Abstract
The Institute of Medicine and the National Institute on Aging increasingly understand that knowledge alone is necessary but insufficient to improve healthcare outcomes. Adapting the behaviors of clinicians, patients, and stakeholders to new standards of evidence-based clinical practice is often significantly delayed. In response, over the past twenty years, Implementation Science has developed as the study of methods and strategies that facilitate the uptake of evidence-based practice into regular use by practitioners and policymakers. One important advance in Implementation Science research was the development of Standards for Reporting Implementation Studies (StaRI), which provided a 27-item checklist for researchers to consistently report essential elements of the implementation and intervention strategies. Using StaRI as a framework, this review discusses specific Implementation Science challenges for research with older adults, provides solutions for those obstacles, and opportunities to improve the value of this evolving approach to reduce the knowledge translation losses that exists between published research and clinical practice.
Keywords: implementation science, knowledge translation, geriatrics, reporting standards
INTRODUCTION
In 2001 the Institute of Medicine (IOM) report Crossing the Quality Chasm: A New Health System for the 21st Century highlighted the concept of Knowledge Translation in which “Making use of new knowledge requires health professionals…use new tools to access and apply the expanding knowledge base”.1 Over the subsequent decades, Implementation Science arose as the study of methods and strategies that facilitate the uptake of evidence-based practice into regular use by practitioners and policymakers. A decade later, the National Institutes of Health created a framework depicting the components of and objectives to Implementation Science research (Figure 1).2 Shortly thereafter, Standards for Reporting Implementation Studies (StaRI) provided a 27-item checklist for researchers to consistently report essential elements of the implementation and intervention strategies.3,4
Figure 1.
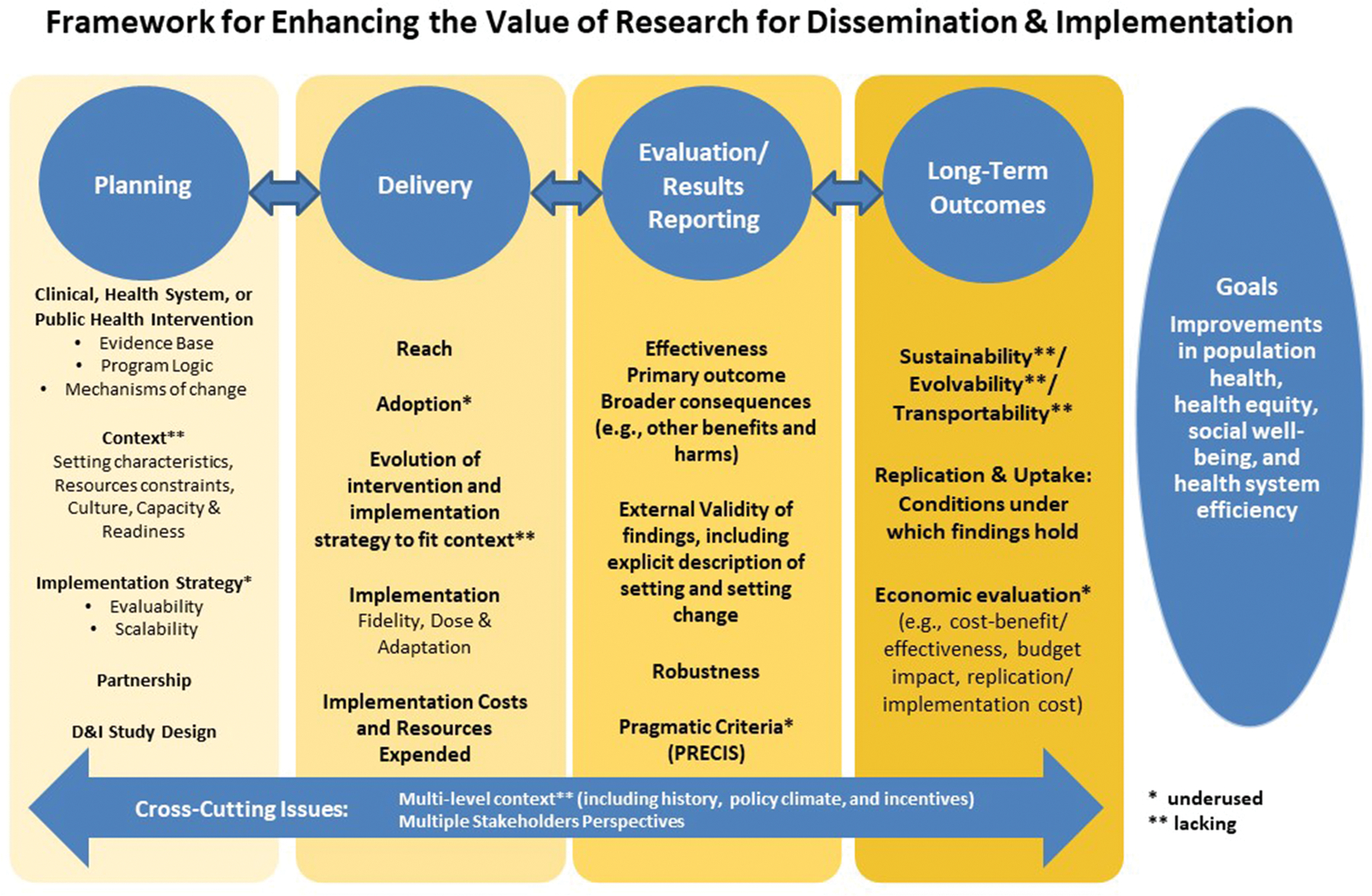
Framework for Enhancing the Value of Dissemination and Implementation Research developed by National Institute of Health Work Group
Journal of the American Geriatrics Society (JAGS) readers were introduced to StaRI in 2017 and implementation scientists were encouraged to use this new Enhancing the Quality and Transparency of Health Research (EQUATOR) Network reporting standard.5 The National Institute on Aging increasingly understands that knowledge alone is necessary but insufficient to improve healthcare outcomes since adapting the behaviors of clinicians, patients, and stakeholders to new standards of evidence-based clinical practice is complex, disjointed, and often significantly delayed.6 To improve the quality and relevance of clinical research outcome for older adults, the National Institutes of Health recognized that the inclusion of participants across the lifespan, such as at the extremes of age, is an important factor to consider when assessing funding priority.7Implementation Science research is appearing with increasing frequency in JAGS as we discover more about older adults, caregivers, and aging infrastructure.8–13 Implementation Science is needed to accelerate the uptake and sustainability of knowledge across healthcare settings in the team-based environment that contemporary older adult medical and surgical management exists. The objectives of this review are to highlight Implementation Science challenges for geriatric researchers, provide solutions for those obstacles, and identify opportunities to improve the value of this evolving approach in order to reduce the knowledge translation decay that exists between published research and clinical practice.
