Abstract
Background:
Many advances have been made in hip labral repair and reconstruction and in the restoration of the suction seal.
Purpose/Hypothesis:
The purpose of this study was to evaluate the biomechanical effects of segmental labral reconstruction with a synthetic polyurethane scaffold (PS) in comparison with segmental labrectomy. Our hypothesis was that reconstruction with a icroporous polyurethane implant would normalize joint kinetics of the hip and restore the suction seal.
Study Design:
Controlled laboratory study.
Methods:
We used 10 hips from 5 fresh-frozen pelvises with an intact acetabular labrum without osteoarthritis. Using an intra-articular pressure measurement system, the contact area, contact pressure, and peak force were assessed for the following conditions: intact labrum, partial anterosuperior labrectomy, and PS reconstruction. For each condition, all specimens were analyzed in 4 positions (90° of flexion, 90° of flexion and internal rotation, 90° of flexion and external rotation, and 20° of extension) and underwent a labral seal test. The relative change from the intact condition was determined for all conditions and positions.
Results:
Compared with the intact labrum, labrectomy resulted in a significant decrease in the contact area (P < .001) and a significant increase in the peak force (P < .001) and contact pressure (P < .001) across all positions. Compared with labrectomy, PS reconstruction resulted in a significant increase in the contact area (P < .001) and a significant decrease in the contact pressure (P ≤ .02) and peak force (P < .001) across all positions. Compared with the intact labrum, PS reconstruction restored the contact area and peak force to normal values in all positions (P > .05), whereas the contact pressure was significantly decreased compared with labrectomy (P < .05) but did not return to normal values. The labral seal was lost in all specimens after labrectomy but was restored in 80% of the specimens after PS reconstruction.
Conclusion:
Femoroacetabular contact biomechanics significantly worsened after partial labrectomy; reconstruction using a PS restored the contact area and peak force to the intact state and improved the contact pressure increases seen after partial labrectomy. The contact area and peak force were normalized, and the labral seal was re-established in most cases.
Clinical Relevance:
This study provides biomechanical evidence for the use of a scaffold for labral reconstruction.
Keywords: labral reconstruction, biomechanics, polyurethane scaffold
The acetabular labrum plays a crucial role in the stability, lubrication, and kinematics of the hip joint. 2,13,14,16,23,27,29 The purpose of hip preservation surgery in the presence of femoroacetabular abnormalities is to maintain and preserve the anatomy, correcting morphological alterations and repairing the labral lesion (when possible instead of performing labral debridement). When this repair is not possible, reconstructing the acetabular labrum should be attempted with the aim of regaining joint function, decreasing pain, and allowing a return to activities of daily living. 2,11,20,22,27,29,43
When labral ruptures occur, the vast majority can be addressed with primary repair techniques. With the shift in recent decades from debridement to preservation, treatment methods that are aimed at restoring the negative pressure gradient created by the labral suction seal and improving contact mechanics have become popular. 10,13,37 Labral repair has been shown to have better clinical outcomes than labrectomy, 35 but when repair is not possible, labral reconstruction is indicated. 32 Performing allogeneic labral transplantation can achieve good results, but graft availability from tissue banks may be limited, and sizing may be challenging particularly when a more severe labral rupture than expected is diagnosed intraoperatively. In this situation, autografts can be used from the fascia lata or hamstring with satisfactory results. 24,28 The use of these autografts requires express authorization from the patient through informed consent and can also lead to possible morbidity in the donor area and an increase in surgical time. 2,7,9
As an alternative to human tissue usage, biodegradable, synthetic, polyethylene scaffolds were developed more than 15 years ago for restoration of the meniscus in the knee, with successful results clinically up to 10 years. 3,6,15,41 Owing to the abundant vascular supply in the acetabulum, 33 integration of the scaffold can be expected. With the lack of compressive and shear forces found in the knee, comparable or superior results may be obtained when implanted in the hip.
The objective of this biomechanical study was to evaluate the effect of reconstruction of an acetabular labral injury, caused by partial anterosuperior labrectomy, using an artificial macroporous polyurethane scaffold (PS). Our hypothesis was that partial anterosuperior labrectomy would decrease the contact area and increase the contact pressure and peak force compared with the intact acetabular labrum, while reconstruction with a macroporous PS would normalize joint kinetics of the hip and restore the labral seal.
