Abstract
Background
Healthcare providers performing aerosol-generating procedures like airway management are at the highest risk for contamination with coronavirus disease 2019 (COVID-19). We developed an in-situ simulation (ISS) airway management training in confirmed or suspected COVID-19 patients for emergency and anesthesiology staff, evaluated participants’ reactions, and identified perceived challenges.
Methods
We used a cross-sectional study design incorporating a quantitative questionnaire to describe participants’ reaction to the ISS and a qualitative group interview using the plus-delta debriefing modality to explore participants’ challenges in acquiring the knowledge and skills required for each learning objective. Data were analyzed using descriptive statistics and deductive content analysis.
Results
Two hundred and ninety-nine healthcare providers participated in 62 ISS training sessions. Over 90% of our study participants agreed or strongly agreed that: they understood the learning objectives; the training material appropriately challenged them; the course content was relevant, easy to navigate, and essential; the facilitators’ knowledge, teaching, and style were appropriate; the simulation facilities were suitable; and they had ample opportunities to practice the learned skills. The main challenges identified were anticipating difficult airways, preparing intubation equipment, minimizing the number of personnel inside the room, adhering to the proper doffing sequence, preparing needed equipment outside the intubation room, speaking up, and ensuring closed-loop communication.
Conclusion
The newly developed ISS training was feasible for busy healthcare practitioners to safely perform airway management procedures for suspected or confirmed COVID-19 patients without affecting bedside care. Anticipation of difficult airways and speaking up were the most frequent challenges identified across all specialties in this study.
Keywords: Simulation-based education, COVID-19, Airway management, PPE, Kirkpatrick level 1, Evaluation, Interprofessional training, In-situ simulation
Introduction
Coronavirus disease 2019 (COVID-19), the infectious disease caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), quickly became a worldwide threat to health and, particularly, to the health of healthcare providers. In Italy, healthcare professionals comprised 10.7% of the total number of cases [1]. In China, healthcare professionals represented 3.8% of all COVID-19 registered cases by February 2020, and 14.8% of these suffered severe or critical disease [2]. Rare breakthrough infections have been reported even among the healthcare providers immunized with the highly efficient BNT162b2 messenger RNA vaccine against SARS-CoV-2 [3]. The primary transmission mode of COVID-19 is via large respiratory droplets and direct contact (fomite) transfer. These virus-laden droplets have a diameter of more than 5 - 10 µm and usually disperse within a 2-m radius when emitted through sneezing and coughing by an infected patient. This contrasts with airborne transmission, which generally refers to particles smaller than 5 µm in diameter [4]. These particles can remain in the air for a prolonged period, disperse further by following the airflow, and penetrate standard surgical facemasks.
COVID-19 is currently not considered an airborne pathogen by the World Health Organization except in the context of aerosol-generating procedures (AGPs) [5]. AGPs are medical interventions that can produce virus-laden aerosolized droplet nuclei of sizes small enough to be considered airborne (e.g., tracheal intubation, non-invasive ventilation, tracheotomy, cardiopulmonary resuscitation, manual ventilation before intubation, bronchoscopy, airway suctioning, nebulization, and high-flow nasal oxygen) [4]. Airway management is a complicated procedure. Airway management of a critically ill patient suffering from infectious diseases comes with even more difficulties for the involved healthcare personnel. Existing literature showed that healthcare workers were at significant risk of infection during the SARS epidemic of 2003 [6], with tracheal intubation posing the highest risk for viral transmission [7]. However, the correct use of personal protective equipment (PPE) reduced transmission incidence significantly [8, 9]. Thus, special PPE donning and doffing procedures and algorithms were recommended for the healthcare practitioners performing airway management procedures [10]. Training of non-intensive care workers on critical care through healthcare courses can be supplied as a short-term education option in practice for a national emergency situation that requires immediate reactions in the event of a national emergency [11]. In-situ simulation (ISS) has been recognized as an essential tool for safety preparedness during the COVID-19 pandemic [12, 13]. To contribute to the COVID-19 prevention among healthcare professionals, we developed a novel ISS. Our goal was to train interprofessional adult and pediatric emergency and anesthesiology teams at King Fahad Medical City in Saudi Arabia in airway management for suspected or confirmed COVID-19 patients. The purpose of this multi-methods research study was to evaluate healthcare providers’ reactions to such training (Kirkpatrick evaluation level 1) and to identify the challenges encountered while adapting to the unique requirements of airway management in suspected or confirmed COVID-19 patients.
Materials and Methods
Study design
Following a pragmatic approach, we used a multi-method cross-sectional research design incorporating a quantitative questionnaire and a qualitative group interview using open-ended questions [14].
Participants and setting
A total of 299 healthcare providers were enrolled to participate in 62 ISS training sessions between April 5 and 24, 2020. We recruited adult emergency medicine, pediatric emergency medicine, and anesthesia departments’ staff to form teams of five healthcare professionals for each ISS session. We arranged the participants’ selection with the clinical department chairpersons and immediate supervisors for each discipline to randomly schedule an interprofessional team in each session. The team members were physicians, nurses, and respiratory therapists, or anesthesia technologists. The selection of the members of each team was decided the day before the ISS training session. Those selected were released from their clinical duties for the ISS training day. All participants signed an informed consent before enrolling in the study. Participation was voluntary and did not impact the participants’ job standing in any way. Participants had various professional backgrounds and had been involved in simulation-based learning activities at the Center of Research, Education, Simulation, and Enhanced Training (CRESENT); however, most participants were not exposed to ISS before this study. The researchers explained to participants the purpose of the study, and their participation in the study is voluntary and can be terminated at any point. The researchers explained to the participants that their decision to participate or refusal to participate would not impact their job standing in any way. This research was performed following the Declaration of Helsinki, and the Ethics Review Committee of the King Fahad Medical City in Riyadh, Saudi Arabia approved the study protocol (No. 20-199 on April 9, 2020).