Implementation Science Barriers for Geriatrics Researchers
StaRI’s 27-item checklist presents numerous challenges for transdisciplinary researchers with Implementation Science objectives. Table 1 is a condensed version of the StarRI checklist illustrating theoretical, operational, and logistical challenges likely to arise as Implementation Science researchers strive to adhere to these reporting recommendations.
TABLE 1.
Older Adult Research Related StaRI Challenges
| STARI Checklist | Implementation Barriers | Intervention Barriers |
|---|---|---|
| Introduction | • Underlying theory/framework/model employed as Implementation Strategy often untested in complex older adult healthcare | • Few unequivocal interventions exist in geriatrics that consistently exhibit benefits that outweigh risks in pre-implementation research settings • Medical complexity of older adult healthcare leads to challenges implementing interventions uniformly across populations. |
| Methods: Description Context |
• Acceptability of new knowledge varies across sites and is challenging to measure objectively • Wide divide in socioeconomic status among older adults. |
• Healthcare may be fractured among multiple providers. • Services may not be reimbursed by Medicare. • Local social services and access to transportation differ greatly between counties. • Rural areas are underserved in research. |
| Methods: Description Targeted “sites” |
• Age cutoffs may be less helpful than frailty levels, but are commonly used for services, clinics, and other interventions. • Access to geriatricians varies significantly across hospitals • Older adults in the community who are homebound or vulnerable are often functionally excluded from study recruitment due to lack of access to internet or healthcare. |
• Eligibility criteria can become overly restrictive, excluding those with cognitive impairment or multiple comorbidities. • Caregiver burden and availability often not considered. |
| Methods: evaluation Outcomes |
• Pre-determined target outcomes are often not aligned with what matters most to older adults. | • Common outcomes are often not patient-centered. • Acceptability of intervention to patient (and caregiver) should be reported. • Outcome assessment scales/tools may not be validated in older adults or those with cognitive impairment. |
| Methods: evaluation Economic evaluation |
• Effective interventions may not be cost-effective unless all aspects of elder care are considered • CMS costs are frequently used as a stand-alone for healthcare costs. This does not include the 21% of people on Medicare who buy Medigap insurance and another 18% dual covered by employee sponsored insurance. |
• Healthcare costs often do not include out of pocket costs to patients or unpaid caregiver time needed for the intervention. |
| Methods: subgroups | • Pertinent subgroups rarely considered or analyzed distinctly for implementation or intervention approaches (frail, dementia, socially isolated) | |
| Results: fidelity | • Geriatric-focused adaptation of implementation approach (who, what, where, when, how) rarely contemplated • Healthcare crises from other comorbidities not addressed by the intervention can interrupt adherence to an intervention. |
• Core components of intervention for older patients and/or care partners and intensity with which those components delivered uncommonly reported |
| Discussion: policy or clinical practice guideline implications | • Investigators often miss opportunities to promote incorporation of effective implementation strategies into clinical practice guidelines | • Healthcare reimbursement structures do not adapt quickly to promote effective interventions. • Clinical Practice Guidelines often miss opportunity to filter recommendations through geriatric perspective |
StaRI Introduction
StaRI recommends explicit and evidence-based justification for the intervention implemented as well as the theory or framework employed as the Implementation Science foundation. Over 100 theoretical models for dissemination and/or implementation research exist with the intent to bridge research and practice.14 Several of these models, including the RE-AIM Framework, Promoting Action on Research Implementation in Health Services (PARIHS), Precede-Proceed Model, Practical Robust Implementation and Sustainability Model (PRISM), and the Consolidated Framework for Implementation Research (CFIR), have been deployed in implementation studies. While some of these models have been used in geriatric research, many others remain theoretical and untested. None of these models has demonstrable superiority over another, so older adult researchers have employed different frameworks across studies. For example, a systematic review of older adult physical activity programs that included 137 studies found that only 11 utilized any framework and those used six different frameworks.15 Others have used the Complex Adaptive Systems model to create collaborative dementia care healthcare systems.8 Clinical informatics researchers using clinical decision support as knowledge translation tools have used PRISM as an integrative framework.16 More frequently, older adult researchers have used CFIR in nursing home and acute care settings.10,13 Ongoing efforts to adapt CFIR for frail older adult primary care populations are underway, as is work to conceptualize inner and outer settings that affect community-based innovations for those with more severe injury or illness in complex healthcare settings.17–19
StaRI Context