Methods
Specimens
The protocol for this study was approved by the ethics committee of the local university. A total of 22 consecutively donated deidentified cadaveric hips (11 complete pelvises and proximal femurs) were obtained from a voluntary human body donation program of the local university, which complies with all legal and ethical procedures for human donation.
The complete pelvises were subjected to a fluoroscopic examination to confirm that there were no dysplastic hips, femoroacetabular impingement, or impairment of the femoral head (Wiberg angle of 25°-40°, alpha angle <55°) and that there was conservation of the joint space (Tönnis grade <2). No specimens with a severe osteochondral lesion were detected radiographically; however, 4 specimens (2 pelvises) presented with severe osteochondral damage on direct inspection and were therefore excluded.
The cadaveric hips were handled following a previously described protocol; however, they were not separated, and the pelvises were kept intact. 26,44 Briefly, the specimens were thawed at room temperature for 12 hours, then carefully dissected, and all the muscles and soft tissue were systematically eliminated. They were then refrozen to be thawed on the day of biomechanical testing. After testing, the pelvises were frozen a third time using the same protocol to preserve them for revalidation if necessary. None of the specimens required a third thawing.
Biomechanical Testing
There were 3 complete pelvises (6 specimens) used for a pilot study to test the calibration and sensor positioning and to refine the reconstruction technique and biomechanical workflow. One pelvis (2 specimens) did not allow for correct positioning of the sensor because of the small size of the acetabulum. These cases were not included in the study. This left 5 pelvises (10 hips) remaining for testing.
The complete pelvis specimens were fixed in an anatomic position on a biomechanical testing bench (Figure 1). This bench allows for angular control in the 3 axes of joint mobility. In the absence of servomotors for movement control, maximum mobility for each specimen can be achieved. The design and methodology have been previously described. 21,39
Figure 1.
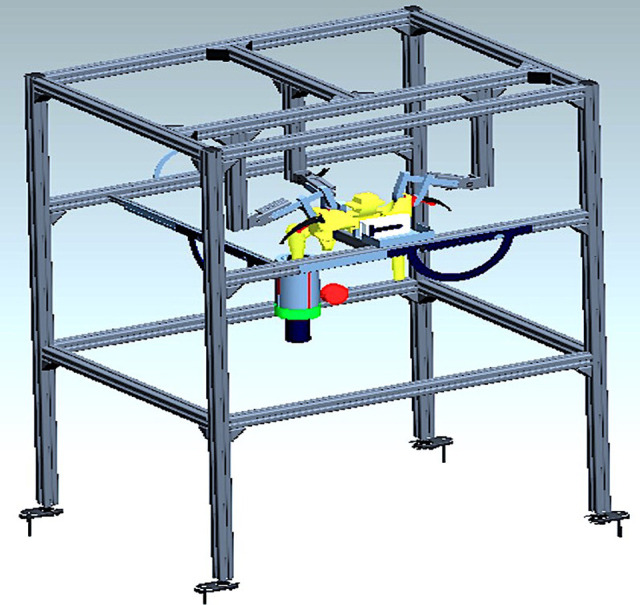
Schematic diagram of the bench used to secure the specimens.
Testing was carried out in 3 different clinical situations for each specimen: (1) with the acetabular labrum intact, (2) after 3 cm–long anterior labrectomy, and (3) after labral reconstruction with a PS.
Intact Labrum
Although normally carried out arthroscopically, for the purposes of this study, we performed an open procedure. Wide 360° capsulotomy was performed on each specimen to 2 mm of the acetabular rim, and the round ligament was sectioned (Figure 2). Visual inspection confirmed the integrity of the acetabular labrum and the state of the acetabular cartilage. Capsulotomy was carried out to manipulate the acetabular labrum to insert dynamic pressure sensors with a semicircle design (model 4400; Tekscan). The sensors were calibrated according to manufacturer guidelines and attached to the capsule and labrum with 3-point capsular sutures (silk 2/0) (Figure 2), achieving a static position during testing and allowing for reproducible measurements. 31
Figure 2.

Tekscan sensor’s cotyloid cavity attachment after joint capsule resection and round ligament sectioning to remove the femoral head. Articular cartilage (crescent shape) (a); acetabular labrum (b); distally sectioned round ligament (c); acetabular fossa (d); transverse ligament (e); and ischial tuberosity (f). The numbers show the distribution in zones according to the clockface position.
