Abstract
Objective:
The link between adverse childhood experiences (ACEs) and negative mental health outcomes is well established. However, the intergenerational link between caregiver ACE history and their child’s psychosocial outcomes is understudied, particularly within minoritized groups. This study aimed to delineate relations between caregiver ACE exposure and their child’s depression and posttraumatic stress disorder (PTSD) symptoms by proposing a serial mediation of caregiver PTSD, family management problems, and child ACEs.
Methods:
273 Caregiver (Mage = 39.27; 88% female) and adolescent (Mage = 14.26; 57% female) dyads from low-income urban communities completed electronic questionnaires measuring PTSD symptoms and ACEs. Child participants also completed a measure of depression and family management problems. Regression and serial mediation analyses were conducted to examine associations among these variables.
Results:
Caregiver ACEs were significantly associated with their child’s PTSD symptoms but were not related to their child’s depression scores. Serial mediation analyses indicated that child ACEs mediated the relation between caregiver ACEs and their child’s PTSD symptoms. Evidence for an overall indirect effect via caregiver PTSD, family management problems, and child ACEs was not found. No indirect effects between caregiver ACEs and child depression were found.
Conclusions:
Findings evidence that higher levels of caregiver ACE exposure is associated with their child’s PTSD symptoms in a sample of African American dyads living in urban, high burden communities. These results suggest a need for ACE screening during medical visits and provides guidance for future clinical interventions. The distinct intergenerational consequences for caregivers with ACEs and their children’s psychosocial wellbeing warrant further study.
Keywords: ACEs, African American, Depression, PTSD, Family Management
Introduction
Adverse childhood experiences (ACEs) include neglect, abuse, and household dysfunction that occur before the age of 18 (Felitti et al., 1998). National prevalence rates indicate around 57% of US adults report experiencing at least one ACE (Giano et al., 2020) which is concerning given that even low levels of ACEs can negatively impact future health outcomes (Felitti et al., 1998; Sheffler et al., 2020). African Americans are disproportionately represented in communities that experience economic, health, and geographic disparities, placing them at higher risk for exposure to ACEs (Giovanelli & Reynolds, 2021). National parent-report data showed 68% of African American children living below the federal poverty line had experienced at least one ACE (Goldstein et al., 2021). Thus, it is important to explore underlying mechanisms that may exacerbate the link between ACEs and subsequent outcomes, particularly for African American youth in low resource communities, to identify how to best intervene in populations at greater risk for exposure.
An expanding line of research suggests an intergenerational link between a caregiver’s ACE exposure and an increased risk for their child’s mental health problems (Schickedanz et al., 2018; Stepleton et al., 2018). Existing intergenerational studies focus mainly on depressive symptoms emerging in early childhood (Doi et al., 2021; Haynes et al., 2020; Madigan et al., 2015) in predominantly white samples (Haynes et al., 2020; Madigan et al., 2015). Haynes et al. (2020) found that children (8- to 17-years) of caregivers who were exposed to four or more ACEs were three times more likely to have higher levels of depression symptoms as compared to children of caregivers who were exposed to fewer ACEs. These authors used a caregiver report of child depression symptoms and found that 31% of caregivers did not know their child’s mental health status, suggesting these numbers may be underreported. For this reason, child self-report of mental health symptoms may provide a more accurate picture of current symptomatology. A cross-sectional study in Japan found that higher numbers of caregiver ACEs were associated with higher rates of child reported depressive symptoms after controlling for age (Doi et al., 2020). However, sexual abuse was not assessed, limiting the generalizability of these findings compared to studies using the full spectrum of ACEs. Lastly, a longitudinal study found that new mothers’ retrospective report of exposure to physical, but not sexual abuse, was indirectly associated with their preschoolers’ internalizing problems via maternal depression (Madigan et al., 2015). The results of these studies provide empirical support for the intergenerational link between a caregiver’s early childhood adversity and their children’s mental health. As previously mentioned, these studies possess significant limitations that warrant addressing, such as a lack of emphasis on a specific developmental time period (e.g., adolescence) and the narrow focus on depression as an outcome. The overall risk for adversity and mental health problems spanning generations (Morris et al., 2012) suggests a need to assess for other psychosocial outcomes. The one study that has examined multiple internalizing outcomes in adolescence (e.g., anxiety, depression, PTSD) focuses on child maltreatment (i.e., abuse and neglect) without considering a broader range of exposure to traumatic stress (Negriff et al., 2020). Given the current paucity of literature in this area, it is important to comprehensively assess for experiences known to heighten risk across multiple developmental periods (e.g., adolescence), particularly in populations at increased risk for ACE exposure.
Theoretical Perspectives
Developmental psychopathology and attachment theory support possible mechanisms by which caregiver ACEs can influence their adolescent’s psychosocial adjustment (Dekel & Goldblatt, 2008; Yehuda et al., 2013). Both theories emphasize early experiences as formative across the lifespan and intergenerationally (Cicchetti, 2016; Thompson, 2000). Parental ACEs are an intergenerational risk factor for both their children’s ACEs (Narayan et al., 2021; Schofield et al., 2018) and internalizing symptoms (Lambert et al., 2014), but processes by which risk may confer are still being explored.
Developmental psychopathology frameworks emphasize the need to consider multiple pathways (Masten & Cicchetti, 2016) as many factors influence the consequences of risk exposure over time (Luthar et al., 2000; Masten et al., 2021). Attachment theorists posit that caregivers’ past relationships inform their current representations, perceptions, and interactions with their child (Bowlby, 1988). Thus, a caregiver’s own adversity may influence their own parenting stress, skills, and behaviors (Narayan et al., 2021). Parenting patterns, whether adaptive or maladaptive, shape a child’s expectations for and relationship with their caregivers. While nurturing and supportive environments promote a child’s sense of safety and future prosocial behavior, environments typified by dysfunction (e.g., abuse) or caregiver psychopathology (e.g., PTSD) may contribute to child traumatic stress exposure and mental health problems (Giovanelli & Reynolds, 2021; Sheidow et al., 2014). Theoretical links between caregiver ACEs and adverse childhood outcomes demonstrate the need to explore multiple pathways for intergenerational risk transmission.
Potential Mediators of Caregiver ACEs and Child Internalizing Symptoms
Identifying mechanisms that explain how caregiver ACEs confer greater risk for child internalizing symptoms could inform tailored intervention and prevention efforts to mitigate intergenerational transmission of risk. ACEs reflect cumulative risk, increasing the likelihood that individuals and families will experience negative outcomes (Narayan et al., 2021) thus, it is important to identify factors that span these domains. Specifically, it is crucial to consider how outcomes of caregiver ACEs in the individual (e.g., PTSD) and family (e.g., poor family management) domains impact child internalizing symptoms.
Child ACEs.
Although prior research has established that caregiver ACE exposure increases the risk of child ACEs (e.g., see Narayan et al., 2021 for a review; Schickedanz et al., 2021), only one study to the authors’ knowledge has explored the indirect effect from caregiver early adversity to their child’s mental health outcomes via child adversity (Negriff et al., 2020). However, as previously mentioned, this study only focused on experiences of maltreatment (i.e., physical, sexual, and emotional abuse, and physical neglect) as opposed to a wider range of ACEs. There is a need for studies to assess this mediating effect using the full ACE score, as opposed to individual subtypes, because various types of adversities are thought to impact health outcomes through overlapping risk pathways (Schickedanz et al., 2021; Shonkoff et al., 2012).
Caregiver PTSD and Child ACEs.
