Abstract
Introduction:
Hyperkyphosis commonly affects older people but is not widely acknowledged as a clinically actionable problem, especially in men. There are several techniques to quantify kyphosis including the blocks and Cobb angle measurements. This study includes both kyphosis measures to investigate whether older men with accentuated kyphosis may be at increased mortality risk.
Methods:
Men aged ≥65 years (N=5994) were recruited to participate in the MrOS prospective cohort study from 2000 to 2002 (baseline). Our primary cohort included 2,931 enrollees (mean age 79.3 years; SD 5.2) who underwent blocks-measured kyphosis from 2006–2009. Our secondary cohort included 2,351 participants who underwent radiographic Cobb angle measurements at baseline. Cox proportional hazards analyses were used to determine association between kyphosis and all-cause mortality while adjusting for prevalent radiographic vertebral fractures, bone mineral density, incident fractures, gait speed, timed chair stands, self-reported health, alcohol use, medical co-morbidities, and physical activity.
Results:
During a mean follow-up of 8.3 (SD 3.2) years, 1,393 participants died in the primary cohort. In this group, compared to men with 0–1 block kyphosis, increasing blocks-measured kyphosis was associated with increased mortality (HR: 1.26 to 1.53, p trend <0.001). With addition of prevalent vertebral fracture to adjusted models, the association remained significant in participants with severe kyphosis (3+ blocks-measured). Similarly, with addition of chair stand performance the association remained significant for 4+ blocks kyphosis. Walking speed did not attenuate the association of kyphosis and mortality. In the secondary cohort, there were no significant associations between radiographic Cobb angle kyphosis and mortality.
Conclusions:
Increasing blocks-measured kyphosis was associated with an greater risk of mortality in older men, indicating that hyperkyphosis identified on physical exam should be considered a clinically significant finding that may warrant further evaluation and treatment.
Keywords: Kyphosis, hyperkyphosis, mortality
Introduction
Hyperkyphosis, or increased thoracic curvature, commonly affects older people and is associated with risk of mortality, particularly in older women1–4. Explanations for why increased kyphosis is associated with death are not well delineated, but since many equate kyphosis with osteoporosis, there is an assumption that vertebral fractures and/or low bone density may be the underlying reason. Previous work has suggested that compared to older women without vertebral fractures, those with vertebral fractures suffered earlier mortality in large part due to pulmonary causes possibly due to fracture-induced thoracic changes which may cause restrictive respiratory dysfunction2 However, further investigations have since reported that hyperkyphotic women, irrespective of vertebral fracture status, are at increased mortality risk.4 Although historically thought to affect older women, excessive kyphosis was found in one study to disproportionately affect older men by a ratio of about 2:1.1 Thus, for this investigation, our aim was to investigate the association between kyphosis and mortality in older men while adjusting for prevalent radiographic vertebral fractures, low bone density, and other possible confounders.
Methods
Participants
Between March 2000 and April 2002, 5,994 community-dwelling men aged ≥65 years were recruited from population-based listings to participate in the Osteoporotic Fractures in Men (MrOS) prospective cohort study at six U.S. sites: Birmingham, AL; Minneapolis, MN; Palo Alto, CA; Monongahela Valley near Pittsburgh, PA; Portland, OR; and San Diego, CA. MrOS exclusion criteria included inability to walk without assistance from another person, a history of bilateral hip replacement, inability to consent, or expected survival of less than six months. Institutional review boards at all clinical centers approved the study protocol and written informed consent was obtained from all participants. The MrOS study design and recruitment have been described in detail elsewhere5,6 with its database available online at: https://mrosonline.ucsf.edu.
