Abstract
There are many risk factors associated with the spread of the COVID-19 pandemic, including low wind speed, fossil fuel energy production, air pollution, and smoking. Several studies argue that smoking is not a risk factor for COVID-19 morbidity among males or any other sub-group. The study aims to analyze the following research questions: (1) can smoking prevalence explain COVID-19 indicators (cases, mortality, and recovery)? Are these relationships monotonically increasing or decreasing? In an attempt to test the counter-intuitive possibility of a non-linear relationship, the proposed empirical model relaxes the assumption of monotonic change by applying the quadratic design and testing which one of the two competing models (quadratic or linear) better fits the data. Findings suggest more complex relationships between corona indices and prevalence of smoking than previously thought. These patterns might be explained by several conditions such as the attenuation of hypercytokinemia for mild levels of smoking prevalence compared with non-smokers, elevated social distancing of smokers in countries with lower smoking prevalence, and unidentified factors that should be examined in future research.
Keywords: COVID-19, Smoking Prevalence, ACE2 receptor, Hypercytokinemia, OECD
Introduction
COVID-19 is a global pandemic with an accumulated death toll of 6.328 million persons worldwide (Worldmeter 2022; available at https://www.worldometers.info/coronavirus/). There are many risk factors associated with the spread of the COVID-19 pandemic, including (1) environmental factors: low wind speed and fossil fuel energy production (Coccia 2020; Coccia 2021a); (2) urban and political structure: high population size and/or worse public governance, promoting lower expenditures in health system (Arbel et al. 2022; Coccia 2022); (3) professions: police officers (De Santi et al. 2021); and (4) medical factors: older age cohorts (García-Esquinas et al. 2021), cardio-vascular diseases (De Santi et al. 2021), obesity (Yanover et al. 2020), first vs. second wave (Coccia 2021b), and smoking (De Santi et al. 2021).1
The tobacco epidemic is one of the biggest public health threats the world has ever faced, killing more than 8 million people a year around the world (World Health Organization (WHO) 2020c). With the outburst of the COVID-19 pandemic (World Health Organization (WHO) 2020a; Wu and McGoogan 2020), several researchers identified smoking as one of the serious risk factors causing coronavirus-related complications.2 Smoking is also strongly associated with respiratory diseases such as bronchitis (Balte et al. 2020). Yet, two recent studies found an underrepresentation of current smokers among coronavirus patients in China, only 1.4% (Zhang et al. 2020) and 16.9% among severe patients (Guan et al. 2020), compared with the 50.5% prevalence of smokers among the overall adult Chinese population. Moreover, the current literature does not support smoking as a predisposing factor in men or any subgroup for infection with SARS-CoV-2. Also, differences in COVID-19 disease prevalence and severity are associated with differences of expression of ACE2 receptor in smokers, responsible for severe acute respiratory syndrome coronavirus (Cai 2020).
Indeed, there is a debate in the literature over whether current smoking increase individuals’ risk of developing symptomatic COVID-19. On the one hand, Hopkinson et al. (2021) support the conclusion that smoking increases individual risk from COVID-19 in England. Based on information from the UCLA hospital, Monteiro et al. (2020) suggest that obesity, smoking history, and elevated inflammatory markers were associated with increased need for IMV (intermittent mandatory ventilation) in patients with COVID-19. Rosoff et al. (2021) provide strong genetic evidence in support of smoking as a risk factor of COVID-19 and suggest that prevention programs aimed at reducing smoking may be important for the COVID-19 pandemic and have substantial public health benefits.
On the other hand, based on meta-analysis of China and US studies, Farsalinos et al. (2021) mention the unusually low prevalence of smokers (approximately 1/4th the expected prevalence) among hospitalized COVID-19 patients. The authors conclude that pharmaceutical nicotine or other nicotinic cholinergic agonists should be explored as potential therapeutic options, based on a recently presented hypothesis.3 According to Yanover et al. (2020), and based on reports from Israeli hospitals, there is no statistical evidence in support of the null hypothesis that smoking and respiratory diseases are associated with COVID-19 complications. Finally, De Santi et al. (2021) demonstrated that smoking habit is associated with only 33.56% chance of infection from SARS-CoV2 (see footnote 1).