A precision dynamometer (Digital Force Gauge SF-500; Beslands) was used to ensure that stable pressure was maintained throughout the study for all specimens (maximum load: 500 N/50 kg; load division value: 0.1 N/0.01 kg; inner sensor accuracy: ±0.5%; operating temperature: –15° to 35°C; transport temperature: 23° to 60°C; relative humidity: 15% to 80%).
The peak force, contact pressure, and contact area of the acetabular cartilage were measured after the introduction of the femoral head into the acetabular cavity. The same 4 sequences of movement were reproduced for each specimen. Dynamic testing began from the anatomic position in extension, neutral rotation, and neutral abduction, and progressive flexion was performed to 90°. The joint was then brought to maximum internal rotation (flexion + IR), followed by maximum external rotation (flexion + ER) and back to neutral, finishing with an excursion at 20° of extension. The mean of 3 consecutive examinations was used for each measurement. Movement was carried out manually, timing and documenting each position. Throughout the study, a constant compressive force of 50 N was applied with the dynamometer, with a variation of ±5 N. Each cycle lasted 30 seconds (±10%). If greater variations in strength or duration occurred, they were discarded and the cycle repeated. Each test was repeated 3 times, and the mean of the results was used (Figure 3).
Figure 3.
Cycle performed on a biomechanical bench with a 50-N dynamometer fixed intramedullary in the distal femur with K-wire to manipulate rotations: (A) 90° of flexion, (B) 90° of flexion plus maximum internal rotation (arrow), (C) 90° of flexion plus maximum external rotation (arrow), and (D) 20° of extension (arrow).
Labrectomy
After testing with the intact native labrum was completed, the pressure sensor was detached from the capsule, and the capsule was retracted laterally. A longitudinal labral cut of 3 cm in length in the anterolateral zone was performed with a No. 10 scalpel, leaving a 2-mm lateral margin for later attachment of the scaffold (Figure 4). The sensor was reattached to the capsule and the specimen repositioned on the bench. Testing was performed with the routine described above.
Figure 4.

Anterosuperior labrectomy of 3 cm performed on a right hip, with resected labrum (a) and native labrum (b). The number represents the 12-o’clock position.
PS Reconstruction
After testing in the labrectomy condition, the sensor was removed as described above. Reconstruction was carried out with the insertion of a biodegradable, synthetic PS (Actifit; Orteq). This scaffold is highly porous and composed of aliphatic polyurethane (Figure 5). There were three 5-mm anchors (Wedge Anchor II with No. 2 Force Fiber; Stryker) placed every 7 mm in the middle to secure the implant, and 1 side-to-side suture was used to attach the labral remnant at each end (Figure 6). Because of the quality of the bone for specimen 8, an extra anchor was used in the middle of the scaffold. Testing was completed as described above.
Figure 5.

Macroporous polyurethane implant (Actifit).
Figure 6.
(A) Reconstruction with a polyurethane implant (specimen 4, left hip) using 3 anchors and 2 side-to-side translabral sutures. (B) Superior and side view of the sensor position fixed with silk sutures. Sup, superior; Med, medial; Lat, lateral, Inf, inferior.
Labral Seal Testing
The suction seal test 37 consisted of a qualitative type of analysis that was performed with the hip in a neutral anatomic position. After capsulotomy, a section of the round ligament of the femoral head was rearticulated, and an axial distraction force was applied according to Suppauksorn et al 37 and rated qualitatively to see if the seal was maintained. Losing the seal or vacuum results in a negative sealing pressure that produces an audible sound and dislocation of the hip. If the seal is not maintained, no resistance to the distracting force is perceived, nor is the sound heard. This test was performed on all specimens to determine if it was present in the intact labrum, after labrectomy, and again after reconstruction with the PS. All labral seal tests were performed by the same investigator (B.C.).
Statistical Analysis
We measured quantitative variables: maximum pressure determined by the peak force and contact area on the acetabular surface. These 2 parameters were measured in each specimen in 3 predetermined clinical situations. When measuring the contact area, normalization of the values was necessary, as each hip was of a different size and adaptation of the sensor may have been influenced by that difference. This was achieved by dividing the raw data for each value of stage 1 (intact labrum).
PS values were normalized to analyze differences in the peak force, contact area, and contact pressure and were compared with the intact state using measurements from the 4 different positions (90° of flexion in neutral, flexion + IR, flexion + ER, and 20° of extension). Because multiple measurements were taken per specimen, normalized values were modeled using repeated-measures analysis of variance to account for potential correlations within each specimen. The least squares means and 95% CIs are reported, along with a P value that reflects the test: H0: mean = 1 versus H1: mean ≠ 1. Statistical significance was set at P < .05 with an alpha error of .05 and an effect size of 0.8. Statistical analyses were performed using SAS (Version 9.4; SAS Institute).
