Abstract
Background
Adolescent pregnancy is a public health issue with well-defined causes and health risks with social and economic implications. Aim of this review was to examine adverse pregnancy outcomes and risk factors associated with adolescent pregnancy in Africa.
Method
PubMed Central, Science Direct and JSTOR were the main databases for the literature review. Other online sources and experts were consulted for relevant studies. In all, 11,574 records were identified and 122 were considered as full-text studies for evaluation after thorough screening and removal of duplicates. Finally, 53 studies were included in this review for thematic synthesis.
Results
The 53 studies sampled 263,580 pregnant women, including 46,202 adolescents (< 20 years) and 217,378 adults (> 20 years). Adolescent pregnancy was associated with higher risks of adverse pregnancy outcomes. Factors of poor pregnancy outcomes included low socioeconomic and educational status, poor utilization of antenatal care, risky lifestyles such as alcohol consumption, and unattractive health care factors. Maternal health care utilization was identified as an important factor to improve pregnancy outcomes among adolescents in Africa.
Conclusion
To prevent adolescent pregnancy, stakeholders need to help lower socioeconomic inequalities, poor utilization of antenatal care, alcohol consumption, and improve adolescents’ health care and their educational status. Issues such as child marriage, abortion, poor health care infrastructure and non-adolescent friendly health facilities need to be addressed.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-022-04821-w.
Keywords: Adolescent pregnancy, Adverse pregnancy outcomes, Risk factors, Africa
Background
The stage of adolescence, ages between 10 and 19, is critical and must be a concern to every person, parents, schools and governments [1]. They account for approximately 16% (1.2 billion) of the global population [1]. In 2015 alone, approximately 1.3 million adolescents died worldwide, resulting in approximately 3561 deaths per day [2]. It is worth noting that two-thirds of these deaths occurred in low-income countries [2]. Every year, approximately 21 million adolescent girls become pregnant in low-income countries, with approximately 12 million of them giving birth [3]. Furthermore, 2.5 million adolescent girls under the age of 16 give birth each year in these countries [4]. Recent data suggest that approximately 777,000 adolescent girls under the age of 15 give birth each year at a rate of 43 births per 1000 girls globally [5]. This requires provision of quality education, health care and well-being opportunities for all citizens as well as to ensure healthy lives and well-being for all at all ages [6].
Complications of pregnancy, childbirth and abortion are the leading causes of death among adolescent girls [5]. High prevalence of hypertensive disorders, low birth weight and preterm birth in adolescent pregnancies have been reported in studies from both high and low-income countries [7]. Adolescents are more likely to have unwanted pregnancies, and those who become pregnant are typically from low-income families, are less educated and live in rural areas [1, 2, 4, 7, 8]. The relationship between adverse pregnancy outcomes and adolescent pregnancy has been a source of debate, whether adverse pregnancy outcomes in adolescents are caused by age, a risky lifestyle, lack of access to maternal health care, pre-existing health conditions or adolescents’ poor socioeconomic and demographic status [7, 9–11]. The prevalence of adverse perinatal outcomes such as low birth weight (LBW) and preterm birth also vary significantly across geographical areas [10, 12].
This scoping review included studies that looked at sub-group risk factors and adolescent pregnancy outcomes. Furthermore, due to geographical variations in pregnancy outcomes, this scoping review focused on Africa, which has the highest prevalence of teen pregnancy globally, with approximately 28% of girls in West and Central Africa and about 25% in Southern and Eastern Africa giving birth before the age of 18 [13]. Even though recent reviews on adolescent pregnancy and its related adverse obstetric and neonatal outcomes have included a few studies from Africa, they did not review evidence on risk factors that predispose adolescents to adverse pregnancy outcomes [7, 14]. This scoping review aimed at examining whether childbearing before age 20 in Africa is associated with increased adverse maternal and neonatal outcomes. The review also explored evidence regarding risk factors associated with adverse pregnancy outcomes.
Methods
This scoping review was based on the guidelines of Arksey and O’Malley [15]. We also applied the preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews (PRISMA-ScR) checklist [16]. The research questions included: (1) what are the adverse obstetric and perinatal/neonatal outcomes associated with adolescent childbirth in Africa? and (2) what are the risk factors associated with adverse pregnancy outcomes among adolescents in Africa?
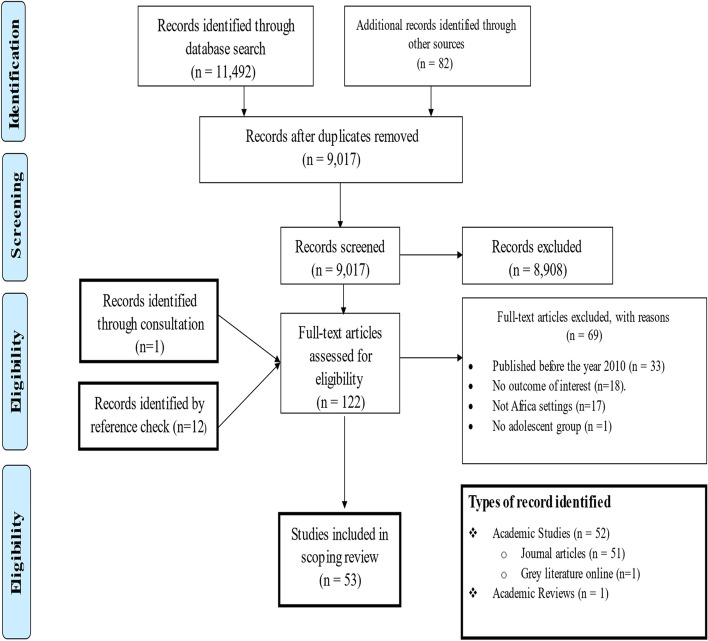
We included literature that reported adolescents’ adverse pregnancy outcomes and associated risk factors which were published in English between January 2010 and 31st of August, 2021 from Africa. We included published articles and grey literature [dissertations] and other studies during the screening process. An initial search was carried out in Google Scholar with search terms: “Adolescent pregnancy” OR “adverse outcomes” OR “risk factors” OR “Africa” and yielded 67.800 results. Search terms were refined in January 2021 from academic databases and online search engines (i.e., PubMed Central, Science Direct, JSTOR, The WHO Library, Maternal Surveillance and Response Action Network, Google Scholar, Google, Z-library and Sci-Hub). The last search was done on August 31st, 2021. We also consulted a content expert and a chartered librarian throughout the process of writing this paper. Details of search and screening results are summarized in Table 1 and presented graphically in Fig. 1 using the PRISMA flow diagram.
Table 1.