Another strand of the literature investigated the impact of COVID-19 lockdowns on prevalence of smoking and smoking cessation. Jackson et al. (2022) demonstrated that in England, the first COVID-19 lockdown was associated with increased smoking prevalence among younger adults and increased high-risk drinking prevalence among all adults. Smoking cessation activity also increased: more younger smokers made quit attempts during lockdown and more smokers quit successfully.
The objective of the current study is to address the following research questions: (1) can smoking prevalence explain COVID-19 indicators (cases, mortality, and recovery)? Are these relationships monotonically increasing or decreasing?4 The collected indicators are updated to April 28, 2020, and include number of corona infections, number of severe cases of illness from corona, number of recovered cases from corona, the number of deaths from corona, coronavirus as the cause of death (percent of the total number of deaths), and the population of the country as of July 2019. The Organization for Economic Cooperation and Development (OECD Report 2020) issued a report, which specifies for each member country the prevalence of smoking among the population between 1960 and 2020 (available at https://data.oecd.org/healthrisk/daily-smokers.htm).
In an attempt to test the counter-intuitive possibility of a non-linear relationship between the prevalence of smoking and coronavirus indicators, the empirical model in the study relaxes the assumption of monotonic change by applying the quadratic design and testing which one of the two competing models (quadratic or linear) better fits the data. To the best of our knowledge, this possibility has not been examined previously in the context of smoking patterns and COVID-19.
In line with Lombardi et al. (2021), results indicate more complex relationships between corona indices and the prevalence of smoking than previously considered. Indeed, as anticipated, there is a linear increase of projected mortality rate from corona and corona as the cause of death with an elevated prevalence of smoking. Nevertheless, other projected indicators, such as the number of infected per 100,000 persons, rates of severe corona cases, and rates of recovered corona patients, exhibit quadratic, rather than linear, patterns. The reasons for these non-linear patterns might be explained by several conditions such as attenuation of hypercytokinemia for mild levels of smoking prevalence compared with non-smokers, which offsets the lack of sufficient lung reserves in heavy smokers, elevated social distancing of smokers in countries with lower smoking prevalence, and unidentified factors that should be examined in future research.
The remainder of the article is organized as follows. The “Material and methods” section portrays the methodology and the “Results and discussion” section presents the results. Finally, the “Conclusions” section concludes and summarizes.
Material and methods
Sample and data
The Organization for Economic Cooperation and Development (OECD Report 2020) issued a report, which specifies for each member country the prevalence of smoking among the population between 1960 and 2020 (available at https://data.oecd.org/healthrisk/daily-smokers.htm).
The collected COVID-19 indicators are updated to April 28, 2020, and include number of corona infections, number of severe cases of illness from corona, number of recovered cases from corona, the number of deaths from corona, and coronavirus as the cause of death (percent of the total number of deaths). To normalize these indicators based on the population of the country we used information from July 2019 (on the eve of COVID-19 pandemic outburst).
Measures of variables
Table 1 provides the descriptive statistics of all the normalized variables latter incorporated in the regression models. INFECTED are Corona cases per 100,000 persons. SEVERE are severe divided by total corona cases. RECOVERED are recovered divided by total corona cases. CAUSE OF DEATH indicates the ratio between the number of deaths from corona divided by total number of deaths in the country. MORTALITY RATE is the ratio between number of dead and infected cases from corona. SMOKERS is the prevalence of smokers in OECD countries.
Table 1.
