Abstract
Objective: To investigate the effect of standardized quality control management on the rehabilitation of children with palsy in Ningbo City. Methods: In this retrospective study, a total of 400 pediatric patients requiring rehabilitation therapy admitted to Ningbo Rehabilitation Hospital from July 2017 to May 2021, were selected as the research subjects. Pediatric patients were divided into an observation group (standardized model) and a control group (routine model) based on the different quality management models. The rehabilitation efficacy, nursing quality, negative emotion, satisfaction, DQ scores, ADL scores, PDI scores, MDI scores, compliance rate, complaint rate of nursing, and incidence of adverse events were compared between the two groups. Results: The rehabilitation efficacy in the observation group was better than that in the control group (P<0.05). Compared to the control group, the nursing quality score and satisfaction rate were higher, and the negative emotion score was lower in the observation group (all P<0.05). DQ scores, ADL scores, PDI scores, and MDI scores in the observation group were higher than the control group (all P<0.05). The statistical differences were observed in the compliance rate, complaint rate in nursing, and incidence of adverse events between the two groups (all P<0.05). Conclusions: The standardized quality control management enhanced the rehabilitation efficacy, promoted the nursing quality, improved the clinical effects, increased the satisfaction rate, and decreased the negative emotions in pediatric patients.
Keywords: Quality control management, standardized model, pediatric rehabilitation, nursing quality, clinical effects
Introduction
Pediatric cerebral palsy is considered the most common movement disorder in children worldwide. An epidemiological survey showed that the incidence of pediatric cerebral palsy was 0.25%. It was 1.47% among the intellectually disabled children aged from 0 to 14 years old [1-3]. It was reported that the number of intellectually disabled children at home was more than six hundred thousand [4]. There was an increased trend on the demands of rehabilitation for these pediatric patients. Failure to address the rehabilitation needs of these children can have long-term consequences on their recovery. Pediatric rehabilitation medicine, as the intersection of rehabilitation medicine and pediatrics, has gradually become important in the hospital in recent years [1,5]. The proper management of a pediatric rehabilitation ward helps to improve the physical function of pediatric patients and promote their growth and development. It plays an important role in the recovery of chronic diseases.
Domestic pediatric rehabilitation medicine has made great progress regardless of the late start, weak academic foundation, and lack of quality control standards. A large gap remains for the level of basic and clinical research compared with developed countries and the needs of society [6]. Compared to adult rehabilitation, pediatric rehabilitation has its differences, a larger workload, and a higher difficulty of rehabilitation care [7]. At the end of 2019, there were 2,303 disabled children under the age of 14 years old in Ningbo city. The surveys of Ningbo city regarding child rehabilitation showed that the quality of rehabilitation institution, the qualifications of practitioners and the levels of diagnosis, and treatment varied greatly. All of these caused poor quality control management for pediatric rehabilitation. It is urgent to formulate unified quality control management guidelines to regulate child rehabilitation.
By using relevant research and normative standards at home and abroad in recent years, and taking Ningbo Children’s Rehabilitation Hospital as a reference unit, we enrolled 400 pediatric patients into this study. We aimed to investigate the performance of standardized quality control management in the rehabilitation of pediatric patients and its influences on rehabilitation effects and nursing quality. The results of this study would guide the quality management of clinical pediatric rehabilitation medicine and related medical behaviors.
Materials and methods
General information
In this retrospective study, 400 pediatric patients from The Child Rehabilitation Division in Ningbo Rehabilitation Hospital, from July 2017 to May 2021, were enrolled and divided into two groups based on the different methods of rehabilitation quality control and management.
Inclusion criteria: Patients with an age of 1-14 years old; Patients who met the diagnostic criteria of pediatric cerebral palsy [8]; and Patients’ guardians who signed the informed consent.
Exclusion criteria: Pediatric patients with severe liver and kidney dysfunction; Pediatric patients with cardiovascular diseases; Pediatric patients who suffered from blindness and deafness. Pediatric patients complicated with limb dysfunction; Pediatric patients with brain tumor diseases; or Pediatric patients with incomplete medical records.