To assess each specific area of the acetabular surface, an analysis of the data was carried out for each of the 4 positions. The peak force, contact area, and contact pressure on the acetabular surface were compared in the following situations: (1) intact labrum versus labrectomy, (2) intact labrum versus PS-reconstructed labrum, and (3) labrectomy versus PS-reconstructed labrum. The relative change from the intact condition (value of 1) was determined for all conditions and positions.
Results
Contact Area
In comparison with the intact labrum, labrectomy resulted in a significant decrease in the contact area. In flexion, it decreased to 82% of normal values (95% CI, 0.77-0.87), in flexion + IR to 83% (95% CI, 0.78-0.88), in flexion + ER to 83% (95% CI, 0.78-0.88), and in extension to 82% (95% CI, 0.76-0.86) (P < .001 for all).
After labrectomy, which decreased the contact area, PS reconstruction restored the contact area to more than 96% of the intact labrum in all positions (P > .05), with no statistically significant differences found between PS and native values. In flexion, the contact area was restored to 96% (95% CI, 0.93-1.00; P = .061), in flexion + IR to 98% (95% CI, 0.94-1.01; P = .187), in flexion + ER to 98% (95% CI, 0.94-1.02; P = .243), and in extension to 97% (95% CI, 0.93-1.00; P = .076). When the contact area of PS reconstruction was compared with labrectomy, the values were significantly increased in all positions (P < .001).
Contact Pressure
The contact pressure increased significantly after partial labrectomy compared with the intact labrum in all positions (P < .001 for all). In flexion, it increased 1.28% (95% CI, 1.19-1.38); in flexion + IR, 1.28% (95% CI, 1.19-1.38); in flexion + ER, 1.32% (95% CI, 1.23-1.42); and in extension, 1.28% (95% CI, 1.19-1.38).
Compared with the partial labrectomy state, PS reconstruction significantly decreased the contact pressure, but the values still remained significantly higher than the intact state in all positions (flexion: 11% increase [95% CI, 1.05-1.17]; P = .003) (flexion + IR: 8% [95% CI, 1.03-1.13]; P = .008) (flexion + ER: 11% [95% CI, 1.04-1.16]; P = .0004) (extension: 12% [95% CI, 1.03-1.21]; P = .02). Figure 7 represents a 3-dimensional visualization of the results. When comparing the contact pressure of PS reconstruction with labrectomy, all P values were statistically significant for all positions (P = .02).
Figure 7.
A 3-dimensional (3D) visualization of contact pressure across all positions. Interpretation of a Tekscan software image, scaled from blue to red, where the areas of least pressure are dark blue and of the highest pressure are red. ER, external rotation; IR, internal rotation.
Peak Force
When comparing the intact labrum with partial labrectomy, the peak force increased significantly in all positions: 27% (95% CI, 1.19-1.35) in flexion, 25% (95% CI, 1.17-1.33) in flexion + IR, 22% (95% CI, 1.14-1.29) in flexion + ER, and 26% (95% CI, 1.19-1.34) in extension (P < .001 for all).
When comparing the peak force between the intact labrum and PS reconstruction, we observed a recovery of more than 95% of the peak force, with no statistically significant differences found. In flexion, the peak force decreased to 5% above normal values (95% CI, 0.99-1.11; P = .07) from the labrectomy state; in flexion + IR, it decreased to 3% (95% CI, 0.99-1.07; P = .20), in flexion + ER to 2% (95% CI, 0.99-1.05; P = .26), and in extension to 4% (95% CI, 1.00-1.08; P = .07). When comparing the peak force of PS reconstruction with labrectomy, the differences were statistically significant for all positions (P < .001).
In summary, reconstruction with a synthetic PS significantly increased the contact area (P < .001) and significantly decreased both the contact pressure (P ≤ .02) and peak force (P < .001) compared with the effects caused by partial labrectomy, bringing the alteration in joint kinematics closer to the intact condition. Box plots for all procedures and conditions can be found in Figure 8.
Figure 8.
Box plots showing the distribution of (A) contact area, (B) contact pressure, and (C) peak force by procedure and position compared with normal (1.0). Lab, labrectomy; Nor, normal; PS, polyurethane scaffold.