Descriptive statistics
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Descriptive statistics | INFECTED | SEVERE | RECOVERED | CAUSE OF DEATH | MORTALITY RATE |
| Average | 146.76 | 1.33 | 41.09 | 6.01 | 8.81 |
| Median | 29.06 | 0.99 | 31.94 | 4.07 | 2.20 |
| SD | 221.27 | 0.87 | 23.44 | 4.57 | 11.06 |
| Min | 10.73 (IND) | 0.07 (LUX) | 5.71 (MEX) | 1.24 (AUS) | 0.1 (IND) |
| Max | 1,275.58 (MEX) | 3.08 (CHE) | 83.75 (ISR) | 15.49 (BEL) | 43 (BEL) |
| SMOKERS | SMOKERS | SMOKERS | SMOKERS | SMOKERS | |
| Average | 26.34 | 26.34 | 26.37 | 26.34 | 26.26 |
| Median | 24.3 | 24.3 | 24.5 | 24.3 | 24.1 |
| SD | 10.94 | 10.94 | 11.19 | 10.94 | 11.17 |
| Min | 7.2 (BRAZIL) | 7.2 (BRAZIL) | 7.2 (BRAZIL) | 7.2 (BRAZIL) | 7.2 (BRAZIL) |
| Max | 57.5 (DNK) | 57.5 (DNK) | 57.5 (DNK) | 57.5 (DNK) | 57.5 (DNK) |
| Observations | 490 | 490 | 461 | 490 | 426 |
Notes: INFECTED are corona cases per 100,000 persons. SEVERE are severe divided by total corona cases. RECOVERED are recovered divided by total corona cases. CAUSE OF DEATH indicates the ratio between the number of deaths from corona divided by total number of deaths in the country. MORTALITY RATE is the ratio between number of dead and infected cases from corona. SMOKERS is the prevalence of smokers in OECD countries
The mean prevalence of smokers among the OECD countries is 26.26–26.37% and the median is 24.1–24.5%. The implication is that the distribution is right-tailed and the modal prevalence is lower than the median. While Brazil exhibits the minimum prevalence of 7.2%, Denmark exhibits the maximum prevalence of 57.5% (SMOKERS). Further regression outcomes (available upon request) demonstrate that in 1960, the projected prevalence of smokers in OECD countries is 52.27%. This percent steadily drops by 0.6479% per annum. The 99% confidence interval is 0.6043–0.6915% annual drop. Consequently, this percent is anticipated to drop to 13.40 percent in 2020.
