Summary
This meta-analysis compared the clinical outcomes between two alternative surgeries for patients with cervical spondylosis, namely anterior cervical discectomy and fusion (ACDF) without plate (ACDFWP) vs. anterior cervical disc arthroplasty (ACDA). We searched databases, including PubMed, EMBASE, Cochrane Library, Google Scholar, and Web of Science (firstly available-2019). A standard meta-analysis was performed with the included studies. A Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool was used for the evaluation of the study quality of nonrandomized-controlled trials (nRCTs), while a Risk of Bias (RoB) battery was used for randomized controlled trials (RCTs). Eight studies involving 640 patients were included. No significant difference was found in the indices of Neck Disability Index (NDI) score, Visual Analog Score (VAS), Japanese Orthopaedic Association (JOA) score, operative time, blood loss, Swallowing Quality of Life Score (SWAL-QL), and complications. Cervical alignment was significantly better in the ACDFWP than in ACDA (mean difference (MD) = −0.67, 95% confidence interval (CI) [−1.11, −0.23], P = 0.003, I2 = 20%). Although the alternative ACDFWP was slightly superior in terms of the index of cervical alignment, the limited research on this subject present insufficient evidence. Further well-designed studies are warranted in the future.
Keywords: cervical spondylosis, anterior cervical discectomy and fusion without plate, anterior cervical disc arthroplasty, cervical alignment, meta-analysis
1. Introduction
Cervical spondylosis is a common disease characterized by progressive degeneration in the cervical spine and is regarded as a natural process of aging. The main symptoms of cervical spondylosis are neck pain and neck stiffness. Recently, an increasing number of young people are experiencing cervical spondylosis. It has been a public health concern related to remarkable disease burden. Since the 1950s, anterior cervical discectomy and fusion (ACDF) with plate has been regarded as the gold standard of therapy for cervical spondylosis (1-3). Although it has been well documented regarding its satisfactory efficacy, some complications, such as dysphagia (4), hoarseness (2), and adjacent segment disease (ASD) (3) are also reported. Some authors believe that these complications are caused by the influence of anterior vertebral plate fixation (4). Kepler et al. found that the fusion itself may contribute to more pressure between the adjacent segmental discs (5). Moreover, ASD might also result from the progression of cervical degeneration (6,7). Thus, the conventional ACDF with plate has limitations, and the adverse events cannot be ignored. To prevent these adverse events, alternative surgeries, such as ACDF without plate (ACDFWP) and anterior cervical disc arthroplasty (ACDA) were developed against cervical spondylosis (Figure 1).
Figure 1.
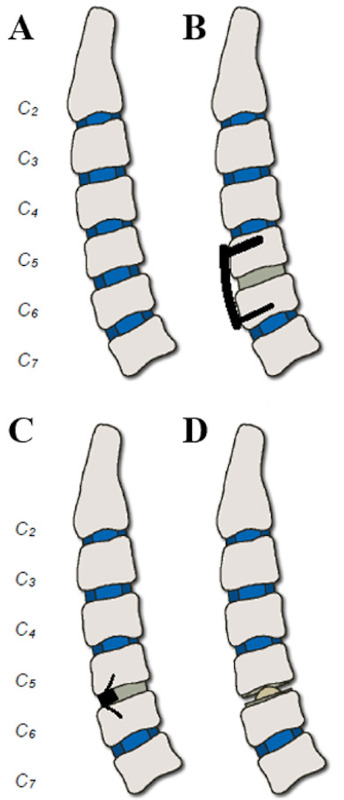
Schematic diagram of the surgeries for cervical spondylosis. A. Schematic diagram of the cervical spine. B. Conventional anterior cervical discectomy and fusion (ACDF) with plate. C. Anterior cervical discectomy and fusion without plate (ACDFWP). D. Anterior cervical disc arthroplasty (ACDA). Most of previous studies compared ACDF with plate and ACDA (B vs.D), in the present study we compared ACDFWP vs. ACDA (C vs. D).
Currently, many studies have reported a comparison of the clinical outcomes of conventional ACDF (with plate) and alternative ACDFWP. Recently, Cheung et al. found that ACDFWP provides better clinical outcomes than conventional ACDF (with plate) (8). Other studies have also compared the clinical outcomes between conventional ACDF (with plate) and ACDA. Latka et al. reported that compared to conventional ACDF (with plate), ACDA significantly lowered the probability of ASD development at the 60-month follow-up. (9). And Maharaj et al. compared ACDA and ACDF (including with and without plate). They found that ACDA has superiority in terms of reoperation rate and reduction in neurological deficits (10). However, to our knowledge, no meta-analyses have compared the clinical outcomes between alternative surgeries, ACDFWP and ACDA. Thus, in order to provide a complete chain of evidence to enable the selection of an appropriate surgical technique for cervical spondylosis treatment by the clinicians, we designed this study to compare the clinical outcomes of the alternative ACDFWP and ACDA (Figure 1), strictly as per the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (11).