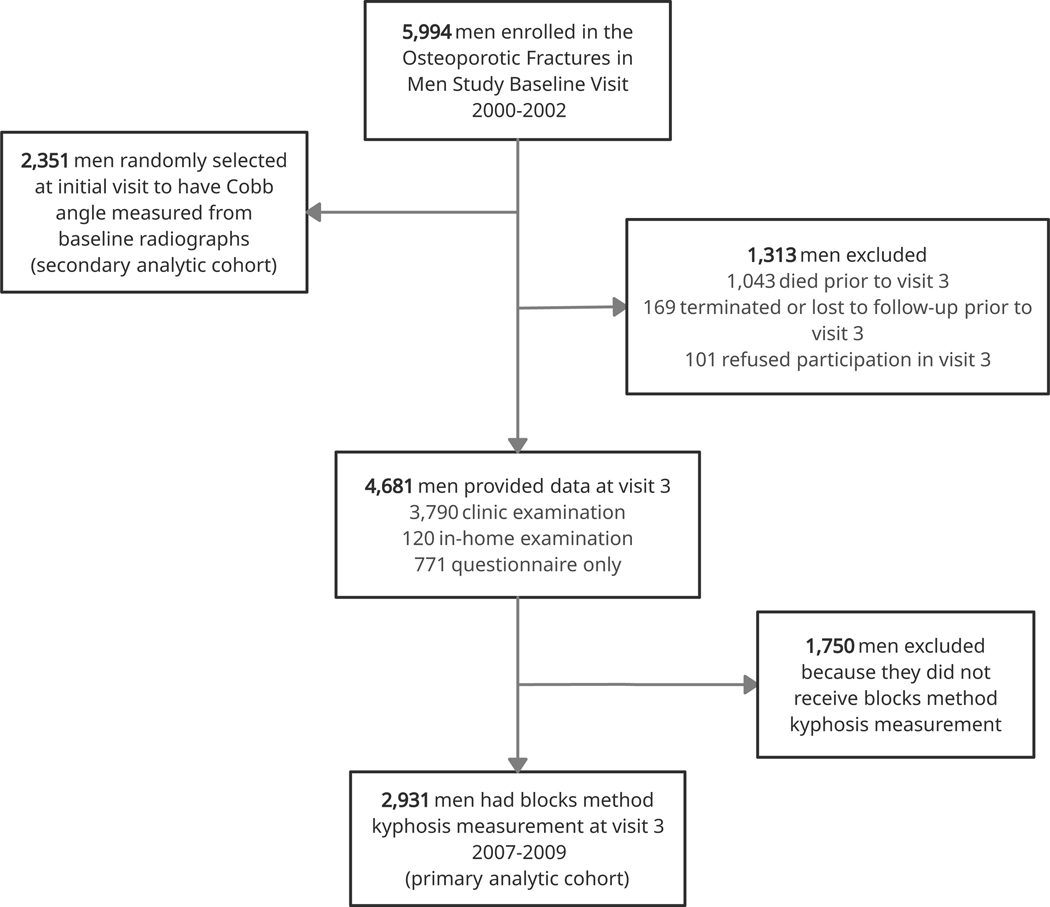
For this study, we used two different kyphosis assessments that were measured at different times during the overall MrOS study. Our a priori primary predictor was blocks-measured kyphosis, as this clinical measure had been previously shown to be associated with mortality in older women and men.1 Among the 5,994 MrOS enrollees, 4,681 men returned for visit 3 (March 2007 – March 2009) comprising the primary analytic cohort (see Figure 1). The blocks method kyphosis measurement was implemented late during visit 3 due to funding limitations so only 2,931 MrOS enrollees who attended visit 3 in the latter part of 2007–2009 completed blocks kyphosis measurements.
Figure 1.
Participant flow chart
The second measure of kyphosis was the Cobb angle measure from radiographs obtained during the baseline clinic visit (2000–2002). Of the original cohort of 5,994 men, 2,351 were randomly selected to have the Cobb angle measured. Of the 2,351 men who had Cobb angle kyphosis measured, 1,137 men also had the blocks measure of kyphosis performed.