Numerous studies have established that childhood trauma can lead to the development of PTSD (Narayan, 2017; Pratchett & Yehuda, 2011; Seng, 2002). Early exposure to potentially traumatic events may have lasting effects that increase risk for PTSD across the lifespan (Yehuda & Meaney, 2018). Caregiver PTSD has been proposed as a mediator between caregiver and child ACEs across generations (Narayan et al., 2021), but has yet to be explored in a larger model encompassing child internalizing symptoms as the primary outcome during adolescence to further delineate this pathway.
It has been found that young children of caregivers who exhibit PTSD symptoms are at higher risk for developing internalizing symptoms (Lambert et al., 2014; Leen-Feldner et al., 2011). Similarly, caregiver PTSD has been found to positively correlate with their child’s depression (Smith et al., 2001) and PTSD symptoms (Davidson & Mellor, 2001). It is possible the presence of PTSD during parenthood inhibits a caregiver’s ability to interpret their children’s signals of distress and to protect them in the context of threat (Lieberman et al., 2020). Certain manifestations of PTSD symptoms (e.g., avoidance, negative mood) may interfere with a caregiver’s ability to identify and seek out the resources and support systems needed to mitigate feelings of stress and isolation that ultimately heighten their children’s risk for ACEs (Chemtob et al., 2013; Seng, 2002). Taken together, the extant literature provides strong rationale for considering a caregiver’s psychopathology within empirical models.
Family Management and Child ACEs.
Early traumatic experiences have also been shown to be predictive of poor parenting later in life, including lower responsivity and empathy, and higher levels of aggression and punitiveness (Banyard et al., 2003; Bert et al., 2009). Narayan and colleagues (2021) posited that early adversity influences later parenting stress, which is likely related to difficulties in parenting. Earlier studies found that mothers with a history of sexual or physical abuse exhibit impaired parenting such as higher levels of child neglect, lower confidence in parenting abilities, and less interest in being a parent (Roberts et al., 2004). Further, children of mothers with a maltreatment history show higher rates of adjustment difficulties and greater risk for experiencing adverse events (Collishaw et al., 2007).
Less is known about the cumulative effects of ACEs on later parenting. The fact that the full ACE measure includes items examining household dysfunction, along with growing evidence to support the intergenerational continuity of parenting styles and subsequent emotional dysfunction (Lomanowska et al., 2017), demonstrates a need to explore the cumulative impact of ACEs beyond replicating prior studies focused only on maltreatment subtypes. Family management style is a key potential mediator of risk pathways leading to child internalizing outcomes that integrate the family environment as a precursor of risk and related outcomes.
Caregiver PTSD, Family Management, and Child ACEs.
While previous studies have investigated pieces of the proposed model, none have examined the serial effect of these factors within a larger model. Empirical and theoretical evidence supports examining the effect of caregiver PTSD on family management to child ACEs as a plausible indirect pathway linking caregiver ACEs to their child’s internalizing outcomes. Ample research exists on the association between ACEs and the short- and long-term development of PTSD (Yehunda & Meaney, 2018), supporting inclusion of caregiver psychopathology as a potential mediating factor. Further, Levendosky and Graham-Bermann (2000) emphasized the importance of expanding current frameworks to include parent mental health as a significant outcome of trauma exposure due to its influence on parenting and child outcomes. Studies have since examined the negative impact of early maltreatment on parenting, including a parent’s ability to establish clear rules and adhere to set guidelines (Banyard et al., 2003; Bert et al., 2009), and while relations between a full ACE score and difficulties parenting have been hypothesized (Narayan et al., 2021), this association warrants further investigation. While less is known about the explicit link between a caregiver’s PTSD and difficulties parenting (van Ee et al., 2016), there is evidence to support that a caregiver’s psychological functioning directly impacts their parenting capabilities (Vivrette et al., 2018) and children’s psychosocial outcomes (Lambert et al., 2014). Additionally, Sheidow and colleagues (2014) found that characteristics of family functioning (e.g., parenting practices and organization) exacerbate the negative link between exposure to external stressors and psychological health of family members.
Synthesis of the extant literature supports the relative importance of investigating the direct and indirect effects of aforementioned factors to further elucidate the complex relation between a caregiver’s exposure to ACEs and adolescent’s internalizing outcomes. A more complete understanding of the effects initiated by a caregiver’s early adversity can inform tailored clinical intervention and prevention efforts for populations at higher risk for ACEs.
Current Study
To develop tailored and culturally informed interventions to prevent and mitigate the detrimental impact of a caregiver’s exposure to ACEs on their child’s mental health outcomes, research is needed that explores these constructs within minoritized populations. The current study addressed gaps in the literature by examining the relation between caregiver ACEs and their child’s PTSD and depression symptoms in a sample of African American dyads living in low-income areas in the Southeastern US. Study aims were to: (a) investigate whether a caregiver ACEs are associated with their child’s self-reported internalizing symptoms, (b) examine caregiver PTSD, child-reported family management problems, and child ACEs as potential mediators of this association, and (c) test all three mediators in a serial mediation model where caregiver ACES are related to caregiver PTSD symptoms, caregiver PTSD symptoms are related to family management problems, family management problems are related to child ACEs, and child ACEs are associated with child PTSD symptoms.
We hypothesized that higher numbers of caregiver ACEs would be associated with higher levels of child PTSD symptoms (hypothesis 1), depressive symptoms (hypothesis 2), and that caregiver PTSD, family management problems, and child ACEs would serially mediate positive associations between caregiver ACEs and child internalizing symptoms, with significant paths from caregiver ACEs to caregiver PTSD to family management problems to child ACE exposure, and finally to both PTSD and depression symptoms (hypothesis 3). This study is among the first to examine serial mediation relations between caregiver ACEs and child PTSD and depression symptoms in a sample of low-income African American dyads living in an urban setting using these particular mediators. Overall, this study provides critical information on a vulnerable group, identifies relations that warrant future study, and furthers the current state of the literature on the intergenerational transmission of ACEs on child internalizing symptoms.
Method
Study Design and Procedure
We used combined cross-sectional survey data collected during two distinct time frames from June 2018 to April 2019 and July 2019 to January 2020. Data at each timepoint were collected from unique adolescents-caregivers dyads residing in three under-resourced urban communities in the Southeastern United States identified as having high rates of poverty and youth violence based on surveillance data. The survey data assessed risk and protective factors for youth violence, and were collected as a part of a project aimed at evaluating community-level approaches to youth violence prevention. All study procedures were approved by the University Institutional Review Board. During the consenting process, we stressed that participants could skip any questions and discontinue the survey at any point. If an adolescent communicated that they were experiencing abuse, we followed mandated reporting guidelines. Information about mandated reporting was included in the adolescent assent and parental consent forms. A neighborhood canvassing approach was used to recruit eligible families and written consent/assent was obtained prior to data collection. A total of 67% of eligible families participated in the study, which is consistent with other community-based studies (e.g., Kliewer et al., 2018). Data were collected using REDcap computer software, and participants entered information on laptop computers with study staff available for questions. Participants completed the surveys using headphones and could opt to skip any question. Surveys were completed primarily in participant homes, and participants received $25 for their time.