The population and healthcare setting in which innovations are implemented are essential for researchers to describe and often extend beyond the hospital or medical office into homes and communities. The Equity-focused Implementation Research for health programs (EquIR) framework identifies challenges in the pre-intervention, implementation, and post-implementation phases of community-based participatory research.20 These challenges include the identification of key partners while understanding community perceptions and values, obtaining and maintaining ethical oversight, aligning budgetary concerns with intellectual property rights, and sustainability. Failure to contemplate each of these components limits future investigators’ ability to adapt the intervention or implementation strategy for their population and resources. In addition, understanding the context in which specific interventions fail to demonstrate anticipated benefits provides decision-makers opportunities to distinguish unsuccessful intervention strategies from ineffective interventions. For example, the Strategies To Reduce Injuries and Develop confidence in Elders (STRIDE) fall prevention trial did not reduce injurious falls despite a robust and evidence-based, individually targeted, multifactorial intervention. This may not be an ineffective intervention, as post-hoc interviews guided by CFIR identified multiple potential contextual barriers resulting in unsuccessful implementation.12 By understanding individual patient’s financial resources and mobility, as well as the connectedness of their healthcare setting and ability to navigate between various professional clinics and home health resources across rural and urban settings, older adult researchers can more accurately interpret the applicability of implementation science research for their environment.21,22
StaRI Targeted Populations and Sites
Older adults, particularly frail subsets of the population, have traditionally been underrepresented in pre-implementation efficacy trials which leaves the potential benefits and harms largely undefined.23 For example, the majority of cancer diagnoses and deaths are adults over age 65, yet less than a decade ago a significant knowledge void existed for oncology therapeutics in this population.24 At the patient-level, implementation researchers need to evaluate and report constructs such as frailty and physiological resilience for external stakeholders to assess applicability to their populations.25 Different frailty tools are used in various clinical settings with limited knowledge around how to harmonize measures of frailty between instruments. Whereas brevity must be weighed against accuracy in time-limited settings like the emergency department, primary care settings have the opportunity for serial assessments and longer frailty assessments like the Frailty Index.26,27 Similarly, the assessment of physical resilience is an emerging construct without transdisciplinary acceptance of a uniform measure of resilience across medical, surgical, and mental health settings.28 Measurement approaches for physical resilience will need to incorporate frail phenotype, biological and chronological age, and anticipated disease trajectory within the context of the acute stressor and therapeutic alternatives. Geriatric implementation scientists should carefully contemplate acceptable and reproducible measures of frailty and physical resilience.
Health literacy and socioeconomic constraints often limit patient participation in efficacy research and dissemination into real-world populations.29 The Centers for Medicare & Medicaid Services Accountable Needs Communities Health-Related Social Needs Screening Tool is an established and commonly used instrument as a broad assessment of social determinants of health.30 In addition, complex interventions often require care partner availability and engagement, so objectively reporting their involvement will be an essential component of reproducibility and scale-up.31 The Caregiving Health Engagement Scale is one measure of care partner capacity to participate in another patient’s care.32 At the healthcare system level, describing the interconnectedness of insurance status and equitable access to services is a component of adapting interventions locally to accommodate resource constraints, yet is often unreported or provided only in general demographic tables.33
StaRI Outcomes
Person-centered care requires a collaborative approach to align individual values with attainable outcomes that often requires an understanding of a patient’s decisional conflict, health literacy, and preparedness for decision-making.34 Patient and physician priorities require time and expertise to align in older adults with complex co-morbidities, yet investigators often neglect these factors in reporting the application of an intervention and implementation strategy in research.35 Memory and communication impairments associated with Alzheimer’s dementia and related disorders also create obstacles to both research consent and patient-reported outcomes, so implementation researchers need to accommodate those challenges.36 Successful and ethically acceptable approaches to recruiting and retaining vulnerable older adults in health outcomes research have been described elsewhere and should be applicable to Implementation Science investigations.37,38
The costs and cost-effectiveness of implementing interventions is the most frequently omitted element of StaRI in non-geriatric research and is likely more complicated in older adults. An intervention resulting in the best outcomes for older adults may not be economically feasible unless all healthcare costs are considered. For instance, cognitive behavioral therapy for insomnia is generally not well-reimbursed, but is preferred over hypnotic medications due to concerns over falls and other AEs.39,40 Investigators should include a health economist on the research team to ensure reasonable assumptions and cost-analysis approaches are reported.41,42
StaRI Subgroups
Aging populations are hardly monolithic. Instead, older adults represent a heterogeneous patient group ranging from functionally and cognitively intact individuals who are fully and independently engaged in the community to frail and dependent persons (18–60%, depending on the reporting community and frailty score used).43–45 Implementation Science seeking to ramp up effective interventions across real-world settings must contemplate prevalent subsets in whom distinct strategies may be required to attain similar outcomes. Geriatric subsets might include persons living with dementia, frail individuals, and care partner dependency. Also, caregivers of older adults are frequently older adults themselves, who can also suffer from cognitive dysfunction and multiple comorbidities. Interventions relying on caregivers or dyads need to ensure that the caregivers as well have the support and cognition necessary for the intervention. Implementation researchers can remain attuned to these subgroups by utilizing some of the recommendations discussed in the Target Populations section, such as measuring and reporting frailty and describing the interconnectedness of health systems and social determinants of health with patient-oriented outcomes.