2. Materials and Methods
2.1. Literature search strategy
English-language search of databases, including PubMed, EMBASE, Cochrane Library, Google Scholar, and Web of Science was performed with the keywords of "cervical spondylosis" AND "anterior cervical" AND "arthroplasty" AND "discectomy and fusion" OR "replacement". Studies from firstly available-2021 were included.
As per the inclusion criteria, (i) studies that compared the clinical outcomes between ACDA and ACDFWP in patients with cervical spondylosis, (ii) studies where complete data were available, (iii) randomized controlled trials (RCTs) and nonrandomized-controlled trials (nRCTs), and (iv) studies wherein at least one of the following assessments for clinical outcomes were reported: Neck Disability Index (NDI) score, Visual Analog Score (VAS), Japanese Orthopaedic Association (JOA) score, cervical alignment (The overall sagittal alignment of the cervical spine was calculated by the Cobb angle between the C2 and C7 vertebrae on the lateral radiograph), operative time, blood loss, complications, and Swallowing Quality of Life Score (SWAL-QL), were included. Furthermore, (i) non-English studies, (ii) review papers, (iii) meta-analyses, (iv) case reports and serious case reports, as well as (v) letters were excluded.
2.2. Data extraction
Three authors (JP, SL, XL) performed the literature search, read the title and abstract, and then screened the studies as per the inclusion/exclusion criteria. Subsequently, a senior scientist (TA) cross-checked and confirmed the quality of the included literature. Three authors (JP, SL, HS) extracted information (information of enrolled patients, therapy, experimental design, and outcome assessments) from the final selection of studies. We classified the assessments into two groups. One group contained indices that directly evaluated the clinical outcomes, including the NDI, VAS, JOA and cervical alignment; anther group contained the other factors associated with the surgeries, including operative time, blood loss, complications, and SWAL-QL. We discussed the data every day to reach consensus. Finally, all the data were checked by third-party authors (DZ, RZ, MH, PL) before submission for the meta-analysis.
2.3. Statistical analyses
We designed and performed this study strictly as per the PRISMA guidelines (11). We employed a RevMan 5.3 software (The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark) for the meta-analysis. The odds ratio (OR) and the corresponding 95% confidence interval (CI) were calculated for the dichotomous outcomes. The mean difference (MD), and the 95% CI were calculated for the continuous data. During the homogeneity test, when p ≥ 0.1 and I2 ≤ 50%, the studies were considered to be homogeneous, which were analyzed with a fixed-effect model; when p < 0.1 and I2 > 50%, the studies were regarded to be heterogeneous, which were analyzed with a random-effects model. Subgroups analyses were performed for considering the subgroups in some groups, such as VAS (neck and arm), cervical alignment (whole and local) and complications (ASD is regarded as the most important adverse event).
2.4. Assessment of study quality of the included studies
Three authors (SL, JP and RX) performed quality assessment for the study. A Risk of Bias (RoB) in Non-randomized Studies of Interventions (ROBINS-I) tool (12) was employed to assess the study quality of nRCTs. A RoB battery developed by the Cochrane Collaboration was used for the RCTs (13).
3. Results
3.1. Literature searching results
Total 3100 studies were identified in the first search. First, duplicate studies (1,198) and those with an inappropriate title and abstract (1,619) were excluded. Thereafter, the remaining 283 studies were read and selected within which 275 items were excluded. Finally, 8 studies were included and submitted for the meta-analysis (Figure 2). The characteristics of the included studies are listed in Table 1.
Figure 2.
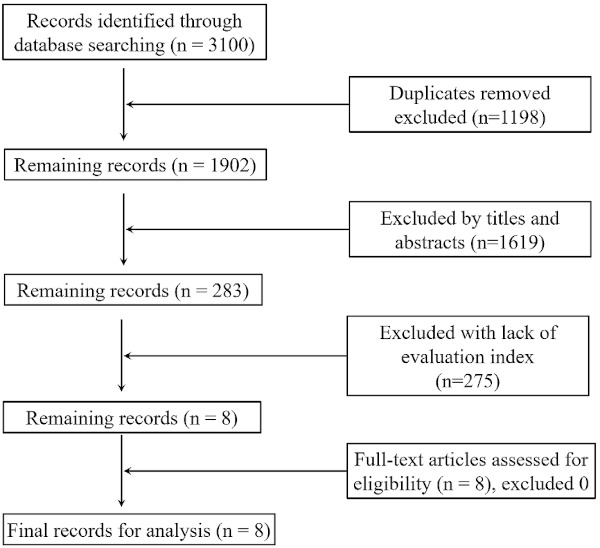
Flow chart of the searching strategy and selection of literature reports.