Simulation scenario
Following the six-step curriculum development approach [15], six of the authors (Sabbagh AY, Cluntun A, Azizalrahman A, Almarshed A, Alzaid H, and Elmasry SH) developed a simulation curriculum targeting the following competencies: 1) Airway management for COVID-19 patients; 2) Infection control measures in AGPs for COVID-19 patients; and 3) Multidisciplinary teamwork and communication skills. We chose plus-delta as a debriefing modality to analyze actions as it is simple and easy to implement and standardize. This modality allows participants to self-reflect on what went well and what needed improvement. In our situation, plus-delta is more advantageous because it can help busy healthcare staff to properly utilize the short time they are present there and allow debriefers to collect as many points as possible [3, 16-23]. The course’ authors designed a standardized format for debriefers when using plus-delta to guide the discussion toward main objectives (Supplementary Material 1, Table S1, www.jocmr.org), and all instructors used Flipchart to collect debriefing points and fill them in the format immediately after the course. The debriefing guide included five steps: reaction, case description, analysis using plus-delta, summarizing, and report and evaluation [24]. The aim of the step, a description of how to conduct it and what questions to ask were provided for each step.
Scenario validation and intervention
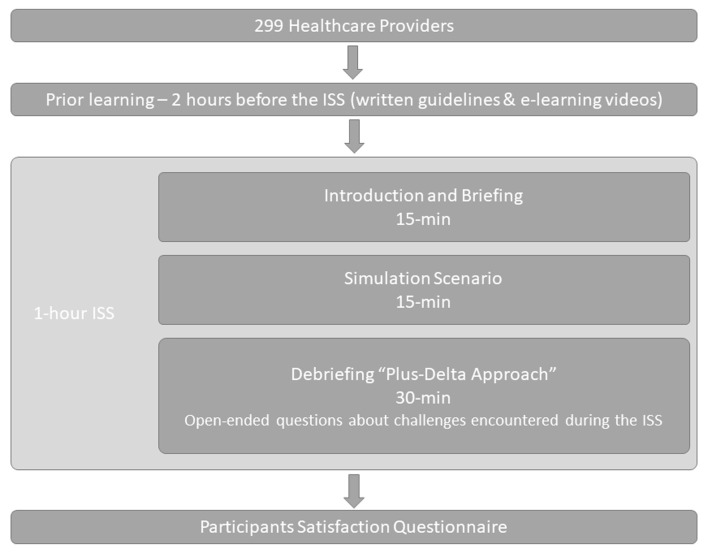
The simulation case scenario was reviewed and approved by the Curriculum Development Department at CRESENT. Between April 5 and 24, 2020, we conducted 62 1-h ISS sesstions to train interprofessional adult emergency, pediatric emergency, and anesthesiology teams in airway management for suspected or confirmed COVID-19 patients at the King Fahad Medical City departments. All ISS sessions took place in an unoccupied emergency room (ER) in the emergency department (ED), the pediatric ED, or an unoccupied operationg room (OR) during working hours. The study flow is presented in Figure 1.
Figure 1.
Study flow for in-situ simulation to train interprofessional adult emergency, pediatric emergency, and anesthesiology teams in airway management for suspected or confirmed COVID-19 patients. COVID-19: coronavirus disease 2019.
All participants were encouraged to read pre-course learning materials 2 h before the ISS. Learning materials were optional refreshers of knowledge about the correct use of PPE and included a checklist of tasks for each team member’s role (Supplementary Material 2, www.jocmr.org) and a video. The 15-min video was created at CRESENT and demonstrated appropriate PPE donning and doffing techniques.
Each ISS session started with a 15-min introduction and briefing in which the facilitator explained to the participants the nature of the simulation-based learning and addressed participants’ psychological safety, fictional contract, simulation fidelity, and confidentiality issues. The learners were also oriented on the simulation equipment. The facilitator explicitly stated the specific learning objectives for each competency. After the introduction and briefing, a simulation case scenario was conducted for 15 min. This specific length of time was determined based on the expected duration for the selected procedures and to provide learning time in-situ. During this time, the participating team practiced airway management of a simulated COVID-19 patient. Simulation intubation instruments were identical to those used in our emergency and anesthesia departments, except for the N95 masks, replaced by simple surgical masks to overcome the shortage during that period. The simulation equipment included the iPad application “Simple Patient Monitor” developed by Michael George, Intubating Airman® task trainer, simulated PPE powered air-purifying respirator (PAPR), yellow gowns, head cover, shoe cover, and protective eyewear (shield or goggles). The simulation developers provided all facilitators with a facilitator guide for the briefing to minimize individual variability (Supplementary Material 3, www.jocmr.org). ISS session facilitators were consultant-level experts in adult emergency medicine, pediatric emergency medicine, and anesthesia, with formal clinical simulation training. During each debriefing, the facilitator asked the participants open-ended questions about the challenges they experienced during the simulation, both individually and as interprofessional team members. The facilitator summarized and reported the emerging topics linked to each objective from the discussion with the participants. The facilitators used the same approach for all sessions. After the simulation scenario ended, the facilitator followed a debriefing guide using the plus-delta approach and a reflection on takeaways points (Supplementary Material 1, www.jocmr.org) to facilitate the debriefing session (30 min duration). The participants were given a chance to be engaged and self-reflected on the experience in a safe learning environment. During each debriefing, the facilitator asked the participants open-ended questions about the challenges they experienced during the simulation, both individually and as interprofessional team members.