For the control group, 200 pediatric patients received routine quality control management. For the observation group, 200 pediatric patients were treated with standardized quality control management. This study was approved by the Ethics Committee of Ningbo Rehabilitation Hospital (Approval No. 2017-078).
Methods
Control group
Before starting rehabilitation, the basic conditions of pediatric patients were carefully evaluated, and the health promotion and education was implemented. Attention was paid to the supervision of daily basic nursing to prevent complications and adverse reactions.
Observation group
The details were as follows: ① A quality control management working group was established. The group was composed of the principal responsible person of the rehabilitation department, doctors, the head nurse, and nurses. The group leader was the major principal. ② The responsibility of team members was assigned. The nurses were responsible for the admission of pediatric patients, the health promotion, and education. The doctor was responsible for the data collection, evaluations of basic conditions, case writing, examination application forms, and the composition of the rehabilitation team for the pediatric patients. The doctors developed a rehabilitation treatment plan within one week, organized monthly mid-term evaluation meetings and final evaluation meetings before discharge, and formulated a family rehabilitation plan for the patients. The evaluation of the rehabilitation treatment plan, the evaluation of various assessment meeting’s performance, and the adjustment of the plan were conducted by the group leader. The head nurse was responsible for completing the satisfaction survey and organizing these data within one month following the discharge. ③ A rehabilitation team was established. The rehabilitation team consisted of the main person in charge of the rehabilitation department, the attending physicians, the head nurse, the relevant therapists, and parents or guardians. ④ The workflow of standardized quality control management was performed. (1) Regarding hospital admission, health promotion, and education, the experienced head nurse was responsible for the reception in a kind and friendly manner to eliminate worries of the children and their families. Various health education forms, such as brochures and explanation, were implemented to allow the guardians to have a general understanding of the disease and rehabilitation course. (2) Concerning pre-habitation preparation, the doctors inquired the past medical history of pediatric patients at their admission, organized a physical examination, collected the general information, evaluated and recorded the basic conditions of the children, and wrote the cases related to their conditions. Auxiliary inspections were carried out and corresponding inspection sheets were issued and signed. Within one week of admission, the physician in charge was able to formulate a personalized rehabilitation treatment plan based on the general information and examination results and reported it to the group leader to organize a meeting for evaluation and adjustment. (3) Regarding the establishment of a rehabilitation team, a doctor in charge organized a rehabilitation team. This team was composed of both the hospital staff and family members of the pediatric patients. The hospital staff included the main person in charge of the rehabilitation department, the doctor in charge, and the head nurse. Family members of pediatric patients included the parents or guardians of the children. After formulating the family rehabilitation plan, the attending physician communicated with the family members about the specific contents and precautions, and informed them that they could ask for the guidance of the medical staff as necessary. The rehabilitation treatment plan included basic and long-term rehabilitation training. This training was composed of limb movement training, infant touch training, and training with audio-visual stimulation. Motor function training included training of fine motor, turning over in bed, crawling, sitting, walking, toileting, and eating. The rehabilitation team provided the pediatric patients with the intelligence training. The team communicated with these patients using language, facial expression, and physical expression. This imparted perceptual knowledge, improved their cognition, and enhanced the patients’ intelligence. (4) Concerning evaluation, including initial evaluation, mid-term evaluation, and final evaluation before discharge, all evaluation meetings were organized by the attending physician and supported by the group leader. The initial evaluation referred to the first evaluation following the establishment of the rehabilitation treatment plan. After the discussion in the rehabilitation quality control group, the inappropriate parts were revised to make it more suitable for the individuals. The objectives of rehabilitation work were established at the initial evaluation meeting. A mid-term evaluation meeting was organized in the middle of each month. At the meeting, the group leader summarized the implementation of the plan in the previous stage, adjusted the details and goals of the plan to focus on the specific rehabilitation situation of each pediatric patient, and evaluated the outcome of the previous stage. A final assessment was performed before discharge. At the meeting, the group leader apprised the outcome of previous stages, and a community or family rehabilitation plan for the pediatric patients was discussed and evaluated. (5) In terms of the satisfaction survey, the head nurse completed the satisfaction survey within a month after leaving the hospital, establishing a monthly report of the satisfaction survey, and included it in the team assessment. (6) In terms of regular follow-up after discharge, the attending physician conducted the regular telephone follow-up or the outpatient management.