Table 1. Characteristics of the included studies.
| Included Trials | Study Design | Sample size | Average age (ȳ) | Gender (M/F) | Level | Implants |
|---|---|---|---|---|---|---|
| Park et al. 2008 | R | ACDA: 21 | 45 | 11/10 | 1 | Mobi-C |
| ACDFWP: 32 | 47 | 20/12 | Solis | |||
| Vorsic et al. 2010 | P | ACDA: 40 | 48.1 | 13/27 | 1/2 | ProDisc-C |
| ACDFWP: 40 | 51.3 | 12/28 | ChronOS | |||
| Park et al. 2012 | R | ACDA: 22 | 39.9 | 19/3 | 1 | ProDisc-C |
| ACDFWP: 21 | 44.3 | 11/10 | Solis | |||
| Qizhi et al. 2016 | RCT | ACDA: 14 | 46.79 | 9/5 | 2 | Discover |
| ACDFWP: 16 | 48.13 | 11/5 | Zore-P | |||
| Shi et al. 2016a | R | ACDA: 60 | 46.5 | 24/36 | 1 | Discover |
| ACDFWP: 68 | 47.4 | 33/35 | Zore-P | |||
| Shi et al. 2016b | P | ACDA: 55 | 48.9 ± 7.0 | 30/25 | 1 | Discover |
| ACDFWP: 57 | 50.6 ± 7.2 | 37/20 | Zore-P | |||
| Donk et al. 2017a | RCT | ACDA: 50 | 44.1 ± 6.4 | 24/26 | 1 | Bryan |
| ACDFWP: 47 | 43.1 ± 7.5 | 25/22 | Brantigan | |||
| Donk et al. 2017b | RCT | ACDA: 50 | 53.6 ± 6.9 | 24/26 | 1 | Bryan |
| ACDFWP: 47 | 52.2 ± 8.1 | 25/22 | Brantigan |
ACDA: anterior cervical disc arthroplasty; ACDFWP: anterior cervical discectomy and fusion without plate; R: Retrospective; P: Prospective; RCT: Randomized controlled study.
3.2. Assessments of the study quality
Figure 3 shows the results of the assessments of study quality using a RoB tool (for RCTs) and a ROBINS-I tool (for nRCTs). Overall, three RCTs had low RoB. Only one study (Qizhi et al. 2016) had a high risk of blinding, and one study a had high risk of other bias (Donk et al. 2017b). The study quality of the included RCTs was satisfactory (Figure 3A). However, the study quality of the included nRCTs was weaker. The study by Park et al. 2008 had a serious RoB and that by Vorsic et al. 2010 had a critical RoB. Confounding bias was involved in 2 studies (14,15). One study had missing data (14). Overall, two studies were of low quality (14,15), and other 3 studies were identified as having moderate study quality (Figure 3B). We could not evaluate the publication bias because only 3 RCTs and 5 nRCTs were included in this study.
Figure 3.
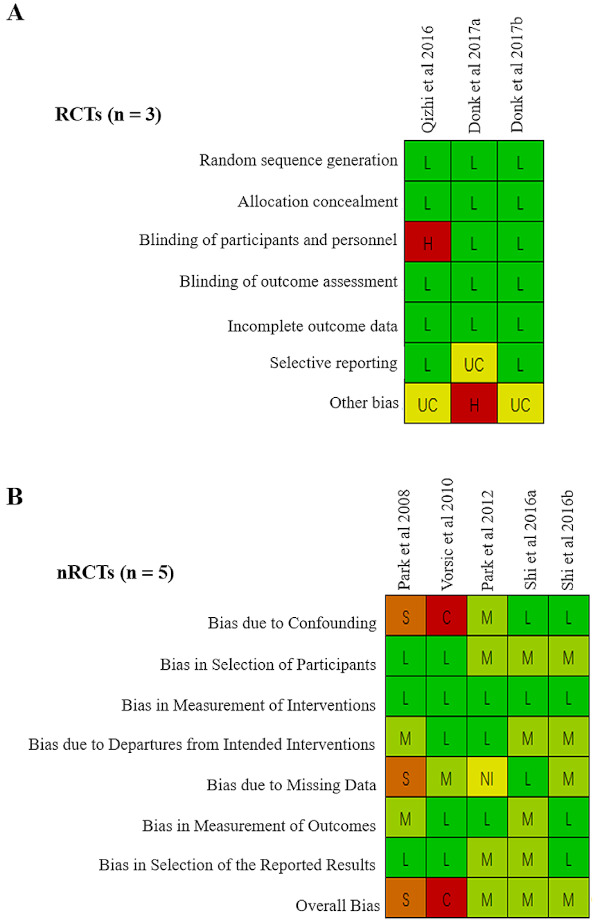
Quality assessment of the involved literatures with a RoB tool for RCTs (A) and a ROBINS-I tool for nRCTs (B). L = Low, UC = Unclear, H = High, M = Moderate, S = Serious, C = Critical, NI = No information.