Search strategy
| Items | Search Strategy |
|---|---|
| Database | PubMed, CENTRAL, Science direct, JSTOR, The WHO library, Maternal Surveillance and Response Action Network Google Scholar, Google, Z-library and Sci-Hub. |
| Language filter | 2010 and later |
| Spatial filter | Africa OR Sub-Saharan Africa |
| Keywords | 1. “Adolescents” OR “Adolescent” OR “Adolescence” OR “Teenage” OR “Teen” OR “Teens” OR “Youth” OR “Youths” OR “Girl” OR “Girls”. |
| 2. “Pregnancy” OR “Childbearing” OR “Pregnancies” OR “Pregnant” OR “Childbirth” OR “Childbirth” OR “Birth” OR “Births”. | |
| 3. “Maternal Mortality” OR “Maternal death” OR “Maternal deaths” OR “Perinatal deaths” OR “Neonatal deaths” OR “Perinatal death” OR “Neonatal death” OR “Low birth Weight” OR “Eclampsia” OR “Preeclampsia” OR “Preterm” OR “Premature” OR “Small-for gestational age” OR “Stillbirth” OR “Premature rapture of membrane” OR “Postpartum hemorrhage” OR “Antepartum hemorrhage” OR “Sepsis” OR “Gestational diabetes” OR “Gestational anemia” OR “Apgar score” OR “Cesarean section” OR “Hospital admission” OR “Fetal infections” OR “Prolonged labor” OR “Fetal distress” OR “Respiratory distress” OR “Pelvic Dystocia” OR “Tearing of tissue” OR “Cephalopelvic disproportion” OR “Pregnancy induced hypertension” OR “NICU admission” OR “Asphyxia” OR “Obstructed labor” OR “Assisted delivery”. | |
| 4. “Risk factors” OR “dangers” OR “Age” OR “Weight” OR “Obesity” OR “ANC attendance” OR “Hospital bookings” OR “Underweight” OR “Diabetes” OR “Malaria” OR “Sexual Transmitted disease” OR “Sexual transmitted infections” OR “HIV/AIDS” OR” HIV” OR “AIDS” OR “High blood pressure” OR “Autoimmune disease” OR “Kidney disease” OR “Asthma” OR “Multiparity” OR “Gravidity” OR “High order pregnancy” OR “Poor nutritional intake” OR “Anemia” OR “Low level of education” OR “Low socioeconomic status” OR “Low health literacy” OR “Rural dwellers” OR “Rural area” OR “Lack of social support” OR “Stigma” OR “Unskilled birth attendants” OR “Long queues at clinics” OR “Attitude of health workers” OR “Abandonment” OR “Child marriage”. | |
| Inclusion criteria |
Papers included were: a) Conducted in Africa or Sub-Saharan Africa. b) Conducted on adolescents and reported on adverse pregnancy outcomes and/or associated risks c) peer-reviews articles, literature reviews, dissertation or grey literature. d) Reported in English language e) Conducted 2010 or later. |
| Exclusion criteria |
Papers excluded were: a) Conducted outside Africa b) Full-text articles or conference papers that were not available. c) Studies designed as editorials, letters to editors, commentaries, expert opinions, case reports, and case series. d) Studies that did not provide reports on adolescents’ adverse pregnancy outcomes and/or associated risk factors. e) Studies conducted in a language apart from English. f) Studies completed or published online before 2010. |
Fig. 1.
PRISMA flow diagram
The first two authors screened the titles together to ensure consistency in approach and independently charted the data, while the third author resolved all discrepancies that occurred. The authors met weekly to discuss issues that resulted from the screening process, disagreements included. Analysis involved thematic and content analysis.
Results
Of the 53 studies, 51 were journal articles, one was grey literature and one was a review. Fifty-one were quantitative studies, one was a qualitative study, one a mixed-method study and one was a review. Fifty studies sampled 263,580 pregnant women; 46,202 adolescents and 217,378 adults (> 20 years;). One study sampled the live births of 68,191 adolescents and 215,199 adults. Additional file 1: Table 2 summarizes the characteristics of the included studies. Details of the data are presented in Additional file 1: Table 2, Tables 2, 3 and 4.
Table 2.
Adverse obstetric outcomes associated with adolescent pregnancy
| Pregnancy outcome | Age groups | Study |
|---|---|---|
| Preeclampsia/ eclampsia | 10–19 years | Mezmur et al., 2021 [17]; Tshakweni et al., 2020 [18]; Grønvik et al., 2018 [7]; Abdelsattar et al., 2016 [19]; Edessy et al., 2015 [20]; Ijarotimi et al., 2014 [21]; Adeyinka et al., 2010 [22]; Zeck et al., 2010 [23]; Abebe et al., 2020 [24]; Alyamani et al., 2021 [25]; Gueye et al., 2020 [26] |
| 10–15 years | Moraes et al., 2018 [27]; Rasheed et al., 2011 [28]; Govender et al., 2018 [29] | |
| 20–45 years | Mezmur et al., 2021 [17]; Tembo et al., 2020 [30] | |
| Maternal death | 10–19 years | November et al., 2018 [31]; de Wet, 2016 [32]; Ijarotimi et al., 2014 [21]; Grønvik et al., 2018 [7]; Ganchimeg et al., 2013 [33]; Alyamani et al., 2021 [25] |
| Cesarean Section | 10–19 years | Yussif et al., 2017 [34]; Edessy et al., 2015 [20]; Ijarotimi et al., 2014 [21]; Iklaki et al., 2012 [35]; Ayuba et al., 2012 [36]; Tebeu et al., 2011 [37]; Zeck et al., 2010 [23]. |
| 10–15 years | Ganchimeg et al., 2013 [33]; Rasheed et al., 2011 [28] | |
| 20–45 years | Alyamani et al., 2021 [25]; Hussein Eldessouki et al., 2020 [38]; Abebe et al., 2020 [24]; Abbas et al., 2017 [39]; Abdelsattar et al., 2016 [19]; Hoque et al., 2014 [40]; Muganyizi et al., 2013 [41]; Omole_Ohonsi et al., 2010 [42]; Hoque et al., 2010 [43] | |
| Obstetric hemorrhage | 10–19 years | Gyimah et al., 2020 [44]; Tembo et al., 2020 [30]; Ijarotimi et al., 2014 [21]; Ayuba et al., 2012 [36]; Hussein Eldessouki et al., 2020 [38] |
| 10–15 years | Moraes et al., 2018 [27] | |
| Obstructed labor | 10–19 years | Tembo et al., 2020 [30]; Tshakweni et al., 2020 [18]; Ijarotimi et al., 2014 [21] |
| PROM | 10–19 years | Abdelsattar et al., 2016 [19]; Tembo et al., 2020 [30] |
| 10–15 years | Rasheed et al., 2011 [28] | |
| ICU admission/ hospital admission | 10–19 years | Alyamani et al., 2021 [25] |
| Gestational hypertension | 10–19 years | Edessy et al., 2015 [20] |
| 20–45 years | Alyamani et al., 2021 [25]; Tembo et al., 2020 [30]; Abdelsattar et al., 2016 [19] | |
| Gestational diabetes | 10–19 years | Abdelsattar et al., 2016 [19]; Alyamani et al., 2021 [25] |
| Gestational anemia | 10–19 years | Tshakweni et al., 2020 [18]; Ijarotimi et al., 2014 [21]; Ezegwui et al., 2012 [45] |
| 10–15 years | Govender et al., 2018 [29] | |
| Cephalopelvic disproportion | 10–19 years | Gueye et al., 2020 [26]; Mubikayi, 2020 [46] |
| 10–15 years | Moraes et al., 2018 [27]; Ganchimeng et al., 2013 [33] | |
| Prolonged labor | 10–19 years | Tshakweni et al., 2020 [18] |
| 10–15 years | Moraes et al., 2018 [27] | |
| Assisted vaginal birth | 10–19 years | Ezegwui et al., 2012 [45]; Zeck et al., 2010 [23] |
| 20–45 years | Ayuba et al., 2012 [36]; Omole_Ohonsi et al., 2010 [42] | |
| Emotional vulnerability | 10–15 years | Govender et al., 2018 [29] |
Table 3.