Data collection
After participating in the ISS training, each participant completed an online, self-administered survey focused on three different elements: topic content, delivery, and facilitator evaluation. The survey contained 21 close-ended questions adapted from Kirkpatrick’s learner-centered reaction sheet and a free narrative space for the participants to write takeaway points to see if they had achieved the desired learning outcomes (Supplementary Material 4, www.jocmr.org). The closed-ended questions were anchored on a four-point Likert scale ranging from 1 - strongly disagree to 4 - strongly agree.
The qualitative data were collected via group interviews during the plus-delta debriefing for all the simulation sessions. The debriefing facilitator wrote the participants’ answers to the open-ended questions on a board during each debriefing, then transcribed them verbatim into an Excel file immediately following the debriefing session.
Main outcome measures
We assessed participants’ reaction to the ISS training regarding the session’s objectives, materials, content relevance, simulation facilitator’s knowledge, delivery, and style, and program and facilities evaluation. We also investigated participants’ perceptions regarding the achievement of desired competencies (Kirkpatrick evaluation level 1).
Secondary outcome measures
We explored participants’ challenges - both individually and as members of the interprofessional team - in acquiring the knowledge and skills required for each learning objective.
Data analysis
We performed a descriptive statistical analysis to describe participants’ reactions to the simulation training. All statistical analyses were performed using Microsoft Excel (2021). The debriefing transcripts of responses to the open-ended questions were analyzed using deductive qualitative content analysis, drawing on the course objectives as the coding frame. The themes for our analysis were preset according to the course learning objectives. Several researchers performed individual open coding then met to discuss and agree on codes and code definitions (analysts triangulation) for credibility. Following open coding, similar codes were grouped into categories and subcategories. Each category was fitted into the corresponding theme. To ensure the confirmability of the findings, categories and subcategories were revised and discussed with Rosu CA, who has extensive experience in qualitative research (peer debriefing).
Results
Statistical analysis
A total of 62 ISS sessions were conducted: 15 for pediatric emergency teams, 20 for adult emergency teams, and 27 for anesthesia teams, respectively. Two hundred seventy-eight responses were collected from 299 participants (100% response rate from adult and pediatric emergency and 91.7% response rate from anesthesia participants). The description of our teams’ demographic characteristics is presented in Table 1.
Table 1. Teams’ Characteristics.
| Participants | Pediatric, N (%) | Adult, N (%) | Anesthesia, N (%) | Total, N (%) |
|---|---|---|---|---|
| Total participants | 71 | 99 | 129 | 299 |
| Consultants | 9 | 20 | 37 | 170 |
| Physician specialists | 12 | 3 | 34 | 49 |
| Fellows | 14 | - | - | 14 |
| Residents | 0 | 16 | 25 | 41 |
| Nurses | 30 | 40 | - | 70 |
| Anesthesia technologist | - | - | 33 | 33 |
| Respiratory therapists | 6 | 20 | - | 26 |
Participants’ reaction to the simulation training
Over 90% of the participants in our study agreed or strongly agreed that they understood and could relate each learning objective to the achieved learning and were appropriately challenged by the training material (Table 2). Similar percentages agreed or strongly agreed that course materials were easy to navigate and essential for the procedure’s safe practice, and the content was relevant. Facilitators’ knowledge, teaching, and style were deemed appropriate by more than 90% of the trainees. Similar percentages of study participants agreed or strongly agreed that they were given ample opportunity to practice the skills they learned and that the simulation facilities were suitable for such training.
Table 2. Participants’ Satisfaction With the Session’s Objectives, Materials, Content Relevance, and Facilitator’s Knowledge, Delivery, and Style.
| In-situ simulation session item | Agree, N (%) | Strongly agree, N (%) |
|---|---|---|
| Program objectives | ||
| I understood the learning objectives. | 40 (14.39%) | 235 (84.53%) |
| I was able to relate each of the learning objectives to the learning I achieved. | 45 (16.19%) | 230 (82.73%) |
| I was appropriately challenged by the material. | 50 (17.99%) | 225 (80.94%) |
| Course materials | ||
| I found the course materials easy to navigate. | 65 (23.38%) | 205 (73.74%) |
| I felt that the course materials will be essential for my success. | 64 (23.02%) | 208 (74.82%) |
| Content relevance | ||
| I will be able to immediately apply what I learned. | 59 (21.22%) | 216 (77.70%) |
| Facilitator knowledge | ||
| My learning was enhanced by the knowledge of the facilitator. | 42 (15.11%) | 232 (83.45%) |
| My learning was enhanced by the experiences shared by the facilitator. | 40 (14.39%) | 234 (84.17%) |
| Facilitator delivery | ||
| I was well engaged during the session. | 43 (15.47%) | 232 (83.45%) |
| It was easy for me to get actively involved during the session. | 45 (16.19%) | 230 (82.73%) |
| I was comfortable with the pace of the program. | 47 (16.91%) | 228 (82.01%) |
| I was comfortable with the duration of the session. | 47 (16.91%) | 227 (81.65%) |
| Facilitator style | ||
| I was engaged during the session. | 42 (17.52%) | 234 (84.17%) |
| I was given ample opportunity to get answers to my questions. | 39 (14.03%) | 236 (84.89%) |
| I was given ample opportunity to practice the skills I am asked to learn. | 39 (14.03%) | 236 (84.89%) |
| Program evaluation | ||
| I was given ample opportunity to demonstrate my knowledge. | 44 (15.83%) | 231 (83.09%) |
| I was given ample opportunity to demonstrate my skills. | 43 (15.47%) | 232 (83.45%) |
| Pre-course reading and video | ||
| It was helpful to review knowledge and skills related to the simulation objectives. | 51 (18.35%) | 219 (78.78%) |
| Facility | ||
| I found the room atmosphere to be comfortable. | 62 (22.30%) | 209 (75.18%) |
| I was pleased with the room set-up. | 67 (24.10%) | 205 (73.74%) |
| I experienced minimal distraction during the session. | 67 (24.10%) | 203 (73.02%) |
Content analysis
Airway management challenges identified by the participants
Sixty-two Excel data files with the transcripts gathered from 62 simulations were analyzed. The absolute frequencies of the codes for each theme are presented in Table 3. The qualitative analysis identified themes and sub-themes common across the three specialties: pediatric emergency, adult emergency, and anesthesia for the three main learning competencies.