3.3. Assessments of the postoperative clinical efficacy achieved with the ACDFWP and ACDA.
Figure 3 shows the results of the assessments of study quality using a RoB tool (for RCTs) and a ROBINS-I tool (for nRCTs). Overall, three RCTs had low RoB. Only one study (Qizhi et al. 2016) had a high risk of blinding, and one study a had high risk of other bias (Donk et al. 2017b). The study quality of the included RCTs was satisfactory (Figure 3A). However, the study quality of the included nRCTs was weaker. The study by Park et al. 2008 had a serious RoB and that by Vorsic et al. 2010 had a critical RoB. Confounding bias was involved in 2 studies (14,15). One study had missing data (14). Overall, two studies were of low quality (14,15), and other 3 studies were identified as having moderate study quality (Figure 3B). We could not evaluate the publication bias because only 3 RCTs and 5 nRCTs were included in this study.
3.3.1. NDI
From among the studies that have reported postoperative NDI scores, one study (14) was excluded owing to lack of data on standard deviation of NDI. The remaining five studies (15-19) reported the postoperative NDI for 378 patients. No significant difference was observed in the NDI scores of the ACDFWP and ACDA (MD = 0.15, 95% CI [−0.21, 0.51], P = 0.40, I2 = 0%) (Figure 4A).
Figure 4.
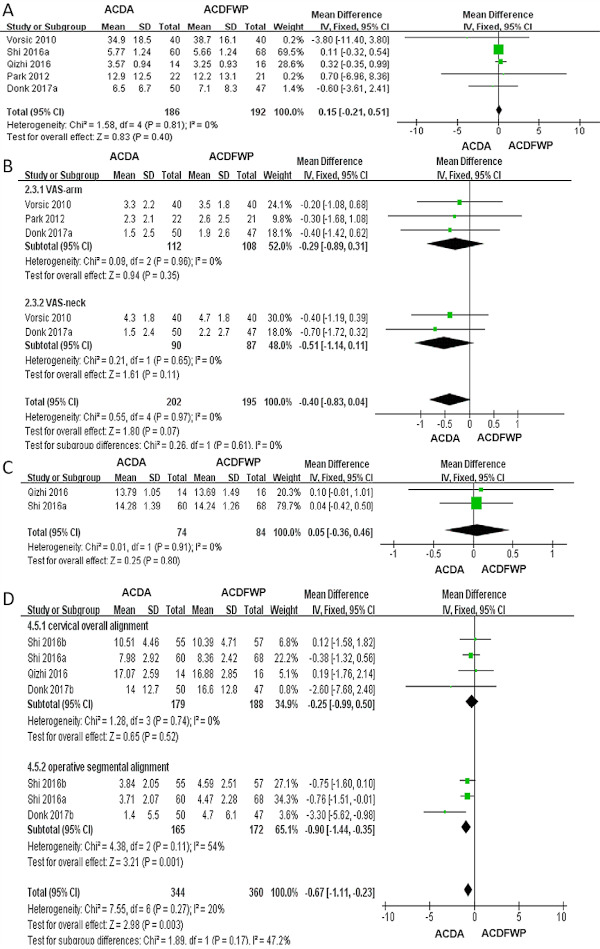
Meta-analysis for the clinical assessments of ACDA and ACDFWP. A. Forest plot for the scores of NDI. B. Forest plot for the scores of VAS. C. Forest plot for the scores of JOA. D. Forest plot for the scores of cervical alignment.
3.3.2. VAS
Four studies (14-16,19) reported the postoperative VAS scores, within one study (14) was withdrawn for analysis because they did not report the standard deviation. The remaining three studies suggested non-significant differences in the VAS scores of the two groups (MD = −0.40, 95% CI [−0.83, 0.04], P = 0.07, I2 = 0%). We also introduced subgroups analysis and found no difference between the subgroups (Figure 4B).
3.3.3. JOA
Two studies reported the postoperative JOA scores (17,18), with 158 patients being enrolled. The pooled analysis showed no significant difference in the postoperative JOA scores of the ACDFWP and ACDA (MD = 0.05, 95% CI [−0.36, 0.46], P = 0.80, I2 = 0%) (Figure 4C).