Participants
The original sample consisted of 377 caregiver-adolescent dyads. Only participants who self-identified as Black or African American were included in the current study (N = 316). Additionally, 52 dyads were excluded if they had missing data on any key study variables, resulting in a final analytic sample of 273 dyads. Caregivers identified as primarily female (88%) with a mean age of 39 years. For education level, 34% reported achieving less than a high school degree, 35% received their high school degree or GED, and 31% obtained a degree beyond high school. The median yearly household income for our sample was less than $10,000. Over half (57%) of adolescents (ages 12–17) identified as female. All adolescents in the sample qualified for free meals via their school district’s Community Eligibility Provision for the National School Lunch Program.
Measures
Adverse Childhood Experiences.
The ACE Study questionnaire (Dube et al., 2003; Felitti et al., 1998) was completed by both caregivers and adolescent participants to assess ACEs occurring before the age of 18 or lifetime prevalence in the case of the adolescent participants. The scale included 10 items assessing abuse and neglect; witnessing intimate partner violence, parental marital discord, substance abuse, mental illness, and incarceration of a household member. Responses were binary (i.e., “yes” or “no”) and total ‘yes’ scores were summed and ranged from 0 to 10. An example question included “did a parent or other adult in the household often…push, grab, slap, or throw something at you?” Alpha coefficients were .83 and .89 for caregiver and child ACE surveys, respectively. Previous studies have found that retrospective reports of ACEs had good to excellent test-retest reliability (Dube et al., 2003). Additionally, ACEs has been used to measure outcomes in Black children and their parents (Ports et al., 2021), as well as Black families in urban communities (Whiteside-Mansell et al., 2019).
Depression.
The 10-item Center for Epidemiological Studies Depression scale (CES-D; Radloff, 1977) assessed the frequency of adolescents’ depression symptoms during the past week including feelings of frustration, sadness, demoralization, loneliness, and pessimism about the future (e.g., “I was bothered by things that usually don’t bother me”). Participants responded using a 4-point scale ranging from 0 = rarely or none of the time (less than 1 day) to 3 = most or all of the time (5–7 days). Items were summed for a total score, and higher scores indicated greater frequency and number of symptoms. A score of 16 or higher indicated clinical concern. The CES-D demonstrates strong psychometrics in adolescent and adult African American populations (Bradley et al., 2010; Kim et al., 2011), including Black adults, and demonstrated exemplary internal consistency (a = .98) in the current sample.
Family Management Problems.
The 6-item scale from the Communities That Care Survey (CTC; Arthur et al., 2002) measured caregivers’ use of consistent and clear expectations and parental monitoring (e.g., “The rules in my family are clear” and “If you skipped school, would you be caught by your parents?”). Youth selected which choice best described their own family. Response options included: 1= YES!, 2 = yes, 3 = no, 4 = NO!. Items were averaged for a mean score, and the scale demonstrated moderate internal consistency (a = .63) within the current sample. A study conducted by Arthur and colleagues (2002) examining the psychometric properties, found this survey to be reliable across a broad range of ecological contexts. Additionally, the survey has been shown to demonstrate good reliability and validity across racial/ethnic groups, including African American adolescents.
Trauma and Distress.
Adolescent trauma symptoms were assessed using the 26-item Child Report of Posttraumatic Symptoms (CROPS; Greenwald & Rubin, 1999) that was developed using diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders, 4th edition. This scale assessed PTSD symptoms including intrusive thoughts/memories (e.g., “I have bad dreams or nightmares”), psychological arousal (e.g., “I am nervous or jumpy”), and avoidance (e.g., “I avoid reminders of bad things that have happened”). Youth indicated the extent to which they have been experiencing each symptom on a 3-point Likert scale: 0 = None, 1 = Some, and 2 = Lots. Scores were summed and ranged from 0 to 52, such that higher scores indicated a higher level of posttraumatic stress symptoms. Scores of 19 or higher indicated clinical concern. The alpha coefficient was .91. The CROPS has shown good reliability and validity across several settings and populations, including youth in urban communities exposed to community violence (Becker et al., 2011; Greenwald & Rubin, 1999; Greenwald et al., 2002).
Trauma symptoms in caregivers were assessed using the 20-item self-report Posttraumatic Stress Checklist for Diagnostic and Statistical Manual of Mental Disorders, 5th edition (PCL-5; Weathers et al., 2013), which tested for trauma exposure and distress (e.g., “Trouble remembering important parts of the stressful experience”). Caregivers responded to each item following the prompt “In the past month, how much were you bothered by…”. using a 4-point response scale that ranged from 0 = Not at all, 1 to 4 = Extremely. Responses were summed for a total score. A score of 33 or above indicated clinical concern. The reliability and validity of this measure is psychometrically strong (test-retest reliability, r = .84; Bovin et al., 2016; Hoge et al., 2014) with exemplary internal consistency (a = .94) within the current sample. Additionally, this measure has been used previously in non-clinical samples with excellent reliability (a = .95; Moody & Lewis, 2019).
Covariates.
For all analyses, covariates included intervention condition, adolescent age and gender, and caregiver education level. Caregiver education options included: (a) “Attended some grade school but did not go to high school,” (b) “Attended some high school but didn’t graduate,” (c) “Graduated from high school or earned a GED,” (d) “Attended some college, vocational, or trade school but didn’t graduate,” (e) “Graduated from a two-year college, vocational, or trade school,” (f) “Graduated from a four-year college,” (g) “Attended some graduate or professional school after college,” and (h) “Earned a graduate degree (Masters, Ph.D., M.D., J.D., etc.).” Household income was initially considered as an additional covariate due to the potential confounding effect on study variables since all participants lived in a public housing community at the time of data collection. However, preliminary analyses revealed no significant relation between household income and any main variable, thus it was not included.
Data Analysis
Analyses were conducted using SPSS Version 27.0 (IBM Corp, 2020). Prior to running the primary analyses, the data were assessed for assumptions of normality. All data were distributed as expected given the context of the current sample. The skewness and kurtosis of each study variable was examined and determined to fall within acceptable ranges. Data were determined to be missing at random and thus was left as missing due to the similar rates found in other community-based studies (Kliewer et al., 2018). Descriptive statistics were generated to summarize the demographic and risk characteristics of the study population. Primary and secondary hypotheses were tested using separate multiple regression analyses to test possible associations between caregiver ACE scores and their child’s internalizing symptoms. Our third hypothesis was tested using Hayes (2018) serial mediation modeling approach (model 6) to test direct and indirect effects. In addition to testing direct and simple indirect effects, this modeling approach tests serial indirect effects between variables. In the hypothesized models, caregiver ACE scores were entered as the independent variable (IV), either child PTSD or depression was entered as the dependent variable (DV), caregiver PTSD was entered as the first mediator (M1), youth-reported family management problems was entered as the second mediator (M2), and child ACE scores were entered as the third mediator (M3). Separate models were run for each outcome and used the recommended 10000 bootstrapped samples (Hayes, 2013) to estimate indirect effect pathways in accordance with study aims.
Results
Descriptive Statistics
Correlations, means, and standard deviations among study variables can be found in Supplementary Table S1. Over three-fourths (77.5%) of caregivers reported one or more ACE. Parental divorce (61%), substance use (33.8%), and household incarceration (31.2%) were most prevalent. ACE frequencies can be found in Supplemental Table S2. A total of 27.2% of caregivers and 56.1% of adolescent participants met the clinical cutoff for PTSD. Approximately one-third (32.4%) of adolescent participants met the clinical cutoff for depression.
Regression Analyses
Separate regression analyses were conducted to test study hypotheses. After adjusting for covariates, caregiver ACEs was significantly associated with child PTSD (B = .64, p = .007, 95% CI [.18, 1.10]), accounting for 4.9% of the variance in CROPs scores. Caregiver ACEs were not significantly associated with child depression (B = .17, p = .16, CI [−.06, .40]), accounting for 2.6% of the variance in CES-D scores. See Supplementary Table S3 for full regression results.