Table 3. Absolute Frequencies of Codes for Each Theme.
| Theme | Category | Subcategory | Number of codes | Example of facilitators’ summaries of participants’ comments |
|---|---|---|---|---|
| Airway management | Anticipation | Anticipation of difficult airway | 33 | Anticipated difficult airway |
| Preparation | Preparation of intubation equipment | 29 | Equipment checks before intubation | |
| Connection of the catheter (extension) device in pediatric patients | 6 | Use the catheter (extensor) | ||
| Connection of the bag-mask ventilation device to the PEEP valve device | 5 | Do not forget the PEEP valve | ||
| Pre-oxygenation | Pre-oxygenation using two-handed bag-mask ventilation technique (V-E) for 3 - 5 min | 18 | Pre O2 with two hands technique, V shape holding the mask | |
| Administration of low flow O2 in case desaturation with minimal pressure < 20 mm Hg | 15 | Low flow O2 | ||
| Application of high flow nasal cannula in case of desaturation | 6 | Need to improve oxygenation for COVID-19 patients by using high flow nasal cannula and minimize using Ambu bag | ||
| Application of high flow non-rebreathing mask in case desaturation | ||||
| Avoidance of non-invasive ventilation | ||||
| Protection | Closure of the suction system | 19 | Close suction | |
| Placement | Assignment of the expert to intubate | 14 | Intubation need to be done by a most expert in the room | |
| Usage of video laryngoscopy | 9 | Order video laryngoscope | ||
| Performance RSI | 9 | RSI medication | ||
| Post-intubation management | Inflation of the cuffed endotracheal tube 5 mm Hg > PAWP | 9 | Inflating the cuff before the ventilation | |
| Assure of the placement of the endotracheal tube | 12 | Check the tube position | ||
| Assure clamping of ETT | 22 | Clamp ETT | ||
| Infection control | Equipment | Familiarization with the equipment placement in the emergenct room | 5 | Need to be more familiar with equipment place |
| Prepare all the needed equipment outside the intubation room | 33 | Bring all the needed equipment inside to prevent going outside and inside the room, or assign a runner to prepare equipment from outside | ||
| Crowd control | Minimization the number of personnel inside the room | 24 | Limit the number of personnel in the room to limit exposure | |
| COVID-19 protection | Consideration of use of plastic cover for pediatric patients or plastic box for adults | 23 | Order the plastic cover for pediatric or the plastic box for adult | |
| Attachment of viral filter | 24 | Need to use a viral filter for the Ambu bag | ||
| Follow CDC/institutional guidelines for AGPs | 13 | Follow KFMC protocol | ||
| Application of surgical mask on the patient to minimize aerosolization | 5 | Keep an eye to minimize aerosolization by applying a mask | ||
| Prioritization of healthcare workers safety | 12 | Check with the team and make sure everyone is wearing a proper mask, and request PAPR if needed. | ||
| Donning | Adherence to the proper sequence of donning | 25 | The sequence of donning and doffing Do not wear a surgical mask under N95 |
|
| Doffing | Adherence to the proper sequence of doffing | 30 | Doffing is done outside | |
| PPE | Assignments of compliance observer during the procedure | 15 | Having a person outside to monitor appropriate donning and doffing | |
| Room ventilation | Assure the presence of HEPA filter maximum power | 5 | Check if filter inside the room | |
| Assure closure of the door during intubation | Closing the door throughout the procedure | |||
| Team dynamics | Clear orders | Loudness and clearness of the team leader voice | 15 | Avoid floating order Raise voices |
| Speaking up | Speaking up | 29 | The team needs to speak up if they have suggestions for the team leader. | |
| Role assignment | Assignment of the team members and roles clarity | 23 | Know your role | |
| Share mental model | A shared mental model with the team members | 17 | Share mental model | |
| Communication | Insure closed-loop communication | 20 | Close the loop of communication | |
| Leadership | Synchronous communication between the team leader and team | 14 | Avoid floating order and assign it to a specific person | |
| Anticipation | Anticipation of the challenges | 25 | Anticipate and act properly | |
| Situation awareness | Acquaintance with the equipment | 11 | The team leader needs to make sure that his team is familiar and knows how to use the equipment |
PPE: personal protective equipment; PEEP: positive end-expiratory pressure; HEPA: high-efficiency particulate air; COVID-19: coronavirus disease 2019; PAWP: pulmonary artery wedge pressure; ETT: endotracheal tube; RSI: rapid sequence intubation; CDC: Centers for Disease Control and Prevention; AGPs: aerosol-generating procedures; PAPR: powered air-purifying respirator.