Models and data analysis procedure
Consider the following two competing empirical models:
| 1 |
| 2 |
where j = 1,2,3,4,5; ; ; ; Y4 = CORONA (the cause of death from the total number of dead persons); ; SMOKERS is the prevalence of smokers among the population; α1j, α2j, α3j and β1j, β2j are the parameters; and u1j, u2j are the stochastic random disturbance terms. All of these models are estimated via regression analyses based on the Ordinary-Least-Square (OLS) procedure, the conventional methodology to identify correlations between variables. Unlike Eq. (2), Eq. (1) permits non-monotonic change of the corona indicator with the SMOKERS variable.
To test which of these two models better fits the data for each indicator, the Ramsey RESET test is employed (e.g., Ramanathan 2002, pp. 270–271). The test is based on estimating the models: , where ; j = 1,2,3,4,5; X = SMOKERS; H0: cj = 0; and H1: cj ≠ 0. Rejection of the null hypothesis suggests that compared to the linear model, the quadratic model fits the data better.
Results and discussion
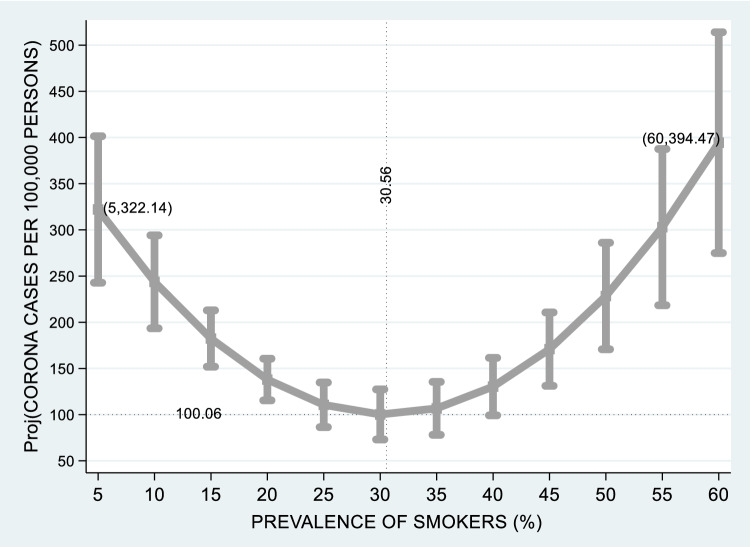
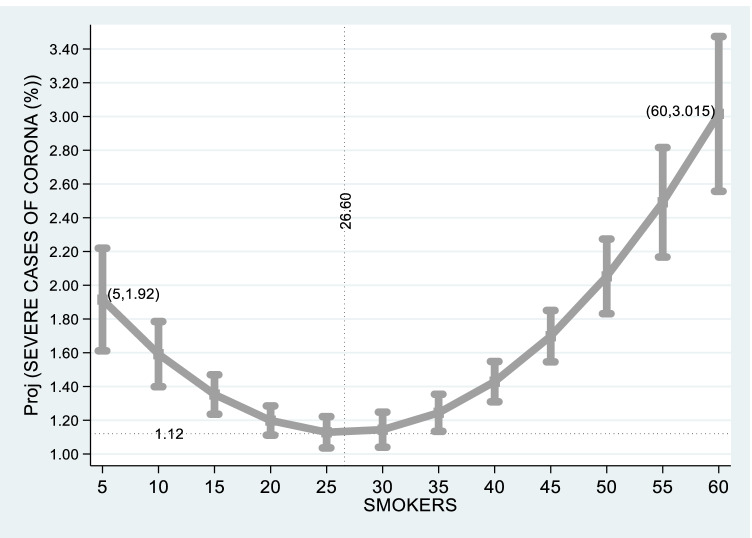
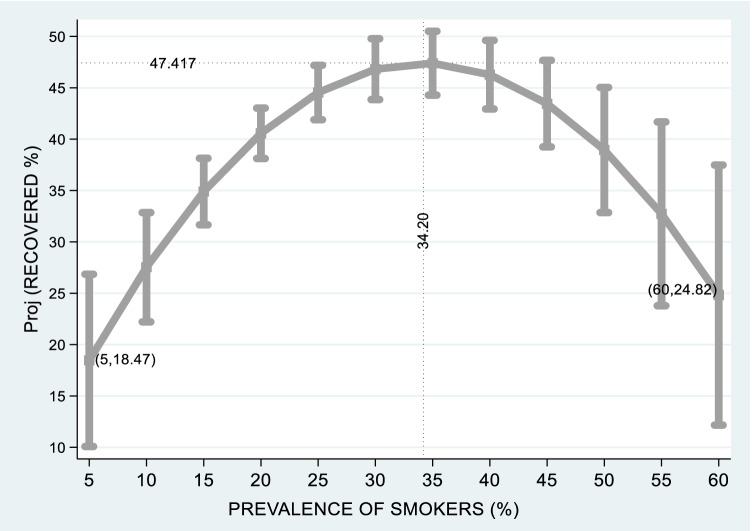
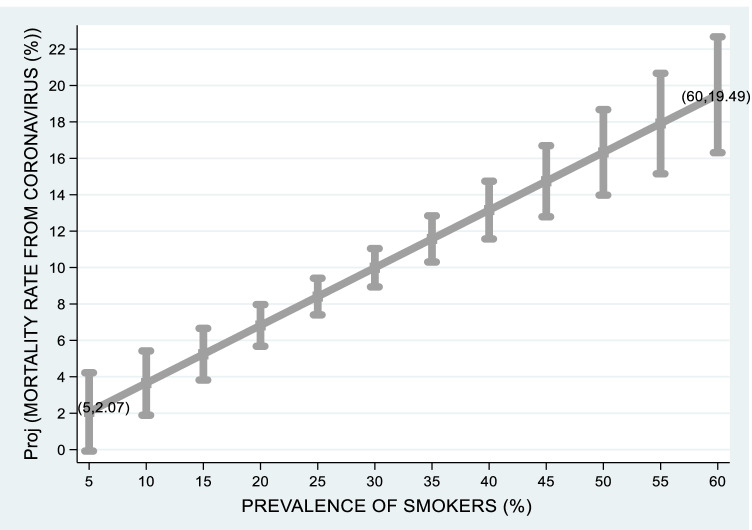
Table 2 provides the regression outcomes. Based on these regressions, Figures 1 and 2 are based on projections obtained from regression outcomes reported in columns (1) and (2) of Table 2 and 95% confidence intervals. Appendices Figure 3 and 4 are based on projections obtained from regression outcomes reported in columns (3) and (5) of Table 2 and 95% confidence intervals.