StaRI Results
Fidelity represents the extent to which an intervention was delivered in terms of content and quality as conceived by the developers.46 Improving older adult outcomes often requires the delivery of education, communication, or interventions that require a sustained effort from multiple stakeholders. For example, one fall prevention exercise trial required instructors to review home exercises and Tai Chi over the course of a 24-week program, but observers noted the omission of 25% of this content.47 The concept of fidelity is challenging to capture in a reportable manner, particularly when the key components of an implementation intervention require meaningful engagement of multiple individuals across time and locations. Nonetheless, complex implementation trials must pre-plan assessments of fidelity for key stakeholders and specify the unit of analysis.48,49 Tele-observation (video conference or recording sessions for asynchronous review), direct observation, or asking participants to rate the elements of an intervention by how compliant they were to each one may be ways to assess intervention fidelity. One study of a palliative care nurse intervention used a 5 point likert “helpfulness” scale, to assess participants ability to use the intervention tools.50
Fidelity assessments can greatly inform future trials, and often yield interesting new barriers or motivations. A study of a Coach2Move intervention led by physical therapists for older adults assessed fidelity through a scale and follow up qualitative interviews. They found fundamental differences in the theoretical approach to physical therapy in therapists who were high fidelity to the intervention and those who were low fidelity.51
StaRI Discussion
Clinical practice guidelines represent medicine’s effort to synthesize research evidence into actionable recommendations based on factors including the consistency of effect, potential harms, health equity, resources, and feasibility. The Grading of Recommendations Assessment Development and Evaluation (GRADE) approach recommends an implementation component to accompany guideline recommendations to reduce knowledge translation obstacles and facilitate uptake in clinical practice.52 Unfortunately, geriatric clinical practice guidelines are rare and those that exist often neglect implementation resources.53 More frequently, efforts to integrate clinical practice guidelines are a local effort that requires the investment of time and innovation repeatedly across healthcare systems.54 Future geriatric clinical practice guideline development should incorporate implementation science by providing an implementation toolkit that could be operationalized at the local level.55
Opportunities to Improve the Value of Implementation Science for Geriatrics
StaRI must be considered at the initial planning stage of an implementation study, and even better during the intervention development. We suggest even further consideration for interventions with older adults (Table 2). Obvious targets exist to accelerate the uptake of research into practice for older adults. One immediate priority is to include a representative spectrum of older adults in ongoing research across specialties and healthcare settings rather than the historical approach of excluding complex older adults from efficacy trials. The 21st Century Cures Act and the National Institutes of Health Inclusion Across the Lifespan initiative target populations at the extremes of age and provide funding priorities to promote this paradigm shift.7 The American Geriatrics Society advocates the 5Ts (Target Population, Team, Tools, Time, and Tips to Accommodate) to increase the inclusivity of health outcomes research for aging populations.56 Inclusion of older adults into health outcomes research from rural populations and chaotic acute care settings is also necessary and quite challenging.37,57 Increasing the inclusion of older adults will provide a more compelling rationale for the intervention component of implementation research.
TABLE 2.
STARI-65 Recommendations
| STARI Checklist | Barriers | STARI-65 Recommendations |
|---|---|---|
| Introduction | • Underlying theory/framework/model employed as Implementation Strategy often untested in complex older adult healthcare • Few unequivocal interventions exist in geriatrics that consistently exhibit benefits that outweigh risks in pre-implementation research settings |
• Acknowledge the limitations of frameworks and implementation strategies and how they are adapted to the population in question. • Include a representative spectrum of older adults in ongoing research across specialties and healthcare settings rather than the historical approach of excluding complex older adults from efficacy trials. |
| Methods: Description Context |
• Acceptability of new knowledge and readiness to change varies across sites and is challenging to measure objectively • Wide divide in socioeconomic status among older adults. • Healthcare may be fractured among multiple providers. • Services may not be reimbursed by Medicare. • Local social services and access to transportation differ greatly between counties. • Rural areas are underserved in research. |
• Contemplate key components such as identification of key partners, community perceptions and values, obtaining and maintaining ethical oversight, aligning budgetary concerns with intellectual property rights, and sustainability. • Understand the context in which specific interventions fail to demonstrate anticipated benefits • Consider patient characteristics such as financial resources, mobility, their connectedness to the healthcare setting, and ability to navigate between various professional clinics and home health resources. |
| Methods: Description Targeted sites and populations |
• Age cutoffs may be less helpful than frailty levels, but are commonly used for services, clinics, and other interventions. • Access to Geriatrics varies significantly across hospitals • Eligibility criteria can become overly restrictive, excluding those with cognitive impairment or multiple comorbidities. • Caregiver burden and availability often not considered. |
• Evaluate and report patient-level constructs such as frailty, physiological resilience, health literacy, and socioeconomic status. • Describe the interconnectedness of insurance status and equitable access to services. • Justify inclusion/exclusion of those with frailty or cognitive impairment. |
