ABSTRACT
Young adult patients with symptomatic acetabular dysplasia and marginal secondary osteoarthritis can be faced with the decision to either undergo periacetabular osteotomy (PAO) to relieve symptoms and slow osteoarthritis progression or wait until progression to more advanced disease and undergo total hip arthroplasty (THA). The decision can be difficult, and contemporary literature to guide these decisions is sparse. Therefore, we retrospectively assessed complication rate, survivorship and patient-reported clinical outcomes [modified Harris Hip score (mHHS), UCLA Activity score] in two, consecutive cohorts of patients aged 18–40 years that underwent either PAO for symptomatic acetabular dysplasia (mean age 28.9 years) or THA for advanced secondary osteoarthritis (32.5 years). PAO patients were followed for a mean of 10.5 years (8–19) and THA patients for 11.9 (8–17) years. Between PAO and THA groups, there were no differences in overall complication rate (4.7% versus 4.7%), non-revision reoperation rate (5.9% versus 2.3%, P = 0.37) or end-revision rate [7 (8.2%) PAOs converted to THA at mean 10.8 years versus 3 (7.0%) THAs revised at 6.2 years, P = 0.80]. Latest scores remained significantly improved from baseline in both the PAO (mHHS 86.1 versus 63.3, P < 0.001; UCLA 7.5 versus 6.9, P < 0.05) and THA (mHHS 82.6 versus 48.4, P < 0.001; UCLA 7.2 versus 4.6, P < 0.001) cohorts. Final scores were similar between groups (mHHS 86.1 versus 82.6, P = 0.46; UCLA 7.5 versus 7.2, P = 0.37). Clinical success [mHHS minimal clinically important difference (8) OR PASS (>70) at latest follow-up without end-revision] was achieved in 81.2% of PAO hips and 83.7% of THA hips (P = 0.72).
INTRODUCTION
Acetabular dysplasia is a condition of considerable prevalence found in as many as 50% of hips with early degenerative disease and is defined by insufficient acetabular coverage of the femoral head [1]. In addition to pain and variable hip instability, this morphology has been directly associated with increased loading of the acetabular rim, local chondrolabral injury and frequent progression to more global secondary osteoarthritis—often by an early age [2, 3].
Despite the efficacy of modern hip arthroplasty in the treatment of end-stage osteoarthritis, its use in younger patients may come with considerable lifetime risk of revision surgery and suboptimal long-term outcomes [4–6]. In skeletally mature patients without advanced secondary osteoarthritis, attempts can be made to improve the geometry of the native joint to alleviate symptoms, slow degenerative change and delay the potential need for arthroplasty until an age at which long-term outcomes may be more favorable [7, 8].
The mainstay surgical treatment for achieving this goal remains the periacetabular osteotomy (PAO) first described by Ganz et al. [9, 10]. The PAO attempts to normalize acetabular coverage of the femoral head through a series of osteotomies that provide complete mobility of the acetabular fragment. Reorientation of the acetabulum relative to the femoral head is then performed, medializing the joint and compensating for version abnormalities and deficiencies in femoral head coverage. PAO has been shown to achieve not only short-term improvements in pain, function and quality of life [11–16] but also potentially significant prolongation of the time to eventual need for joint replacement [17–20]. Since the time of many of these studies, PAO surgery has evolved significantly [21–27]. While shorter-term reports of contemporary PAO outcomes have demonstrated good results, mid- to long-term data remain more limited [28]. THA surgery has similarly evolved, with modern fixation and bearing materials offering potential reductions in the high rates of wear and loosening-related failure historically associated with THA in younger, more active patients.
Patients with symptomatic acetabular dysplasia and marginal secondary osteoarthritis can be faced with the decision to either undergo PAO to relieve symptoms and slow osteoarthritis progression or wait until progression to more advanced disease and undergo total hip arthroplasty (THA). Previously, we compared outcomes of PAO (for symptomatic acetabular dysplasia) and THA (for advanced secondary osteoarthritis) in two cohorts of patients aged 18–40 years at minimum 2-year follow-up and found no difference in complication rates or patient-reported outcome scores between groups [29]. To date, however, there has remained a paucity of longer-term comparative outcome data for these contemporary surgeries by which decision-making might be better guided. Such data will provide additional information regarding PAO safety, outcomes and survivorship relative to THA. The purpose of the current study was therefore to define and compare longer-term outcomes (minimum 8-year follow-up) in these same two, previously established cohorts.