Observation indicators
The rehabilitation efficacy was compared between the two groups. Regarding the clinical manifestations of pediatric patients, the rehabilitation efficacy was divided into three grades: excellent effectiveness, effectiveness, and ineffectiveness. Excellent effectiveness indicated that the physiological functions were close to those of typical children of the same age. The effectiveness suggested that physiological functions were improved, but they were inferior to those of typical children of the same age. Ineffectiveness was considered that the physiological functions did not meet the above standards. The formula for total effective rate was as follows: Total effective rate = Number of (excellent effective cases+ effective cases)/Total number of pediatric patients ×100%.
The quality assessment for nursing care was about the quality control group in the hospital, including communication efficiency, service attitude, disease observation, problem finding, formulation of rehabilitation plan, and nursing procedures. Each item scored from 1 to 10. Higher scores indicated better results.
The negative emotion from family members of pediatric patients was compared between the two groups. The negative emotion was assessed by Hamilton Depression Rating Scale (HAMD) scores and Hamilton Anxiety Scale (HAM-A) scores [9]. High scores indicated poor negative emotion.
The assessment of satisfaction for the rehabilitation department was subjectively made according to the environment, rehabilitation management, nursing professionality, working attitudes, and rehabilitation effects [10]. The satisfaction questionnaire was established by the quality control group. The survey was performed by the head nurse. It was composed of a satisfaction questionnaire of pediatric patients and satisfaction questionnaire of family members with a total score of 100. More than 80 indicated satisfaction.
Scores of developmental quotients (DQ) and Activities of Daily Living (ADL) scores were compared between the two groups. The DQ in both groups were evaluated by Gesell Developmental Schedules that included adaptive behavior, gross motor, fine motor, language, and personal-social behavior [11]. It was calculated as follows: Developmental quotient (DQ) = development age/chronological age*100. The ADL scale was applied to assess the children’s daily living ability. It included nine items, such as eating, dressing, undressing, toileting, and walking [12]. Each item was calculated according to the completion rate, representing “dependence” (0 point), “moderate difficulty” (1 point), “slight difficulty” (2 points), and “independence” (3 points), with a maximum score of 27 points. Higher scores indicated better daily living ability of the children.
The scores of psychomotor development index (PDI) and mental developmental index (MDI) were compared between the two groups. The Bayley Scales of Infant Development were applied to measure the PDI and MDI scores [13]. The Motor Scale of the Bayley Scales of Infant Development included 81 items such as laying prone head up, standing, sitting, turning over, walking, and running, with separate assessments of gross motor and fine motor ability. The Mental Scale of the Bayley Scales of Infant Development was performed to assess the sensorimotor ability. Chichi was composed of 163 items such as discriminating shapes, building blocks, and placing shaped boards. The maximum score was 100 points. The highest score indicated better motor and intelligence function.
The compliance rate of pediatric patients, complaint rate of nursing, and incidence of adverse events were recorded and compared between the two groups.
Statistical analysis
The data included in this study were analyzed using SPSS statistical software version 22.0 (IBM, USA). The graphic software exploited in this study was GraphPad Prism version 8.0 (GraphPad Software, Inc., La Jolla, CA, USA). The measured data were expressed as Mean ± Standard Deviation (SD). The T test was used for comparison between the two groups. The enumeration data were expressed as number/percentage (n/%). The Chi-square test was conducted for the comparison between the two groups. P<0.05 indicated the statistical difference.
Results
Comparison of general information
As shown in Table 1, there were no obvious statistical differences in age, gender, body weight, course of disease, and types of disease between the two groups (all P>0.05).
Table 1.