3.3.4. Cervical alignment
Six studies (14,16-18,20,21) reported the cervical alignment, while two (14,16) were excluded because they did not report the standard deviation. We conducted subgroups analyses to decrease the potential heterogeneity, and no significant differences were observed between the subgroups. Overall, the remaining four studies indicated that the cervical alignment was better in the ACDFWP (vs. ACDA, MD = −0.67, 95% CI [−1.11, −0.23], P = 0.003, I2 = 20%) (Figure 4D).
The assessment of postoperative clinical efficacy showed that the ACDFWP exhibited better efficacy only in the cervical alignment. No other significant difference was found in the other 3 indices.
3.4. Assessments of other clinical factors
3.4.1. Operation time
Four studies reported the operation time; two studies (14,16) were excluded owing to lack of data on standard deviation. Analysis of the remaining two studies (18,20) that included 240 patients found no difference between the ACDFWP and ACDA (MD = −3.11, 95% CI (−11.44, 5.22), P = 0.46, I2 = 93%) (Figure 5A).
Figure 5.
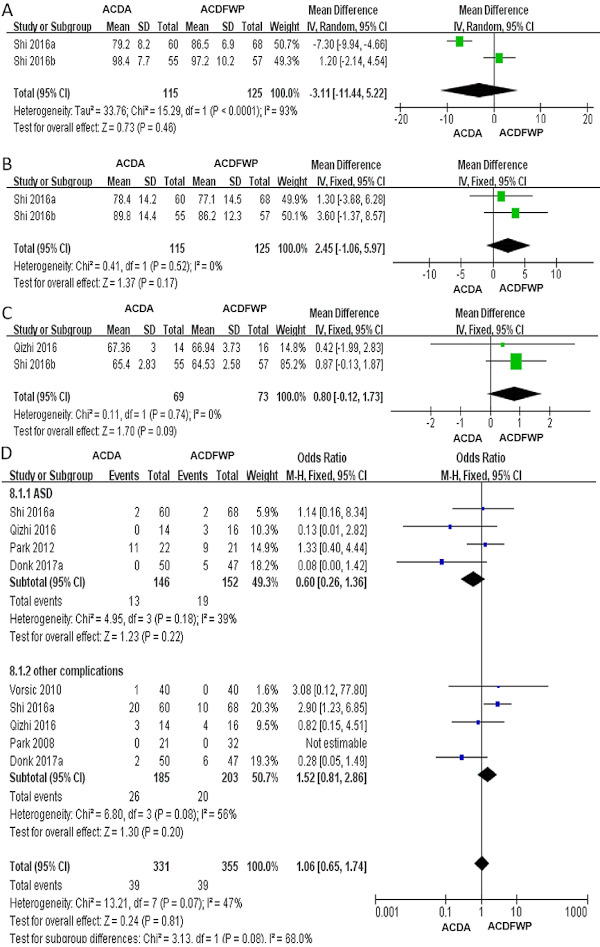
Meta-analyses of the other outcome indices of ACDA and ACDFWP. A. Forest plot for the operative time. B. Forest plot for the scores of blood loss. C. Forest plot for the scores of SWAL-QL. D. Forest plot for the scores of complications.
3.4.2. Blood loss
Two studies reported blood loss (18,20). Total 240 patients were enrolled. However, no significant difference was identified between the ACDFWP and ACDA (MD = 2.45, 95% CI [−1.06, 5.97], P = 0.17, I2 = 0%) (Figure 5B).
3.4.3. Swallowing Quality of Life Score
SWAL-QL was reported in two studies (17,20) that involved 142 patients enrolled. No significant difference was found in the SWAL-QL of the two groups (MD = 0.80, 95% CI [−0.12, 1.73], P = 0.09, I2 = 0%) (Figure 5C).
3.4.4. Complications
Complications were reported in 6 studies (14-19) that involved 431 patients enrolled. No significant difference was observed in the complications between the two groups (MD = 1.06, 95% CI [0.65, 1.74], P = 0.81, I2 = 47%) (Figure 5D). Particularly, with regard to the frequency of occurrence of ASD, there were 19 cases in the ACDFWP and 13 cases in the ACDA, no significant difference was found between two groups (Z =1.23, P = 0.22) (Figure 5D).
No significant difference was found in the other clinical-related indices.
4. Discussion
The present study compared the efficacy and other factors associated with the clinical outcome of ACDFWP and ACDA. To our knowledge, this is the first meta-analysis to compare these two alternative surgeries. We found that the ACDFWP seems had better efficacy in terms of cervical alignment than that ACDA. No significant difference was found in the other indices. Our results suggest a slight superiority of ACDFWP. These findings might contribute to the selection of surgery type in patients with cervical spondylosis. However, the relatively small number of included studies lowered the evidence level.
In the present study, 8 studies (3 RCTs and 5 nRCTs, 640 patients enrolled) were evaluated. Although 3 RCTs were included, the quality of the included RCTs were satisfactory, and the quality of the included nRCTs was moderate (Figure 3). Evidence-based comparison of the studies has limited worthiness.