METHODS
Institutional review board approval was obtained for this study. A prospective institutional database was then retrospectively reviewed for all patients of a single surgeon who underwent either PAO for symptomatic acetabular dysplasia or THA for advanced secondary osteoarthritis between 2000 and 2009 at the age of 18–40 years. Out of the initially identified 130 PAO hips, 5 had prior ipsilateral pelvic or proximal femoral osteotomy and 25 were second-side surgeries in bilateral patients and were excluded. Out of the initially identified 69 THA hips, 2 had prior ipsilateral PAO and 12 were second-side surgeries and were excluded. Of the remaining 100 PAO hips (100 patients), 85 (85%) had available minimum 8-year follow-up [mean 10.5 (8–19) years]. Of the remaining 55 THA hips (55 patients), 43 (78%) had minimum 8-year follow-up [mean 11.9 (8–17) years]. These 85 PAO and 43 THA patients were the focus of the current study.
Among PAO surgeries, one or more concomitant procedure was performed in 72 (85%) cases. These included femoral head–neck osteochondroplasty (42 hips, 49%), labral repair or resection (9, 11%) and intertrochanteric osteotomy (2, 2%). All THAs were performed through a posterolateral approach. Cementless femoral and acetabular components were used in all cases and highly-crosslinked polyethylene liners in 96% of cases. Femoral heads were cobalt chrome (31%), alumina ceramic (42%) and biolox ceramic (27%).
A retrospective chart review was conducted for each patient to the latest follow-up, and all complications and reoperations were recorded. For the purpose of this study, complications reported were only those involving deviation from expected postoperative clinical course requiring pharmacological or surgical intervention (‘major complication’). For both groups, recommended routine follow-up after the first postoperative year included 2-, 5- and 10-year clinical appointments. For patients between 5- and 10-year appointments or who had not been seen for more than 2 years since their 10-year appointment, every effort was made to obtain recent follow-ups—including by-mail and by-phone outcome questionnaires. In the THA group, the latest follow-up was by clinical appointment in 38% of patients and by phone in 62% of patients. In the PAO cohort, latest follow-up was by clinical appointment in 44% of patients and by phone in 56% of patients.
Clinical outcomes were assessed using the modified Harris Hip score (mHHS) and UCLA activity score, both of which were collected for every included patient at the latest follow-up for comparison with preoperative scores. In PAO patients that underwent reoperation for persistent symptoms or THA conversion, and in THA patients that underwent revision THA, scores collected prior to these re-interventions were instead assessed. The primary outcome measure, the mHHS, was additionally assessed relative to the minimal clinically important difference (MCID) (mHHS improvement of 8) and patient-acceptable symptom state (PASS) (mHHS final score >70) [30].
Pre- and postoperative radiographs were reviewed by a surgeon with experience in radiographic evaluation of the young adult hip, independently of the treating surgeon. For hips in the PAO cohort, pre- and postoperative measurements included Tonnis and lateral center edge angle (LCEA) on AP pelvic view, and anterior center edge angle (ACEA) on false profile view [31]. For hips in the THA cohort, postoperative acetabular component abduction angles were measured [32]. Preoperative Tonnis grades in the surgical hip were assigned for all patients of both groups. All continuous radiographic measures were analyzed with intraclass correlation coefficients (ICCs). ICCs were calculated using a two-way random model for single measurement with absolute testing. All measurements demonstrated high or very high agreement (ICC 0.96 for LCEA, 0.91 for Tonnis angle and 0.99 for ACEA).
Statistical analysis
Comparisons between treatment groups were performed using student t-tests for continuous variables (age, BMI, outcome scores) and chi-squared tests for categorical variables (sex, Tonnis Grade, clinical outcome states). A P-value <0.05 defined significance.
RESULTS
The final PAO group included 85 hips [age 29 (18–40) years, BMI 25 (18–34), 73% female] followed for a mean of 11.9 (8–17) years and the final THA group 43 hips [age 32 (18–40) years, BMI 27 (18–35), 65% female] followed for 10.5 (8–19) years.
Consistent with the differed indications for each procedure, at the time of index surgery, hips in the THA cohort were slightly older than those in the PAO cohort (32.5 versus 28.9 years, P = 0.004) and had significantly more extensive preoperative osteoarthritis as approximated by Tonnis Grade (P < 0.001). This was reflected in the THA cohort’s lower preoperative mHHS (48.4 versus 63.3, P < 0.001) and UCLA activity (4.6 versus 6.9, P < 0.002) scores, as compared with hips in the PAO cohort (Table I).