| Methods: evaluation Outcomes |
• Pre-determined target outcomes are often not aligned with what matters most to older adults. • Common outcomes are often not patient-centered. • Acceptability of intervention to patient (and caregiver) should be reported. • Assessing effectiveness outcomes qualitatively may be limited due to cognitive impairment. |
• Understand a patient’s decisional conflict, health literacy, and preparedness for decision-making. • Contemplate how memory and communication impairments, such as those associated with Alzheimer’s dementia and related disorders, have an impact on outcomes. • Include caregiver outcomes. |
| Methods: evaluation Economic evaluation |
• Healthcare costs often do not include out of pocket costs to patients or unpaid caregiver time needed for the intervention. • CMS costs are frequently used as a stand-alone for healthcare costs. This does not include the 21% of people on Medicare who buy Medigap insurance and another 18% dual covered by employee sponsored insurance. |
• Report insurance status. • Report out of pocket costs. • Report non-reimbursable costs to health systems or clinics. |
| Methods: subgroups | • Pertinent subgroups rarely considered or analyzed distinctly for implementation or intervention approaches (frail, dementia, socially isolated) | • Contemplate prevalent subsets of older adults, such as persons living with dementia, frail individuals, and care partner dependency, in whom distinct strategies may be required to attain similar outcomes. |
| Results: fidelity | • Geriatric-focused adaptation of implementation approach (who, what, where, when, how) rarely contemplated • Core components of intervention for older patients and/or care partners and intensity with which those components delivered uncommonly reported |
• Pre-plan assessments of fidelity, understanding that this will be challenging to capture in a reportable manner, particularly when the key components of an implementation intervention require meaningful engagement of multiple individuals across time and locations. • Report any differences between high fidelity and low fidelity users. |
| Discussion: policy or clinical practice guideline implications | • Investigators often miss opportunities to promote incorporation of effective implementation strategies into clinical practice guidelines • Healthcare reimbursement structures do not adapt quickly to promote effective interventions. • Clinical Practice Guidelines often miss opportunity to filter recommendations through geriatric perspective |
• Report how the study evidence may affect the strength of recommendations for existing guidelines. |
Concurrently, subtypes of Implementation Science such as de-implementation are emerging as essential precursors to both reduce practices overused by health care providers and to promote uptake of new research in older populations.58 De-implementing outdated or non-evidence based health interventions mandates an understanding of the comparative efficacy of alternatives, the values of the patient currently receiving the inferior intervention, and the rationale of the healthcare team delivering the outdated alternative.59 De-adoption may simply require trial evidence of preventable harms or lack of efficacy, but will often mandate a more proactive approach to facilitate practice change with a transparent understanding of the context in which healthcare teams and service leaders conceptualize de-implementation of the status quo.60 In geriatric research StaRI principles are being leveraged to increase the deprescribing of potentially harmful medications, but de-implementation likely requires an approach that differs from Implementation Science and older adult patient populations will probably present unique challenges in removing suboptimal interventions from routine practice.61
Another priority is to learn to think in terms of Implementation Science across the spectrum of research. Designing for dissemination and implementation as early as the basic science phase of discovery provides a novel pathway to accelerate knowledge translation from the bench to the bedside.62 The National Center for Advancing Translational Science created the Integrative Framework of Dissemination, Implementation, and Translation to provide a rationale for basic researchers to engage with clinical implementation investigators and vice versa.63 Pragmatically, research networks like the Latin America and Caribbean Consortium on Dementia are concurrently planning multidisciplinary research platforms spanning basic science to translational research that harmonizes approaches to diagnosis and interventional strategies with the vision to accelerate post-discovery implementation into patient care.64 Health outcomes investigators will likely benefit from increased exposure to Implementation Science during their research training.65 In the meantime, Implementation Science experts can collaborate with geriatric investigators during the early stages of research planning and beyond to provide a foundation upon which to build for widespread dissemination, incorporation into clinical practice, and sustainability across healthcare settings and aging populations.66 Implementation Science experts can help guide researchers’ exploration of an intervention’s efficacy and effectiveness as a roadmap to readiness for a StaRI-guided approach along the spectrum of translational research.67
Conclusions
StaRI will need to adapt to encompass the unique complexities of older adult Implementation Science. Few Implementation Science studies in this population currently cite StaRI as a reporting standard and the issues described in this article may be one reason for that omission. Subtypes of Implementation Science such as de-implementation may emerge as essential precursors to promote uptake of new research in older populations. Early exposure to Implementation Science principles and structured collaboration with Implementation Science experts may catalyze more expeditious incorporation of geriatric clinical research evidence into widespread healthcare delivery while StaRI is adapted to the unique complexities of older adult interventional investigations.
Figure 2.
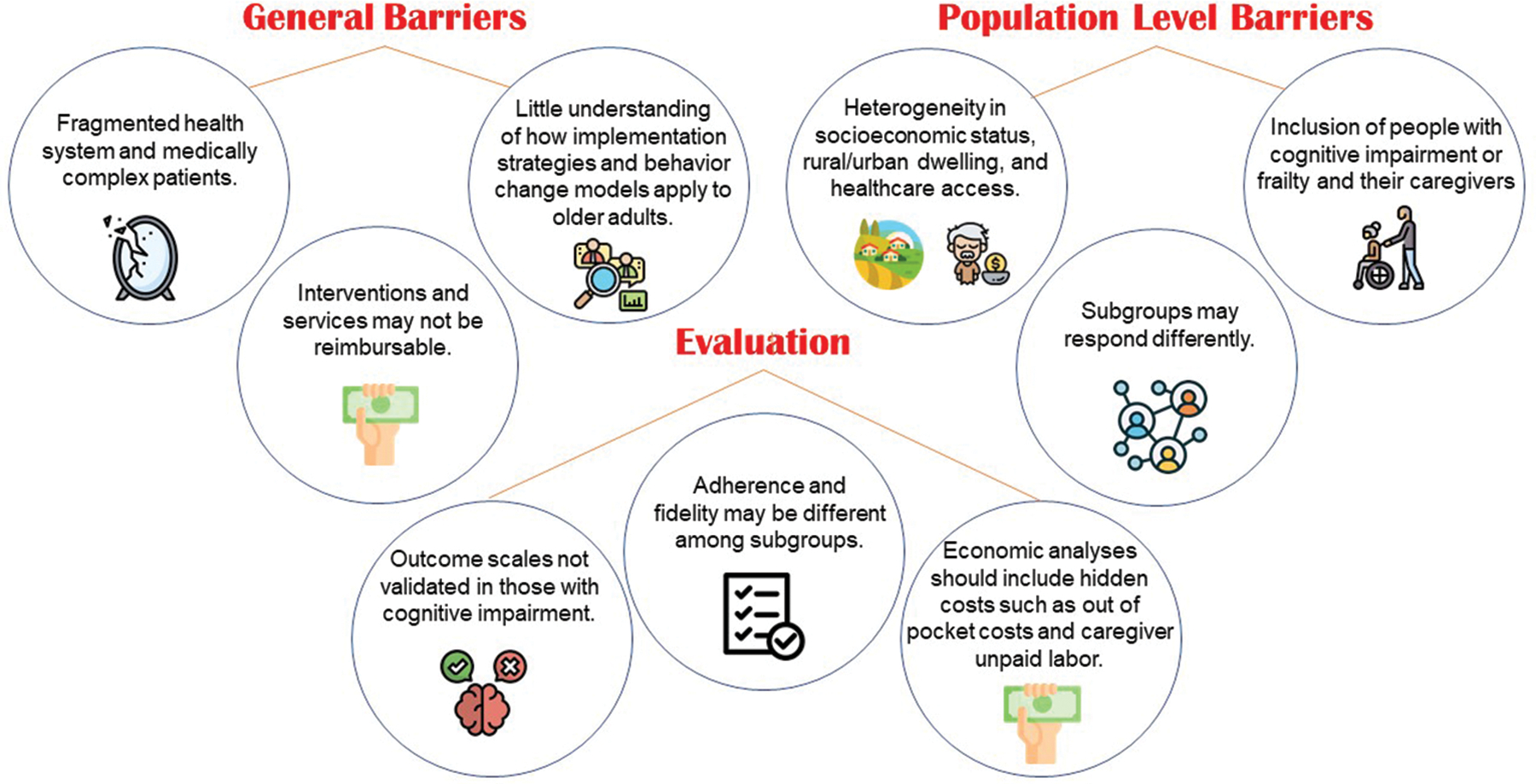
Investigators utilizing Implementation Science in older adults with complex disease co-morbidities frequently encounter barriers at multiple levels which require attention during the design, conduct, interpretation, and reporting of research.
