Abstract
The occurrence of Brown-Sequard syndrome with Horner’s syndrome in a child with spinal trauma is a very rare and unusual entity. Brown-Sequard syndrome results from hemisection injury of the spinal cord, mostly in the cervical cord region. The Horner’s syndrome presents when the injury is in the cervical region involving the sympathetic pathway. We present you with the case of a 12-year-old boy who was referred from a local hospital with weakness on the left half of his body after sustaining a penetrating injury to his neck by a khuru (Bhutanese dart). Clinical examination was consistent with the diagnosis of Brown-Sequard syndrome with ipsilateral Horner’s syndrome. Although cervical spine plain radiographs showed no fracture, computed tomography and magnetic resonance imaging showed a C2 lamina fracture at the left side of the spinous process with indentation to the cord. He was managed conservatively with a soft cervical collar, intravenous antibiotics, and physiotherapy. He had complete resolution of Brown-Sequard syndrome and Horner’s syndrome after 1 year. Patients with Brown-Sequard syndrome associated with Horner’s syndrome usually have a good prognosis and full recovery rate with regular physiotherapy and rehabilitation. Early diagnosis and treatment will have a better chance of recovery and return to pre-injury status.
Keywords: Brown-Sequard syndrome, Horner’s syndrome, penetrating injury, cervical region, khuru, dart
Introduction
Brown-Sequard syndrome (BSS) is a rare form of spinal cord injury which was first described in 1846 by Charles-Edouard Brown-Sequard.1,2 BSS results from hemisection injury of the spinal cord, mostly in the cervical cord region, which leads to ipsilateral loss of motor function, proprioception, and vibration at the level of the lesion as well as contralateral loss of pain and temperature sensation approximately two levels below the lesion.3,4 The distribution of the BSS is 75% thoracic, 17% cervical, and 8% lumbar. 5
BSS occurs in the setting of traumatic spinal cord injuries, spinal cord tumors, and epidural hematomas.6–9 BSS can be associated with Horner’s syndrome when there is a coexistent injury to the cervical paravertebral sympathetic chain and inferior cervical ganglion. 10 Horner’s syndrome is characterized by the classic triad of miosis, partial ptosis, and hemifacial anhidrosis. Although concurrence of Horner’s syndrome is common in spinal cord lesions at the cervicothoracic region, the combination of Horner’s with BSS is very rare with very limited reports. 5
According to the literature, the occurrence of BSS in combination with Horner’s syndrome was mostly due to trauma, which ranged from a blunt to penetrating stab injuries to the cervical region.5,10–13 Other rare causes were cervical epidural hematoma,14–16 cervical disk herniation,6,17 and cervical spinal cord infarction.18,19
Herein, we report an interesting and unusual case of penetrating injury to the cervical spine by a khuru (Bhutanese dart) causing BSS and Horner’s syndrome in a 12-year-old boy. The occurrence of such a syndrome was initially not suspected at the local hospital but was diagnosed at the national referral hospital upon thorough neurological examination. The bone injury was confirmed by radiographic imaging.
Case presentation
A 12-year-old boy was witnessing a khuru (Bhutanese dart) match with his friends when he was accidentally hit by the khuru/dart at the posterior aspect of his neck. The dart was removed by his friends at the site of incident and he was taken to the nearby local hospital. He did not have either active bleeding or loss of consciousness, but he complained of left-sided weakness. Plain radiography of his cervical spine at a local hospital showed no fracture. Since magnetic resonance imaging/computed tomography (MRI/CT) facilities were not available at the local hospital, the patient was referred with a cervical collar in an ambulance to the national referral hospital for further evaluation and management of his left-sided body weakness.
On general examination, he was conscious and fully oriented. His Glasgow coma scale was 15/15 and his vital signs were all stable. On physical examination, he had a small puncture wound, measuring 5 mm × 5 mm over the posterior aspect of the upper cervical region, slightly toward the right side of the midline. There was no active bleeding or any leakage from the wound.
Neurological examination revealed a motor grade of 4/5 on the right limbs and 0/5 on the left side of his body. The Babinski sign was also positive on his left side. He had a loss of pain sensation over his right side below the C4 region; however, light touch was preserved. In addition, he had partial drooping of his left upper eyelid (Figure 1) and miosis of his left pupil but with intact direct and consensual reflexes. He also had anhidrosis on the left side of his face, consistent with Horner’s syndrome.
Figure 1.

Partial ptosis of left eyelid of our patient (image was taken with consent from boy’s parents).
He had normal bowel and bladder functions. Together, these findings were consistent with BSS associated with ipsilateral Horner’s syndrome. His other systemic examination was unremarkable.
