., Xue X. Efficacy of early prone position for COVID-19 patients with severe hypoxia: a single-center prospective cohort study. Intensive Care Med. 2020;46:1927–1929. doi: 10.1007/s00134-020-06182-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziehr D.R., Alladina J., Petri C.R., Maley J.H., Moskowitz A., Medoff B.D., et al. Respiratory pathophysiology of mechanically ventilated patients with COVID-19: A cohort study. Am. J. Respir. Crit. Care Med. 2020;201:1560–1564. doi: 10.1164/rccm.202004-1163LE. [DOI] [PMC free article] [PubMed] [Google Scholar]