Serial Mediation Models
Model 1.
In serial association order, the direct associations from caregiver ACEs to child ACEs (b = .10, p < .05) and from child ACEs to child PTSD (b = 1.68, p < .001) were both statistically significant. The indirect effect of caregiver ACEs on child PTSD via child ACEs was also significant (b = .17, 95% CI [.0013, .3651]). See Figure 1.
Figure 1. Serial mediation models with child posttraumatic stress disorder (Model 1) and depression (Model 2) as the outcome.
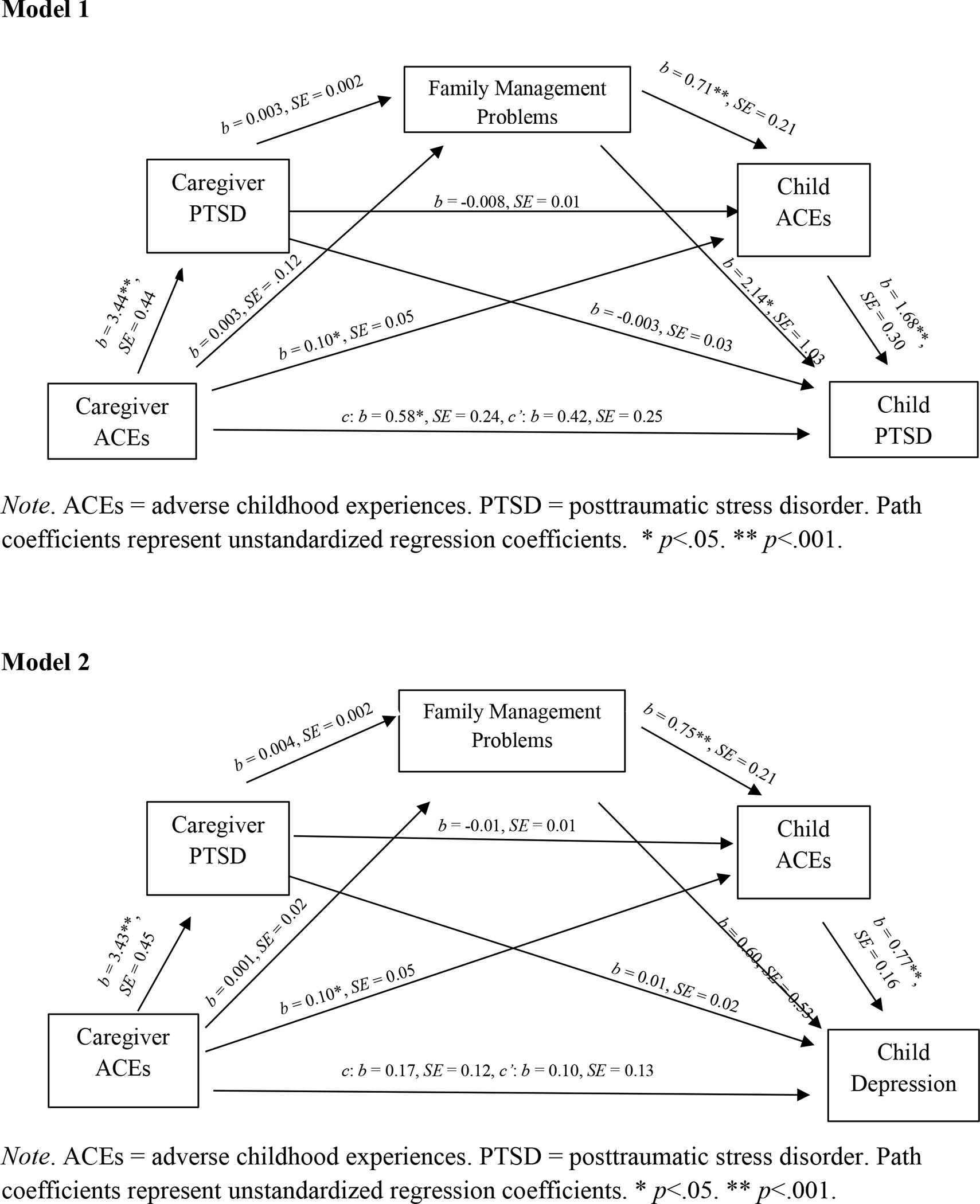
In serial association order, the direct association from caregiver ACEs to caregiver PTSD (b = 3.44, p < .001) was significant, but from caregiver PTSD to child ACES (b = −.01, p = .25) a direct association was not indicated. A significant direct association from child ACEs to child PTSD (b = 1.68, p < .001) was found (Figure 1). Due to the non-significant path from caregiver PTSD to child ACEs, examination of indirect effects was precluded.
In serial association order, the direct association was not significant from caregiver ACEs to family management problems (b = .003, p = .86), but was significant from family management problems to child ACES (b = .71, p < .001); A significant direct association from child ACEs to child PTSD (b = 1.68, p < .001) was found (Figure 1). Due to the non-significant path from caregiver ACEs to family management problems, the indirect effect was not examined.
When all three mediators were examined in serial order within the model, indirect associations for caregiver ACEs to child PTSD were not significant (b = .01, 95% CI [−.0022, .0400]). Remaining direct and indirect pathways are not reported because serial meditation was only hypothesized for models that included a pathway from child ACEs to child PTSD (see Figure 1 for full model).
Model 2.
Significant direct associations were found from caregiver ACEs to child ACEs (b = .10, p < .05) and from child ACEs to child depression (b = .77, p < .001). However, the indirect association of caregiver ACEs on child depression through child ACEs was not significant (b = .10, 95% CI [−.0041, .1710]). See Figure 1.
In serial association order, the direct effect from caregiver ACEs to caregiver PTSD (b = 3.43, p < .001) was significant, whereas the pathway from caregiver PTSD to child ACEs was non-significant (b = −.01, p = .20). There was also a significant direct association from child ACEs to child depression (b = .77, p < .001) (Figure 1). Due to the non-significant path from caregiver PTSD to child ACEs, the indirect effect was not examined.
In serial association order, the direct association was not significant from caregiver ACEs to family management problems (b = .005, p = .97), but significant direct effects were found for family management problems to child ACES (b = 0.75, p < .001) and from child ACEs to child depression (b = .77, p < .001) (Figure 1). Due to the non-significant path from caregiver ACEs to family management problems, examination of indirect effects was precluded.
When all three mediators were examined in serial order, indirect associations for caregiver ACEs to child depression through caregiver PTSD, family management problems, and child ACEs was not significant, (b = 0.01, 95% CI [−0.0004, 0.0212]). Remaining direct and indirect pathways are not reported because serial meditation was only hypothesized for models that included a mediation from child ACEs to child depression (see Figure 1 for full model).
Discussion
This study is among the first to examine: a) the intergenerational impact of caregiver ACEs on child mental health problems via the serial mediation of caregiver PTSD, family management problems, and child ACEs, and b) PTSD as a distal outcome of caregiver cumulative ACE scores. ACE patterns in the current study sample showed that over three-fourths (77.5%) of caregivers reported one or more ACEs, which is higher than estimates in the general population (63.9%; CDC, 2016). Compared to a representative sample of U.S. adults (i.e., CDC-Kaiser ACE Study), caregivers in our sample overall demonstrated higher prevalence rates per item [e.g., emotional abuse (23.2% vs. 10.6%), parental divorce (61% vs. 23.3%), and household incarceration (31.2% vs. 4.7%)]. These discrepancies add to the extant literature that suggests individuals living in areas of concentrated disadvantage, who also experience other systemic issues (e.g., racism), may be at greater risk for ACE exposure (Giovanelli & Reynolds, 2021; Bernard et al., 2021; Hampton-Anderson et al., 2021).