Table 2.
Regression outcomes
| Variables | (1) | (2) | (3) | (4) | (5) |
|---|---|---|---|---|---|
| INFECTED | SEVERE | RECOVERED | CAUSE OF DEATH | MORTALITY RATE | |
| SMOKERS | −20.77*** (1.27 × 10−6) | −0.0902*** (4.57 × 10−8) | 2.322*** (3.80×10−7) | 0.128*** (<0.001) | 0.317*** (<0.001) |
| SMOKERS2 | 0.340*** (1.03 × 10−6) | 0.00169*** (2.86 × 10−10) | −0.0340*** (4.42 × 10−6) | - | - |
| Constant | 417.5*** (<0.001) | 2.324*** (<0.001) | 7.702 (0.218) | 2.648*** (3.65×10−7) | 0.486 (0.708) |
| Observations | 490 | 490 | 461 | 490 | 426 |
| R-squared | 0.048 | 0.099 | 0.062 | 0.093 | 0.102 |
| Calculated F-value | 12.30*** | 26.88*** | 15.02*** | 50.28*** | 24.71*** |
| D.F. numerator | 2 | 2 | 2 | 1 | 1 |
| D.F. denominator | 487 (5.85 × 10−6) | 487 (7.61 × 10−12) | 458 (4.51 × 10−7) | 488 (2.17 × 10−12) | 424 (4.75 × 10−7) |
| RESET test | 24.50*** (<0.001) | 41.48*** (<0.001) | 21.59*** (<0.001) | 0.89 (0.3464) | 1.08 (0.2989) |
Notes: Corona indicators are based on information published on April 28, 2020 for OECD countries. INFECTED are corona cases per 100,000 persons. SEVERE are severe divided by total corona cases. RECOVERED are recovered divided by total corona cases. CAUSE OF DEATH indicates the ratio between the number of deaths from corona divided by total number of deaths in the country. MORTALITY RATE is the ratio between number of dead and infected cases from corona. The p-values are given in parentheses: *p < 0.05, **p < 0.01, ***p < 0.001
Fig. 1.
Projected corona cases per 100,000 persons vs. prevalence of smokers
Fig. 2.
Projected rate of severe corona patients vs. prevalence of smokers. Note that Figs. 1 and 2 are based on projections obtained from regression outcomes reported in columns (1) and (2) of Table 2 and 95% confidence intervals
Fig. 3.
Projected rate of recovered corona patients vs. prevalence of smokers
Fig. 4.
Projected mortality rate from coronavirus vs. prevalence of smokers. Note that Appendices A and B are based on projections obtained from regression outcomes reported in columns (3) and (5) of Table 2 and 95% confidence intervals
Figure 1 displays the projected number of corona cases per 100,000 persons vs. the prevalence of smokers in OECD countries. Based on column (1) in Table 1, the RESET test supports the quadratic model in favor of the linear model. The figure demonstrates that at the 5–30.56% prevalence of smokers, projected corona cases per 100,000 persons drop from 322 to 100 cases. At the 30.56–60% prevalence of smokers, projected corona cases per 100,000 persons rise from 100 to 394 cases.
Figure 2 reports the projected rate of severe corona patients vs. the prevalence of smokers in OECD countries. Based on column (2) in Table 1, the RESET test supports the quadratic model in favor of the linear model. The figure demonstrates that at the 5–26.6% prevalence of smokers, the projected rate of severe corona patients drops from 1.92 to 1.12%. At the 26.6–60% prevalence of smokers, the projected rate of severe corona patients rises from 1.12 to 3.015%.
Appendix Figure 3 reports the projected rate of recovered corona patients vs. the prevalence of smokers in OECD countries. Based on column (3) in Table 1, the RESET test supports the quadratic model in favor of the linear model. The figure demonstrates that at the 5–34.20% prevalence of smokers, the projected rate of recovered corona patients rises from 18.47 to 47.417%. At the 34.20–60% prevalence of smokers, the projected rate of recovered corona patients drops from 47.47 to 24.82%.