Table I.
Preoperative patient characteristics
| Variable | PAO (n = 85) | THA (n = 43) | P-value | ||
|---|---|---|---|---|---|
| Age | 28.9 | (SD 7.5) | 32.5 | (SD 6.3) | 0.004 |
| BMI | 25.4 | (SD 3.7) | 27.0 | (SD 4.4) | 0.02 |
| Female | 74% | 64% | 0.24 | ||
| mHHS | 63.3 | (SD 10.5) | 48.4 | (SD 12.3) | <0.001 |
| UCLA | 6.9 | (SD 2.5) | 4.6 | (SD 2.0) | <0.001 |
| Tonnis | n (%) | n (%) | <0.001 | ||
| Grade 0 | 26 (35) | – | |||
| Grade 1 | 42 (57) | – | |||
| Grade 2 | 5 (7) | 19 (44) | |||
| Grade 3 | 1 (1) | 24 (56) | |||
In the PAO group, all radiographic measures of dysplasia improved significantly postoperatively. Mean LCEA improved from 8.0° ± 9.2 to 29.4° ± 7.8 (P < 0.001), ACEA from 6.8° ± 13.5 to 30.5° ± 9.8 (P < 0.001) and Tönnis angle from 22.6° ± 8.6 to 6.3° ± 5.6 (P < 0.001). In the THA group, mean acetabular component abduction angle was 44.3o.
Complications were experienced at a rate of 4.7% in the PAO cohort (n = 4) and 4.7% in the THA cohort (n = 2). In the PAO cohort, these included (i) one femoral deep vein thrombosis treated with inferior vena cava filter and long-term anticoagulation, (ii) one wound hematoma requiring surgical evacuation, (iii) one acetabular fracture within 2 postoperative weeks that was open reduced and internally fixed in the third postoperative week (later converted to THA at 1.3 years due to osteoarthritis (OA) progression) and (iv) one loss of acetabular reduction in a patient noncompliant with weight-bearing precautions and smoking cessation that required revision at 6 postoperative weeks (recovered without further sequalae but went on to convert to THA at 19 years due to OA progression). In the THA cohort, complications included: (i) one hematoma requiring surgical evacuation and (ii) one deep infection within 6 postoperative weeks treated with surgical irrigation and debridement with head and liner exchange.
Five (5.9%) PAO patients underwent reoperation other than THA conversion, and one (2.3%) THA patient underwent reoperation other than THA revision (P = 0.37). Reoperations among PAO patients included: (1–4) four hip arthroscopies (one with femoral osteochondroplasty) at 1.8, 3.2, 5.2 and 7.3 years and (5) one psoas tendon lengthening for psoas tendinitis at 0.8 years. The one reoperation among patients in the THA group was a psoas tendon lengthening at 2.0 years.
By the latest follow-up, seven (8.2%) PAO patients had converted to THA at a mean of 10.8 years (one due to the above-noted failure of fixation at <6 weeks, and the remainder due to progression of joint degeneration and unsatisfactory function), and three (7.0%, P = 0.80) THA patients had undergone revision THA at a mean of 6.2 years (one for periprosthetic infection within 6 postoperative weeks, one for acetabular component loosening and one for wear with osteolysis) (Figs 1–2).
Fig. 1.
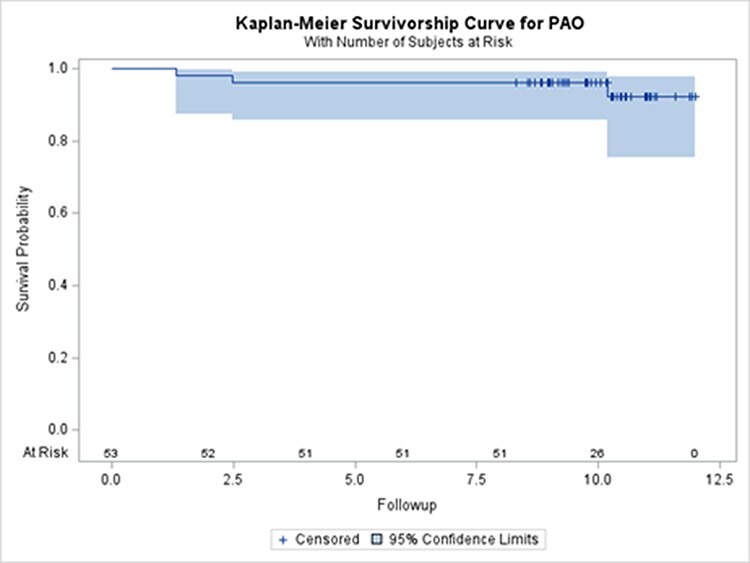
PAO Cohort—Survival freee from THA conversion.