As anticipated, we found a significant association between caregiver ACEs and adolescents’ self-reported PTSD. Over half (56%) of adolescents in the sample met the clinical cut off for PTSD, well above the national estimated lifetime prevalence of PTSD in adolescents (5%; National Institute for Mental Health, 2021). Given that we assessed this relation using a composite ACE score, it is difficult to compare to prior literature focused primarily on child maltreatment (e.g., Negriff et al., 2020). Current findings suggest that adolescents reared by caregivers with a history of ACEs may experience higher levels of PTSD symptoms, reinforcing Masten & Cicchetti’s (2016) emphasis on delineating multiple intergenerational risk pathways.
Contrary to our hypothesis and prior research findings (Doi et al., 2020; Haynes et al., 2020), caregiver ACEs were not significantly associated with adolescent depression symptoms. Despite comparative differences in significant findings, the current study’s use of adolescents’ self-reported symptoms is a considerable strength in relation to studies utilizing caregiver report (e.g., Haynes et al, 2020), due to early evidence that parents’ assessment of their children’s mental health is unreliable, especially as they transition into adolescence (Barrett et al., 1991). The aforementioned research also utilized data drawn from state or international samples and included wider age ranges of child participants (e.g., 8- to 17-years), limiting the generalizability of previous findings to the specific context and developmental period of the current study. Caregiver ACE history might also contribute more heavily to depression in earlier childhood, since adolescent outcomes are more heavily influenced by other external factors (e.g., peers, beginning puberty) and is a developmental period typically associated with an increase in mental health symptoms (NIMH, 2021). Null results could also be attributed to the low prevalence of self-reported clinical levels of depression in our sample (32.4%) compared to rates (47%) found in similar samples (Hammack et al., 2004).
Within the proposed serial mediation models, a significant simple indirect effect provided evidence for the relation between caregiver ACEs and child’s self-reported PTSD (but not depression) symptoms via adolescent ACE exposure. While prior research has focused on child ACE scores as an outcome (e.g., Narayan et al., 2021; Schickedanz et al., 2021), our results support inclusion of child ACEs as a mediator to build empirical support for the intergenerational transmission of ACEs and to examine precursors of a child’s psychological health within the larger context of a caregiver’s developmental history and current functioning. Despite the absence of significant indirect effects for other hypothesized serial mediation paths, several significant direct effects are worth highlighting. In both models, the direct path between family management problems and child ACEs were significant. The family management problems scale (Arthur et al., 2002) in the current study measures aspects of parental monitoring. Thus, adolescents with caregivers who experience difficulties monitoring their adolescents’ behaviors may be more likely to be exposed to traumatic events across contexts (Collishaw et al., 2007). A significant direct effect also emerged for the pathway connecting family management problems to adolescent PTSD, but not depression. The significant pathways found in the current study provide additional empirical rationale for theoretical support of delineating multiple pathways that confer risk (Luthar & Masten, 2021; Masten & Chicchetti, 2016). To the authors’ knowledge, only one prior study has shown family functioning to confer additional risk for negative psychological health that emerged from exposure to external stressors (Sheidow et al., 2014), signifying a continued need to consider the importance of family-level factors. Given the current study’s nonsignificant pathway from family management problems to depression symptoms, it is important to further explore the impact of family management on children’s psychological outcomes within the context of exposure to ACEs.
Despite support for examining parental PTSD as a mediator between caregiver and child ACEs (Narayan et al., 2021), we did not find support for this indirect effect within current models. Serial mediation analyses also showed no significant associations between caregiver PTSD and other study variables aside from caregiver ACEs. However, a trend towards significance is likely for the direct effect of caregiver PTSD on family management in Model 1 (p=.08) and Model 2 (p=.06). It is possible that a larger sample size would help further elucidate this pathway. Additionally, exploring possible associations between distinct symptom manifestations of a caregiver’s PTSD (e.g., hypervigilance, avoidance) and their overall family management tendencies might aid in understanding the negative impact caregiver psychopathology can have on parenting (Vivrette et al., 2018). Additionally, further delineating a caregiver’s own childhood family dynamic and relationship with their caregivers would provide additional insight into how parenting behaviors confer across generations (Bowlby, 1988). We also did not find support for a direct significant association between a caregiver’s ACE scores and adolescent report of family management problems. Including caregiver-report of family management in future studies may help establish a more accurate picture of family functioning and provide further insight into these relations.
Results of the current study adds to the current literature and holds important implications including evidence for the effects of caregiver ACEs intergenerationally and across multiple ecological levels. Given that our sample is exclusively African American dyads residing in areas of concentrated disadvantage, context must be considered when interpreting findings. Bernard and colleagues (2020) presented a culturally informed ACE model to consider the impact of disparities and environmental stressors that exist particularly for African Americans in under-resourced, urban contexts. The proposed model recognizes the historical, intergenerational, and ongoing effects of racism as contributors to the overall biopsychosocial vulnerability of risk for ACEs and the interaction of these and other factors’ influence on health outcomes. Thus, future research conducted with African American dyads should include culturally and contextually relevant adverse experiences (e.g., exposure to community violence, racism) in addition to the conventional ACE items. There is also a continued need to further examine ACE prevalence and ACE-related intergenerational consequences in other distinct African American subgroups (Narayan et al., 2017).
Our findings also emphasize the need to screen caregivers for ACE history during child wellness visits to identify distal risk factors. In the last decade, the American Academy of Pediatrics published guidelines to include screening for ACEs in routine medical visits, including recommendations to assess ACEs in children and parents. However, issues such as feasibility, mandated reporting, and fear of upsetting parents are considered barriers to this practice (Finkelhor, 2018; Gillespie, 2019). In the current study, we included information about mandated reporting in the adolescent assent and parental consent form and this may have contributed to the low lifetime prevalence of exposure to abuse reported by adolescents.
Second, data provide support that being reared by a caregiver with a history of ACEs may increase risk for various deleterious outcomes including their own ACE exposure and subsequent PTSD. Despite research supporting that adolescence is a developmental period typically characterized by increased mental health difficulties (NIMH, 2021), our descriptive findings suggest that African Americans in urban contexts may develop PTSD at higher rates, emphasizing a need to identify factors that may mitigate this consequence of exposure to risk. Additionally, despite null findings for any significant direct effect of caregiver PTSD, the potential importance of this factor should not be ignored, given previous findings of positive correlations between caregiver PTSD and measures of child distress (Lambert et al., 2014), implications for parenting challenges (Muzik et al., 2017), and increased risk for child exposure to adversity (Narayan et al., 2021). Previous findings highlight the need to implement effective intervention and prevention programs aimed to reduce the risk caregiver ACE exposure confers on their psychological health as well as family and child functioning. Current intervention efforts include the use of early intervention (Survivor Mom’s Companion; Sperlich & Seng, 2018), parent management training (Forgatch & Gewirtz, 2017), and family level interventions (Mom Power; Rosenblum et al., 2017) for children at increased risk for deleterious outcomes due to a caregiver’s history of ACEs. Supporting caregivers by providing access to mental health treatment and parent management training before and during parenthood is an important step to mitigating the intergenerational risk of ACEs on psychological, family, and child outcomes.