Comparison of basic information between the two groups
| Group | Control group (n=200) | Observation group (n=200) | t/χ2 value | P value |
|---|---|---|---|---|
| Age (years) | 8.36±3.80 | 8.32±3.55 | 0.109 | 0.913 |
| Gender (n) | 0.648 | 0.421 | ||
| Male | 107 | 115 | ||
| Female | 93 | 85 | ||
| Course of disease (years) | 4.6±1.2 | 4.4±1.0 | 1.811 | 0.071 |
| Body weight (kg) | 13.4±1.5 | 13.2±1.2 | 1.472 | 0.142 |
| Types of disease | 1.125 | 0.570 | ||
| Spastic form (n) | 71 | 75 | ||
| Dyskinesia (n) | 79 | 69 | ||
| Mix (n) | 50 | 56 |
Comparison of the rehabilitation efficacy
As seen in Table 2, there were 24 cases with excellent effectiveness, 121 cases with effectiveness, and 55 cases with ineffectiveness in the control group. There were 31 cases with excellent effectiveness, 160 cases with effectiveness, and 9 cases with ineffectiveness in the observation group. The total effective rate in the observation group was higher than that in the control group (P<0.05).
Table 2.
Comparison of the rehabilitation efficacy between the two groups
| Group | Excellent effectiveness | Effectiveness | Ineffectiveness | Total effective rate |
|---|---|---|---|---|
| Control group | 24 | 121 | 55 | 72.50% |
| Observation group | 31 | 160 | 9 | 95.50% |
| χ2 value | 5.148 | |||
| P value | 0.031 |
Comparison of the scores for nursing quality
In the observation group, the scores for communication efficiency, service attitude, disease observation, problem finding, formulation of rehabilitation plan, and nursing procedures were 8.27±0.68, 9.33±0.75, 8.26±0.78, 8.64±0.67, 9.01±0.62, and 8.26±0.68, respectively. Those in the control group were 7.35±0.67, 8.24±0.81, 7.43±0.69, 7.57±0.71, 7.82±0.59, and 7.39±0.66, respectively (all P<0.05), as seen in Table 3.
Table 3.
Comparison of the scores for nursing quality between the two groups (Scores)
| Groups | Communication efficiency | Service attitude | Disease observation | Problem finding | Formulation of rehabilitation plan | Nursing procedures |
|---|---|---|---|---|---|---|
| Observation group (n=200) | 8.27±0.68 | 9.33±0.75 | 8.26±0.78 | 8.64±0.67 | 9.01±0.62 | 8.26±0.68 |
| Control group (n=200) | 7.35±0.67 | 8.24±0.81 | 7.43±0.69 | 7.57±0.71 | 7.82±0.59 | 7.39±0.66 |
| t value | 13.629 | 13.964 | 11.271 | 15.501 | 19.663 | 12.984 |
| P value | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
Comparison of the negative emotion
There was no statistical difference in HAMA scores and HAMD scores in the negative emotion before intervention between the two groups. After intervention, the HAMA score was 11.5±1.8 and the HAMD score was 13.2±1.4 in the observation group. This was statistically lower than those in the control group (all P<0.001), as seen in Table 4.
Table 4.
Comparison of HAMA scores and HAMD scores after intervention between the two groups
| Groups | HAMA scores | HAMD scores |
|---|---|---|
| Observation group | 11.5±1.8 | 13.2±1.4 |
| Control group | 18.2±2.5 | 17.6±1.8 |
| t value | 14.472 | 12.082 |
| P value | <0.001 | <0.001 |
Note: Hamilton Anxiety Scale (HAMA), Hamilton Depression Rating Scale (HAMD).
Comparison of satisfaction rate
As shown in Table 5, the satisfaction rate of pediatric patients in the observation group was higher than that in the control group (96.50% vs 82.00%, P<0.001). The satisfaction rate of family members in the observation group was 95.50% and 83.00% in the control group (all P<0.001).
Table 5.
Comparison of the satisfaction rate between the two groups [n (%)]
| Groups | Satisfaction rate of pediatric patients | Satisfaction rate of family members |
|---|---|---|
| Observation group (n=200) | 193 (96.50) | 191 (95.50) |
| Control group (n=200) | 164 (82.00) | 166 (83.00) |
| χ2 value | 21.914 | 16.286 |
| P value | <0.001 | <0.001 |
Comparison of DQ scores and ADL scores
Before the intervention, there was no significant difference in DQ scores (60.5±4.8 vs 61.2±5.1) and ADL scores (3.4±0.7 vs 3.6±0.8) between the two groups. After the intervention, the scores of both groups were increased (P<0.001). The DQ score (76.2±6.1 vs 97.2±6.4, P<0.001) and ADL score (5.8±0.9 vs 7.4±1.1, P<0.001) in the observation group were higher than those in the control group, as shown in Figure 1.