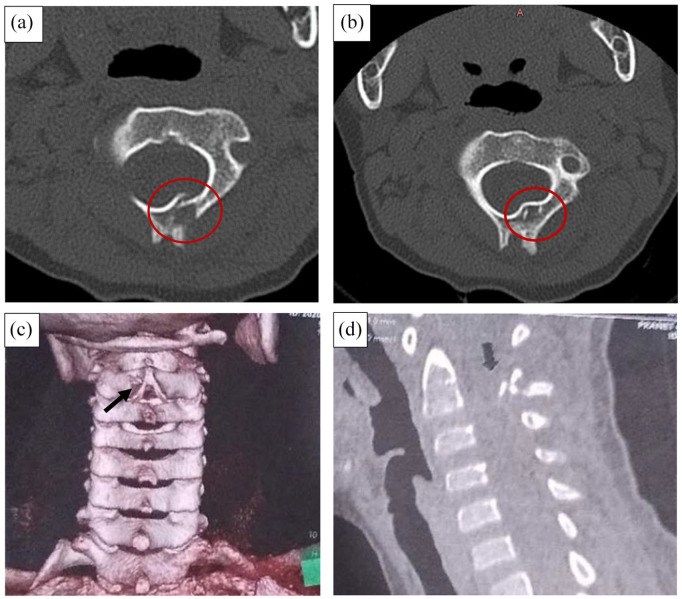
Plain radiograph of the cervical spine showed no significant abnormality. However, CT showed a C2 lamina fracture on the left side with impingement of the canal with a bony fragment (Figure 2(a) and (b)). The 3-D image of the cervical spine showed a small bony defect at C2 lamina corresponding to the injury site by the khuru (Figure 2(c)). A small bony fragment was appreciated inside the spinal canal in the sagittal view of the cervical spine (Figure 2(d)).
Figure 2.
CT-cervical spine. (a) and (b) C2 lamina fracture on the left side, red circle (axial view). (c) 3-D image of cervical spine showing a small bony defect (black arrow). (d) The sagittal view of cervical spine showing a bony fragment inside the spinal canal (black arrow).
MRI also showed a C2 lamina fracture at the left side of the spinous process with indentation to the cord (Figure 3(a)) associated with cord edema extending from C2 to C4 (Figure 3(b)).
Figure 3.
MRI of cervical spine. (a) Axial view C2 lamina fracture showing indentation to the cord, red arrow (axial view). (b) Sagittal view showing C2–C4 cord edema (red circle).
The boy was admitted to the Orthopedic ward of the National referral hospital in Thimphu, Bhutan. After wound irrigation, prophylactic antibiotics were given. He received a tetanus toxoid at the local hospital. Since the fracture was open, the steroid was not initiated. He was started on physiotherapy the next day with a soft cervical collar.
After 1 week of physiotherapy, the motor function of his right limbs was intact with a grade of 5/5, but his left limbs showed a motor grade of 2/5. The sensation was still diminished. At 2 weeks, there was an improvement in his left limbs motor function with the grade of 3/5 on the upper limb and 4/5 on the lower limb. He was able to walk with assistance and did not have any other complaints. He was discharged with a cervical collar and advised to continue rehabilitation at the local health center. The cervical collar was removed at 1 month at the local hospital. He was followed up for 1 year. His motor power and sensation recovered fully with complete resolution of his Horner’s syndrome at the 1-year follow-up.
Discussion
The concomitant occurrence of BSS with Horner’s syndrome in children with a spinal cord injury is very rare. Injuries to the spine are mostly related to motor vehicle accidents, falls, or sports-related injuries. Degenerative disk disease, tumors, hematoma, infections, ischemia, and vasculitis are also known to cause BSS. 12 The reports of traumatic BSS with Horner’s syndrome consisted mainly of adult patients who sustained a stab injury to the neck.11,13,20 There are reports of adult patients with concomitant occurrence of BSS and Horner’s syndrome following penetrating injury to the neck by a screw driver 5 and drill bit. 12 BSS with Horner’s syndrome secondary to blunt injury is less common with only limited reports. 10
Traumatic injuries to the spine are common in adults but very rare in children. There are reports of 5- and 15-year-old children diagnosed with Brown-Sequard-plus-syndrome after they sustained a stab injury to the back,21,22 but these children did not have associated Horner’s syndrome. A penetrating injury to the neck by the khuru/Bhutanese dart leading to both BSS and Horner’s syndrome in a 12-year-old child is a very unusual case. To the best of our knowledge, this is the first reported case of a dart injury to the cervical spine leading to concomitant occurrence of BSS and Horner’s syndrome.