With respect to the comparisons of clinical efficacy, the indices of NDI (MD = 0.15, 95% CI [−0.21, 0.51], P = 0.40, I2 = 0%), VAS (MD = −0.40, 95% CI [−0.83, 0.04], P = 0.07, I2 = 0%), and JOA (MD = 0.05, 95% CI [−0.36, 0.46], P = 0.80, I2 = 0%) showed the same tendency. The homogeneity of the involved studies was high. We did not find any difference between the two surgeries. However, the results of the cervical alignment (MD = −0.67, 95% CI [−1.11, −0.23], P = 0.003, I2 = 20%) indicated better efficacy of ACDFWP (Figure 4). Under the support of cage, ACDF could achieve good operative alignment recovery.
With regard to the indices of other factors, we found no difference between the operation time [MD = −3.11, 95% CI (−11.44, 5.22), P = 0.46, I2 = 93%], blood loss [MD = 2.45, 95% CI (−1.06, 5.97), P = 0.17, I2 = 0%], SWAL-QL [MD = 0.80, 95% CI (−0.12, 1.73), P = 0.09, I2 = 0%], and complications [MD = 1.06, 95% CI (0.65, 1.74), P = 0.81, I2 = 47%]. There was no difference in the operation time and blood loss, postoperative QOL, and complications. ASD is the most important complication that must be considered while selecting the surgery. The aim of developing these alternative surgeries was to reduce the risk of complications, particularly, the onset of ASD because placing the anterior plate during the conventional ACDF is risky (22,23). It was reported that the incidence of ASD in ACDFWP was significantly lower than that in conventional ACDF (24). ACDA is another alternative surgery that is believed to lower the incidence of ASD onset. Previous evidence shows that ACDA contributes to maintain the motion at the involved segments and had a lower reoperation rate than those in conventional ACDF (1,25-27); a current study proved the long-term efficacy of ACDA in reducing the risk of ASD (9). However, our study found no difference between the ACDFWP and ACDA (X2 = 4.95, P = 0.18, I2 = 39%) (Figure 5).
However, conventional ACDF (with plate), alternative ACDFWP, and ACDA, all the existing surgeries have their specific advantages and disadvantages. i) Conventional ACDF vs. alternative ACDF: Although alternative ACDF achieved low onset of ASD, the conventional ACDF (with plate), as the gold standard therapy for cervical spondylosis, also has its merits. Current two studies indicated that conventional ACDF is good for ensuring greater restoration of alignment in the operative segment (21,28). A long-term follow-up study found that the operative segmental alignment gradually decreased, and the overall alignment increased with time (21). ii) Convention ACDF vs. ACDA: In addition to the low risk of ASD, ACDA has good efficacy. According to the results of several meta-analyses (29,30), the efficacy and safety of ACDA were superior to those of conventional ACDF. After a long-term follow-up, Ma et al. reported that ACDA was superior to conventional ACDF in terms of VAS and the overall success rate (30). Zhao et al. found that ACDA achieved a higher SF-36, a larger range of movement, a higher rate of neurological improvement, a lower VAS, a lower NDI, and a lower reoperation rate than conventional ACDF (29). Other studies have also indicated that ACDA was slightly better than the conventional ACDF in terms of the VAS score (15,16,19) and SWAL-QL (17,20). However, ACDA also has its disadvantages. Tian et al. reported that ACDA might contribute to promote the progression of heterotopic ossification, especially for patients who had been preoperatively developed (31). Latka et al. reported that ACDA involved a longer operation time and more blood loss than the conventional ACDF. A longer traction on the structures of the soft neck is a major disadvantage of ACDA (9). iii) Alternative ACDF vs. ACDA (the present study): We found that only the alternative ACDF exhibited a slight benefit in the cervical alignment as compared to ACDA. No significant difference was found in the other indices between alternative ACDF and ACDA. In sum, both the conventional and alternative surgeries have their strengths and weaknesses. Based on the evidence available today, they cannot replace each other. The appropriate surgery should be seriously selected according to the individual pathophysiological state of each patient.
There are certain limitations of this study, as follows: i) The small number of included studies; only 3 RCTs were included; only studies published in English were included. Two studies by the same authors were included, namely Shi 2016a (20) and Shi 2016b (18), and Donk 2017a (19) and Donk 2017b (21). Although we have investigated the studies and excluded the possibility of overlap of patients, but the data sources were too narrow, which lowered the reliability of the evidence. ii) The study quality of some the included studies was low. iii) The heterogeneity of some items (operation time, complications) was high, lowering the level of evidence. iv) Long-term observation was not performed in all included literatures, which is required on the study of ASD. More rigorous studies with long-term follow-up are expected to compare the alternative ACDF and ACDA, particularly for the onset of ASD.