Fig. 2.
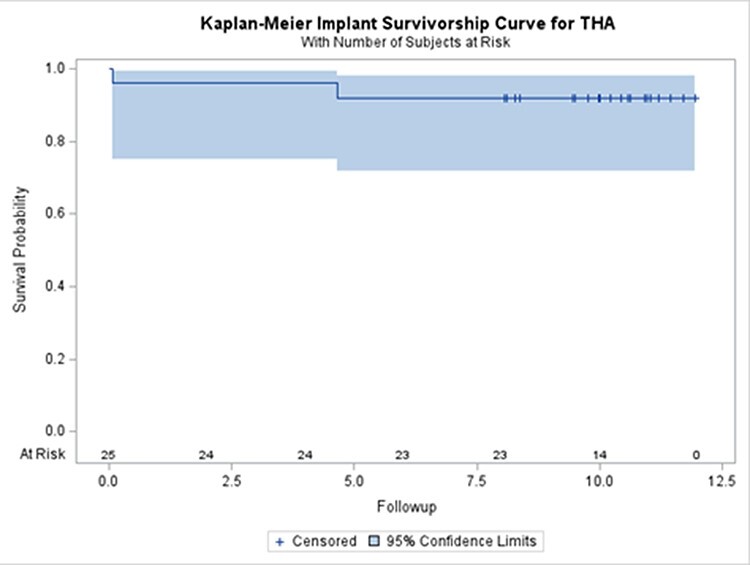
THA Cohort—Survival free from THA revision.
Outcome scores at the latest follow-up continued to reflect considerable improvements from preoperative baseline in both the PAO (mHHS 86.1 versus 63.3, P < 0.001; UCLA 7.5 versus 6.9, P < 0.05) and THA (mHHS 82.6 versus 48.4, P < 0.001; UCLA 7.2 versus 4.6, P < 0.001) cohort. The latest scores were not significantly different between PAO and THA groups (mHHS 86.1 versus 82.6, P = 0.46; UCLA 7.5 versus 7.2, P = 0.37). Clinical success at the latest follow-up defined as mHHS MCID (8) or PASS (>70) without reoperation for persistent symptoms or end-revision was achieved in 81.2% hips in the PAO cohort and 83.7% of hips in the THA cohort (P = 0.72). (Table II)
Table II.
Clinical outcomes
| Variable | PAO group (n = 85) | THA group (n = 43) | P-value (between groups) |
|---|---|---|---|
| mHHS | |||
| Preoperative | 63.3 (SD 10.5) | 48.4 (SD 12.3) | <0.001 |
| Postoperative | 86.1 (SD 14.7) | 82.6 (SD 22.9) | 0.46 |
| change | 23.1 | 34.2 | 0.002 |
| P-value (within groups) | <0.001 | <0.001 | |
| MCID (8) | 67 (78.8%) | 36 (83.7%) | 0.51 |
| PASS (>70) | 65 (76.5%) | 30 (69.8%) | 0.41 |
| MCID OR PASS | 69 (83.7%) | 36 (81.2%) | 0.72 |
| UCLA Activity Score | |||
| Preoperative | 6.9 (SD 2.5) | 4.6 (SD 2.0) | <0.001 |
| Postoperative | 7.5 (SD 2.1) | 7.2 (SD 2.2) | 0.37 |
| change | 0.6 | 2.6 | 0.004 |
| P-value (within groups) | <0.05 | <0.001 | |
| Categorical | |||
| Preoperative | |||
| 8 to 10 | 30% | 8% | 0.007 |
| 6 to 8 | 17% | 14% | |
| 6 or less | 53% | 78% | |
| Postoperative | |||
| 8 to 10 | 42% | 35% | 0.22 |
| 6 to 8 | 13% | 25% | |
| 6 or less | 45% | 40% | |
PAO hips that converted to THA (n = 7) had similar outcome scores pre- and post-THA compared with hips in the THA-only cohort (n = 43). Pre-THA functional scores were very similar between groups (mHHS 48.5 versus 48.4, P = 0.98). Pre-THA UCLA Activity scores were slightly higher in those with prior PAO, although this difference did not reach significance (5.4 versus 4.6, P = 0.47). At a mean of 5.7 years (1–15) after THA conversion, hips with prior PAO had a mean mHHS improvement of 44.1 points (mean final score 92.6) [versus +34.2 points (mean final score 82.6) in the THA-only group; P = 0.45] and a mean UCLA improvement of 1.2 points (mean final score 6.6) (versus +2.6, mean final score 7.2 in the THA-only group; P = 0.22). There were no complications or reoperations following THA conversion in any of the seven converted hips at the latest follow-up. (Table III)
Table III.