Finally, Appendix Figure 4 reports the projected mortality rate from coronavirus vs. the prevalence of smokers in OECD countries. Based on column (5) in Table 1, the RESET test supports the linear model in favor of the quadratic model. The figure demonstrates a steady rise from a mortality rate of 2.07%, where 5% of the population are smokers to 19.49%, where 60% of the population are smokers.
Smoking is considered by the WHO as one of the biggest public health threats the world has ever faced, killing more than 8 million people a year, and causing respiratory illness, such as bronchitis (World Health Organization (WHO) 2020c; Balte et al. 2020). Coronavirus disease 2019 (COVID-19) is a declared global pandemic and is considered as a respiratory illness (World Health Organization (WHO) 2020a; Wu and McGoogan 2020). Consequently, given that (1) the act of smoking means that fingers (and possibly contaminated cigarettes) are in contact with lips which increases the possibility of transmission of virus from hand to mouth and (2) the lack of sufficient lung reserves among heavy smokers; smoking is considered a serious risk factor for both coronavirus disease infection and complications (World Health Organization (WHO) 2020b: Are smokers and tobacco users at higher risk of COVID-19 infection?). Yet, recent studies found a significantly lower prevalence of smokers in China among corona patients compared with the high prevalence of smokers in the total population (e.g., Guan et al. 2020; Zhang et al. 2020). Moreover, the current literature does not support smoking as a predisposing factor in men or any subgroup for infection with SARS-CoV-2. Also, differences in COVID-19 disease prevalence and severity are associated with differences of expression of ACE2 receptor, responsible for severe acute respiratory syndrome coronavirus (Cai 2020).
The objective of the current study is to analyze the potential relationships between different corona indicators and smoking prevalence on a statewide level, based on an OECD report. To test the counter-intuitive possibility of non-linear relationship, the proposed empirical model relaxes the assumption of monotonic change by applying the quadratic design and testing which one of the two competing models (quadratic or linear) better fits the data.
Conclusions
This section concludes and summarizes the manuscript. Findings of this article suggest more complex relationships between corona indices and prevalence of smoking than previously thought. Indeed, as anticipated, there is a linear increase of the projected mortality rate from corona and corona as the cause of death with an elevated prevalence of smoking. Nevertheless, other projected indicators, such as the number of infected per 100,000 persons, rates of severe corona cases, and rates of recovered corona patients, exhibit quadratic, rather than linear, patterns. The reasons for these non-linear patterns might be explained by several conditions such as attenuation of hypercytokinemia for mild levels of smoking prevalence compared with non-smokers, which offsets the lack of sufficient lung reserves in heavy smokers, elevated social distancing of smokers in countries with lower smoking prevalence, and unidentified factors that should be examined in future research.
The short-run public policy repercussions would be warning of the public by publicity campaigns to avoid crowding and reduce the exit from home in the face of the pandemic. If possible, the public should be encouraged to relocate on countryside regions with reduced levels of pollution.
The long-run public policy repercussions of our study are the following. In countries with high smoking prevalence, it would be of great importance to convince the public of smokers to quit smoking or at least reduce the consumption of cigarettes. This recommendation is strengthened following our findings, indicating a monotonic increase of COVID-19 mortality with smoking prevalence.
The limitation of our study includes the potential supplement of control variables, such as the level of pollution in each OECD country. If the pollution variance in OECD countries is high, this might lead to biased coefficients. This should be the subject of future studies.
Acknowledgements
The authors are grateful to Yifat Arbel, Nissim Ben David (the President), and the participants at the “light at the corona tunnel” zoom meeting in Western Galilee College for the helpful comments.
Abbreviations
- ACE2
angiotensin-converting enzyme 2
- OECD
Organization for Economic Co-operation and Development
Appendix
Author contribution
Yuval Arbel contributed to the study conception and design, data collection and analysis, the first draft, and comments on previous versions of the manuscript.