Preamble:
This is the first of a series of manuscripts for the Journal of the American Geriatrics Society supported by the Clinician-Scientists Transdisciplinary Aging Research Leadership Core. While multiple textbooks and review articles exist to support the design, conduct, and reporting of research methods for general populations, investigators in the field of geriatrics often encounter unique challenges related to the complexities of aging. The intent of this series will be to provide first-hand insights for geriatric researchers on topics such as pragmatic randomized controlled trials, diagnostics, machine learning, and big data investigations.
Key Points.
The EQUATOR Network provides a 27-item StaRI checklist to standardize the quality of Implementation Science research reporting, but older adults present unique challenges for researchers to adhere to these recommendations.
Anticipated obstacles for geriatric researchers occur with each component of StaRI, including selection of frameworks, contextual descriptors, meaningful subgroups, outcomes that matter, and comprehensive cost analyses.
Early engagement of implementation science researchers and opportunities to overcome these barriers could accelerate knowledge translation.
Why does this paper matter? Implementation Science is an emerging research method across healthcare fields and is being applied with increasing frequency in geriatrics, yet the unique obstacles in older adults remain undefined.
Sponsor’s Role:
No funding source
Footnotes
Conflict of Interest: CRC is on the Clinician-Scientists Transdisciplinary Aging Research Leadership Core. CRC also co-authored the EQUATOR Network StaRI reporting guidelines.
References
- 1.Crossing the Quality Chasm: A New Health System for the 21st Century Washington DC: Institute of Medicine Committee on Quality of Health Care in America; 2001. [Google Scholar]
- 2.Neta G, Glasgow RE, Carpenter CR, et al. A Framework for Enhancing the Value of Research for Dissemination and Implementation. Am J Public Health 2015;105:49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pinnock H, Barwick M, Carpenter CR, et al. Standards for Reporting Implementation Studies (StaRI) Statement. BMJ 2017;356:i6795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinnock H, Barwick M, Carpenter CR, et al. Standards for Reporting Implementation Studies (StaRI): Explanation and Elaboration Document. BMJ Open 2017. 7:e013318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carpenter CR, Pinnock H. StaRI Aims to Overcome Knowledge Translation Inertia: The Standards for Reporting Implementation Studies Guidelines J Am Geriatr Soc 2017;65:1664–6. [DOI] [PubMed] [Google Scholar]
- 6.Onken L Implementation Science at the National Institute on Aging: The Principles of It. Public Policy & Aging Report 2022. 32:39–41. [Google Scholar]
- 7.Vaughan CP, Dale W, Allore HG, et al. AGS Report on Engagement Related to the NIH Inclusion Across the Lifespan Policy J Am Geriatr Soc 2019;67:211–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boustani M, Alder CA, Solid CA. Agile Implementation: A Blueprint for Implementing Evidence-Based Healthcare Solutions. J Am Geriatr Soc 2018;66:1372–6. [DOI] [PubMed] [Google Scholar]
- 9.Gulasingam P, Haq R, Mascarenhas-Johnson A, et al. Using Implementation Science to Promote the Use of the G8 Screening Tool in Geriatric Oncology. J Am Geriatr Soc 2019;67:898–904. [DOI] [PubMed] [Google Scholar]
- 10.Zúñiga F, De Geest S, Guerbaai RA, et al. Strengthening Geriatric Expertise in Swiss Nursing Homes: INTERCARE Implementation Study Protocol. J Am Geriatr Soc 2019;67:2145–50. [DOI] [PubMed] [Google Scholar]
- 11.Brunkert T, Simon M, Ruppen W, Zúñiga F. Pain Management in Nursing Home Residents: Findings from a Pilot Effectiveness-Implementation Study. J Am Geriatr Soc 2019;67:2574–80. [DOI] [PubMed] [Google Scholar]
- 12.Reckrey JM, Gazarian P, Reuben DB, et al. Barriers to implementation of STRIDE, a national study to prevent fall-related injuries. J Am Geriatr Soc 2021;69:1334–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Southerland LT, Hunold KM, Van Fossen J, et al. An implementation science approach to geriatric screening in an emergency department. J Am Geriatr Soc 2021. (in press). [DOI] [PMC free article] [PubMed]
- 14.Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med 2012;43:337–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gray SM, McKay HA, Nettlefold L, et al. Physical activity is good for older adults-but is programme implementation being overlooked? A systematic review of intervention studies that reported frameworks or measures of implementation. Br J Sports Med 2021;55:84–91. [DOI] [PubMed] [Google Scholar]
- 16.Trinkley KE, Kahn MG, Bennett TD, et al. Integrating the Practical Robust Implementation and Sustainability Model With Best Practices in Clinical Decision Support Design: Implementation Science Approach. J Med Internet Res 2020;22:e19676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sims-Gould J, Elliott J, Tong CE, Giguère A, Mallinson S, Stolee P. A national intervention to support frail older adults in primary care: a protocol for an adapted implementation framework. BMC Geriatr 2021;21:453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warner G, Kervin E, Pesut B, Urquhart R, Duggleby W, Hill T. How do inner and outer settings affect implementation of a community-based innovation for older adults with a serious illness: a qualitative study. BMC Health Serv Res 2021;21:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hill JN, Locatelli SM, Bokhour BG, et al. Evaluating broad-scale system change using the Consolidated Framework for Implementation Research: challenges and strategies to overcome them BMC Res Notes 2018;11:560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nkimbeng M, Han HR, Szanton SL, et al. Exploring challenges and strategies in partnering with community-based organizations to advance intervention development and implementation with older adults. Gerontologist 2022. (in press). [DOI] [PMC free article] [PubMed]