Clinical outcomes of THA (PAOs that converted to THA versus THA-only group)
| Variable | THA Conversion group (n = 7) |
THA group
(n = 43) |
P-value (between groups) |
|---|---|---|---|
| mHHS | |||
| Preoperative | 48.5 (SD 15.2) | 48.4 (SD 12.3) | 0.98 |
| Postoperative | 92.6 (SD 9.4) | 82.6 (SD 22.9) | 0.41 |
| change | 44.1 | 34.2 | 0.45 |
| P-value (within groups) | <0.001 | <0.001 | |
| MCID (8) | (100%) | 36 (83.7%) | – |
| PASS (>70) | (100%) | 30 (69.8%) | – |
| MCID OR PASS | (100%) | 36 (81.2%) | – |
| UCLA Activity Score | |||
| Preoperative | 5.4 (SD 2.7) | 4.6 (SD 2.0) | 0.47 |
| Postoperative | 6.6 (SD 2.4) | 7.2 (SD 2.2) | 0.68 |
| change | 1.2 | 2.6 | 0.22 |
| P-value (within groups) | <0.05 | <0.001 | |
DISCUSSION
Patients with acetabular dysplasia and marginal secondary osteoarthritis may be faced with the decision to either undergo PAO to relieve symptoms and slow osteoarthritis progression or wait until progression to more advanced disease and undergo THA. Despite the efficacy of modern hip arthroplasty in the treatment of end-stage osteoarthritis, its use in younger patients may come with a considerable risk of revision surgery and suboptimal long-term outcomes [4–6]. Younger age alone is an important factor when lifetime risk of revision is considered. Each additional revision comes with compounding risk of poor outcomes, complications and the possibility of bone stock loss complicating further surgery. PAO attempts to temper these risks by delaying the potential need for arthroplasty until an age at which long-term outcomes may be more favorable [7].
Although mid- to long-term outcomes have been reported for both procedures, comparative outcome data for young patients with hip dysplasia remain very limited. Furthermore, key refinements of both THA [33] and PAO [21–27] have taken place since the time of the surgeries examined by many longer-term studies, which may limit the applicability of their findings to the modern patient. A recent meta-analysis of the contemporary comparative PAO/THA literature found only four studies that compared outcomes at greater than 4-year mean follow-up (mean 5.8 years in these four studies) [34]. Across these, mean PAO cohort size was limited to 34 hips [14–62] and mean age at PAO surgery was >40 years.
Outcome comparisons between PAO and THA surgery are of greatest relevance to patients with marginal secondary osteoarthritis, of ages at which good PAO outcomes have been most reliably achieved (<40) [17, 35] and at which lifetime risk of revision and subsequent poor outcomes with THA are of most concern. The current study’s 85 PAO patients with limited osteoarthritis (92% Tonnis Grade <2) and a mean age of 29 years are representative of the population most likely to encounter this decision between PAO or later THA, and for which the potential benefit of PAO is theoretically greatest. While shorter-term PAO outcomes in similar populations have been encouraging [28], fuller confidence in the decision to pursue PAO is dependent upon understanding how reliably satisfactory function is maintained up to the ages at which THA outcomes may be more predictable and lifetime revision risk is less. Specifically for these patients, this requires comparative data up to and beyond 10 postoperative years.
The current study found that for patients in this young to middle-age, marginal OA population, modern PAO can reliably achieve durable improvements in pain, function and activity out to and beyond 10 postoperative years. Differences between PAO and THA groups at this interval were insignificant with respect to survival (end-stage revision rate 8.2% versus 7.0%, P = 0.80), function (postop mHHS, P = 0.46) and activity (postop UCLA, P = 0.37). Despite similar final scores between groups, mean score improvements were greater among THA hips due to their relatively advanced disease, poor function and low activity at the time of index surgery. This was an unavoidable and expected consequence of the indications for favoring THA over PAO being chiefly those of disease severity. The more clinically valuable observation across these two cohorts was that the similarly satisfactory postoperative function achieved in both was durable over the 10-year postoperative interval for which direct comparative data has to date been lacking. Compared to the scores we reported previously in these same two cohorts at a minimum 2-year follow-up, scores in the current study were relatively unchanged with respect to both mHHS (PAO 86.5 versus 86.1 at 11.9 years; THA 80.2 versus 82.6 at 10.5 years) and UCLA Activity (PAO 7.5 versus 7.5 at 11.9 years; THA 6.6 versus 7.2 at 10.5 years).