Labral Seal
The labral seal was preserved in 100% of the intact labrum specimens but was lost in 100% of cases after labrectomy. The seal was restored in 80% of the specimens after PS reconstruction.
Discussion
The most important finding of this study was that partial reconstruction of the labrum with a macroporous PS restored joint kinematics to that of the intact labrum, restoring the contact area and peak force back to normal and improving the contact pressure closer to normal than the partial labrectomy state. Labral reconstruction with a PS restored the labral seal in the majority of cases.
In anatomic studies, the acetabular labrum increased the contact area of the cotyloid cavity by 28%. 38 This increases congruence and joint stability, allowing the correct distribution of loads while reducing contact pressure and stress in the joint cartilage. 5 In all measurements made in this biomechanical study, partial anterosuperior labrectomy decreased the contact area from normal, on average, to 82%. It is interesting to note that despite being partial anterosuperior labrectomy of 3 cm, it produced a decrease in the contact area similar to that of total labrectomy that was reported in a previous study. 39 PS reconstruction managed to increase the contact area after labrectomy by normalizing that parameter relative to the intact labrum. Our results showed that reconstruction with a PS re-established the contact area and normalized intra-articular stress, which was consistent with the cadaveric study by Philippon et al, 29 demonstrating that labral reconstruction produced improvements in the hip joint’s contact area and contact pressure compared with labral resection.
One of the main functions of the labrum is to distribute pressures in the femoroacetabular joint. 25 In vivo and in vitro biomechanical studies have shown that the intact labrum allows direct pressure loads from solid-to-solid and interstitial fluid to be evenly distributed within the femoroacetabular joint. 14 This is corroborated by the results of this study, which showed that the intra-articular contact pressure increased significantly after partial anterosuperior labrectomy compared with the intact labrum and that the contact pressure decreased significantly with PS reconstruction. Although reconstruction decreased the contact pressure, it did not return to normal values of the intact labrum.
There is a relationship between increased stress forces and damage to the chondral surface, which has been described as an independent risk factor of osteoarthritis. 17 Areas of cartilage exposed to higher loads may have an increased risk of damage and a reduced ability to effectively distribute loads during movement. 18 Shi et al 34 reported that labral reconstruction with an autograft in a porcine model provides benefits in terms of reducing the development of osteoarthritis compared with labral resection. They concluded that the development of osteoarthritis can be attenuated by labral reconstruction, contributing to homeostasis of the hip joint. 34 In this study, the peak force increased significantly after partial labrectomy but decreased significantly after reconstruction with the PS to approximately 95% of normal values. While not normalizing the contact pressure to the intact state, if it manages to restore the peak force close to normal, a decrease in elevated tissue deformation and shear forces that produce fibrillation and chondral delamination could occur, 4 which may attenuate the progression of osteoarthritis.
The positions of 90° of flexion, 20° of extension, and maximum internal and external rotation at 90° of flexion were chosen with the aim of analyzing whether joint kinetics could be reconstructed throughout the cone of circumduction of the enarthrosis. 19 In the range of motion that we studied, reconstruction with a PS after labrectomy normalized the contact area, contact pressure, and peak force. We also observed that labral reconstruction restored joint kinetics in internal and external rotation at 90°.
Biomechanical cadaveric studies have shown that simulated labral injury or resection conditions decrease the pressurization of intra-articular fluid 29 and decrease distraction resistance 27 but that repair and reconstruction improve the distracting stability of the hip fluid seal. Ejnisman et al 12 demonstrated that incorporation of the allograft and maintenance of the suction seal in the joint were obtained. To analyze this scenario in depth, Suppauksorn et al 37 compared the results of primary labral repair of an anterosuperior lesion and 270° allograft reconstruction in 8 cadaveric specimens. They found that when reconstruction was performed at 270°, there was a decrease in the intra-articular contact area and a greater loss of the labral seal compared with labral repair. With the “suction seal test” that they described, 100% of the specimens with labral repair recovered the seal compared with only 22.5% with 270° reconstruction. Our results using the same labral seal test showed that the labral seal after wide capsulotomy was maintained in 100% of the intact labrum specimens, that 100% of specimens after partial labrectomy lost their labral seal, but that it was re-established in 80% of specimens after reconstruction with the PS. Unlike the study of Suppauksorn et al, our study analyzed reconstruction after 3-cm partial anterosuperior labrectomy, not total labrectomy after 270° reconstruction. This could explain the difference between our 80% recovery of the seal and their 22.5% rate with reconstruction at 270°. Based on these results, it could be suggested that it is better to perform partial reconstruction rather than 270° reconstruction to recover the labral seal function.