- 21.Levasseur M, Routhier S, Demers K, et al. Importance of collaboration and contextual factors in the development and implementation of social participation initiatives for older adults living in rural areas. Aust Occup Ther J 2021;68:504–19. [DOI] [PubMed] [Google Scholar]
- 22.Carpenter CR, Malone ML. Avoiding Therapeutic Nihilism from Complex Geriatric Intervention “Negative” Trials: STRIDE Lessons J Am Geriatr Soc 2020;68:2752–6. [DOI] [PubMed] [Google Scholar]
- 23.Singh S, Zieman S, Go AS, et al. Statins for Primary Prevention in Older Adults-Moving Toward Evidence-Based Decision-Making. J Am Geriatr Soc 2018;66:2188–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hurria A, Dale W, Mooney M, et al. Designing therapeutic clinical trials for older and frail adults with cancer: U13 conference recommendations J Clin Oncol 2014;20:2587–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walston J, Robinson TN, Zieman S, et al. Integrating Frailty Research into the Medical Specialties-Report from a U13 Conference. J Am Geriatr Soc 2017;65:2134–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arendts G, Burkett E, Hullick C, Carpenter CR, Nagaraj G, Visvanathan R. Frailty, thy name is… Emerg Med Australas 2017;29:712–6. [DOI] [PubMed] [Google Scholar]
- 27.Boreskie KF, Hay JF, Boreskie PE, Arora RC, Duhamel TA. Frailty-aware care: giving value to frailty assessment across different healthcare settings BMC Geriatr 2022;22:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Whitson HE, Duan-Porter W, Schmader KE, Morey MC, Cohen HJ, Colón-Emeric CS. Physical Resilience in Older Adults: Systematic Review and Development of an Emerging Construct. J Gerontol A Biol Sci Med Sci 2016;71:489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Durand MA, Lamouroux A, Redmond NM, et al. Impact of a health literacy intervention combining general practitioner training and a consumer facing intervention to improve colorectal cancer screening in underserved areas: protocol for a multicentric cluster randomized controlled trial BMC Public Health 2021;21:1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The Accountable Health Communities Health-Related Social Needs Screening Tool Centers for Medicare & Medicaid Services, 2017. (Accessed June 22, 2022, at https://innovation.cms.gov/files/worksheets/ahcm-screeningtool.pdf) [Google Scholar]
- 31.Leinert C, Brefka S, Braisch U, et al. A complex intervention to promote prevention of delirium in older adults by targeting caregiver’s participation during and after hospital discharge - study protocol of the TRAnsport and DElirium in older people (TRADE) project BMC Geriatr 2021;21:646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barello S, Castiglioni C, Bonanomi A, Graffigna G. The Caregiving Health Engagement Scale (CHE-s): development and initial validation of a new questionnaire for measuring family caregiver engagement in healthcare. BMC Public Health 2019;19:1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Amani PJ, Hurtig AK, Frumence G, Kiwara AD, Goicolea I, San Sebastian M. Health insurance and health system (un) responsiveness: a qualitative study with elderly in rural Tanzania. BMC Health Serv Res 2021;21:1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fung CH, Martin JL, Liang LJ, et al. Efficacy of a patient decision aid for improving person-centered decision-making by older adults with obstructive sleep apnea J Clin Sleep Med 2021;17:121–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tinetti M, Dindo L, Smith CD, et al. Challenges and strategies in patients’ health priorities-aligned decision-making for older adults with multiple chronic conditions. PLoS One 2019;14:e0218249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carpenter CR, McFarland F, Avidan M, et al. Impact of Cognitive Impairment Across Specialties: Summary of a Report From the U13 Conference Series. J Am Geriatr Soc 2019;67:2011–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hunold KM, Goldberg EM, Caterino JM, et al. Inclusion of older adults in emergency department clinical research: Strategies to achieve a critical goal. Acad Emerg Med 2022. 29:376–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prusaczyk B, Cherney SM, Carpenter CR, Dubois JM. Informed Consent to Research with Cognitively Impaired Adults: Transdisciplinary Challenges and Opportunities Clin Gerontol 2017;40:63–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Natsky AN, Vakulin A, Chai-Coetzer CL, et al. Economic evaluation of cognitive behavioural therapy for insomnia (CBT-I) for improving health outcomes in adult populations: A systematic review. Sleep Med Rev 2020;54:101351. [DOI] [PubMed] [Google Scholar]
- 40.Dopheide JA. Insomnia overview: epidemiology, pathophysiology, diagnosis and monitoring, and nonpharmacologic therapy Am J Manag Care 2020;26:S76–S84. [DOI] [PubMed] [Google Scholar]