5. Conclusions
In this study, we compared the clinical outcomes between the alternative ACDFWP and ACDA. We found that the ACDFWP exhibited slightly better cervical alignment than ACDA. No significant difference was found in the other items, including NDI, VAS, JOA, operation time, blood loss, SWAL-QL, and complications. These findings may contribute to the selection of the appropriate surgery for patients with cervical spondylosis. However, limited studies exist; thus, the evidence level is low. Larger, better-planned studies are required in the future.
Funding: This work was supported by Fujian Natural Science Foundation (2016J01560), grant from the Youth Program of the Health Commission of Fujian Province (2016-ZQN-73).
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- 1. Loumeau TP, Darden BV, Kesman TJ, Odum SM, Van Doren BA, Laxer EB, Murrey DB. A RCT comparing 7-year clinical outcomes of one level symptomatic cervical disc disease (SCDD) following ProDisc-C total disc arthroplasty (TDA) versus anterior cervical discectomy and fusion (ACDF). Eur Spine J. 2016; 25:2263-2270. [DOI] [PubMed] [Google Scholar]
- 2. Nanda A, Sharma M, Sonig A, Ambekar S, Bollam P. Surgical complications of anterior cervical diskectomy and fusion for cervical degenerative disk disease: a single surgeon's experience of 1,576 patients. World Neurosurg. 2014; 82:1380-1387. [DOI] [PubMed] [Google Scholar]
- 3. Laxer EB, Brigham CD, Darden BV, Bradley Segebarth P, Alden Milam R, Rhyne AL, Odum SM, Spector LR. Adjacent segment degeneration following ProDisc-C total disc replacement (TDR) and anterior cervical discectomy and fusion (ACDF): does surgeon bias effect radiographic interpretation? Eur Spine J. 2017; 26:1199-1204. [DOI] [PubMed] [Google Scholar]
- 4. Hofstetter CP, Kesavabhotla K, Boockvar JA. Zero-profile Anchored Spacer Reduces Rate of Dysphagia Compared With ACDF With Anterior Plating. J Spinal Disord Tech. 2015; 28:E284-290. [DOI] [PubMed] [Google Scholar]
- 5. Kepler CK, Hilibrand AS. Management of adjacent segment disease after cervical spinal fusion. Orthop Clin North Am. 2012; 43:53-62, viii. [DOI] [PubMed] [Google Scholar]
- 6. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999; 81:519-528. [DOI] [PubMed] [Google Scholar]
- 7. Helgeson MD, Bevevino AJ, Hilibrand AS. Update on the evidence for adjacent segment degeneration and disease. Spine J. 2013; 13:342-351. [DOI] [PubMed] [Google Scholar]
- 8. Cheung ZB, Gidumal S, White S, Shin J, Phan K, Osman N, Bronheim R, Vargas L, Kim JS, Cho SK. Comparison of Anterior Cervical Discectomy and Fusion With a Stand- Alone Interbody Cage Versus a Conventional Cage-Plate Technique: A Systematic Review and Meta-Analysis. Global Spine J. 2019; 9:446-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Latka D, Kozlowska K, Miekisiak G, Latka K, Chowaniec J, Olbrycht T, Latka M. Safety and efficacy of cervical disc arthroplasty in preventing the adjacent segment disease: a meta-analysis of mid- to long-term outcomes in prospective, randomized, controlled multicenter studies. Ther Clin Risk Manag. 2019; 15:531-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maharaj MM, Mobbs RJ, Hogan J, Zhao DF, Rao PJ, Phan K. Anterior cervical disc arthroplasty (ACDA) versus anterior cervical discectomy and fusion (ACDF): a systematic review and meta-analysis. J Spine Surg. 2015; 1:72-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009; 339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sterne JA, Hernan MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016; 355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods G, Cochrane Statistical Methods G. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Park JH, Roh KH, Cho JY, Ra YS, Rhim SC, Noh SW. Comparative analysis of cervical arthroplasty using Mobi-c® and anterior cervical discectomy and fusion using the Solis® -cage. J Korean Neurosurg Soc. 2008; 44:217‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vorsic M, Bunc G. ProDisc-C versus fusion with Cervios chronOS prosthesis in cervical degenerative disc disease: Is there a difference at 12 months? Evid Based Spine Care J. 2010; 1:51-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Park JY, Kim KH, Kuh SU, Chin DK, Kim KS, Cho YE. What are the associative factors of adjacent segment degeneration after anterior cervical spine surgery? Comparative study between anterior cervical fusion and arthroplasty with 5-year follow-up MRI and CT. Eur Spine J. 2012; 22:1078-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Qizhi S, Lei S, Peijia L, Hanping Z, Hongwei H, Junsheng C, Jianmin L. A Comparison of Zero-Profile Devices and Artificial Cervical Disks in Patients With 2 Noncontiguous Levels of Cervical Spondylosis. Clin Spine Surg. 2016; 29:E61-66. [DOI] [PubMed] [Google Scholar]