The khuru is an outdoor Bhutanese traditional sport played by a team composed mostly of 8–12 players. The khuru involves throwing of a pair of darts (Figure 4(a)) at the target (Figure 4(b)), approximately at a distance of 15–20 m. The dart is made up of approximately a 20 cm long wooden stick with a sharp point at the tip (usually a nail) and four fins at the rear. The target is made up of a wooden flat-sided post stuck into the ground. The audience and players who have thrown both of their khurus gather around the target witnessing other players throw their khurus at the target. The game is quite popular among Bhutanese men and is usually played during festivals and government holidays. However, owing to the sharp nature of the khuru, incidences happen now and then with injuries occurring mostly in the lower limbs of the players or audiences.
Figure 4.
(a) Khuru (Bhutanese dart) and (b) players gathering around the target (images taken with permission from players).
The clinical presentation of BSS may range from mild to severe neurological deficit. However, the diagnosis of BSS is made on the basis of history and physical examination. The plain radiographs and CT scan of the cervical spine are helpful for detecting bony abnormalities and play a major role in the initial management of spine-injured patients. 23 However, MRI is the choice of investigation for evaluating BSS as it can illustrate the extent of injury to the spinal cord and the surrounding soft tissues, the damage to the intervertebral disks, and confirmation of the overall spinal alignment. 23
The treatment of patients with BSS consists of conservative management and decompression surgery depending on the cause, and is mainly focused on preventing complications. 3 As per the NASCIS-3, administration of methylprednisolone within 3 h of injury has been associated with a reduction of the convalescent and rehabilitative phases. 5 However, the role of methylprednisolone in penetrating or traumatic spinal cord injury is controversial due to the risk of infections. 3 Nevertheless, the standard perioperative prophylactic antibiotics are recommended. 3
Decompression surgery is indicated for patients who have a traumatic injury or any tumor or abscess causing cord compression 3 or for removing a foreign body or bony fragment. However, if a patient develops severe neurological deficit, decompressive surgery will not give much improvement. Our patient did not undergo surgery because the bony fragment did not compress the spinal cord. The prognosis of patients with BSS is usually good with favorable improvement of neurological deficits.8,24 Our patient had complete resolution of BSS and Horner’s syndrome after 1 year of dedicated physiotherapy and rehabilitation.
Conclusion
Patients with BSS associated with Horner’s syndrome usually have a good prognosis and full recovery rate with regular physiotherapy and rehabilitation. Although bony injury may not be appreciated in a plain radiograph, healthcare workers should be aware of the clinical manifestation of such an entity and do a thorough neurological examination to come to a correct diagnosis, especially in a resource-poor setting where CT/MRI facilities are not always available. Early diagnosis and treatment will have a better chance of recovery and return to pre-injury status.
Acknowledgments
The author thanks the boy’s father for giving consent to publish his identified clinical information and photos. He also thanks Dr Sam Baker (Orthopedic Surgeon, USA), Dr Robert Hoffman (Orthopedic Surgeon, USA), and Professor Dr Tashi Tenzin Neurosurgeon and Dean of Khesar Gyalpo University of Medical Science of Bhutan for proofreading this article.
Footnotes
Author contributions: K.W. conceived of the research, collected the data, and compiled and revised the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the child’s parent (father) for his anonymized information to be published in this article. This informed consent is available on request from the corresponding author.