Figure 1.
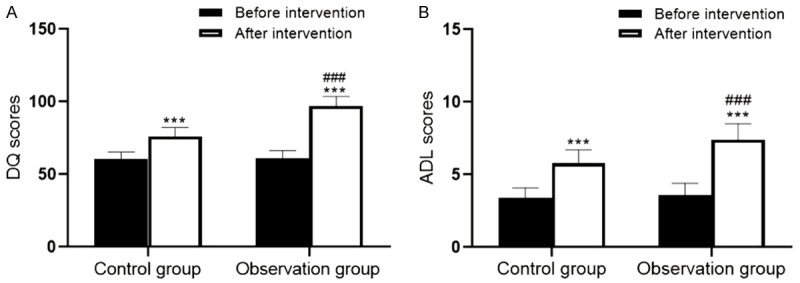
Comparison of DQ scores and ADL scores between the two groups. Compared with before intervention, ***P<0.001; Compared with the control group, ###P<0.001. Developmental quotient (DQ), Activities of Daily Living (ADL).
Comparison of the PDI and MDI scores
As seen in Figure 2, before the intervention, there was no significant difference in the PDI and MDI scores between the two groups. After the intervention, the PDI and MDI scores in both groups were increased (P<0.001). The PDI and MDI scores after intervention in the observation group were much higher than those in the control group (P<0.001).
Figure 2.
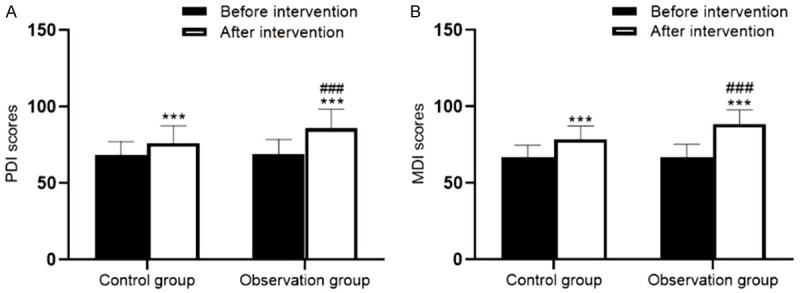
Comparison of PDI scores and MDI scores between the two groups. Compared with before intervention, ***P<0.001; Compared with the control group, ###P<0.001. Psychomotor development index (PDI), mental developmental index (MDI).
Comparison of compliance rate of pediatric patients, complaint rate of nursing and incidence of adverse events
As shown in Table 6, the compliance rate of pediatric patients in the observation group was 91.00%, which was higher than 77.00% in the control group. The complaint rate of nursing was 0.50% in the observation group, which was lower than 13.00% in the control group (all P<0.001). The incidence of adverse events was 11.00% in the control group. There was no adverse event in the observation group (P<0.001).
Table 6.
Comparison of compliance rate of pediatric patients, complaint rate of nursing, and incidence of adverse events between the two groups [n (%)]
| Groups | Compliance rate of pediatric patients | Complaint rate of nursing | Incidence of adverse events |
|---|---|---|---|
| Observation group (n=200) | 182 (91.00) | 1 (0.50) | 0 (0.00) |
| Control group (n=200) | 154 (77.00) | 26 (13.00) | 22 (11.00) |
| χ2 value | 14.583 | 24.824 | 23.280 |
| P value | <0.001 | <0.001 | <0.001 |
Discussion
The development of rehabilitation medicine has promoted the establishment of pediatric rehabilitation wards. The quality control management model in rehabilitation nursing has become a hot topic. Previous studies reported that the implementation of standardized quality control management in pediatric rehabilitation medicine can promote the recovery of pediatric patients and improve the quality of nursing care in hospitals, optimizing the medical system [14,15]. In this study, the comparison of quality control management between the conventional model and the standardized mode was performed, providing clinical evidence for guiding the pediatric rehabilitation treatment.