This study has several limitations that warrant consideration. Although this study allowed us to delineate outcomes that are foundational to further study of intergenerational associations between caregiver adverse experiences and their child’s trauma symptoms, use of cross-sectional data denies the ability to infer causal relations between variables. The CROPSs measure used for the current study was based on the DSM-IV and not the DSM-V, however, it has shown good psychometric properties with samples of youth from low income, urban communities (Becker et al., 2011; Greenwald & Rubin, 1999; Greenwald et al., 2002). Additionally, because our sample primarily consisted of female caregivers, this study was unable to explore possible differences in outcomes of maternal versus paternal ACE exposure. Future research should also consider including other individuals (i.e., grandparents, older siblings) who may take on a caregiving role in the home. Further, despite the novel nature of the study sample within the ACE literature, these findings cannot be generalized to all African American families or to other socio ecological contexts.
Lastly, although we considered three sequential mediating pathways that assessed factors (i.e., caregiver PTSD, family management problems, child ACEs) that may influence relations between caregiver ACE scores and child internalizing symptoms, there are important contextual and environmental factors unable to be adequately addressed including racial discrimination and gun violence, which are known to be elevated in low-income, urban settings (Aufrichtig et al., 2017; Bernard et al., 2021; Hampton-Anderson et al., 2021). Future research should include these potential stressors within analytic models. Lastly, future research should aim to utilize longitudinal data to examine causality between empirically supported outcomes of ACE exposure and intergenerational consequences of risk among African American families living in high burden urban communities, due to the additional risk this context confers.
Conclusion
This study demonstrated the indirect effect of caregiver ACEs on adolescent post-traumatic symptoms via child ACEs and is a departure from most of the present literature that focused primarily on depression symptoms (Doi et al., 2020; Haynes et al., 2020). While the hypothesized indirect effects for overall serial mediation models were not supported, significant paths emerged from family management to child ACEs to both child post-traumatic symptoms and depressive symptoms, highlighting the importance of considering these relations in future studies. Perhaps equally important to the constructs explored in this study is the examination of these associations in a traditionally under researched population of African American families living in high burden urban communities. These findings portray a basis of justification for ACE screening in healthcare settings as a method for early identification and mitigation of intergenerational consequences. By examining intergenerational outcomes associated with ACEs, researchers and mental health professionals will be better able to anticipate and address posttraumatic symptoms.
Supplementary Material
Clinical Impact Statement.
Adverse childhood experiences (ACEs) have a deleterious influence on mental health, yet the impact of this exposure on future generations’ functioning, particularly within urban, African American populations, remains crucial to explore. Findings suggest caregiver exposure to ACEs are associated with their child’s PTSD symptoms. Thus, caregivers and children should be screened for ACEs and subsequent consequences at medical visits. Special attention should be paid to families with caregivers who report exposure to prior trauma and appropriate referrals should be made to mitigate intergenerational consequences of ACEs.
Funding
This study was funded by the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, CDC Cooperative Agreement U01CE002766. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
We have no known conflict of interest to disclose.
References
- Arthur MW, Hawkins JD, Pollard JA, Catalano RF, & Baglioni AJ (2002). Measuring risk and protective factors for substance use, delinquency, and other adolescent problem behaviors: The communities that care youth survey. Evaluation Review, 26(6), 575–601. 10.1177/019384102237850 [DOI] [PubMed] [Google Scholar]
- Aufrichtig A, Beckett L, Diehm J, & Lartey J (2017). CDC WONDER Database. Retrieved from https://efsgv.org/learn/type-of-gun-violence/community-gun-violence/
- Banyard VL, Williams LM, & Siegel JA (2003). The Impact of Complex Trauma and Depression on Parenting: An Exploration of Mediating Risk and Protective Factors. Child Maltreatment, 8(4), 334–349. 10.1177/1077559503257106 [DOI] [PubMed] [Google Scholar]
- Barrett ML, Berney TP, Bhate S, Famuyiwa OO, Fundudis T, Kolvin I, & Tyrer S (1991). Diagnosing childhood depression. Who should be interviewed - Parent or child? The Newcastle Child Depression Project. British Journal of Psychiatry, 159(SUPPL. 11), 22–27. 10.1192/s0007125000292118 [DOI] [PubMed] [Google Scholar]
- Becker J, Greenwald R & Mitchell C (2011). Trauma-Informed Treatment for Disenfranchised Urban Children and Youth: An Open Trial. Child Adolesc Soc Work J 28, 257–272. 10.1007/s10560-011-0230-4 [DOI] [Google Scholar]
- Bernard DL, Calhoun CD, Banks DE, Halliday CA, Hughes-Halbert C, & Danielson CK (2021). Making the “C-ACE” for a Culturally-Informed Adverse Childhood Experiences Framework to Understand the Pervasive Mental Health Impact of Racism on Black Youth. Journal of Child and Adolescent Trauma, 14(2), 233–247. 10.1007/s40653-020-00319-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bert SC, Guner BM, & Lanzi RG (2009). The Influence of Maternal History of Abuse on Parenting Knowledge and Behavior. Family Relations, 58(2), 176–187. 10.1111/j.1741-3729.2008.00545.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Bowlby J (1988). A secure base: Clinical applications of attachment theory. London: Routledge. [Google Scholar]
- Bradley KL, Bagnell AL, & Brannen CL (2010). Factorial validity of the center for epidemiological studies depression 10 in adolescents. Issues in Mental Health Nursing, 31(6), 408–412. 10.3109/01612840903484105 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, Kaiser Permanente. The ACE Study Survey Data [Unpublished Data]. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2016. [Google Scholar]
- Chemtob CM, Gudiño OG, & Laraque D (2013). Maternal posttraumatic stress disorder and depression in pediatric primary care: Association with child maltreatment and frequency of child exposure to traumatic events. JAMA Pediatrics, 167(11), 1011–1018. 10.1001/jamapediatrics.2013.2218 [DOI] [PubMed] [Google Scholar]
- Cicchetti D (2016). Socioemotional, personality, and biological development: Illustrations from a multilevel developmental psychopathology perspective on child maltreatment. Annual Review of Psychology, 67, 187–211. 10.1146/annurev-psych-122414-033259. [DOI] [PubMed] [Google Scholar]
- Collishaw S, Dunn J, O’Connor TG, & Golding J (2007). Maternal childhood abuse and offspring adjustment over time. Development and Psychopathology, 19(2), 367–383. 10.1017/S0954579407070186 [DOI] [PubMed] [Google Scholar]
- Davidson AC, & Mellor DJ (2001). The adjustment of children of Australian Vietnam veterans: Is there evidence for the transgenerational transmission of the effects of war-related trauma? Australian and New Zealand Journal of Psychiatry, 35(3), 345–351. 10.1046/j.1440-1614.2001.00897.x [DOI] [PubMed] [Google Scholar]