Limitations
There are limitations to our study. Although the initial sample size was 22 specimens, only 10 specimens were included in the biomechanical study. This was a relative limitation, as most sample sizes in biomechanical cadaveric studies are 5 to 10 specimens. 1,36,37,39 The Tekscan sensors utilized in this study were specifically designed for use in the hip. They are arranged in a semicircle and connected by USB to a computer. Their 5 connectors are approximately 1 cm wide and are separated by 1.5 cm. This requires wide capsulotomy with a section of the ligamentum teres to be able to insert and fix the sensor in the required position, which may affect the study in terms of the distribution of loads and the subjectivity of the suction seal test. However, this was not considered a significant limitation, as we compared 3 clinical conditions with the same instability that is produced by total capsulotomy. The hip joint is a system that requires the capsule to maintain joint liquid. Despite having lubricated the cartilage with saline and cadaveric fat, it may not have remained in the same condition as normal. Pressures measured in the study may differ from those measured in a surgical setting, making the raw value of the data not transferable. However, this bias is understood in all cadaveric biomechanical studies with a similar study protocol. 21,27,29,37,40 The biomechanical bench used in this study permitted the specimens to be placed in an anatomic position and allowed for unlimited hip range of motion, with analog control of all angles of motion. The angular measurements were made on that bench with a visual analog system; however, angular measurements can sustain a bias. A goal in this study was to standardize range of motion for each specimen, limiting the differences among the specimens. Finally, the PS used in this study was developed for meniscal replacement in the knee but was adapted to the hip. Although there are clinical and histological studies of this implant that show that it integrates well in the knee and no inflammatory response has been reported up to 10 years, 8,30,41,42 it is largely unknown how this implant will act in the hip. We are limited, at present, by the study of Tey-Pons et al, 39,40 who observed good clinical outcomes at 4 years’ follow-up and no progression to osteoarthritis using the same scaffold as in this study.
Conclusion
The biomechanical effects of a synthetic PS for labral reconstruction are described for the first time. Femoroacetabular contact biomechanics significantly worsened after partial labrectomy; reconstruction with a PS restored the contact area and peak force to the intact state and improved the contact pressure increases seen after partial labrectomy. The contact area and peak force were normalized. The labral seal was preserved after complete capsulotomy but was lost after partial labrectomy and re-established in 80% of cases after reconstruction with a PS. Further studies are needed to compare the results with other autograft reconstruction techniques.
Acknowledgment
The authors acknowledge Miriam Hidalgo and Marçal Asso for their invaluable work in the anatomy laboratory and Dr Eduard Tornero for his support with statistical analysis.
Footnotes
Final revision submitted May 18, 2022; accepted May 26, 2022.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Hospital Universitari de Girona Doctor Josep Trueta (No. 2018/8109/I).
References
- 1. Afoke NY, Byers PD, Hutton WC. Contact pressures in the human hip joint. J Bone Joint Surg Br. 1987;69(4):536–541. [DOI] [PubMed] [Google Scholar]
- 2. Ayeni OR, Alradwan H, de Sa D, Philippon MJ. The hip labrum reconstruction: indications and outcomes–-a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):737–743. [DOI] [PubMed] [Google Scholar]
- 3. Bouyarmane H, Beaufils P, Pujol N, et al. Polyurethane scaffold in lateral meniscus segmental defects: clinical outcomes at 24 months follow-up. Orthop Traumatol Surg Res. 2014;100(1):153–157. [DOI] [PubMed] [Google Scholar]
- 4. Bsat S, Frei H, Beaule PE. The acetabular labrum: a review of its function. Bone Joint J. 2016;98-B(6):730–735. [DOI] [PubMed] [Google Scholar]