Kyphosis Measurements:
Blocks
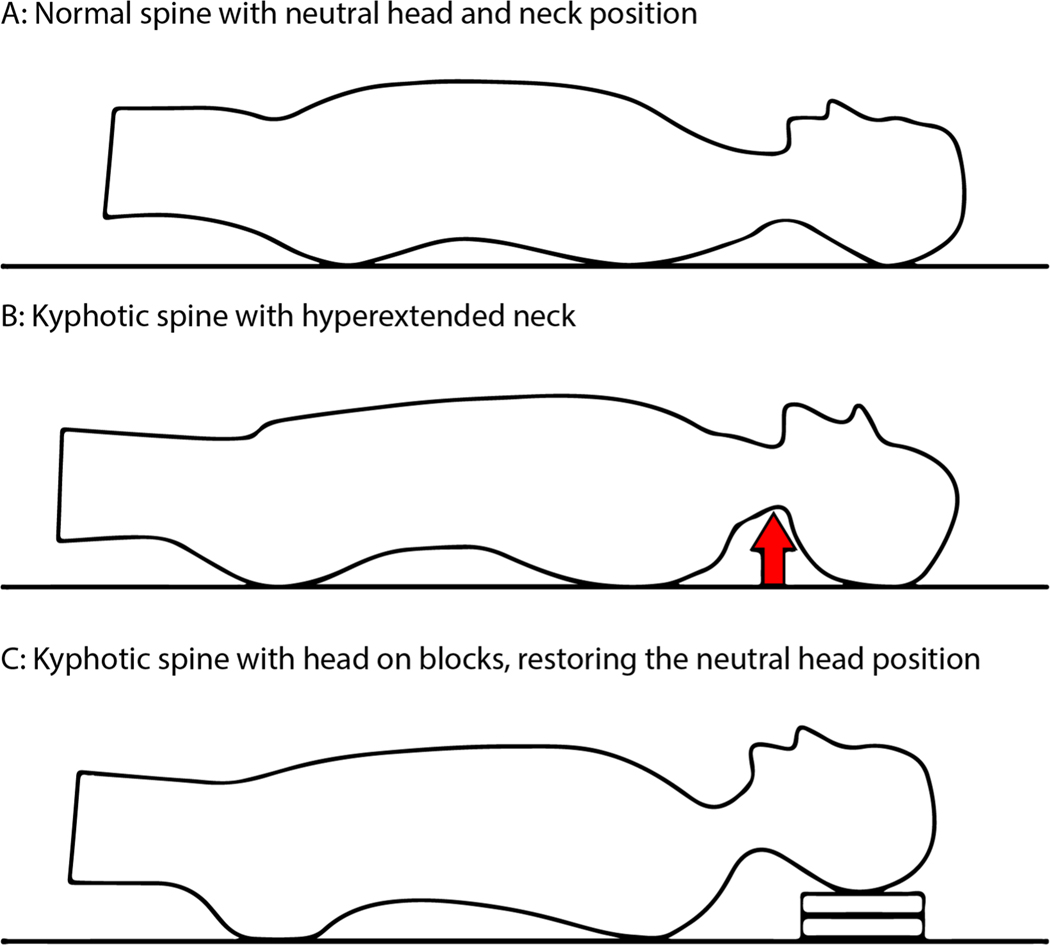
Kyphotic posture was measured using the blocks method (see Figure 2). Participants attending the third clinic visit were asked to lie supine on a radiology table. As needed, 1.7-cm blocks were placed under each participant’s head until a neutral position (participant’s head neither hyperextended nor hyperflexed) was achieved and the participant’s eyes were directed toward the ceiling (range 0–10 blocks). The number of 1.7-cm blocks needed to achieve this position was recorded. The interrater reliability of the blocks method was calculated using Spearman correlation coefficients and ranged from 0.85 to 1.00, depending on the clinic site.
Figure 2.
Measure of hyperkyphotic posture. A: Normal spine with neutral head and neck position. B: Kyphotic spine with hyperextended neck position. C: Kyphotic spine with head on blocks restores neutral head and neck position. Modified from Kado et al., (2004).1
Cobb angle
From lateral spine radiographs obtained while the participant was in a lying supine position, one study investigator (JTS) used Optasia software to place digitized points at the superior edge of T4 and the inferior edge of T12 from which the Cobb angle of kyphosis was calculated. If T4 and/or T12 were unable to be visualized, T5 and/or T11 were used.
Ascertainment of Mortality
Deaths were identified from participants’ families or contacts in responses to triannual questionnaires or phone calls. Deaths were confirmed by a study physician adjudicator utilizing death certificates. For the primary analytic cohort, the mean follow-up for mortality was 9.0 (SD=3.8) years and for the secondary cohort, the mean follow-up time was 13.0 (SD=5.8) years.
Prevalent Radiographic Vertebral Fractures
Radiographic vertebral fracture assessment was done at baseline and visit 2 (2005–2006) in the MrOS study and has been detailed elsewhere.7 For the primary analytic cohort at visit 2, lateral thoracic and lumbar spine radiographs were performed according to protocol and triaged by trained technicians. All films considered to have a possible fracture or other abnormality (“triage positive”) were evaluated by a study physician reader (JTS) using the Genant semi-quantitative (SQ) grading method7 to rate each vertebral level for fracture, with the modification that grade 1 fractures had to exhibit cortical discontinuity or depression of most of either the superior or inferior endplate to be considered fractured. Participants were defined as having a prevalent radiographic vertebral fracture when any baseline thoracic or lumbar vertebra had an SQ grade of ≥2. For the secondary analytic cohort, prevalent vertebral fractures were assessed at the baseline visit.