These results are consistent with prior comparative studies which—although all at significantly shorter follow-up—reported similarly insignificant differences between PAO and THA groups [36–38]. A recent meta-analysis including these studies [34] found this to be true at 5.8-year mean follow-up with respect to rates of overall complication [OR 2.14 (95% CI 0.58–7.96), P = 0.26], major complication [OR 2.56 (95% CI 0.60–10.98), P = 0.21] and end-stage revision [OR 0.95 (95% CI 0.33–2.79) P = 0.93]. Postoperative WOMAC function scores were also similar between groups [standard mean difference −0.16 (95% CI −1.29–0.97), P = 0.78]. Postoperative WOMAC pain scores were higher among THA hips [standard mean difference −0.57 (95% CI −0.93–−0.21), P = 0.002], although this was likely a function of the more severe disease and pain seen preoperatively in the THA patients, as the authors themselves pointed out. Interestingly, postoperative UCLA Activity scores were significantly higher in PAO hips [standard mean difference 0.28, (95% CI 0.02–0.53), P = 0.03]. While the current study observed a similar difference in postoperative UCLA Activity scores between PAO (7.5 ± 2.1) and THA (7.2 ± 2.2) hips, this difference did not reach statistical significance (P = 0.37).
This study has several limitations. Firstly, the two cohorts are not matched and differ in preoperative levels of pain and function, as well as the severity of disease and OA. However, we feel that with these two operations it is impractical to perform a randomized controlled trial since the indications are different. THA has long been the accepted standard treatment for end-stage symptomatic disease of the hip because of its established clinical efficacy and safety profile. Therefore, its inclusion in this study was more as a benchmark for the performance of PAO. The differing indication for either PAO or THA procedures also made a direct, matched comparison of dysplastic hips with similar disease characteristics impractical. A second limitation is whether the results for a single surgeon’s series from a single, high-volume institution could be generalized. Given the learning curve associated with the PAO, one must consider this limitation when interpreting our results.
Consideration of multiple patient and disease-specific factors is important for both the surgeon and patient in making a well-informed treatment decision. In patients with relatively preserved joint space, early cartilage disease on magnetic resonance imaging and preserved hip range of motion, we prefer PAO surgery if the patient is healthy, well-conditioned and interested in joint preservation surgery. In patients with more advanced articular cartilage disease, extensive subchondral edema and/or cystic changes, early loss of hip range of motion, significant comorbidities and less enthusiasm for joint preservation surgery we are more likely to advocate THA.
Until the lifetime risk of multiple revisions and suboptimal long-term outcomes in young THA patients are better understood, the 10-year durability of satisfactory function achieved with PAO observed by the current study may further support a preference for PAO in a well-selected subgroup of patients with symptomatic acetabular dysplasia. Major complications with PAO were no more common than in the THA comparison group, and PAO surgery appeared to have no deleterious effect on subsequent THA outcomes in the subgroup of PAO hips that converted to THA during the study period.
Contributor Information
Frank W Parilla, Department of Orthopaedic Surgery, Washington University School of Medicine, Campus Box 8233, 660 S. Euclid Ave., Saint Louis, MO 63110, USA.
Serena Freiman, Department of Orthopaedic Surgery, Washington University School of Medicine, Campus Box 8233, 660 S. Euclid Ave., Saint Louis, MO 63110, USA.
Gail E Pashos, Department of Orthopaedic Surgery, Washington University School of Medicine, Campus Box 8233, 660 S. Euclid Ave., Saint Louis, MO 63110, USA.
Susan Thapa, Department of Orthopaedic Surgery, Washington University School of Medicine, Campus Box 8233, 660 S. Euclid Ave., Saint Louis, MO 63110, USA.
John C Clohisy, Department of Orthopaedic Surgery, Washington University School of Medicine, Campus Box 8233, 660 S. Euclid Ave., Saint Louis, MO 63110, USA.
DATA AVAILABILITY
The data underlying this article will be shared on reasonable request to the corresponding author.