Chaim Fialkoff contributed to the study conception and design, data collection and analysis, the first draft, and comments on previous versions of the manuscript.
Amichai Kerner contributed to the study conception and design, data collection and analysis, the first draft, and comments on previous versions of the manuscript.
Miryam Kerner contributed to the study conception and design, data collection and analysis, the first draft, and comments on previous versions of the manuscript.
Availability of data and materials
This research is based on information downloaded from OECD website. After acceptance of the manuscript, full Information and replication instructions in Stata software package will be given upon request.
Declarations
Ethics approval and consent to participate
This research does not require an IRB approval since it does not involve any experiment or manipulation of subjects. All authors read and approved the final manuscript for submission.
Consent for publication
All authors agreed to submit to Environmental Science and Pollution Research.
Competing interests
The authors declare no competing interests.
Footnotes
According to the World Health Organization (WHO) (2020b): “Smokers are likely to be more vulnerable to COVID-19 as the act of smoking means that fingers (and possibly contaminated cigarettes) are in contact with lips which increases the possibility of transmission of virus from hand to mouth. Smokers may also already have lung disease or reduced lung capacity which would greatly increase risk of serious illness.”
Yet, this conclusion should not be interpreted as a supporting view in favor of smoking. The authors explicitly states that smokers should be advised to quit due to long-term health risks.
For the development of models of inquiry in the philosophy of science, see, for example, Coccia (2018).
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yuval Arbel, Email: YuvalAr@wgalil.ac.il, Email: yuval.arbel@gmail.com.
Chaim Fialkoff, Email: cfialk@gmail.com.
Amichai Kerner, Email: kerneram@netvision.net.il.
Miryam Kerner, Email: kerneram@technion.ac.il.
References
- Arbel Y, Arbel Y, Kerner A, Kerner M (2022) Can the regime type (Democracy versus Autocracy) explain the covid-19 recovery rates? Chin Polit Sci Rev. Available at: 10.1007/s41111-022-00218-4
- Balte PP, Chaves PH, Couper DJ, et al. Association of nonobstructive chronic bronchitis with respiratory health outcomes in adults. JAMA Intern Med. 2020;180(5):676–686. doi: 10.1001/jamainternmed.2020.0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai H (2020). Sex difference and smoking predisposition in patients with COVID-19 https://www.thelancet.com/respiratory Vol 8. Available at: 10.1016/S2213-2600(20)30117-X. Accessed 10 June 2022 [DOI] [PMC free article] [PubMed]
- Coccia M. An introduction to the methods of inquiry in social sciences. J Soc Adm Sci. 2018;5(2):116–126. doi: 10.1453/jsas.v5i2.1651. [DOI] [Google Scholar]
- Coccia M. How (un) sustainable environments are related to the diffusion of COVID-19: the relation between coronavirus disease 2019, air pollution, wind resource and energy. Sustainability. 2020;12:9709. doi: 10.3390/su12229709. [DOI] [Google Scholar]
- Coccia M. High health expenditures and low exposure of population to air pollution as critical factors that can reduce fatality rate in COVID-19 pandemic crisis: a global analysis. Environ Res. 2021;199:111339. doi: 10.1016/j.envres.2021.111339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. The impact of first and second wave of the COVID-19 pandemic in society: comparative analysis to support control measures to cope with negative effects of future infectious diseases. Environ Res. 2021;197:111099. doi: 10.1016/j.envres.2021.111099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. Preparedness of countries to face COVID-19 pandemic crisis: strategic positioning and factors supporting effective strategies of prevention of pandemic threats. Environ Res. 2022;203:111678. doi: 10.1016/j.envres.2021.111678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Santi M, Diotallevi A, Brandi G. Seroprevalence of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection in an Italian cohort in Marche Region, Italy. Acta Bio-Medica : Atenei Parmensis. 