Pediatric rehabilitation is an important factor improving the intellectual and motor development of pediatric patients with cerebral palsy. To better facilitate recovery in these patients, this study exploited the standardized mode of quality control management. The results revealed that compared with the conventional model, the total rehabilitation effective rate in the standardized mode of quality control management was higher. The scores of DQ, ADL, PDI, and MDI of the observation group were increased. The negative emotions scores were decreased. All these results indicated that the standardized mode of quality control management could improve the pediatric neurological function, contributing to their intellectual and motor development. This was because the rehabilitation under standardized quality control management stimulated the development of brain cells and proliferation of glial cells. This promoted the pediatric mental development, restored the energy metabolism of nerve cells, decreased the necrosis of brain cells, and accelerated nerve repair. A rehabilitation study reported that the intelligence training using the standardized mode of quality control management could enhance the pediatric intelligence in patients with the cerebral palsy [16]. Popernack et al. reported that the standardized rehabilitation strategies in pediatric traumatic brain injury could improve the neurological function to some extent, due to physical and mental development of children [17].
The standardized mode of quality control management was helpful to improve the nursing care quality of pediatric rehabilitation. This standardized model had better performance in terms of communication efficiency, service attitude, disease observation, problem finding, formulation of rehabilitation program, and nursing procedures. According to the standardized mode, the rehabilitation quality control management working group was well organized and each member performed their own duties. Pediatric patients admitted to the hospital were received by the experienced head nurse, who detected the problems in each pediatric patient. The doctor in charge inquired about the past medical history, organized auxiliary examinations for the pediatric patients, and discovered the problems. In this standardized mode, the rehabilitation treatment plan was evaluated for three rounds. Communication between doctors, nurses, and the group leader was timely. The plan was constantly adjusted according to the situation of pediatric patients, which showed the characteristics of individualization. Some studies reported that the standardized model could enhance the responsibility of medical staff [18]. In various evaluation meetings, the assessments of the implemented plan and the recovery status of pediatric patients were completed. The nursing care and rehabilitation were performed and adjusted in strict accordance with the requirements of the plan. This resulted in better performance in service attitudes, nursing procedures, and higher working enthusiasms.
The standardized mode of quality control management could increase the compliance of pediatric patients, and the satisfaction rate from children and their families. Under the standardized mode, the rehabilitation treatment plan and family rehabilitation plan would be individually tailored following understanding accurately the pediatric patients’ conditions. During the process of implementation, continuous evaluation and adjustment were carried out so that it always met the needs of the pediatric patients. From admission to discharge, the entire quality control management group maintained a professional nursing procedure and a warm service attitude. This coupled with a good recovery effect, increased the trust of the pediatric patients and their family members and reduced the generation of negative emotions. It was reported that good psychological states were conducive to the recovery of the pediatric patients, entering a virtuous circle of good mood-excellent recovery effect-good mood. This improved the satisfaction rate of the pediatric patients and their families [19]. Due to young age and immature physiology and psychology, establishment of a harmonious and cordial relationship with pediatric patients, coupled with scientific and easy-to-implement nursing care methods, increased the compliance rate [16,20,21]. This was similar to the results in this study.
The standardized mode of quality control management can decrease the complaint rate of nursing and incidence of adverse events, ensuring the medical safety. Under the standardized mode of quality control management, the hospital staff could detect the problems in the plans and the improper procedures and make adjustments, reducing the incidence of adverse events [22,23]. This standardized model improved the satisfaction of pediatric patients and their families from all perspectives including personalized rehabilitation treatment plans, professionalism of medical staff, the relationships between doctor and patient, and high-quality of nursing care. This reduced the complaint rate of the medical care received [24-26].
In conclusion, the application of the standardized model of quality control management in pediatric rehabilitation medicine improved rehabilitation effects and the nursing quality. It had good performance in communication efficiency, service attitude, disease observation, problem finding, establishment of rehabilitation treatment plan, and nursing procedures. This standardized model could reduce negative emotions, incidences of adverse events and complaint rate, and increase the satisfaction of pediatric patients and their families. More promotion and application in clinical practice is needed. Our study had several limitations, such as the single-center study, the small sample size, short-term intervention of quality control management, lack of subgroup comparison, and long-term results. There was no additional evidence of the influencing factors that affected the standardization of rehabilitation quality control management. Exploitations of larger sample sizes of multi-center randomized controlled studies using long-term follow-up should solidify our conclusions.