- 18. Shi S, Zheng S, Li XF, Yang LL, Liu ZD, Yuan W. Comparison of 2 Zero-Profile Implants in the Treatment of Single-Level Cervical Spondylotic Myelopathy: A Preliminary Clinical Study of Cervical Disc Arthroplasty versus Fusion. PloS One. 2016; 11:e0159761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Donk R, Verbeek A, Verhagen W, Groenewoud H, Hosman A, Bartels R. What's the best surgical treatment for patients with cervical radiculopathy due to single-level degenerative disease? A randomized controlled trial. PloS One. 2017; 12:e0183603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shi S, Li XF, Zhao QT, Yang LL, Liu ZD, Yuan W. Risk Factors for Dysphagia After Single-Level Anterior Cervical Decompression with Arthroplasty or Fusion: A Prospective Study Comparing 2 Zero-Profile Implants. World Neurosurg. 2016b; 95:148-155. [DOI] [PubMed] [Google Scholar]
- 21. Donk RD, Arnts H, Verhagen WIM, Groenewoud H, Verbeek A, Bartels RHMA. Cervical sagittal alignment after different anterior discectomy procedures for single-level cervical degenerative disc disease: randomized controlled trial. Acta Neurochir (Wien). 2017; 159:2359-2365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Burkhardt BW, Simgen A, Wagenpfeil G, Reith W, Oertel JM. Adjacent Segment Degeneration After Anterior Cervical Discectomy and Fusion With an Autologous Iliac Crest Graft: A Magnetic Resonance Imaging Study of 59 Patients With a Mean Follow-up of 27 Years. Neurosurgery. 2018; 82:799-807. [DOI] [PubMed] [Google Scholar]
- 23. Alhashash M, Shousha M, Boehm H. Adjacent Segment Disease After Cervical Spine Fusion Evaluation of a 70 Patient Long-Term Follow-Up. Spine. 2018; 43:605-609. [DOI] [PubMed] [Google Scholar]
- 24. Lu Y, Bao W, Wang Z, Zhou F, Zou J, Jiang W, Yang H, Zhang Z, Zhu X. Comparison of the clinical effects of zero-profile anchored spacer (ROI-C) and conventional cage-plate construct for the treatment of noncontiguous bilevel of cervical degenerative disc disease (CDDD): A minimum 2-year follow-up. Medicine (Baltimore). 2018; 97:e9808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pisano A, Helgeson M. Cervical disc replacement surgery: biomechanical properties, postoperative motion, and postoperative activity levels. Curr Rev Musculoskelet Med. 2017; 10:177-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hisey MS, Bae HW, Davis RJ, Gaede S, Hoffman G, Kim KD, Nunley PD, Peterson D, Rashbaum RF, Stokes J, Ohnmeiss DD. Prospective, Randomized Comparison of Cervical Total Disk Replacement Versus Anterior Cervical Fusion: Results at 48 Months Follow-up. J Spinal Disord Tech. 2015; 28:E237-243. [DOI] [PubMed] [Google Scholar]
- 27. Yang X, Janssen T, Arts MP, Peul WC, Vleggeert- Lankamp CLA. Radiological follow-up after implanting cervical disc prosthesis in anterior discectomy: a systematic review. Spine J. 2018. [DOI] [PubMed] [Google Scholar]
- 28. Di Martino A, Papalia R, Albo E, Cortesi L, Denaro L, Denaro V. Cervical spine alignment in disc arthroplasty: should we change our perspective? Eur Spine J. 2015; 24 Suppl 7:810-825. [DOI] [PubMed] [Google Scholar]
- 29. Zhao GS, Zhang Q, Quan ZX. Mid-term efficacy and safety of cervical disc arthroplasty versus fusion in cervical spondylosis: A systematic review and meta-analysis. Biomed Rep. 2017; 6:159-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ma Z, Ma X, Yang HL, Guan XM, Li X. Anterior cervical discectomy and fusion versus cervical arthroplasty for the management of cervical spondylosis: A meta-analysis. Eur Spine J. 2017; 26:998-1008. [DOI] [PubMed] [Google Scholar]
- 31. Tian W, Han X, Liu B, He D, Lv Y, Yue J. Generation and Development of Paravertebral Ossification in Cervical Artificial Disk Replacement. Clin Spine Surg. 2017; 30:E179-E188. [DOI] [PubMed] [Google Scholar]