Bone Mineral Density
For the primary analytic cohort, at visit 3, areal bone mineral density (BMD) (g/cm2) was measured for the right hip using dual x-ray absorptiometry (DXA) (QDR4500W, Hologic, Inc., Waltham, MA), unless the participant reported a right hip replacement or metal objects in the right leg, in which case the left hip was measured. MrOS DXA quality assurance measures have been detailed previously.8 Based on common phantoms measured at all clinics, variability across clinics was limited, and cross-calibration correction factors were not required. Precision of hip DXA scans is 1 to 2%.9 For the secondary analytic cohort, bone density was measured at baseline.
Incident fractures
Postcard follow-up every four months collected information regarding incident fractures of any type. All self-reported fractures were confirmed by physician review of the radiologic report. For the primary analytic cohort, the mean follow-up time was 9.5 (SD= 3.4) years. For the secondary analytic cohort, the mean follow-up time was 14.2 (SD = 5.0) years.
Other Measurements
At visit 3, participants completed a self-administered questionnaire and were interviewed and examined in the clinical centers. Date of birth, race (white vs. nonwhite), smoking status (current vs. past/never), and current alcohol use (yes/no) were self-reported at baseline. Additionally, participants provided self-reported health (good-excellent vs. not), medical comorbidities that included a history of stroke, cancer (excluding non-melanoma skin cancer), diabetes, chronic obstructive pulmonary disease, hypertension, congestive heart failure, myocardial infarction, and Parkinson’s Disease. Self-reported physical activity was assessed using the Physical Activity Scale for the Elderly.10 Study staff also measured each participant’s height (stadiometer) and weight (balance beam or digital scale), and body mass index (BMI) was calculated as kg/m2. Gait speed was measured in two trials over a 6-m course. Each trial began with the participant standing still, and the two trials occurred consecutively without a rest between attempts. The result was reported in m/s as the mean of both times. Participants completed a timed five chair stands task with arms crossed at their chest.
Statistical Analyses
Baseline characteristics of men in the primary analytic cohort were compared across each blocks group (0–1, 2, 3, and 4+ blocks) using Mantel-Haenszel test for categorical data and ANOVA for continuous data (Table 1). We compared differences in visit 3 characteristics between 2,931 men who completed blocks measurements and 1,750 men who attended visit 3 but didn’t complete these measures using Chi-Square for categorical and T-Test for continuous variables (Table 2).
Table 1.
Baseline Characteristics of Primary Analytic Cohort by Blocks Kyphosis Group
| Block Kyphosis Group | p-value | ||||
|---|---|---|---|---|---|
| 0–1 Blocks (N=595) | 2 Blocks (N=875) | 3 Blocks (N=821) | 4+ Blocks (N=640) | ||
| Clinic Site | |||||
| Birmingham | 115 (19.3%) | 107 (12.2%) | 109 (13.3%) | 86 (13.4%) | <0.0001 |
| Minneapolis | 92 (15.5%) | 144 (16.5%) | 121 (14.7%) | 113 (17.7%) | |
| Palo Alto | 62 (10.4%) | 122 (13.9%) | 117 (14.2%) | 177 (27.7%) | |
| Pittsburgh | 57 (9.6%) | 183 (20.9%) | 173 (21.1%) | 62 (9.7%) | |
| Portland | 20 (3.4%) | 132 (15.1%) | 191 (23.3%) | 153 (23.9%) | |
| San Diego | 249 (41.8%) | 187 (21.4%) | 110 (13.4%) | 49 (7.7%) | |
| Age | 77.8 (SD 4.7) | 78.8 (SD 4.8) | 79.6 (SD 5.3) | 80.7 (SD 5.7) | <0.0001 |
| Caucasian | 520 (87.4%) | 760 (86.9%) | 733 (89.3%) | 588 (91.9%) | 0.003 |
| BMI | 26.4 (SD 3.6) | 27.2 (SD 3.6) | 27.3 (SD 4.3) | 27.3 (SD 4.0) | 0.0001 |
| Current Alcohol Use | 387 (65.4%) | 566 (65.0%) | 508 (62.0%) | 390 (61.0%) | 0.053 |
| Current Smoker | 12 (2.0%) | 14 (1.6%) | 17 (2.1%) | 14 (2.2%) | 0.64 |
| Excellent/Good Health Status | 538 (90.9%) | 770 (88.1%) | 678 (82.7%) | 529 (82.7%) | <0.001 |
| # of Comorbidity | 1.2 (SD 1.0) | 1.4 (SD 1.1) | 1.5 (SD 1.1) | 1.5 (SD 1.1) | <0.0001 |
| PASE Score | 138.9 (SD 65.5) | 134.3 (SD 67.6) | 128.7 (SD 71.6) | 118.7 (SD 68.6) | <0.0001 |
| Total Hip BMD | 0.94 (SD 0.14) | 0.95 (SD 0.14) | 0.94 (SD 0.15) | 0.92 (SD 0.16) | 0.0002 |
| Any Incident Fracture | 113 (19.0%) | 155 (17.7%) | 152 (18.5%) | 151 (23.6%) | 0.034 |
N (%) or Mean (SD)
Table 2.