Disclosure of conflict of interest
None.
References
- 1.Downs J, Blackmore AM, Epstein A, Skoss R, Langdon K, Jacoby P, Whitehouse AJO, Leonard H, Rowe PW, Glasson EJ Cerebral Palsy Mental Health Group. The prevalence of mental health disorders and symptoms in children and adolescents with cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2018;60:30–38. doi: 10.1111/dmcn.13555. [DOI] [PubMed] [Google Scholar]
- 2.Tseng SH, Lee JY, Chou YL, Sheu ML, Lee YW. Association between socioeconomic status and cerebral palsy. PLoS One. 2018;13:e0191724. doi: 10.1371/journal.pone.0191724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hollung SJ, Vik T, Wiik R, Bakken IJ, Andersen GL. Completeness and correctness of cerebral palsy diagnoses in two health registers: implications for estimating prevalence. Dev Med Child Neurol. 2017;59:402–406. doi: 10.1111/dmcn.13341. [DOI] [PubMed] [Google Scholar]
- 4.Li S, Tong G. An etiological study of intellectually disabled children under 14 years old in Anhui Province, China. Am J Transl Res. 2021;13:2670–2677. [PMC free article] [PubMed] [Google Scholar]
- 5.Birnkrant DJ, Bushby K, Bann CM, Apkon SD, Blackwell A, Brumbaugh D, Case LE, Clemens PR, Hadjiyannakis S, Pandya S, Street N, Tomezsko J, Wagner KR, Ward LM, Weber DR DMD Care Considerations Working Group. Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol. 2018;17:251–267. doi: 10.1016/S1474-4422(18)30024-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Merritt RJ, Cohran V, Raphael BP, Sentongo T, Volpert D, Warner BW, Goday PS Nutrition Committee of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. Intestinal rehabilitation programs in the management of pediatric intestinal failure and short bowel syndrome. J Pediatr Gastroenterol Nutr. 2017;65:588–596. doi: 10.1097/MPG.0000000000001722. [DOI] [PubMed] [Google Scholar]
- 7.Case LE, Apkon SD, Eagle M, Gulyas A, Juel L, Matthews D, Newton RA, Posselt HF. Rehabilitation management of the patient with duchenne muscular dystrophy. Pediatrics. 2018;142:S17–S33. doi: 10.1542/peds.2018-0333D. [DOI] [PubMed] [Google Scholar]
- 8.Yuan J, Wang J, Ma J, Zhu D, Zhang Z, Li J. Paediatric cerebral palsy prevalence and high-risk factors in Henan province, Central China. J Rehabil Med. 2019;51:47–53. doi: 10.2340/16501977-2486. [DOI] [PubMed] [Google Scholar]
- 9.Sun Z, Wang Y, Feng X. Effect of continuous nursing on negative emotion and quality of life in patients with leukemia under chemotherapy. Am J Transl Res. 2021;13:7935–7943. [PMC free article] [PubMed] [Google Scholar]
- 10.Hanson KT, Carlson KF, Friedemann-Sanchez G, Meis LA, Van Houtven CH, Jensen AC, Phelan SM, Griffin JM. Family caregiver satisfaction with inpatient rehabilitation care. PLoS One. 2019;14:e0213767. doi: 10.1371/journal.pone.0213767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meinzen-Derr J, Wiley S, Phillips J, Altaye M, Choo DI. The utility of early developmental assessments on understanding later nonverbal IQ in children who are deaf or hard of hearing. Int J Pediatr Otorhinolaryngol. 2017;92:136–142. doi: 10.1016/j.ijporl.2016.11.024. [DOI] [PubMed] [Google Scholar]
- 12.Poncet F, Swaine B, Dutil E, Chevignard M, Pradat-Diehl P. How do assessments of activities of daily living address executive functions: a scoping review. Neuropsychol Rehabil. 2017;27:618–666. doi: 10.1080/09602011.2016.1268171. [DOI] [PubMed] [Google Scholar]