ORCID iD: Kuenzang Wangdi  https://orcid.org/0000-0002-4029-4395
https://orcid.org/0000-0002-4029-4395
References
- 1. Komarowska M, Debek W, Wojnar JA, et al. Brown-Séquard syndrome in a 11-year-old girl due to penetrating glass injury to the thoracic spine. Eur J Orthop Surg Traumatol 2013; 23(Suppl. 2): S141–S143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rengachary SS, Colen C, Guthikonda M. Charles-Edouard Brown-Séquard: an eccentric genius. Neurosurgery 2008; 62(4): 954–964; discussion 964. [DOI] [PubMed] [Google Scholar]
- 3. Shams S, Arain A. Brown Sequard syndrome. Treasure Island, FL: StatPearls Publishing, 2022. [PubMed] [Google Scholar]
- 4. Van Wittenberghe IC, Peterson DC. Corticospinal tract lesion. Treasure Island, FL: StatPearls Publishing, 2022. [PubMed] [Google Scholar]
- 5. García-Manzanares MD, Belda-Sanchis JI, Giner-Pascual M, et al. Brown-Sequard syndrome associated with Horner’s syndrome after a penetrating trauma at the cervicomedullary junction. Spinal Cord 2000; 38(11): 705–707. [DOI] [PubMed] [Google Scholar]
- 6. Meng Y, Zhou L, Liu X, et al. Brown-Sequard syndrome associated with Horner syndrome following cervical disc herniation. Spinal Cord Ser Cases 2016; 2: 16037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pouw MH, van de Meent H, van Middendorp JJ, et al. Relevance of the diagnosis traumatic cervical Brown-Séquard-plus syndrome: an analysis based on the neurological and functional recovery in a prospective cohort of 148 patients. Spinal Cord 2010; 48(8): 614–618. [DOI] [PubMed] [Google Scholar]
- 8. McKinley W, Santos K, Meade M, et al. Incidence and outcomes of spinal cord injury clinical syndromes. J Spinal Cord Med 2007; 30(3): 215–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Abouhashem S, Ammar M, Barakat M, et al. Management of Brown-Sequard syndrome in cervical disc diseases. Turk Neurosurg 2013; 23(4): 470–475. [DOI] [PubMed] [Google Scholar]
- 10. Edwards A, Andrews R. A case of Brown-Sequard syndrome with associated Horner’s syndrome after blunt injury to the cervical spine. Emerg Med J 2001; 18(6): 512–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Johnson S, Jones M, Zumsteg J. Brown-Séquard syndrome without vascular injury associated with Horner’s syndrome after a stab injury to the neck. J Spinal Cord Med 2016; 39(1): 111–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Russell JH, Joseph SJ, Snell BJ, et al. Brown-Sequard syndrome associated with Horner’s syndrome following a penetrating drill bit injury to the cervical spine. J Clin Neurosci 2009; 16(7): 975–977. [DOI] [PubMed] [Google Scholar]
- 13. McCarron MO, Flynn PA, Pang KA, et al. Traumatic Brown-Séquard-plus syndrome. Arch Neurol 2001; 58(9): 1470–1472. [DOI] [PubMed] [Google Scholar]
- 14. Shen CC, Wang YC, Yang DY, et al. Brown-Séquard syndrome associated with Horner’s syndrome in cervical epidural hematoma. Spine 1995; 20(2): 244–247. [DOI] [PubMed] [Google Scholar]
- 15. Jeon E-H, Song J-H, Park H-K, et al. A cervical epidural hematoma caused by ruptured arteriovenous malformation presenting as a Brown-Sequard and Horner’s syndrome—a case report. J Korean Neurosurg Soc 2001; 30(Suppl. 1): 144–148. [Google Scholar]
- 16. Panciani PP, Forgnone S, Fontanella M, et al. Unusual presentation of a spontaneous spinal epidural haematoma. Acta Neurol Belg 2009; 109(2): 146–148. [PubMed] [Google Scholar]
- 17. Baudracco I, Grahovac G, Russo VM. Spontaneous cervical intradural disc herniation presenting with Brown-Séquard and Horner’s syndrome: lesson learned from a very unique case. Eur Spine J 2017; 26(Suppl. 1): 218–221. [DOI] [PubMed] [Google Scholar]
- 18. Sohn SI, Park SW, Hong JH, et al. Cervical spinal cord infarction presenting Brown-Séquard-plus syndrome. Keimyung Med J 2014; 33(1): 44–47. [Google Scholar]
- 19. Ginos J, McNally S, Cortez M, et al. Vertebral artery dissection and cord infarction—an uncommon cause of Brown-Séquard and Horner syndromes. Cureus 2015; 7(8): e308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McCann MR, Villamar MF. Two classical neurological syndromes following a stab wound. Eur J Intern Med 2018; 54: e3–e4. [DOI] [PubMed] [Google Scholar]
- 21. Issaivanan M, Nhlane NM, Rizvi F, et al. Brown-Séquard-plus syndrome because of penetrating trauma in children. Pediatr Neurol 2010; 43(1): 57–60. [DOI] [PubMed] [Google Scholar]
- 22. Millichap JG. Brown-Sequard-plus syndrome after stab injury. Pediatr Neurol Briefs 2010; 24(7): 55–56. [Google Scholar]
- 23. Miranda P, Gomez P, Alday R, et al. Brown-Sequard syndrome after blunt cervical spine trauma: clinical and radiological correlations. Eur Spine J 2007; 16(8): 1165–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Alrabiah AA, Alskait GA, Alwakeel TS, et al. Conservative management of traumatic Brown-Séquard syndrome: a case report. Am J Case Rep 2021; 22: e930036. [DOI] [PMC free article] [PubMed] [Google Scholar]