- Dekel R, & Goldblatt H (2008). Is There Intergenerational Transmission of Trauma? The Case of Combat Veterans’ Children. American Journal of Orthopsychiatry, 78(3), 281–289. 10.1037/a0013955 [DOI] [PubMed] [Google Scholar]
- Doi S, Fujiwara T, & Isumi A (2021). Association between maternal adverse childhood experiences and mental health problems in offspring: An intergenerational study. Development and Psychopathology, 33(3), 1041–1058. 10.1017/S0954579420000334 [DOI] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, & Anda RF (2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics, 111(3), 564–572. 10.1542/peds.111.3.564 [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258. 10.1016/S07493797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Finkelhor D (2018). Screening for adverse childhood experiences (ACEs): Cautions and suggestions. Child Abuse and Neglect, 85(July 2017), 174–179. 10.1016/j.chiabu.2017.07.016 [DOI] [PubMed] [Google Scholar]
- Forgatch MS, & Gewirtz AH (2017). The evolution of the Oregon model of parent management training. Evidence-based psychotherapies for children and adolescents, 3, 85–102. The Guilford Press. [Google Scholar]
- Giano Z, Wheeler DL, & Hubach RD (2020). The frequencies and disparities of adverse childhood experiences in the U.S. BMC Public Health, 20(1), 1–12. 10.1186/s12889-020-09411-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie RJ, & Folger AT (2017). Feasibility of Assessing Parental ACEs in Pediatric Primary Care: Implications for Practice-Based Implementation. Journal of Child and Adolescent Trauma, 10(3), 249–256. 10.1007/s40653-017-0138-z [DOI] [Google Scholar]
- Giovanelli A, & Reynolds AJ (2021). Adverse childhood experiences in a low-income black cohort: The importance of context. Preventive Medicine, 148, 106557. 10.1016/j.ypmed.2021.106557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser RR, Horn M, Arthur MW, Hawkins JD, & Catalano RF (2005). Measurement properties of the Communities That Care® Youth Survey across demographic groups. Journal of Quantitative Criminology, 21(1), 73–102. 10.1007/s10940-004-1788-1 [DOI] [Google Scholar]
- Goldstein E, Topitzes J, Miller-Cribbs J, & Brown RL (2021). Influence of race/ethnicity and income on the link between adverse childhood experiences and child flourishing. Pediatric Research, 89(7), 1861–1869. 10.1038/s41390-020-01188-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald R, & Rubin A (1999). Assessment of Posttraumatic Symptoms in Children: Development and Preliminary Validation of Parent and Child Scales. Research on Social Work Practice, 9(1), 61–75. 10.1177/104973159900900105 [DOI] [Google Scholar]
- Greenwald R, Rubin A, Jurkovic GJ, Wiedemann J, Russell AM, O’Connor MB, et al. (2002, November). Psychometrics of the CROPS & PROPS in multiple cultures/translations. Poster session presented at the annual meeting of the International Society for Traumatic Stress Studies, Baltimore. [Google Scholar]
- Hammack PL, Richards MH, Luo Z, Edlynn ES, & Roy K (2004). Social support factors as moderators of community violence exposure among inner-city African American young adolescents. Journal of Clinical Child and Adolescent Psychology, 33(3), 450–462. 10.1207/s15374424jccp3303_3 [DOI] [PubMed] [Google Scholar]
- Hampton-Anderson JN, Carter S, Fani N, Gillespie CF, Henry TL, Holmes E, Lamis DA, LoParo D, Maples-Keller JL, Powers A, Sonu S, & Kaslow NJ (2021). Adverse childhood experiences in African Americans: Framework, practice, and policy. The American Psychologist, 76(2), 314–325. 10.1037/amp0000767 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2013, May). Multilevel mediation analysis. In Workshop presented at the annual meeting of the Association for Psychological Science, Washington, DC. [Google Scholar]
- Haynes E, Crouch E, Probst J, Radcliff E, Bennett K, & Glover S (2020). Exploring the association between a parent’s exposure to Adverse Childhood Experiences (ACEs) and outcomes of depression and anxiety among their children. Children and Youth Services Review, 113(April). 10.1016/j.childyouth.2020.105013 [DOI] [Google Scholar]
- Hoge CW, Grossman SH, Auchterlonie JL, Riviere LA, Milliken CS, & Wilk JE (2014). PTSD treatment for soldiers after combat deployment: Low utilization of mental health care and reasons for dropout. Psychiatric Services, 65(8), 997–1004. 10.1176/appi.ps.201300307 [DOI] [PubMed] [Google Scholar]
- IBM Corp. (Released 2020). IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY. [Google Scholar]
- Kim G, DeCoster J, Huang C-H, & Chiriboga DA (2011). Race/ethnicity and the factor structure of the Center for Epidemiologic Studies Depression Scale: A meta-analysis. Cultural Diversity and Ethnic Minority Psychology, 17(4), 381–396. 10.1037/a0025434 [DOI] [PubMed] [Google Scholar]
- Kliewer W, Sosnowski DW, Wilkins S, Garr K, Booth C, McGuire K, & Wright AW (2018). Do Parent-Adolescent Discrepancies Predict Deviant Peer Affiliation and Subsequent Substance Use? Journal of Youth and Adolescence, 47(12), 2596–2607. 10.1007/s10964-018-0879-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert JE, Holzer J, & Hasbun A (2014). Association Between Parents’ PTSD Severity and Children’s Psychological Distress: A Meta-Analysis. Journal of Traumatic Stress, 27(1), 9–17. 10.1002/jts.21891 [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Feldner MT, Bunaciu L, & Blumenthal H (2011). Associations between parental posttraumatic stress disorder and both offspring internalizing problems and parental aggression within the National Comorbidity Survey-Replication. Journal of Anxiety Disorders, 25(2), 169–175. 10.1016/j.janxdis.2010.08.017 [DOI] [PubMed] [Google Scholar]
- Levendosky A, & Graham-Bermann S (2000). Behavioral observations of parenting in battered women. Journal of Family Psychology, 14(1), 80–94. 10.1037/0893-3200.14.1.80 [DOI] [PubMed] [Google Scholar]
- Lieberman AF, Diaz MA, Castro G, & Bucio GO (2020). Make room for baby: Perinatal child-parent psychotherapy to repair trauma and promote attachment. Guilford Publications. [Google Scholar]
- Lomanowska AM, Boivin M, Hertzman C, & Fleming AS (2017). Parenting begets parenting: A neurobiological perspective on early adversity and the transmission of parenting styles across generations. Neuroscience, 342, 120–139. 10.1016/j.neuroscience.2015.09.029 [DOI] [PubMed] [Google Scholar]
- Luthar SS, Cicchetti D, & Becker B (2000). The construct of resilience: A critical evaluation and guidelines for future work. Child Development, 71(3), 543–562. 10.1111/1467-8624.00164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madigan S, Wade M, Plamondon A, & Jenkins J (2015). Maternal abuse history, postpartum depression, and parenting: Links with preschoolers’ internalizing problems. Infant Mental Health Journal, 36(2), 146–155. 10.1002/imhj.21496 [DOI] [PubMed] [Google Scholar]
- Masten AS, & Cicchetti D (2016). Resilience in development: Progress and transformation. In Cicchetti D (Ed.) (3rd ed.,, Vol. 4. Developmental psychopathology (pp. 271–333). New York, NY: Wiley. 10.1002/9781119125556.devpsy406. [DOI] [Google Scholar]
- Masten AS, Lucke CM, Nelson KM, & Stallworthy IC (2021). Resilience in Development and Psychopathology: Multisystem Perspectives. Annual Review of Clinical Psychology, 17, 521–549. 10.1146/annurev-clinpsy-081219-120307 [DOI] [PubMed] [Google Scholar]