Adverse perinatal/neonatal outcomes associated with adolescence pregnancy
| Pregnancy outcome | Age groups | Study |
|---|---|---|
| LBW | 10–19 years | Mezmur et al., 2021 [17]; Serunjogi et al., 2021 [47]; Pons-Duran et al., 2021 [48]; Gyimah et al., 2020 [44]; Siakwa et al. 2020 [49]; Abebe et al., 2020 [24]; Kamala et al., 2018 [50]; Gronvik et al., 2018 [7]; Agbor et al., 2017 [51]; Njim et al., 2017 [52]; Abbas et al., 2017 [39]; Abdelsatter et al., 2016 [19]; Njim et al., 2016 [53]; Schipulle 2015 [54]; Ngowa et al., 2015 [55]; Muganyizi et al., 2013 [41]; Ezegwui et al., 2012 [45]; Adeyinka et al., 2010 [22]; Kurth et al., 2010 [56]; Omole- Ohonsi et al., 2010 [42]; Zeck et al., 2010 [23]; Hussein Eldessouki et al., 2020 [38]; Kassa et al., 2019 [57]; Bihoun et al., 2017 [58]; Egbe et al., 2015 [59]; Granchimeng et al., 2013 [33] |
| 10–15 years | Moraes et al., 2018 [27]; Govender et al., 2018 [29]; Mombo-Ngoma et al., 2016 [60] | |
| 35+ years | Kamala et al., 2018 [50]; Muganyizi et al., 2013 [41] | |
| Preterm birth | 10–19 years | Mezmur et al., 2021 [17]; Serunjogi et al., 2021 [47]; Pons-Duran et al., 2021 [48]; Gyimah et al., 2020 [44]; Andemel et al., 2020 [61]; Abebe et al., 2020 [24]; Grønvik et al., 2018 [7]; Njim et al., 2016 [53]; Ngowa et al., 2015 [55]; Edessy et al., 2015 [20]; Fouelifack et al., 2014 [62]; Ezegwui et al., 2012 [45]; Ayuba et al., 2012 [36]; Omole- Ohonsi et al., 201 0[42]; Gueye et al., 2020 [26]; Hussein Eldessouki et al., 2020 [38]; Kassa et al., 2019 [57]; Bihoun et al., 2017 [58]; Egbe et al., 2015 [59]; Granchimeng et al., 2013 [33] |
| 10–15 years | Mombo-Ngoma et al., 2016 [60]; Rasheed et al., 2011 [28]; Tebeu et al., 2011 [37] | |
| 20–45 years | Siakwa et al., 2020 [49] | |
| Neonatal death | 10-19 years |
Serunjogi et al., 2021 [47]; Gyimah et al., 2020 [44]; Noveber et al., 2018 [31] Yussif et al., 2017 [34]; de Wet, 2016 [32]; Ganchimeng et al., 2013 [33] |
| 10-15 years | Moraes et al., 2018 [27]; Neal et al., 2018 [10]; Ijarotimi et al., 2014 [21] | |
| Perinatal deaths | 10-19 years | Andemel et al., 2020 [61]; Kamala et al., 2018 [50]; Grønvik et al., 2018 [7]; Ezegwui et al., 2012 [45]; Laari et al., 2016 [63] |
| 35+ years | Kamala et al., 2018 [50] | |
| Stillbirth | 10–19 years | Kamala et al., 2018 [50]; Yussif et al., 2017 [34]; Edessy et al., 2015 [20]; Iklaki et al., 2012 [35]; Tebeu et al., 2011 [37]; Adeyinka et al., 2010 [22]; Hussein Eldessouki et al., 2020 [38]; Fouelifack et al., 2014 [62]; Zeck et al., 2010 [23] |
| 35+ years | Kamala et al., 2018 [50]; Muganyizi et al., 2013 [41] | |
| Low Apgar score | 10–19 years | Mezmur et al., 2021 [17]; Tshakweni et al., 2020 [18]; Abbas et al., 2017 [39]; Kamala et al., 2018 [50]; Hogue et al., 2014 [40]; Muganyizi et al., 2013 [41]; Ezegwui et al., 2012 [45]; Adeyinka et al., 2010 [22] |
| 10–15 years | Moraes et al., 2018 [27]; Govender et al., 2018 [29] | |
| 20–45 years | Siakwa et al., 2020 [49] | |
| 35+ years | Kamala et al., 2018 [50] | |
| Small-for-gestational age | 10–19 years | Pons-Duran et al., 2021 [48] |
| 10–15 years | Govender et al., 2018 [29] | |
| Neonatal respiratory distress | 10–19 years | Jaen-Sanchez et al., 2020 [64]; Gueye et al., 2020 [26] |
| Fetal/perinatal distress | 10–19 years | Tshakweni et al., 2020 [18]; Fouelifack et al., 2014 [62] |
| Fetal infections | 10–19 years | Gueye et al., 2020 [26] |
| Birth asphyxia | 10–19 years | Agbor et al., 2017 [51]; Njim et al., 2016 [53]; Ijarotimi et al., 2014 [21]; Gueye et al., 2020 [26] |
| 10–15 years | Moraes et al., 2018 [27] | |
| NICU admission | 10–19 years | Abdelsattar et al., 2016 [19] |
| Congenital disorders | 10–19 years | Edessy et al., 2015 [20] |
Table 4.