Regarding the airway management competency, the panel identified six categories (anticipation, preparation, pre-oxygenation, protection, placement, and post-intubation management) and 14 sub-themes. For the second competency - infection control measures - seven themes (equipment, crowd control, COVID-19 protection, donning, doffing, PPE, and room ventilation) and 12 sub-themes were described. Lastly, nine themes (clear orders, speaking up, role assignment, shared mental model, communication, mutual respect, leadership, anticipation, and situation awareness) and nine sub-themes were developed for the team dynamic. Each facilitator summarized an average of nine challenges per session documented on the board during the debriefing as delta (areas needing improvement). Table 4 presents the top three challenges encountered during the ISS training by specialty.
Table 4. Top Three Challenges Encountered During the In-Situ Simulation Training by Specialty.
| Pediatric emergency | Adult emergency | Anesthesia | |
|---|---|---|---|
| Airway management | Anticipation of difficult airway | Preparation of intubation equipment | Anticipation of difficult airway |
| Assignment of the most expert provider to perform intubation | Using non-rebreathing mask/using high flow nasal cannula/avoidance non-invasive ventilation | Closure of the suction system | |
| Use of video laryngoscopy | Anticipation of difficult airway | Administration of low flow O2 in case desaturation with minimal pressure < 20 mm Hg | |
| Infection control | Minimization of the total number of personnel inside the room | Adherence to the proper sequence of doffing | Preparation of all needed equipment outside the intubation room |
| Prioritization of healthcare workers safety | Avoidance of incomplete donning or doffing of the PPE | Attachment of a viral filter | |
| Adherence to the proper sequence of donning | Consideration of using plastic cover for the pediatric or plastic box for adult | Following CDC/institutional guidelines in aerosol-generating procedure | |
| Team dynamic | Speaking up | Assure closed-loop communication | Speaking up |
| Assignment of the team and clarity of roles | Speaking up | Assignment of the team and clarity of roles | |
| Loudness and clarity of the team leader voice | Synchronous communication between the team leader and team | Loudness and clarity of the team leader voice |
CDC: Centers for Disease Control and Prevention; PPE: personal protective equipment.
Discussion
We developed and implemented a novel ISS to train interprofessional adult emergency, pediatric emergency, and anesthesiology teams in airway management for suspected or confirmed COVID-19 patients. We verified that most of the participants in these simulations found these efforts useful for their daily practice. We also identified specific challenges for the clinical practice and areas for which the intervention might protect healthcare providers and increase the safety of performing airway management procedures [14]. Our study offers an ISS curriculum that is feasible and can provide learning opportunities in a safe, simulated environment in the clinical area and can be replicated as deliberate practice. It helped explore possible challenges of both individual and system that help plan and prepare patients’ unexpected patterns related to the COVID-19 pandemic [25]. Hospital staff training was identified among the priorities during the COVID-19 pandemic [26]. Several studies utilized ISS to enhance hospital preparedness for the expected surge of COVID-19 patients. These studies identified and tested the readiness of the hospitals for the potential threats and risks imposed by COVID-19 and uncovered areas for improvement and timely staff training in the workplace [27-30].
Furthermore, the literature reports the advantages of ISS training for airway management of COVID-19 patients conducted for interprofessional teams training in EDs, critical care units, and operating rooms [31-34]. Our results are consistent with previous reports and support the benefits of ISS with interprofessional teams training for airway management in the pediatric emergency, adult emergency, and anesthesiology departments [12, 26, 28, 35]. In general, airway management is a complicated procedure that requires a combination of healthcare providers’ knowledge, skills, and behaviors. Simulation-based airway management training is superior to non-simulation intervention to achieve desired educational outcomes [36]. Simulation-based training conducted in real clinical environments using the available equipment and resources and involving actual healthcare teams offers experiential learning that promotes safety and enhanced team communication [29, 34]. ISS is more feasible for healthcare professionals in scheduling and availability without taking staff away from their clinical work and settings. In previous applications, ISS accelerated the development of skills and agility [29, 33, 37]. Similarly, in our study, participants in different clinical areas (pediatric ED and adult ED and ORs) reported that they felt prepared to care for COVID-19 patients’ airways while working in interprofessional teams utilizing appropriate infection control measures.
Other studies utilizing simulation-based training revealed significant latent risks and provided recommendations and corrections in the systems to respond to airway management for COVID-19 patients and infection prevention measures [29]. The use of ISS helped develop workable guidelines and visual aids that enhanced infection control measures implementation [31]. Using frequent ISS in the OR in preparation for surgical management of COVID-19 patients allowed the identification of potential threats and needed logistics for the work processes [38]. A study utilizing ISS to evaluate the readiness of intesive care unit (ICU) staff for COVID-19 patients identified deficiencies in ICU isolation rooms’ operation. These findings led to corrective actions to be taken before their first COVID-19 patient admission [31]. A similar study that utilized multidisciplinary ISS to understand preparation requirements for an outbreak and to assess the status quo before implementing adjustments resulted in mindful planning and resource allocation. The interdepartmental ISS training opportunities helped identify system issues and safety hazards in acute care settings [32].