- 41.O’Leary MC, Hassmiller-Lich K, Frerichs L, Leeman J, Reuland DS, Wheeler SB. Extending analytic methods for economic evaluation in implementation science Implement Sci 2022;17:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Saldana L, Ritzwoller DP, Campbell M, Block EP. Using economic evaluations in implementation science to increase transparency in costs and outcomes for organizational decision-makers Implement Sci Commun 2022;3:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O’Halloran AM, Hartley P, Moloney D, McGarrigle C, Kenny RA, Romero-Ortuno R. Informing patterns of health and social care utilisation in Irish older people according to the Clinical Frailty Scale. HRB Open Res 2021;4:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Qin Y, Li J, McPhillips M, Lukkahatai N, Yu F, Li K. Association of fear of falling with frailty in community-dwelling older adults: A cross-sectional study. Nurs Health Sci 2021;23:516–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Muszalik M, Kotarba A, Borowiak E, Puto G, Cybulski M, Kedziora-Kornatowska K. Socio-Demographic, Clinical and Psychological Profile of Frailty Patients Living in the Home Environment and Nursing Homes: A Cross-Sectional Study. Front Psychatry 2021;12:736804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Allen JD, Shelton RC, Emmons KM, Linnan LA. Fidelity and Its Relationship to Implementation Effectiveness, Adaptation, and Dissemination. In: Brownson RC, Colditz GA, Proctor EK, eds. Dissemination and Implementation Research in Health: Translating Science into Practice 2nd ed. New York, NY: Oxford University Press; 2018:267–84. [Google Scholar]
- 47.Orton E, Lafond N, Skelton DA, et al. Implementation fidelity of the Falls Management Exercise Programme: a mixed methods analysis using a conceptual framework for implementation fidelity. Public Health 2021;197:11–8. [DOI] [PubMed] [Google Scholar]
- 48.Carter HE, Lee XJ, Farrington A, et al. A stepped-wedge randomised controlled trial assessing the implementation, effectiveness and cost-consequences of the EDDIE+ hospital avoidance program in 12 residential aged care homes: study protocol. BMC Geriatr 2021;21:347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ginsburg LR, Hoben M, Easterbrook A, Anderson RA, Estabrooks CA, Norton PG. Fidelity is not easy! Challenges and guidelines for assessing fidelity in complex interventions Trials 2021;22:372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Piamjariyakul U, Smothers A, Young S, et al. Verifying intervention fidelity procedures for a palliative home care intervention with pilot study results Res Nurs Health 2021;44:854–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.van de Sant AJW, de Vries NM, Hoogeboom TJ, Nijhuis-van der Sanden MWG. Implementation of a Personalized, Cost-Effective Physical Therapy Approach (Coach2Move) for Older Adults: Barriers and Facilitators. J Geriatr Phys Ther 2019;42:E1–E16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moberg J, Oxman AD, Rosenbaum S, et al. The GRADE Evidence to Decision (EtD) framework for health system and public health decisions Health Res Policy Syst 2018;16:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Parks A, Eagles D, Ge Y, Stiell IG, Cheung WJ. Barriers and enablers that influence guideline-based care of geriatric fall patients presenting to the emergency department. Emerg Med J 2019;36:741–7. [DOI] [PubMed] [Google Scholar]
- 54.van der Maaden T, van der Steen JT, Koopmans RTCM, et al. Symptom relief in patients with pneumonia and dementia: implementation of a practice guideline. Int J Geriatr Psychiatry 2017;32:829–39. [DOI] [PubMed] [Google Scholar]
- 55.Beauchemin M, Cohn E, Shelton RC. Implementation of Clinical Practice Guidelines in the Health Care Setting: A Concept Analysis ANS Adv Nurs Sci 2020;42:307–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bowling CB, Whitson HE, Johnson TM. The 5Ts: Preliminary Development of a Framework to Support Inclusion of Older Adults in Research. J Am Geriatr Soc 2019;67:342–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Croff R, Gowen LK, Lindauer A, Shofner S, Brown K, Eckstrom E. Including older rural adults in research: Practical guidance for addressing the NIH Inclusion Across the Lifespan policy J Clin Transl Sci 2020;4:431–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Walsh-Bailey C, Tsai E, Tabak RG, et al. A scoping review of de-implementation frameworks and models. Implement Sci 2021;16:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Norton WE, Chambers DA. Unpacking the complexities of de-implementing inappropriate health interventions Implement Sci 2020;15:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Niven DJ, Mrklas KJ, Holosinsky JK, et al. Towards understanding the de-adoption of low-value clinical practices: a scoping review. BMC Med 2015;13:255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ailabouni NJ, Reeve E, Helfrich CD, Hilmer SN, Wagenaar BH. Leveraging implementation science to increase the translation of deprescribing evidence into practice Res Social Adm Pharm 2022;18:2550–5. [DOI] [PubMed] [Google Scholar]
- 62.Brownson RC, Jacobs JA, Tabak RG, Hoehner CM, Stamatakis KA. Designing for dissemination among public health researchers: findings from a national survey in the United States Am J Public Health 2013;103:1693–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Leppin AL, Mahoney JE, Stevens KR, et al. Situating dissemination and implementation sciences within and across the translational research spectrum. J Clin Transl Sci 2019;4:152–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ibanez A, Yokoyama JS, Possin KL, et al. The Multi-Partner Consortium to Expand Dementia Research in Latin America (ReDLat): Driving Multicentric Research and Implementation Science. Front Neurol 2021;12:631722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Brownson RC, Jacob JA, Carothers BJ, et al. Building the Next Generation of Researchers: Mentored Training in Dissemination and Implementation Science. Acad Med 2021;96:86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tabak RG, Bauman AA, Summers-Holtrop J. Roles dissemination and implementation scientists can play in supporting research teams. Implement Sci Commun 2021;2:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lane-Fall MB, Curran GM, Beidas RS. Scoping implementation science for the beginner: locating yourself on the “subway line” of translational research BMC Med Res Methodol 2019;19:133. [DOI] [PMC free article] [PubMed] [Google Scholar]