Risk factors associated adolescence poor pregnancy outcomes
| Major theme | Sub-theme | Study |
|---|---|---|
| Socio-demographic factors | Poor socioeconomic status | Alyamani et al., 2021 [25]; Mezmur et al., 2021 [17]; Hussein Eldessouki et al., 2020 [38]; Noveber et al., 2018 [31]; Govender et al., 2018 [29]; Abbas et al., 2017 [39]; Egbe et al., 2015 [59]; Ijarotimi et al., 2014 [21]; Ganchimeg et al., 2013 [33]; Ezegwui et al., 2012 [45]; Ayuba et al., 2012 [36]; Zeck et al., 2010 [23] |
| Low education | Hussein Eldessouki et al., 2020 [38]; Kamala et al., 2018 [50]; Abbas et al., 2017 [39]; Rasheed et al., 2011 [28]; Zeck et al., 2010 [23] | |
| Low health literacy | November et al., 2018 [31]; Zeck et al., 2010 [23] | |
| Married | Agbor et al., 2017 [51]; Abdelsatter et al., 2016 [19] | |
| Not married | Kassa et al., 2019 [57]; Fouelifack et al., 2014 [62]; Ayyuba et al., 2012 [36]; Egbe et al., 2015 [59] | |
| Age [10–16] | Moraes et al., 2018 [27]; neal et al., 2018 [10]; Mombo-Ngoma et al., 2016 [60]; Rasheed et al., 2011 [28]; Kurth et al., 2010 [56] | |
| Age [< 20] | Andemel et al., 2020 [61]; Abebe et al., 2020 [24]; Mubikayi, 2020 [46]; Kamala et al., 2018 [50]; Grønvik et al., 2018 [7]; Bihoun et al., 2017 [58]; Yussif et al., 2017 [34]; Abbas et al., 2017 [39]; Egbe et al., 2015 [59]; Ngowa et al., 2015 [55]; Edessy et al., 2015 [20]; Fouelifack et al., 2014 [62]; Ijarotimi et al., 2014 [21]; Ayuba et al., 2012 [36]; Tebeu et al., 2011 [37]; Adeyinka et al., 2010 [22]. | |
| Rural area | Hussein Eldessouki et al., 2020 [38]; Kassa et al., 2019 [57]; Agbor et al., 2017 [51]; Bihoun et al., 2017 [58]; Abbas et al., 2017 [39]; Laari et al., 2016 [63]; Abdelsatter et al., 2016 [19]; Edessy et al., 2015 [20]; Rasheed et al., 2011 [28]. | |
| Risky behaviour/ attitudes | No/low/late ANC attendance | Alyamani et al., 2021 [25]; Mezmur et al., 2021 [17]; Jean-Sanchez et al., 2020 [64]; Gueye et al., 2020 [26]; Tshakweni et al., 2020 [18]; Abebe et al., 2020 [24]; Kassa et al., 2019 [57]; Kamala et al., 2018 [50]; Govender et al., 2018 [29]; Laari et al., 2016 [63]; Schipulle, 2015 [54]; Edessy et al., 2015 [20]; Ijarotimi et al., 2014 [21]; Muganyizi 2013 [41]; Ganchimeng et al., 2013 [33]; Iklaki et al., 2012 [35]; Kurth et al., 2010 [56]; Omole-Ohonsi et al., 201 0[42] |
| Delayed care seeking | November et al., 2018 [31] | |
| Inadequate nutrition | Gyimah et al., 2020 [44]; Bihoun et al., 2017 [58]; Neal et al., 2018 [10] | |
| Alcohol intake | Laari et al., 2016 [63] | |
| No facility birth | Omole-Ohonsi et al., 201 0[42] | |
| Pregnancy characteristics | Subsequent births | Neal et al., 2018 [10] |
| Multiparity | Kamala et al., 2018 [50] | |
| Gravidity | Egbe et al., 2015 [59]; Ibrahim et al., 2015 [65] | |
| High order pregnancy | Obare et al., 2012 [66] | |
| Health facility factors | poor ANC quality | Chaibva et al., 2019 [67]; Omole-Ohonsi et al., 2010 [42] |
| Long queues | Govender et al., 2018 [29] | |
| Attitude of health workers | Govender et al., 2018 [29] | |
| Long distance | Govender et al., 2018 [29] | |
| Stigma | November et al., 2018 [31] | |
| Adolescent pregnancy-related Stigma and abuse | Stigma | November et al., 2018 [31] |
| Abandonment | Omole-Ohonsi et al., 2010 [42] | |
| Lack of family and social support | Omel-Ohonsi et al., 2010 [42] | |
| IPV | Mezmur et al., 2021 [17] | |
| Previous obstetric complications | Previous abortion | Jean-Sanchez et al., 2020 [64]; Abass et al., 2017 [39]; de Wet, 2016 [32]; Edessy et al., 2015 [20] |
| Previous CS | Abbas et al, 2017 [39] | |
| Diseases/infections | HIV | Jean-Sanchez et al., 2020 [64]; Govender et al., 2018 [29]; Obare et al., 2012 [66] |
| Malaria | Mombo-Ngoma et al., 2016 [60] | |
| Hypertension | de Wet, 2016 [32] |
Adverse obstetric and perinatal/neonatal outcomes in adolescent pregnancy
To address the first research question, two major themes were generated: (1) adverse obstetric outcomes in adolescent pregnancies and (2) adverse perinatal or neonatal outcomes in adolescent pregnancies.
Adverse obstetric outcomes in adolescent pregnancies
Regardless of the study design, we found a high prevalence of negative obstetric outcomes among adolescent mothers (Table 2). Preeclampsia and eclampsia were found to be more common in pregnant adolescents than in adults [7, 17/27]. Studies focusing on adolescent sub-group analysis found that young adolescents had a higher incidence of preeclampsia and eclampsia than older adolescents and adults [27, 28]. Moreover, maternal mortality is higher among adolescent than among adult mothers [7, 21, 25, 31–33]. One study compared adolescent mothers and advanced age mothers (> 34 years) and found a higher incidence of maternal deaths in the latter [41]. More studies found higher incidences of cesarean birth in adults than in adolescents [19–21, 23–25, 34–43]. Contrarily, two other studies reported a higher incidence of cesarean birth in young adolescents than in older adolescents and adults [28, 33].
Evidence also indicated that adolescents had higher rates of postpartum and antepartum hemorrhage than adults [17]. Obstructed labor, premature rupture of membranes (PROM) and gestational diabetes are also more common among adolescents [18, 19, 21, 25, 27]. Rasheed et al. [28] observed that younger adolescents are more vulnerable to PROM than their older counterparts. It was also revealed that adolescent mothers are more likely than adult mothers to be admitted to intensive care units (ICU) [25, 45]. Furthermore, adolescent mothers had a higher incidence of gestational anemia, prolonged labor and cephalopelvic disproportion than adult mothers [18, 21, 26, 28, 47–49]. Moreover, assisted vaginal births were similar for adolescent and adult mothers [23, 29, 36, 42]. Again, cephalopelvic disproportion [27, 33] and emotional trauma [46] are more common in young adolescent girls [28, 32, 48]. Adults, however, had a higher prevalence of gestational hypertension than adolescents [19, 20, 25, 30].
Adverse perinatal and neonatal outcomes in adolescent pregnancies
We found an increased risk of adverse perinatal and neonatal outcomes for adolescent mothers (Table 3). Adolescent mothers are at higher risk of LBW and preterm births and younger adolescents are at higher risk of LBW with preterm births than their older counterparts [7, 17, 19, 20, 22–24, 26, 28, 29, 32–35, 38, 42, 44–48, 50–63, 65]. The review also showed that the two extreme age groups in pregnant women (below age 15 and above age 40) have a higher incidence of LBW compared with older adolescents [41, 50]. One study, however, found that preterm births are more prevalent in adult mothers compared to adolescents [49].
Studies that compared adolescents to adults have also showed higher risks of neonatal, perinatal and fetal deaths and stillbirths among adolescent mothers [7, 20, 22, 23, 30–32, 34, 39, 41, 44, 45, 47, 50, 52, 62, 63, 66]. Within adolescent groups, some studies reported that young adolescents are at a greater risk of neonatal mortality, while advanced age mothers are at higher risks of perinatal deaths [50] and stillbirths [41, 50] compared to adolescents [10, 21, 28, 33, 52]. Low Apgar scores were more common among adolescents than in adults [17, 18, 22, 29, 39–41, 49, 50]. Meanwhile, other studies have found that low Apgar scores are more common in young adolescents than in older adolescents [27, 46]. According to Kamala et al., low Apgar scores are more common among advanced-age mothers than in adolescents [52]. Newborns from advanced age mothers are also more likely small-for-gestational-age, to have neonatal respiratory distress, fetal or perinatal distress, fetal infections, birth asphyxia, neonatal intensive care units (NICU) admission and congenital disorders [18–21, 26, 45, 51, 53, 62, 64]. However, two studies reported that newborns from younger adolescents are also more likely small-for-gestational-age and to have birth asphyxia [27, 46].