- 13.Jary S, Kmita G, Whitelaw A. Differentiating developmental outcome between infants with severe disability in research studies: the role of Bayley Developmental Quotients. J Pediatr. 2011;159:211–214. e211. doi: 10.1016/j.jpeds.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 14.Melo RS, Lemos A, Paiva GS, Ithamar L, Lima MC, Eickmann SH, Ferraz KM, Belian RB. Vestibular rehabilitation exercises programs to improve the postural control, balance and gait of children with sensorineural hearing loss: a systematic review. Int J Pediatr Otorhinolaryngol. 2019;127:109650. doi: 10.1016/j.ijporl.2019.109650. [DOI] [PubMed] [Google Scholar]
- 15.Moreau NG, Bodkin AW, Bjornson K, Hobbs A, Soileau M, Lahasky K. Effectiveness of rehabilitation interventions to improve gait speed in children with cerebral palsy: systematic review and meta-analysis. Phys Ther. 2016;96:1938–1954. doi: 10.2522/ptj.20150401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castelli E, Fazzi E SIMFER-SINPIA Intersociety Commission. Recommendations for the rehabilitation of children with cerebral palsy. Eur J Phys Rehabil Med. 2016;52:691–703. [PubMed] [Google Scholar]
- 17.Popernack ML, Gray N, Reuter-Rice K. Moderate-to-severe traumatic brain injury in children: complications and rehabilitation strategies. J Pediatr Health Care. 2015;29:e1–7. doi: 10.1016/j.pedhc.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel A, Vieira MM, Abraham J, Reid N, Tran T, Tomecsek K, Vissoci JR, Eucker S, Gerardo CJ, Staton CA. Quality of the development of traumatic brain injury clinical practice guidelines: a systematic review. PLoS One. 2016;11:e0161554. doi: 10.1371/journal.pone.0161554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bravo L, Killela MK, Reyes BL, Santos KMB, Torres V, Huang CC, Jacob E. Self-management, self-efficacy, and health-related quality of life in children with chronic illness and medical complexity. J Pediatr Health Care. 2020;34:304–314. doi: 10.1016/j.pedhc.2019.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mink JW, Jenkins ME. Practice parameter: diagnostic assessment of the child with cerebral palsy: report of the quality standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2004;63:1985–1986. author reply 1985-1986. [PubMed] [Google Scholar]
- 21.O’Neil ME, Fragala-Pinkham MA, Westcott SL, Martin K, Chiarello LA, Valvano J, Rose RU. Physical therapy clinical management recommendations for children with cerebral palsy - spastic diplegia: achieving functional mobility outcomes. Pediatr Phys Ther. 2006;18:49–72. doi: 10.1097/01.pep.0000202099.01653.a9. [DOI] [PubMed] [Google Scholar]
- 22.de Vries U, Hampel P, Petermann F. [Patient education programs in child and adolescent rehabilitation] Rehabilitation (Stuttg) 2017;56:103–108. doi: 10.1055/s-0043-103062. [DOI] [PubMed] [Google Scholar]
- 23.Hainsworth T. The NSF for children, young people and maternity services. Nurs Times. 2004;100:28–30. [PubMed] [Google Scholar]
- 24.Vuillerot C, Dinomais M, Gautheron V, Brochard S. From singular to holistic: approaches in pediatric rehabilitation medicine for children with cerebral palsy. Ann Phys Rehabil Med. 2020;63:391–392. doi: 10.1016/j.rehab.2020.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Steenbergen B, Jongbloed-Pereboom M, Spruijt S, Gordon AM. Impaired motor planning and motor imagery in children with unilateral spastic cerebral palsy: challenges for the future of pediatric rehabilitation. Dev Med Child Neurol. 2013;55(Suppl 4):43–46. doi: 10.1111/dmcn.12306. [DOI] [PubMed] [Google Scholar]
- 26.Lee MJ, Yun YJ, Yu SA, Shin YB, Kim SY, Han JH. Integrative medicine rehabilitation for children with cerebral palsy: a study protocol for a multicenter pragmatic randomized controlled trial. Trials. 2020;21:723. doi: 10.1186/s13063-020-04639-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