Debriefing after the ISS was also one of the leading resources to identify safety threats. Most of the participants reported that they felt more prepared to provide care for COVID-19 patients [29]. Efforts were made to explore using simulation-based disaster exercises to test planned protocols for suspected COVID-19 patients in Saudi Arabia [30]. Mock codes conducted in the ED allowed early identification of defects related to preparedness and increased staff confidence in dealing with COVID-19 patients [39]. At our medical center, we explored individual, team, and system-related challenges experienced during ISS for airway management for COVID-19 patients. Multiple challenges emerged using the plus-delta debriefing method and were grouped into themes with corresponding categories and subcategories. Anticipating difficult airways and speaking up were the two most common ones across all the specialties included in our study.
Safe and secure airway management can be challenging in the OR, extending even postoperative. What’s more, failed intubation remains a significant cause of morbidity and mortality. Previously published literature identified anticipating the possibility of difficult airway preoperatively and modifying the airway management appropriately as a challenge for all the team members involved in the care of such patients [40, 41]. The participants in our study voiced similar concerns. These concerns were discussed in the debriefing in each ISS. The simulated experience helped the participants recognize various possible challenges in airway management and the need for a comprehensive action plan in preparation for possible challenges.
Speaking up is essential in multidisciplinary care teams, particularly in the OR, where patient safety can be in immediate danger. In recent years, simulation has been used to examine this concept in the OR [42-44]. Hierarchy gradients, organizational culture, and education were the most frequent factors affecting one’s ability to speak up and effectively challenge authority. Additionally, leader inclusiveness and creating a psychologically safe environment were found to help team members to overcome professional status differences and foster collaboration [45, 46]. We, too, found speaking up to be one of the two most frequent challenges across all the medical specialties included in the study. Explaining the causes of this finding was beyond the scope of the present study, but it might be due to individual, situational, or interpersonal and cultural factors.
Limitations
Our study has several limitations. We used a convenience sample not to interrupt the staff’s workflow in their specific departments. Thus, we may not have captured the whole range of reactions to our education intervention. We cannot estimate the magnitude of the sampling error since we performed only descriptive statistical analyses. To mitigate the inherent bias in self-reporting data, we collected and analyzed quantitative and qualitative data. In addition, we are unsure when and how many times the participants watched the training video; thus, we cannot eliminate exposure bias. Furthermore, our ISS was employed for adult and pediatric emergency medicine and anesthesiology staff; more research is necessary to assess the replicability of our findings beyond our context. What’s more, while knowing how well a training program is received (Kirkpatrick level 1) is essential, future evaluations to assess participants’ acquisition of the required knowledge and skills and to what extent this training is beneficial to our medical center (Kirkpatrick levels 2 and 3) are necessary to enhance and maintain our newly developed simulation curriculum.
Conclusions
The newly developed ISS training was feasible to train adult and pediatric emergency and anesthesiology healthcare practitioners to safely perform airway management procedures for suspected or confirmed COVID-19 patients without affecting the clinical care at the bedside. “Anticipation of difficult airways” and “speaking up” were the most frequent among the challenges we identified and were shared across all specialties included in this study.
Supplementary Material
Learning materials: checklist of tasks for each team member’s role.
Facilitator guide for briefing.
Debriefing guide for the facilitator (instructor).
Kirkpatrick’s learner-centered reaction sheet.
Acknowledgments
The authors would like to thank Mohammad Alamar, Asim Alsaeed, Areej Almuwaisheer, Rawan Eskandrani, Shadi Almozaini, Mosa Alkhalifa, and Ziad Zikri for their help with this study and also Suzan Kardong-Edgren for reviewing the manuscript.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the study subjects before participating in the study.
Author Contributions
Sabbagh AY and Cluntun A contributed to study conceptualization and design. Sabbagh AY, Cluntun A, Azizalrahman A, Almarshed A, Alzaid H, and Elmasry SH developed the simulation curriculum. Alzaid H and Sabbagh AY contributed to the acquisition of data. Sabbagh AY, Azizalrahman A, Almarshed A, Alzaid H, and Elmasry SH contributed to data analysis and interpretation. Rosu CA contributed to peer debriefing and provided input to the strategy for qualitative data analysis and interpretation. Sabbagh AY, Cluntun A, Almarshed A, Alzaid H, and Alzahrani A wrote the manuscript. Rosu CA and Alzoraigi U edited and revised the manuscript. Alzahrani A prepared and submitted the manscript for publication.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
References
- 1.Lapolla P, Mingoli A, Lee R. Deaths from COVID-19 in healthcare workers in Italy-What can we learn? Infect Control Hosp Epidemiol. 2021;42(3):364–365. doi: 10.1017/ice.2020.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in china: summary of a report of 72314 cases from the chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Bergwerk M, Gonen T, Lustig Y, Amit S, Lipsitch M, Cohen C, Mandelboim M. et al. COVID-19 breakthrough infections in vaccinated health care workers. N Engl J Med. 2021;385(16):1474–1484. doi: 10.1056/NEJMoa2109072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Transmission of SARS-CoV-2: implications for infection prevention precautions [Internet]. Available at: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions. Accessed May 9, 2021.