- Moody AT, & Lewis JA (2019). Gendered racial microaggressions and traumatic stress symptoms among Black women. Psychology of Women Quarterly, 43(2), 201–214. 10.1177/0361684319828288 [DOI] [Google Scholar]
- Morris A, Gabert-Quillen C, & Delahanty D (2012). The association between parent PTSD/depression symptoms and child PTSD symptoms: A meta-analysis. Journal of Pediatric Psychology, 37(10), 1076–1088. 10.1093/jpepsy/jss091 [DOI] [PubMed] [Google Scholar]
- Murphy A, Dube S, Steele M, & Steele H (2007) Clinical ACE and childclinical ACE questionnaires (Unpublished Manuscript). [Google Scholar]
- Muzik M, Morelen D, Hruschak J, Rosenblum KL, Bocknek E, & Beeghly M (2017). Psychopathology and parenting: An examination of perceived and observed parenting in mothers with depression and PTSD. Journal of Affective Disorders, 207, 242–250. 10.1016/j.jad.2016.08.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayan AJ (2017). Intergenerational continuity of adverse childhood experiences in high-risk families. Dissertation Abstracts International: Section B: The Sciences and Engineering, 78(2-B(E)), No-. [Google Scholar]
- Narayan AJ, Lieberman AF, & Masten AS (2021). Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clinical Psychology Review, 85(February), 101997. 10.1016/j.cpr.2021.101997 [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. (2021). Post-Traumatic Stress Disorder (PTSD): Definition. National Institutes of Health (NIH), U.S. Department of Health and Human Services. Retrieved from https://www.nimh.nih.gov/health/statistics/post-traumatic-stress-disorder-ptsd [Google Scholar]
- Negriff S, Palmer Molina A, & Hackman DA (2020). Parental Exposure to Childhood Maltreatment and Offspring’s Mental Health: Investigating Pathways Through Parental Adversity and Offspring Exposure to Maltreatment. Child Maltreatment, 25(4), 422–432. 10.1177/1077559520912342 [DOI] [PubMed] [Google Scholar]
- Ports KA, Tang S, Treves-Kagan S, & Rostad W (2021). Breaking the cycle of Adverse Childhood Experiences (ACEs): Economic position moderates the relationship between mother and child ACE scores among Black and Hispanic families. Children and youth services review, 127, 106067. 10.1016/j.childyouth.2021.106067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratchett LC, & Yehuda R (2011). Foundations of posttraumatic stress disorder: Does early life trauma lead to adult posttraumatic stress disorder? Development and Psychopathology, 23(2), 477–491. 10.1017/S0954579411000186 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Roberts R, O’Connor T, Dunn J, & Golding J (2004). The effects of child sexual abuse in later family life; mental health, parenting and adjustment of offspring. Child Abuse and Neglect, 28(5), 525–545. 10.1016/j.chiabu.2003.07.006 [DOI] [PubMed] [Google Scholar]
- Rosenblum KL, Muzik M, Morelen DM, Alfafara EA, Miller NM, Waddell RM, Schuster MM, & Ribaudo J (2017). A community-based randomized controlled trial of Mom Power parenting intervention for mothers with interpersonal trauma histories and their young children. Archives of Women’s Mental Health, 20(5), 673–686. 10.1007/s00737-017-0734-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schickedanz A, Escarce JJ, Halfon N, Sastry N, & Chung PJ (2021). Intergenerational Associations between Parents’ and Children’s Adverse Childhood Experience Scores. Children, 8(9), 747. 10.3390/children8090747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schickedanz A, Halfon N, Sastry N, & Chung PJ (2018). Parents’ adverse childhood experiences and their children’s behavioral health problems. Pediatrics, 142(2). 10.1542/peds.2018-0023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schofield TJ, Brent Donnellan M, Merrick MT, Ports KA, Klevens J, & Leeb R (2018). Intergenerational continuity in adverse childhood experiences and rural community environments. American Journal of Public Health, 108(9), 1148–1152. 10.2105/AJPH.2018.304598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS (2002). A conceptual framework for research on lifetime violence, posttraumatic stress, and childbearing. Journal of Midwifery and Women’s Health, 47(5), 337–346. 10.1016/S1526-9523(02)00275-1 [DOI] [PubMed] [Google Scholar]
- Sheffler JL, Stanley I, & Sachs-Ericsson N (2020). ACEs and mental health outcomes. In Adverse Childhood Experiences (pp. 47–69). Elsevier. 10.1016/B978-0-12-816065-7.00004-5 [DOI] [Google Scholar]
- Sheidow AJ, Henry DB, Tolan PH, & Strachan MK (2014). The Role of Stress Exposure and Family Functioning in Internalizing Outcomes of Urban Families. Journal of Child and Family Studies, 23(8), 1351–1365. 10.1007/s10826-013-9793-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, McGuinn L, Pascoe J, Wood DL, High PC, Donoghue E, Fussell JJ, Gleason MM, Jaudes PK, Jones VF, Rubin DM, Schulte EE, Macias MM, Bridgemohan C, Fussell J, … Wegner LM (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1). 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- Smith P, Perrin S, Yule W, & Rabe-Hesketh S (2001). War Exposure and Maternal Reactions in the Psychological Adjustment of Children from Bosnia-Hercegovina. Journal of Child Psychology and Psychiatry, 42(3), 395–404. 10.1111/1469-7610.00732 [DOI] [PubMed] [Google Scholar]
- Sperlich M, & Seng J (2018). Survivor Mom’s Companion: A Population-Level Program for Pregnant Women Who Are Survivors of Childhood Maltreatment: The Need for a Public Health Approach to Addressing Unresolved Maternal Trauma (pp. 197–211). 10.1007/978-3-319-65724-0_13 [DOI] [Google Scholar]
- Stepleton K, Bosk EA, Duron JF, Greenfield B, Ocasio K, & MacKenzie MJ (2018). Exploring associations between maternal adverse childhood experiences and child behavior. Children and Youth Services Review, 95(July), 80–87. 10.1016/j.childyouth.2018.10.027 [DOI] [Google Scholar]
- Thompson RA (2000). The legacy of early attachments. Child Development, 71, 145–152. 10.1111/1467-8624.00128. [DOI] [PubMed] [Google Scholar]
- van Ee E, Kleber RJ, & Jongmans MJ (2016). Relational Patterns Between Caregivers With PTSD and Their Nonexposed Children: A Review. Trauma, Violence, and Abuse, 17(2), 186–203. 10.1177/1524838015584355 [DOI] [PubMed] [Google Scholar]
- Vivrette RL, Briggs EC, Lee RC, Kenney KT, Houston-Armstrong TR, Pynoos RS, & Kiser LJ (2018). Impaired Caregiving, Trauma Exposure, and Psychosocial Functioning in a National Sample of Children and Adolescents. Journal of Child and Adolescent Trauma, 11(2), 187–196. 10.1007/s40653-016-0105-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The ptsd checklist for dsm-5 (pcl-5). Scale available from the National Center for PTSD at www.ptsd.va.gov
- Whiteside-Mansell L, McKelvey L, Saccente J, & Selig JP (2019). Adverse childhood experiences of urban and rural preschool children in poverty. International journal of environmental research and public health, 16(14), 2623. 10.3390/ijerph16142623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R, Halligan SL, & Grossman R (2013). Childhood trauma and risk for PTSD: Relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. The Science of Mental Health: Stress and the Brain, 9, 177–197. [DOI] [PubMed] [Google Scholar]
- Yehuda R, & Meaney MJ (2018). Relevance of Psychological Symptoms in Pregnancy to Intergenerational Effects of Preconception Trauma. Biological Psychiatry, 83(2), 94–96. 10.1016/j.biopsych.2017.10.027 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