Risk factors associated with adverse pregnancy outcomes among adolescents
Five major themes were generated about risk factors that expose adolescent pregnancies to adverse outcomes. Socioeconomic factors, risky behaviors or lifestyle, pregnancy characteristics, health facility factors, adolescent pregnancy-related stigma and abuse, previous obstetric complications, disease and infections are important here (Table 4).
Socio-economic factors
Age 10 to 16 years and less than 20 years were identified as major risk factors [7, 10, 20, 21, 24, 28, 29, 32, 33, 35, 38, 39, 41, 49, 52, 53, 58, 59, 61–63, 65]. Some studies revealed that adolescents with low socioeconomic status, low education and low health literacy are at higher risks of maternal and neonatal mortality and morbidities [17, 21, 23, 25, 29, 30, 32, 34, 35, 42, 47, 48, 52, 53]. Moreover, adolescents in rural areas and those who are not married are at risk of having poor pregnancy outcomes [19, 20, 29, 34, 35, 42, 53, 54, 60, 61, 63, 66]. Married adolescents, however, are not immune to unfavorable pregnancy outcomes [19, 51].
Risky behaviors or lifestyle
Pregnant adolescents who have no, few or late appointments for antenatal care (ANC) are more likely to have negative pregnancy outcomes due to delayed care-seeking and a preference for unskilled birth [17, 18, 20, 21, 24–26, 30, 32, 33, 38, 41, 48, 52, 57, 59, 60, 66, 67]. Meanwhile, it is revealed that lifestyle choices such as alcohol consumption and inadequate nutrition intake put pregnant adolescents at higher risk of pregnancy complications [10, 45, 61, 66].
Health facility factors and pregnancy characteristics
Some factors of health facilities also discourage adolescents from seeking and receiving appropriate care. Adolescents are discouraged from seeking maternal health care because of poor ANC quality, long queues and waiting time, negative attitudes of health care workers, long distances to health centers and stigma directed towards pregnant adolescents by health care professionals [31, 42, 46, 67]. Moreover, adolescents who are multiparous or have a high order pregnancy are at higher risks of adverse pregnancy outcomes [10, 40, 52, 53, 64].
Stigma and abuse
Adolescents who are pregnant face stigma and abuse from their peers and family members [31, 42]. Rejection from family members deprives them of necessary family and social support [42]. They may even face partner violence which puts them and the fetus at risk [17].
Previous obstetric complications, disease and infections
Adolescents with a history of abortion and cesarean birth are at higher risks of adverse pregnancy outcomes [20, 32, 39, 64]. Infections and diseases such as HIV/AIDS, malaria and hypertension put pregnant adolescents at risk of having poor pregnancy outcomes [32, 46, 60, 64, 66].
Discussion
Our findings revealed that adolescent pregnancy and childbirth are linked to poor maternal and perinatal health outcomes. Many maternal morbidities, emotional trauma included, are more common in adolescent mothers in Africa. The same holds true for perinatal mortality and morbidity. Younger adolescents [≤15 years] have higher risks of negative pregnancy outcomes than older adolescents [16–19 years] and adult mothers. In addition to maternal mortality, adolescent mothers may face other health risks in the future. The International Diabetes Federation (IDF) observed that among women with gestational diabetes, 5.7% develop Type 1 diabetes within 7 years and 50.4% develop Type 2 diabetes within 23 years [68]. High adolescent fertility, as well as high adverse pregnancy outcomes in the African continent may explain why sub-Saharan Africa had the highest neonatal mortality rates per 1000 live births in 2019 [1, 30]. It is also clear that the majority of perinatal and neonatal deaths in 2017 were caused by preterm birth, LBW, birth asphyxia and sepsis [69]. Can Africa achieve SDG 3 by the year 2030 with these high numbers of complicated adolescent pregnancies?
Adolescent pregnancy is of much concern because adverse pregnancy outcomes are associated with a variety of vulnerabilities such as child marriage, female genital mutilation (FGM) and unsafe abortion [2]. Young adolescents may be physiologically immature and at high risk of nutritional deficiencies and hypertension [10]. Thus, African governments and their health agencies would need to prevent adolescents from becoming pregnant and be physiologically mature enough, when they start with childbearing.
Risk factors affecting poor adolescent pregnancy outcomes in Africa
Our review indicated that adolescents in Africa, regardless of their marital, socioeconomic, educational and health literacy status, are at risk of poor pregnancy outcomes. Risky behaviors or attitudes, such as delayed health care seeking, insufficient nutrition intake, birth at home and alcohol consumption put pregnant adolescents at risk of poor pregnancy outcomes. Moreover, poor ANC quality, poor attitudes of health care professionals, stigma and abuse are risk factors that expose adolescents to poor pregnancy outcomes. Pregnant adolescents in Africa are highly susceptible to highly prevalent infections on the continent that affect birthweight and gestational age at birth [10]. Adolescents have a 20–40% risk of vertical transmission of HIV and other STIs to the fetus.
Pregnant adolescents face rejection, stigma and abuse from family members and intimate partners, which may have both direct and indirect impacts on their pregnancy outcomes [17, 42]. Moreover, with low levels of health literacy, adolescents are likely to face difficulties to access health care, understand health information and effectively use such information to maintain and promote healthy pregnancy outcomes [2, 23, 31]. Pregnant adolescent girls in low-resource settings have negative attitudes toward seeking maternal health care because of highly fragmented, poorly coordinated, low quality of care [2, 7]. Pregnant teenagers regard primary health care as inaccessible for fear of stigma, lack of respect, privacy and confidentiality, discrimination and imposition of moral norms, particularly in resource-limited settings such as Africa [2, 18, 25]. In most African countries, particularly in rural areas, poor health and road infrastructure, as well as lack of health care professionals may also prevent pregnant adolescents from seeking quality health care.
Child marriage is highly prevalent in Africa and has been linked to poor maternal outcomes, intimate partner violence (IPV’, limited decision to seek health care during pregnancy and maternal mortality [70]. A married girl may have little or no ideas about contraception and may lack the decision authority to even time and space pregnancy. Meanwhile, poorly timed or unwanted pregnancies are often associated with a high risk of morbidity and mortality in adolescents, because of high numbers of abortions [71]. Abortion, however, is highly stigmatized in Africa and adolescents are forced to have unsafe abortions due to lack of care, high costs, stigma, refusal by health care workers, needless requirements and morality [1]. In Ghana, for example, unsafe abortions account for 11–30% of maternal deaths, with adolescents accounting for 35% of these [71]. The phenomenon of adolescent pregnancy and its related adverse pregnancy outcomes are multifaceted and interdisciplinary issues, and the earlier evidence-based proactive measures are put in place, the better.
Policy implications
Eliminating adolescent pregnancy will significantly reduce maternal and perinatal mortality, and accelerate progress toward achieving the maternal and perinatal components of the SDGs. We propose not only reducing adolescent births, but also reducing births in the most vulnerable girls, such as those under the age of 16, those living on the streets and in rural areas in displaced settlements in Africa. In Africa, particularly in sub-Saharan Africa, there has been minimal progress in reducing adolescent births, which calls for improvement in young girls’ health by preventing adolescent pregnancy [10].