FUNDING
This work was supported by the Curing Hip Disease Fund (JCC), the Jacqueline & W. Randolph Baker Fund (JCC), The Foundation for Barnes-Jewish Hospital (JCC, Award Reference 5228), Once Upon a Time (JCC) and the Jacqueline & W. Randolph Baker Research Fellowship Fund (JCC).
CONFLICT OF INTEREST STATEMENT
Nepple: Arthroscopy: editorial or governing board; Pediatric Research in Sports Medicine Society: board or committee member; Responsive: IP royalties; Responsive Arthroscopy: Paid consultant; Smith & Nephew: paid consultant; paid presenter or speaker; research support; Zimmer: Research support Pashos: GlaxoSmithKline: stock or stock Options Clohisy: Department of Defense grant: Research support; Hip Society: Board or committee member; International Society for Hip Arthroscopy: Board or committee member; Microport: IP royalties; Microport Orthopedics, Inc.: Paid consultant; Wolters Kluwer Health - Lippincott Williams & Wilkins: Publishing royalties, financial or material support; Zimmer: Paid consultant; Research support.
References
- 1. Weinstein SL. Natural history of congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop Relat Res 1987; 225: 62–76. [PubMed] [Google Scholar]
- 2. Brand RA. Hip osteotomies: a biomechanical consideration. J Am Acad Orthop Surg 1997; 5: 282–91. [DOI] [PubMed] [Google Scholar]
- 3. Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg [Br] 1991; 73-B: 423–9. [DOI] [PubMed] [Google Scholar]
- 4. Adelani MA, Crook K, Barrack RL. et al. What is the prognosis of revision total hip arthroplasty in patients 55 years and younger? Clin Orthop Relat Res 2014; 472: 1518–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pakos EE, Paschos NK, Xenakis TA. Long term outcomes of total hip arthroplasty in young patients under 30. Arch Bone Joint Surg 2014; 2: 157–62. [PMC free article] [PubMed] [Google Scholar]
- 6. Swarup I, Marshall A, Lee Y. et al. Implant survival and patient-reported outcomes after total hip arthroplasty in young patients with developmental dysplasia of the hip. Hip Int 2016; 26: 367–73. [DOI] [PubMed] [Google Scholar]
- 7. Adler KL, Cook PC, Yen Y-M. et al. Current concepts in hip preservation surgery: part I. Sports Health 2015; 7: 518–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sohatee MA, Ali M, Khanduja V. et al. Does hip preservation surgery prevent arthroplasty? Quantifying the rate of conversion to arthroplasty following hip preservation surgery. J Hip Preserv Surg 2020; 7: 168–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ganz R, Klaue K, Vinh TS. A new periacetabular osteotomy for the treatment of hip dysplasias. Clin Orthop Relat Res 1988; 232: 26–36. [PubMed] [Google Scholar]
- 10. Siebenrock KA, Scholl E, Lottenbach M. et al. Bernese periacetabular osteotomy. Clin Orthop Relat Res 1999; 363: 9–20. [PubMed] [Google Scholar]
- 11. Crockarell J Jr, Trousdale RT, Cabanela ME. et al. Early experience and results with the periacetabular osteotomy: the Mayo Clinic experience. Clin Orthop Relat Res 1999; 363: 45–53. [PubMed] [Google Scholar]
- 12. Trumble SJ, Mayo KA, Mast JW. The periacetabular osteotomy: minimum 2 year followup in more than 100 hips. Clin Orthop Relat Res 1999; 363: 54–63. [PubMed] [Google Scholar]
- 13. Biedermann R, Donnan L, Gabriel A. et al. Complications and patient satisfaction after periacetabular pelvic osteotomy. Int Orthop 2008; 32: 611–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Clohisy JC, Barrett SE, Gordon JE. et al. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am 2005; 87: 254–9. [DOI] [PubMed] [Google Scholar]
- 15. Clohisy JC, Nunley RM, Curry MC. et al. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am 2007; 89: 1417–23. [DOI] [PubMed] [Google Scholar]
- 16. Clohisy JC, Schutz AL, St. John L. et al. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res 2009; 467: 2041–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ziran N, Vacadipane J, Kadri O. et al. Ten- and 20-year survivorship of the hip after periacetabular osteotomy for acetabular dysplasia. J Am Acad Orthop Surg 2019; 27: 247–55. [DOI] [PubMed] [Google Scholar]