- 5.Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323(16):1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kamming D, Gardam M, Chung F. Anaesthesia and SARS. Br J Anaesth. 2003;90(6):715–718. doi: 10.1093/bja/aeg173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4):e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicolle L. SARS safety and science. Can J Anaesth. 2003;50(10):983. doi: 10.1007/BF03018360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yao W, Wang T, Jiang B, Gao F, Wang L, Zheng H, Xiao W. et al. Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: lessons learnt and international expert recommendations. Br J Anaesth. 2020;125(1):e28–e37. doi: 10.1016/j.bja.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lois F, Hallet C, Samalea Suarez N, Ghuysen A, Brichant JF. In situ simulation improves perceived self-efficacy of OR nurses and anaesthesiologists during COVID-19 pandemic. BMJ Simul Technol Enhanc Learn. 2021;7(6):555–560. doi: 10.1136/bmjstel-2020-000840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alsolamy S, Cluntun A, Aldekhyl S, Sabbagh AY, Alshehri TO, Yousif S, Abuznadah WT. et al. A national initiative: training nonintensivists in critical care, an educational response to the COVID-19 pandemic. Saudi Crit Care J. 2020;4(Suppl S1):34–39. [Google Scholar]
- 12.Fregene TE, Nadarajah P, Buckley JF, Bigham S, Nangalia V. Use of in situ simulation to evaluate the operational readiness of a high-consequence infectious disease intensive care unit. Anaesthesia. 2020;75(6):733–738. doi: 10.1111/anae.15048. [DOI] [PubMed] [Google Scholar]
- 13.Sharara-Chami R, Sabouneh R, Zeineddine R, Banat R, Fayad J, Lakissian Z. In situ simulation: an essential tool for safe preparedness for the COVID-19 pandemic. Simul Healthc. 2020;15(5):303–309. doi: 10.1097/SIH.0000000000000504. [DOI] [PubMed] [Google Scholar]
- 14.Zuo MZ, Huang YG, Ma WH, Xue ZG, Zhang JQ, Gong YH, Che L. et al. Expert recommendations for tracheal intubation in critically ill patients with noval coronavirus disease 2019. Chin Med Sci J. 2020;35(2):105–109. doi: 10.24920/003724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomas PA, Kern DE, Hughes MT, Chen BY. Curriculum development for medical education: A six-step approach. Johns Hopkins University Press; 2015. [Google Scholar]
- 16.Sawyer T, Eppich W, Brett-Fleegler M, Grant V, Cheng A. More than one way to debrief: a critical review of healthcare simulation debriefing methods. Simul Healthc. 2016;11(3):209–217. doi: 10.1097/SIH.0000000000000148. [DOI] [PubMed] [Google Scholar]
- 17.Fanning RM, Gaba DM. The role of debriefing in simulation-based learning. Simul Healthc. 2007;2(2):115–125. doi: 10.1097/SIH.0b013e3180315539. [DOI] [PubMed] [Google Scholar]
- 18.Mullan PC, Wuestner E, Kerr TD, Christopher DP, Patel B. Implementation of an in situ qualitative debriefing tool for resuscitations. Resuscitation. 2013;84(7):946–951. doi: 10.1016/j.resuscitation.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 19.Sweberg T, Sen AI, Mullan PC, Cheng A, Knight L, Del Castillo J, Ikeyama T. et al. Description of hot debriefings after in-hospital cardiac arrests in an international pediatric quality improvement collaborative. Resuscitation. 2018;128:181–187. doi: 10.1016/j.resuscitation.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 20.Zinns LE, Mullan PC, O'Connell KJ, Ryan LM, Wratney AT. An Evaluation of a New Debriefing Framework: REFLECT. Pediatr Emerg Care. 2020;36(3):147–152. doi: 10.1097/PEC.0000000000001111. [DOI] [PubMed] [Google Scholar]
- 21.Ahmed M, Arora S, Russ S, Darzi A, Vincent C, Sevdalis N. Operation debrief: a SHARP improvement in performance feedback in the operating room. Ann Surg. 2013;258(6):958–963. doi: 10.1097/SLA.0b013e31828c88fc. [DOI] [PubMed] [Google Scholar]
- 22.Rose S, Cheng A. Charge nurse facilitated clinical debriefing in the emergency department. CJEM. 2018;20(5):781–785. doi: 10.1017/cem.2018.369. [DOI] [PubMed] [Google Scholar]
- 23.Eppich W, Cheng A. Promoting excellence and reflective learning in simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Simul Healthc. 2015;10(2):106–115. doi: 10.1097/SIH.0000000000000072. [DOI] [PubMed] [Google Scholar]
- 24.Gardner R. Introduction to debriefing. Semin Perinatol. 2013;37(3):166–174. doi: 10.1053/j.semperi.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 25. COVID-19 Public Health Emergency of International Concern (PHEIC) Global research and innovation forum [Internet]. Available at: https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum. Accessed May 9, 2021.