To be successful in preventing adolescent pregnancy, efforts are needed to eliminate child marriage, poverty and all forms of abuse and stigma directed at adolescent girls, particularly during pregnancy when they attempt to seek quality health care. Adolescents need to have access to abortion and post-abortion care in Africa. Moreover, significant efforts are needed to improve sexual and reproductive health by developing appropriate approaches and strategies to meet the needs of adolescents. All vulnerable and at-risk girls such as homeless, out of school, living in urban slums or displaced, need to be provided with comprehensive, culturally and socially appropriate sexual education as well as essential and adolescent-friendly sexual and reproductive health care.
Pregnant adolescents will have better pregnancy outcomes if they have access to adequate and high-quality ANC and postnatal care. This package of maternal and child care could include nutritional programs, treatments for infection and prompt attention to treatable obstetric conditions. All impediments to pregnant adolescents’ access to health care seeking need to be removed.
Recommendations for future research
Few studies in this review attempted to control for socio-demographic factors. Because the majority were retrospective records´ reviews, some relevant socioeconomic factors such as educational attainment and income status were missing. Future research needs to also prioritize high-quality studies of younger as compared with older adolescents rather than grouping them together. Some studies had small sample sizes drawn from hospital settings, which may exclude more vulnerable groups and have an impact on generalization. There is a high likelihood that pregnant adolescents in Africa will give birth outside a health care setting, and future studies need to include this population to help improve generalization and estimation of adverse pregnancy outcomes and risk factors. Future studies focusing on medical records may avoid information bias, but they will also face incomplete and insufficient medical records.
Limitations
There is a possibility of publication bias, because negative results are unlikely to be published. Studies were also restricted to those published in English, which may have an impact on outcomes of this review. Despite this limitation, this review compiled relevant studies, including a large sample, from four major databases, five other online sources and 21 nations in Africa. Furthermore, the authors sought advice from experts who were deemed relevant for this review to provide comprehensive evidence on adolescent pregnancy and associated adverse pregnancy outcomes in Africa.
Conclusion
Adolescent pregnancy is associated with a higher risk of adverse pregnancy outcomes. Aside age, factors that put pregnant adolescents at high risk of poor pregnancy outcomes include low socioeconomic and educational status, poor utilization of ANC, risky lifestyles such as alcohol consumption, and unappealing health care factors. Maternal health utilization was identified as an important factor in improving pregnancy outcomes among adolescents in Africa. Aside increased efforts to prevent adolescent pregnancy, it is also prudent to increase adolescent utilization of maternal health care, as well as address issues of stigma, abortion and child marriage in Africa. There is a need for high-quality observational studies on young adolescents that account for confounders in Africa.
Supplementary Information
Additional file 1: Table 2. Extracted data and study characteristics.
Acknowledgements
Not applicable.
Abbreviations
- HIV
Human Immunodeficiency Virus
- AIDS
Acquired Immunodeficiency Syndrome
- LBW
Low Birth Weight
- WHO
World Health Organization
- PROM
Premature Rupture of Membranes
- IDF
International Diabetes Federation
- NICU
Neonatal Intensive Care Unit
- ANC
Antenatal Care
- PNC
Postnatal Care
- ICU
Intensive Care Unit
- IPV
Intimate Partner Violence
Authors’ contributions
MA, and DH conceptualized and designed the study, collected and analyzed the data, and wrote the initial draft. EWA is the independent researcher who led and guided the team throughout the review process. All authors read and approved the final version of the manuscript for publication.
Funding
This work received no funding support.
Availability of data and materials
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO . Adolescent pregnancy. World Health Organisation (WHO) 2020. [Google Scholar]
- 2.WHO, UNAIDS . Global standards for quality health-care services for adolescents volume 1: standards and criteria a guide to implement a standards-driven approach to improve the quality Oof health-care services for adolescents. 2015. [Google Scholar]
- 3.Darroch JE, Woog V, Bankole A, Ashford LS, Points K. Costs and benefits of meeting the contraceptive needs of adolescents. 2016. [Google Scholar]
- 4.Neal S, Matthews Z, Frost M, Fogstad H, Camacho AV, Laski L. Childbearing in adolescents aged 12–15 years in low resource countries: a neglected issue. New estimates from demographic and household surveys in 42 countries. Acta Obstet Gynecol Scand. 2012;91(9):1114–8. [DOI] [PubMed]
- 5.WHO . Adolescent and young adult health. Adolescent and young adult health. 2021. [Google Scholar]
- 6.United Nations . The Sustainable Development Goals Report. 2016. [Google Scholar]
- 7.Grønvik T, Sandøy IF. Complications associated with adolescent childbearing in Sub-Saharan Africa: A systematic literature review and meta-analysis. Plos One. 2018;13(9). [DOI] [PMC free article] [PubMed]
- 8.Yeboah-Asiamah Asare B, Baafi D, Dwumfour-Asare B, Adam A-R. Factors associated with adolescent pregnancy in the Sunyani Municipality of Ghana. Int J Afr Nurs Sci. 2019;10:87–91. [Google Scholar]
- 9.Fall CHD, Sachdev HS, Osmond C, et al. Association between maternal age at childbirth and child and adult outcomes in the offspring: a prospective study in five low-income and middle-income countries (COHORTS collaboration) Lancet Glob Health. 2015;3(7):e366–e377. doi: 10.1016/S2214-109X(15)00038-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neal S, Channon AA, Chintsanya J. The impact of young maternal age at birth on neonatal mortality: Evidence from 45 low and middle income countries. Plos One. 2018;13(5). [DOI] [PMC free article] [PubMed]
- 11.Neal S, Mahendra S, Bose K, et al. The causes of maternal mortality in adolescents in low and middle income countries: Systematic review of the literature. BMC Pregnancy Childbirth. 2016;16(1). [DOI] [PMC free article] [PubMed]
- 12.UNICEF . Low Birthweight: Country, Regional and Global Estimates - UNICEF DATA. 2004. [Google Scholar]
- 13.Loaiza E, Liang M. Adolescent pregnancy: a review of the evidence adolescent pregnancy: a review of the evidence UNFPA New York, 2013 1 CONTENTS. 2013. [Google Scholar]
- 14.Gibbs CM, Wendt A, Peters S, Hogue CJ. The impact of early age at first childbirth on maternal and infant Healthp pe_1290 259..284. Paediatr Perinat Epidemiol. 2012;26:259–284. doi: 10.1111/j.1365-3016.2012.01290.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Social Res Methodol Theory Pract. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 16.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Int Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 17.Mezmur H, Assefa N, Alemayehu T. An increased adverse fetal outcome has been observed among teen pregnant women in rural Eastern Ethiopia: a comparative cross-sectional study. Global Pediatric Health. 2021;8. [DOI] [PMC free article] [PubMed]
- 18.Tshakweni N, ter Goon D, Okafor UB. A comparative analysis of teenagers and older pregnant women concerning maternal and neonatal adverse outcomes in raymond mhlaba sub-district, South Africa. Afri J Reprod Health. 2020;24(4):138–146. doi: 10.29063/ajrh2020/v24i4.15. [DOI] [PubMed] [Google Scholar]
- 19.Abdelsattar M. International journal of advanced research in biological sciences teenage pregnancy in Upper Egypt. Int J Adv Res Biol Sci. 2016;3(4).