- 5. Buckwalter JA, Mankin HJ, Grodzinsky AJ. Articular cartilage and osteoarthritis. Instr Course Lect. 2005;54:465–480. [PubMed] [Google Scholar]
- 6. Condello V, Dei Giudici L, Perdisa F, et al. Polyurethane scaffold implants for partial meniscus lesions: delayed intervention leads to an inferior outcome. Knee Surg Sports Traumatol Arthrosc. 2021;29(1):109–116. [DOI] [PubMed] [Google Scholar]
- 7. Cooper JD, Dekker TJ, Ruzbarsky JJ, et al. Autograft versus allograft: the evidence in hip labral reconstruction and augmentation. Am J Sports Med. 2021;49(13):3575–3581. [DOI] [PubMed] [Google Scholar]
- 8. de Caro F, Perdisa F, Dhollander A, Verdonk R, Verdonk P. Meniscus scaffolds for partial meniscus defects. Clin Sports Med. 2020;39(1):83–92. [DOI] [PubMed] [Google Scholar]
- 9. DeFroda SF, Kester BS, Clapp IM, Newhouse AC, Nho SJ. Arthroscopic treatment of femoroacetabular impingement using labral reconstruction with capsular autograft. Arthrosc Tech. 2021;10(10):e2375–e2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dwyer MK, Jones HL, Field RE, McCarthy JC, Noble PC. Femoroacetabular impingement negates the acetabular labral seal during pivoting maneuvers but not gait. Clin Orthop Relat Res. 2015;473(2):602–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ejinsman L, Philippon MJ. Arthroscopic labral reconstruction in the hip using iliotibial band autograft. Oper Tech Sports Med. 2011;19(2):134–139. [Google Scholar]
- 12. Ejnisman L, Philippon MJ, Lertwanich P. Acetabular labral tears: diagnosis, repair, and a method for labral reconstruction. Clin Sports Med. 2011;30(2):317–329. [DOI] [PubMed] [Google Scholar]
- 13. Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36(2):171–178. [DOI] [PubMed] [Google Scholar]
- 14. Ferguson SJ, Bryant JT, Ganz R, Ito K. The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech. 2000;33(8):953–960. [DOI] [PubMed] [Google Scholar]
- 15. Figueroa D, Figueroa F, Calvo R, Gomez C, Vaisman A. Meniscal polyurethane scaffold plus cartilage repair in post meniscectomy syndrome patients without malalignment improves clinical outcomes at mid-term follow-up. J Clin Orthop Trauma. 2020;15:16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Greaves LL, Gilbart MK, Yung AC, Kozlowski P, Wilson DR. Effect of acetabular labral tears, repair and resection on hip cartilage strain: a 7T MR study. J Biomech. 2010;43(5):858–863. [DOI] [PubMed] [Google Scholar]
- 17. Hadley NA, Brown TD, Weinstein SL. The effects of contact pressure elevations and aseptic necrosis on the long-term outcome of congenital hip dislocation. J Orthop Res. 1990;8(4):504–513. [DOI] [PubMed] [Google Scholar]
- 18. Hunt MA, Charlton JM, Esculier JF. Osteoarthritis year in review 2019: mechanics. Osteoarthritis Cartilage. 2020;28(3):267–274. [DOI] [PubMed] [Google Scholar]
- 19. Kapandji AI. Articular Physiology Notebooks: Hip. 3rd ed. Masson; 1984. [Google Scholar]
- 20. Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46–53. [DOI] [PubMed] [Google Scholar]
- 21. Lee S, Wuerz TH, Shewman E, et al. Labral reconstruction with iliotibial band autografts and semitendinosus allografts improves hip joint contact area and contact pressure: an in vitro analysis. Am J Sports Med. 2015;43(1):98–104. [DOI] [PubMed] [Google Scholar]
- 22. Lynch TS, Minkara A, Aoki S, et al. Best practice guidelines for hip arthroscopy in femoroacetabular impingement: results of a Delphi process. J Am Acad Orthop Surg. 2020;28(2):81–89. [DOI] [PubMed] [Google Scholar]
- 23. Maldonado DR, Kyin C, Chen SL, et al. In search of labral restoration function with hip arthroscopy: outcomes of hip labral reconstruction versus labral repair: a systematic review. Hip Int. 2021;31(6):704–713. [DOI] [PubMed] [Google Scholar]
- 24. Matsuda DK, Burchette RJ. Arthroscopic hip labral reconstruction with a gracilis autograft versus labral refixation: 2-year minimum outcomes. Am J Sports Med. 2013;41(5):980–987. [DOI] [PubMed] [Google Scholar]
- 25. Mavcic B, Iglic A, Kralj-Iglic V, Brand RA, Vengust R. Cumulative hip contact stress predicts osteoarthritis in DDH. Clin Orthop Relat Res. 2008;466(4):884–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Moon DK, Woo SL, Takakura Y, Gabriel MT, Abramowitch SD. The effects of refreezing on the viscoelastic and tensile properties of ligaments. J Biomech. 2006;39(6):1153–1157. [DOI] [PubMed] [Google Scholar]