- 26.Munzer BW, Bassin BS, Peterson WJ, Tucker RV, Doan J, Harvey C, Sefa N. et al. In-situ simulation use for rapid implementation and process improvement of COVID-19 airway management. West J Emerg Med. 2020;21(6):99–106. doi: 10.5811/westjem.2020.7.48159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brazil V, Lowe B, Ryan L, Bourke R, Scott C, Myers S, Kaneko H. et al. Translational simulation for rapid transformation of health services, using the example of the COVID-19 pandemic preparation. Adv Simul (Lond) 2020;5:9. doi: 10.1186/s41077-020-00127-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Daly Guris RJ, Doshi A, Boyer DL, Good G, Gurnaney HG, Rosenblatt S, McGowan N. et al. Just-in-time simulation to guide workflow design for coronavirus disease 2019 difficult airway management. Pediatr Crit Care Med. 2020;21(8):e485–e490. doi: 10.1097/PCC.0000000000002435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dharamsi A, Hayman K, Yi S, Chow R, Yee C, Gaylord E, Tawadrous D. et al. Enhancing departmental preparedness for COVID-19 using rapid-cycle in-situ simulation. J Hosp Infect. 2020;105(4):604–607. doi: 10.1016/j.jhin.2020.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lababidi HMS, Alzoraigi U, Almarshed AA, AlHarbi W, AlAmar M, Arab AA, Mukahal MA. et al. Simulation-based training programme and preparedness testing for COVID-19 using system integration methodology. BMJ Simul Technol Enhanc Learn. 2021;7:126–133. doi: 10.1136/bmjstel-2020-000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choi GYS, Wan WTP, Chan AKM, Tong SK, Poon ST, Joynt GM. Preparedness for COVID-19: in situ simulation to enhance infection control systems in the intensive care unit. Br J Anaesth. 2020;125(2):e236–e239. doi: 10.1016/j.bja.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jee M, Khamoudes D, Brennan AM, O'Donnell J. COVID-19 Outbreak Response for an Emergency Department Using In Situ Simulation. Cureus. 2020;12(4):e7876. doi: 10.7759/cureus.7876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Muret-Wagstaff SL, Collins JS, Mashman DL, Patel SG, Pettorini K, Rosen SA, Shaffer VO. et al. In situ simulation enables operating room agility in the COVID-19 pandemic. Ann Surg. 2020;272(2):e148–e150. doi: 10.1097/SLA.0000000000004056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Patterson MD, Geis GL, Falcone RA, LeMaster T, Wears RL. In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ Qual Saf. 2013;22(6):468–477. doi: 10.1136/bmjqs-2012-000942. [DOI] [PubMed] [Google Scholar]
- 35.Fong S, Li E, Violato E, Reid A, Gu Y. Impact of aerosol box on intubation during COVID-19: a simulation study of normal and difficult airways. Can J Anaesth. 2021;68(4):496–504. doi: 10.1007/s12630-020-01825-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kennedy CC, Cannon EK, Warner DO, Cook DA. Advanced airway management simulation training in medical education: a systematic review and meta-analysis. Crit Care Med. 2014;42(1):169–178. doi: 10.1097/CCM.0b013e31829a721f. [DOI] [PubMed] [Google Scholar]
- 37.Dieckmann P, Torgeirsen K, Qvindesland SA, Thomas L, Bushell V, Langli Ersdal H. The use of simulation to prepare and improve responses to infectious disease outbreaks like COVID-19: practical tips and resources from Norway, Denmark, and the UK. Adv Simul (Lond) 2020;5:3. doi: 10.1186/s41077-020-00121-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tong QJ, Chai JX, Tan LH, Prit S, Ong LT, Wu MYL, Ng LXL. Assessing operating room preparedness for COVID-19 patients through in situ simulations. Anesth Analg. 2020;131(2):e104–e106. doi: 10.1213/ANE.0000000000004935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aljahany M, Alassaf W, Alibrahim AA, Kentab O, Alotaibi A, Alresseeni A, Algarni A. et al. Use of in situ simulation to improve emergency department readiness for the COVID-19 pandemic. Prehosp Disaster Med. 2021;36(1):6–13. doi: 10.1017/S1049023X2000134X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gende G, Xing Y, Wen J, Raymond J, Laim E, Konga V, Dimugu L. et al. Management of difficult airways in surgical patients at the Port Moresby General Hospital operating theatre and intensive care unit. P N G Med J. 2012;55(1-4):67–75. [PubMed] [Google Scholar]
- 41.Kollmeier BR, Boyette LC, Beecham GB, Desai NM, Khetarpal S. StatPearls. Treasure Island (FL): 2021. Difficult airway. [PubMed] [Google Scholar]
- 42.Belyansky I, Martin TR, Prabhu AS, Tsirline VB, Howley LD, Phillips R, Sindram D. et al. Poor resident-attending intraoperative communication may compromise patient safety. J Surg Res. 2011;171(2):386–394. doi: 10.1016/j.jss.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 43.Lyndon A, Sexton JB, Simpson KR, Rosenstein A, Lee KA, Wachter RM. Predictors of likelihood of speaking up about safety concerns in labour and delivery. BMJ Qual Saf. 2012;21(9):791–799. doi: 10.1136/bmjqs-2010-050211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pian-Smith MC, Simon R, Minehart RD, Podraza M, Rudolph J, Walzer T, Raemer D. Teaching residents the two-challenge rule: a simulation-based approach to improve education and patient safety. Simul Healthc. 2009;4(2):84–91. doi: 10.1097/SIH.0b013e31818cffd3. [DOI] [PubMed] [Google Scholar]
- 45.Edmondson AC. Speaking up in the operating room: how team leaders promote learning in interdisciplinary action teams. Journal of Management Studies. 2003;40:1419–1452. doi: 10.1111/1467-6486.00386. [DOI] [Google Scholar]
- 46.Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. Journal of Organizational Behavior. 2006;27:941–966. doi: 10.1002/job.413. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Learning materials: checklist of tasks for each team member’s role.
Facilitator guide for briefing.
Debriefing guide for the facilitator (instructor).
Kirkpatrick’s learner-centered reaction sheet.
Data Availability Statement
The authors declare that data supporting the findings of this study are available within the article.