2021;92(1):e2021070. doi: 10.23750/abm.v92i1.10847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farsalinos K, Bagos PG, Giannouchos T, Niaura R, Barbouni A, Poulas K. Smoking prevalence among hospitalized COVID-19 patients and its association with disease severity and mortality: an expanded re-analysis of a recent publication. Harm Reduct J. 2021;18(1):1–9. doi: 10.1186/s12954-020-00437-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Esquinas E, Ortolá R, Gine-Vázquez I, Carnicero JA, Mañas A, Lara E, Alvarez-Bustos A, Vicente-Rodriguez G, Sotos-Prieto M, Olaya B, Garcia-Garcia FJ, Gusi N, Banegas JR, Rodríguez-Gómez I, Struijk EA, Martínez-Gómez D, Lana A, María HJ, Ayuso-Mateos JL, et al. Changes in health behaviors, mental and physical health among older adults under severe lockdown restrictions during the COVID-19 pandemic in Spain. Int J Environ Res Public Health. 2021;18:7067. doi: 10.3390/ijerph18137067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W, Ni Z, Liang W et al (2020) Clinical characteristics of coronavirus disease 2019 in China. New England J Med ; published online Feb 28, 2020. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed]
- Hopkinson NS, Rossi N, El-Sayed Moustafa J, Laverty AA, Quint JK, Freidin M, Visconti A, Murray B, Modat M, Ourselin S, Small K, Davies R, Wolf J, Spector TD, Steves CJ, Falchi M. Current smoking and COVID-19 risk: results from a population symptom app in over 2.4 million people. Thorax. 2021;76(7):714–722. doi: 10.1136/thoraxjnl-2020-216422. [DOI] [PubMed] [Google Scholar]
- Jackson SE, Beard E, Angus C, Field M, Brown J. Moderators of changes in smoking, drinking and quitting behaviour associated with the first COVID-19 lockdown in England. Addiction. 2022;117(3):772–783. doi: 10.1111/add.15656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardi C, Roca E, Ventura L, Cottini M. Smoking and COVID-19, the paradox to discover: an Italian retrospective, observational study in hospitalized and non-hospitalized patients. Med Hypotheses. 2021;146:110391. doi: 10.1016/j.mehy.2020.110391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteiro AC, Suri R, Emeruwa IO, Stretch RJ, Cortes-Lopez RY, Sherman A, Lindsay CC, Fulcher JA, Goodman-Meza D, Sapru A, Buhr RG, Chang SY, Wang T, Qadir N. Obesity and smoking as risk factors for invasive mechanical ventilation in COVID-19: a retrospective, observational cohort study. PLoS One. 2020;15(12):1–13. doi: 10.1371/journal.pone.0238552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD Report (2020) available at: https://data.oecd.org/healthrisk/daily-smokers.htm (Last accessed on May 15, 2020).
- Ramanathan R. Introductory econometrics with applications. 5. South-Western: Thomson Learning; 2002. [Google Scholar]
- Rosoff DB, Yoo J, Lohoff FW. Smoking is significantly associated with increased risk of COVID-19 and other respiratory infections. Commun Biol. 2021;4(1):1–11. doi: 10.1038/s42003-021-02685-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) (2020a): Coronavirus. Available at: https://www.who.int/health-topics/coronavirus#tab=tab_1 and https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (Last accessed on May 15, 2020).
- World Health Organization (WHO) (2020b) : Q&A: Smoking and COVID-19: are smokers and tobacco users at higher risk of COVID-19 infection? Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-on-smoking-and-covid-19 (Last accessed on May 15, 2020).
- World Health Organization (WHO) (2020c) : Tobacco: Key Facts. Available at: https://www.who.int/news-room/fact-sheets/detail/tobacco (Last accessed on May 15, 2020).
- Worldmeter (2022) available at: https://www.worldometers.info/coronavirus/. Accessed 10 June 2022
- Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center For Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- Yanover C, Mizrahi B, Kalkstein N, Marcus K, Akiva P, Barer Y, Shalev V, Chodick G. What factors increase the risk of complications in SARS-CoV-2-infected patients? A Cohort Study in a Nationwide Israeli Health Organization. JMIR Public Health Surveill. 2020;6(3):e20872. doi: 10.2196/20872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang JJ, Dong X, Cao Y et al (2020) Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy ; published online Feb19, 2020. 10.1111/all.14238 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This research is based on information downloaded from OECD website. After acceptance of the manuscript, full Information and replication instructions in Stata software package will be given upon request.