- 18. Wells J, Millis M, Kim Y-J. et al. Survivorship of the Bernese periacetabular osteotomy: what factors are associated with long-term failure? Clin Orthop Relat Res 2016; 475: 396–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Steppacher SD, Tannast M, Ganz R. et al. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res 2008; 466: 1633–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lerch TD, Steppacher SD, Liechti EF. et al. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res 2016; 475: 1154–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Novais EN, Kim YJ, Carry PM. et al. The Bernese periacetabular osteotomy: is transection of the rectus femoris tendon essential? Clin Orthop Relat Res 2014; 472: 3142–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Peters CL, Erickson JA, Anderson MB. et al. Preservation of the rectus femoris origin during periacetabular osteotomy does not compromise acetabular reorientation. Clin Orthop Relat Res 2015; 473: 608–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Clohisy JC, St John LC, Nunley RM. et al. Combined periacetabular and femoral osteotomies for severe hip deformities. Clin Orthop Relat Res 2009; 467: 2221–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cunningham T, Jessel R, Zurakowski D. et al. Delayed gadolinium-enhanced magnetic resonance imaging of cartilage to predict early failure of Bernese periacetabular osteotomy for hip dysplasia. J Bone Joint Surg Am 2006; 88: 1540–8. [DOI] [PubMed] [Google Scholar]
- 25. Albers CE, Steppacher SD, Ganz R. et al. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res 2013; 471: 1602–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sabbag CM, Nepple JJ, Pascual-Garrido C. et al. The addition of hip arthroscopy to periacetabular osteotomy does not increase complication rates: a prospective case series. Am J Sports Med 2019; 47: 543–51. [DOI] [PubMed] [Google Scholar]
- 27. Nassif NA, Schoenecker PL, Thorsness R. et al. Periacetabular osteotomy and combined femoral head-neck junction osteochondroplasty: a minimum two year follow-up cohort study. J Bone Joint Surg [Am] 2012; 94-A: 1959–66. [DOI] [PubMed] [Google Scholar]
- 28. Ricciardi BF, Fields KG, Wentzel C. et al. Complications and short-term patient outcomes of periacetabular osteotomy for symptomatic mild hip dysplasia. Hip Int 2017; 27: 42–8. [DOI] [PubMed] [Google Scholar]
- 29. Gray BL, Stambough JB, Baca GR. et al. Comparison of contemporary periacetabular osteotomy for hip dysplasia with total hip arthroplasty for hip osteoarthritis. Bone Joint J 2015; 97-B: 1322–7. [DOI] [PubMed] [Google Scholar]
- 30. Smith MV, Klein SE, Clohisy JC. et al. Lower extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg [Am] 2012; 94-A: 468–77. [DOI] [PubMed] [Google Scholar]
- 31. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with oste- oarthritis of the hip. J Bone Joint Surg [Am] 1999; 81-A: 1747–70. [DOI] [PubMed] [Google Scholar]
- 32. Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg [Br] 1993; 75-B: 228–32. [DOI] [PubMed] [Google Scholar]
- 33. Rames R, Stambough J, Pashos G. et al. Fifteen-year results of total hip arthroplasty with cobalt-chromium femoral heads on highly cross-linked polyethylene in patients 50 years and less. J Arthroplasty 2019; 34: 1143–9. [DOI] [PubMed] [Google Scholar]
- 34. Kim CH, Kim JW. Periacetabular osteotomy vs. total hip arthroplasty in young active patients with dysplastic hip: systematic review and meta-analysis. Orthop Traumatol Surg Res 2020; 106: 1545–51. [DOI] [PubMed] [Google Scholar]
- 35. Salih S, Groen F, Hossein F. et al. Hypermobility, age 40 years or older and BMI >30 kg m−2 increase the risk of complications following peri-acetabular osteotomy. J Hip Preserv Surg 2020; 7: 511–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kalore N, Cheppalli S, Daner W. et al. Acetabular dysplasia in middle-aged patients: periacetabular osteotomy or total hip arthroplasty? J Arthroplasty 2016; 31: 1894–8. [DOI] [PubMed] [Google Scholar]
- 37. Hsieh PH, Huang KC, Lee PC. et al. Comparison of periacetabular osteotomy and total hip replacement in the same patient: a two- to ten-year follow-up study. J Bone Joint Surg 2009; 91-B: 883–8. [DOI] [PubMed] [Google Scholar]
- 38. Garbuz DS, Awwad MA, Duncan CP. Periacetabular osteotomy and total hip arthroplasty in patients older than 40 years. J Arthroplasty 2008; 23: 960–3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.