- 20.Edessy M, El-Darwish AG, el Rashedy MI, Abo Elhamd H. Pregnancy outcome of teenaged Egyptian women International Journal of Advanced Research in Biological Sciences Pregnancy outcome of teenaged upper Egyptian women. Int J Adv Res Biol Sci. 2015;2(4):92–99. [Google Scholar]
- 21.Ijarotimi AO, Biobaku O, Badejoko O, Loto O, Orji E, et al. Obstetric outcome of teenage pregnancy and labour In Obafemi Awolowo University Teaching Hospital Ile-Ife: a ten year review. Niger J Clin Biomed Res Ijarotimi. 2014;7(3):4–15. [Google Scholar]
- 22.Adeyinka DA, Oladimeji O, Adekanbi TI, Adeyinka FE, Falope Y, Aimakhu C. Outcome of adolescent pregnancies in southwestern Nigeria: a casecontrol study. J Maternal-Fetal Neonat Med. 2010;23(8):785–789. doi: 10.3109/14767050903572166. [DOI] [PubMed] [Google Scholar]
- 23.Zeck W, Wilkinson J, Obure J, Masenga G, Ulrich D, Oneko O. Comparison of obstetrical risk in adolescent primiparas at tertiary referral centres in Tanzania and Austria. J Maternal-Fetal Neonat Med. 2010;23(12):1470–1474. doi: 10.3109/14767051003678077. [DOI] [PubMed] [Google Scholar]
- 24.Abebe AM, Fitie GW, Jember DA, Reda MM, Wake GE. Teenage Pregnancy and Its Adverse Obstetric and Perinatal Outcomes at Lemlem Karl Hospital, Tigray, Ethiopia, 2018. BioMed Res Intl. 2020;2020. [DOI] [PMC free article] [PubMed]
- 25.Alyamani AM, Elewa HA, Newira FA. Maternal and Neonatal Outcome of Teenage Pregnancy at Al-Galaa Maternity Teaching Hospital, Cairo, Egypt. Open J Obstet Gynecol. 2021;11(05):591–601. doi: 10.4236/ojog.2021.115055. [DOI] [Google Scholar]
- 26.Gueye M, Boiro D, Sow A, et al. Neonatal complications of teenage pregnancies: prospective study about 209 Cases in Senegal. Am Jf Pediatr. 2020;6(4):504–507. doi: 10.11648/j.ajp.20200604.29. [DOI] [Google Scholar]
- 27.Moraes AN, Likwa RN, Nzala SH. A retrospective analysis of adverse obstetric and perinatal outcomes in adolescent pregnancy: the case of Luapula Province, Zambia. Matern Health, Neonatol Perinatol. 2018;4(1). [DOI] [PMC free article] [PubMed]
- 28.Rasheed S, Abdelmonem A, Amin M. Adolescent pregnancy in Upper Egypt. Int J Gynecol Obstet. 2011;112:21–24. doi: 10.1016/j.ijgo.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 29.Govender T, Reddy P, Ghuman S. Obstetric outcomes and antenatal access among adolescent pregnancies in KwaZulu-Natal, South Africa. S Afr Fam Pract. 2018;60(1):1–7. doi: 10.1080/20786190.2017.1333783. [DOI] [Google Scholar]
- 30.Tembo T, Koyuncu A, Zhuo H, Mwendafilumba M, Manasyan A. The association of maternal age with adverse neonatal outcomes in Lusaka, Zambia: a prospective cohort study. BMC Pregnancy Childbirth. 2020;20(1). [DOI] [PMC free article] [PubMed]
- 31.November L, Sandall J. “Just because she’s young, it doesn’t mean she has to die”: Exploring the contributing factors to high maternal mortality in adolescents in Eastern Freetown; a qualitative study. Reprod Health. 2018;15(1):1–18. doi: 10.1186/s12978-018-0475-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Wet N. Pregnancy and death: An examination of pregnancy-related deaths among adolescents in South Africa. SAJCH. 2016;10(3):151–155. doi: 10.7196/SAJCH.2016.v10i3.978. [DOI] [Google Scholar]
- 33.Ganchimeg T, Mori R, Ota E, et al. Maternal and perinatal outcomes among nulliparous adolescents in low- and middle-income countries: A multi-country study. BJOG. 2013;120(13):1622–1630. doi: 10.1111/1471-0528.12391. [DOI] [PubMed] [Google Scholar]
- 34.Yussif AS, Lassey A, GYK G, Kantelhardt EJ, Kielstein H. The long-term effects of adolescent pregnancies in a community in Northern Ghana on subsequent pregnancies and births of the young mothers. Reprod Health. 2017;14(1). [DOI] [PMC free article] [PubMed]
- 35.Iklaki CU, Inaku JU, Ekabua JE, Ekanem EI, Udo AE. Perinatal outcome in unbooked teenage pregnancies in the University of Calabar Teaching Hospital, Calabar, Nigeria. Obstet Gynecol. 2012;2012:1–5. [DOI] [PMC free article] [PubMed]
- 36.Ayuba II, Gani O. Outcome of Teenage Pregnancy in the Niger Delta of Nigeria. Ethiop J Health Sci. 2012;22(1):45–50. [PMC free article] [PubMed] [Google Scholar]
- 37.Tebeu PM, Nsangou I, Njotang PN, PTT B, Doh AS, Fomulu JN. Outcome of delivery in nulliparous teenagers aged less than 17 years: the cameroon university centre hospital experience. Open J Obstet Gynecol. 2011;01(02):47–52. doi: 10.4236/ojog.2011.12010. [DOI] [Google Scholar]
- 38.Eldessouki KHM, Quodi MAE, Mahmoud S, Hassane A. Assessment of The Impact of Teenage Pregnancy on Pregnancy Outcome among Pregnant Women in Minia University Hospitals, Minia Governorate. Egypt J Community Med. 2020;38(2):87–95.
- 39.Abbas AM, Ali SS, Ali MK, Fouly H, Altraigey A. The maternal and neonatal outcomes of teenage pregnancy in a Tertiary University Hospital in Egypt. Proc Obstet Gynecol. 2017;7(3):1–10. [Google Scholar]
- 40.Hoque ME, Towobola OA, Mashamba TJ, Monokoane T. Comparison of adverse pregnancy outcome between teenage and adult women at a Tertiary Hospital in South Africa. Biomedical Research (India) 2014;25(2):167–172. [Google Scholar]
- 41.Muganyizi PS, Balandya B. Pregnancy outcomes in the extremes of reproductive age: A seven-year experience in Tanzania. Open J Obstet Gynecol. 2013;03(01):51–57. doi: 10.4236/ojog.2013.31012. [DOI] [Google Scholar]
- 42.Omole-Ohonsi A, Attah RA. Obstetric outcome of teenage pregnancy in Kano, North-Western Nigeria. West Afr J Med. 2010;29(5):18–22. doi: 10.4314/wajm.v29i5.68252. [DOI] [PubMed] [Google Scholar]
- 43.Hoque M, Hoque S. A comparison of obstetrics and perinatal outcomes of teenagers and older women: Experiences from rural South Africa. Afr J Prim Health Care Fam Med. 2010;2(1).