- 27. Nepple JJ, Philippon MJ, Campbell KJ, et al. The hip fluid seal, part II: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip stability to distraction. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):730–736. [DOI] [PubMed] [Google Scholar]
- 28. Philippon MJ, Arner JW, Crawford MD, Bolia IK, Briggs KK. Acetabular labral reconstruction with iliotibial band autograft: outcome and survivorship at a minimum 10-year follow-up. J Bone Joint Surg Am. 2020;102(18):1581–1587. [DOI] [PubMed] [Google Scholar]
- 29. Philippon MJ, Nepple JJ, Campbell KJ, et al. The hip fluid seal, part I: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722–729. [DOI] [PubMed] [Google Scholar]
- 30. Reale D, Lucidi GA, Grassi A, et al. A comparison between polyurethane and collagen meniscal scaffold for partial meniscal defects: similar positive clinical results at a mean of 10-years of follow-up. Arthroscopy. 2022;38(4):1279–1287. [DOI] [PubMed] [Google Scholar]
- 31. Rudert MJ, Ellis BJ, Henak CR, et al. A new sensor for measurement of dynamic contact stress in the hip. J Biomech Eng. 2014;136(3):035001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Safran N, Rath E, Haviv B, Atzmon R, Amar E. The efficacy of labral reconstruction: a systematic review. Orthop J Sports Med. 2021;9(2):2325967120977088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Seeley MA, Georgiadis AG, Sankar WN. Hip vascularity: a review of the anatomy and clinical implications. J Am Acad Orthop Surg. 2016;24(8):515–526. [DOI] [PubMed] [Google Scholar]
- 34. Shi Y, Chen L, Xu Y, et al. Acetabular labral reconstruction using autografts reduces osteoarthritis development compared with labral resection in a porcine model. Am J Transl Res. 2019;11(4):2484–2495. [PMC free article] [PubMed] [Google Scholar]
- 35. Signorelli C, Bonanzinga T, Lopomo N, et al. Evaluation of the sealing function of the acetabular labrum: an in vitro biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):62–71. [DOI] [PubMed] [Google Scholar]
- 36. Smith MV, Panchal HB, Ruberte Thiele RA, Sekiya JK. Effect of acetabular labrum tears on hip stability and labral strain in a joint compression model. Am J Sports Med. 2011;39(suppl):103S–110S. [DOI] [PubMed] [Google Scholar]
- 37. Suppauksorn S, Beck EC, Chahla J, et al. Comparison of suction seal and contact pressures between 270 degrees labral reconstruction, labral repair, and the intact labrum. Arthroscopy. 2020;36(9):2433–2442. [DOI] [PubMed] [Google Scholar]
- 38. Tan V, Seldes RM, Katz MA, et al. Contribution of acetabular labrum to articulating surface area and femoral head coverage in adult hip joints: an anatomic study in cadavera. Am J Orthop (Belle Mead NJ). 2001;30(11):809–812. [PubMed] [Google Scholar]
- 39. Tey-Pons M. Study of the Function of the Acetabular Labrum in the Biomechanics of the Hip. Doctoral dissertation. Universitat Autònoma de Barcelona; 2015. [Google Scholar]
- 40. Tey-Pons M, Capurro-Soler B, Torres-Eguia R, Marques-Lopez F, Leon-Garcia A, Amrin-Pena O. Labral reconstruction with polyurethane implant. J Hip Preserv Surg. 2021;8(suppl 1):i34–i40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Toanen C, Dhollander A, Bulgheroni P, et al. Polyurethane meniscal scaffold for the treatment of partial meniscal deficiency: 5-year follow-up outcomes: a European multicentric study. Am J Sports Med. 2020;48(6):1347–1355. [DOI] [PubMed] [Google Scholar]
- 42. Verdonk P, Beaufils P, Bellemans J, et al. Successful treatment of painful irreparable partial meniscal defects with a polyurethane scaffold: two-year safety and clinical outcomes. Am J Sports Med. 2012;40(4):844–853. [DOI] [PubMed] [Google Scholar]
- 43. White BJ, Herzog MM. Labral reconstruction: when to perform and how. Front Surg. 2015;2:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Woo SL, Orlando CA, Camp JF, Akeson WH. Effects of postmortem storage by freezing on ligament tensile behavior. J Biomech. 1986;19(5):399–404. [DOI] [PubMed] [Google Scholar]