- 44.Gyimah LA, Annan RA, Apprey C, et al. Nutritional status and birth outcomes among pregnant teenagers in Ghana. 2020. [Google Scholar]
- 45.Ezegwui HU, Ikeako LC, Ogbuefi F. Obstetric outcome of teenage pregnancies at a tertiary hospital in Enugu, Nigeria. Niger J Clin Pract. 2012;15(2):147–150. doi: 10.4103/1119-3077.97289. [DOI] [PubMed] [Google Scholar]
- 46.Mubikayi L. The epidemiologic and maternal and fetal prognosis of teenage girls. Open J Obstet Gynecol. 2020;10(03):422–432. doi: 10.4236/ojog.2020.1030038. [DOI] [Google Scholar]
- 47.Serunjogi R, Barlow-Mosha L, Mumpe-Mwanja D, et al. Comparative analysis of perinatal outcomes and birth defects amongst adolescent and older Ugandan mothers: evidence from a hospital-based surveillance database. Reprod Health. 2021;18(1). [DOI] [PMC free article] [PubMed]
- 48.Pons-Duran C, Casellas A, Bardají A, et al. Adolescent, pregnant, and HIV-infected: risk of adverse pregnancy and perinatal outcomes in young women from Southern Mozambique. J Clin Med. 2021;10(8):1564. doi: 10.3390/jcm10081564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Siakwa M, Nyarko-Sampson M, Bruce SD. Obstetric outcomes: a comparison of teenagers and adults in the Cape Coast metropolis, Ghana. Heliyon. 2020;6(11). [DOI] [PMC free article] [PubMed]
- 50.Kamala BA, Mgaya AH, Ngarina MM, Kidanto HL. Predictors of low birth weight and 24-hour perinatal outcomes at Muhimbili national hospital in Dar es Salaam, Tanzania: a five-year retrospective analysis of obstetric records. Pan Afri Med J. 2018;29(1):1–13. doi: 10.11604/pamj.2018.29.220.15247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Agbor VN, Mbanga CM, Njim T. Adolescent deliveries in rural Cameroon: An 8-year trend, prevalence and adverse maternofoetal outcomes. Reprod Health. 2017;14(1). [DOI] [PMC free article] [PubMed]
- 52.Njim T, Agbor VN. Adolescent deliveries in semi-urban Cameroon: Prevalence and adverse neonatal outcomes. BMC Res Notes. 2017;10(1). [DOI] [PMC free article] [PubMed]
- 53.Njim T, Choukem SP, Atashili J, Mbu R. Adolescent deliveries in a secondary-level care hospital of cameroon: a retrospective analysis of the prevalence, 6-year trend, and adverse outcomes. J Pediatr Adolesc Gynecol. 2016;29(6):632–634. doi: 10.1016/j.jpag.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 54.Schipulle V. Adolescent pregnancies in Central Gabon: a description of epidemiology and birth outcomes. 2015. [Google Scholar]
- 55.Ngowa JDK, Kasia JM, Pisoh WD, Ngassam A, Noa C. Obstetrical and perinatal outcomes of adolescent pregnancies in cameroon: a retrospective cohort study at the Yaoundé General Hospital. Open J Obstet Gynecol. 2015;05(02):88–93. doi: 10.4236/ojog.2015.52012. [DOI] [Google Scholar]
- 56.Kurth F, Bélard S, Mombo-Ngoma G, et al. Adolescence as risk factor for adverse pregnancy outcome in central Africa - a cross-sectional study. Plos One. 2010;5(12). [DOI] [PMC free article] [PubMed]
- 57.Kassa GM, Arowojolu AO, Odukogbe AA, Yalew AW. Adverse neonatal outcomes of adolescent pregnancy in northwest Ethiopia. Plos One. 2019;14(6). [DOI] [PMC free article] [PubMed]
- 58.Bihoun B, Zango SH, Coulibaly MT, et al. Low birth weight and prematurity in teenage mothers in rural areas of Burkina Faso. J Pregnancy Child Health. 2017;04(04).
- 59.Egbe TO, Omeichu A, Halle-Ekane GE, Tchente CN, Egbe EN, Oury JF. Prevalence and outcome of teenage hospital births at the buea health district, South West Region, Cameroon. Reprod Health. 2015;12(1). [DOI] [PMC free article] [PubMed]
- 60.Mombo-Ngoma G, Mackanga JR, González R, et al. Young adolescent girls are at high risk for adverse pregnancy outcomes in sub-Saharan Africa: An observational multicountry study. BMJ Open. 2016;6(6). [DOI] [PMC free article] [PubMed]
- 61.Andemel N, Gaoussou S, Barry A, et al. Adverse pregnancy outcomes among women presenting at antenatal clinics in Ouélessébougou, Mali. Reprod Health. 2020;17(1). [DOI] [PMC free article] [PubMed]
- 62.Fouelifack FY, Tameh TY, Mbong EN, et al. Outcome of deliveries among adolescent girls at the Yaoundé central hospital. BMC Pregnancy Childbirth. 2014;14(1):1–10. doi: 10.1186/1471-2393-14-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Laari MN, Laar AS. Exploring Factors Influencing Perinatal Outcomes among Adolescent Pregnancies in Northern Ghana-The Case of Kassena-Nankana Municipality in the Upper East Region. Int J Medi Res Professionals. 2016;2(5).
- 64.Jaén-Sánchez N, González-Azpeitia G, Saavedra-Santana P, et al. Adolescent motherhood in Mozambique. Consequences for pregnant women and newborns. Plos One. 2020;15(6). [DOI] [PMC free article] [PubMed]
- 65.Ibrahim A, O’Keefe AM, Hawkins A, Hossain MB. Levels and Determinants of Low Birth Weight in Infants Delivered Under the National Health Insurance Scheme in Northern Ghana. Matern Child Health J. 2015;19(6):1230–1236. doi: 10.1007/s10995-014-1628-3. [DOI] [PubMed] [Google Scholar]
- 66.Obare F, van der Kwaak A, Birungi H. Factors associated with unintended pregnancy, poor birth outcomes and post-partum contraceptive use among HIV-positive female adolescents in Kenya. BMC Women’s Health. 2012;12. [DOI] [PMC free article] [PubMed]
- 67.Chaibva BV, Olorunju S, Nyadundu S, Beke A. Adverse pregnancy outcomes, “stillbirths and early neonatal deaths” in Mutare district, Zimbabwe (2014): a descriptive study. BMC Pregnancy Childbirth. 2019;19(1). [DOI] [PMC free article] [PubMed]
- 68.International Diabetes Federation . IDF DIABETES ATLAS. 8. 2017. [PubMed] [Google Scholar]
- 69.WHO . Newborns: improving survival and well-being. 2020. [Google Scholar]
- 70.de Groot R, Kuunyem MY, Palermo T. Child marriage and associated outcomes in northern Ghana: a cross-sectional study on behalf of the Ghana LEAP 1000 evaluation team. BMC Public Health. 2018;18(285):1–12. doi: 10.1186/s12889-018-5166-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Guttmacher Institute . Incidence of Abortion and Provision of Abortion-Related Services in Ghana. 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table 2. Extracted data and study characteristics.
Data Availability Statement
All data generated or analyzed during this study are included in this published article (and its supplementary information files).