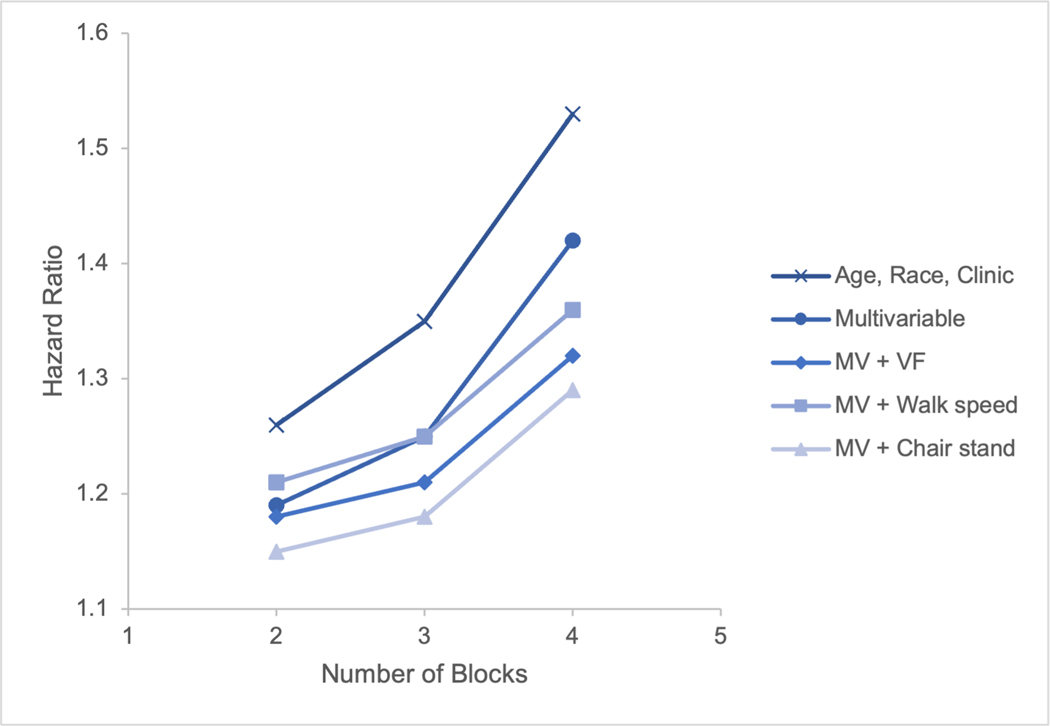
Blocks Kyphosis and All-Cause Mortality
| Kyphosis Classification* Hazard Ratio (95% Confidence Interval) |
||||
|---|---|---|---|---|
| Model† | 0–1 Block | 2 Blocks | 3 Blocks | 4+ Blocks |
| Age, race, clinic | Ref. | 1.26 (1.08 – 1.49) | 1.35 (1.14 – 1.59) | 1.53 (1.29 – 1.81) |
| Multivariable | Ref. | 1.19 (1.01 – 1.40) | 1.25 (1.06 – 1.48) | 1.42 (1.19 – 1.69) |
| MV + prevalent VF | Ref. | 1.18 (0.99 – 1.39) | 1.21 (1.02 – 1.44) | 1.32 (1.10 – 1.58) |
| MV + walk speed | Ref. | 1.21 (1.03 – 1.43) | 1.25 (1.05 – 1.48) | 1.36 (1.14 – 1.62) |
| MV + chair stand | Ref. | 1.15 (0.98 – 1.36) | 1.18 (1.00 – 1.40) | 1.29 (1.08 – 1.56) |
Comparison group is 0 to 1 blocks
Multivariable model adjusted for age, clinic, race, BMI, total hip BMD, comorbidity count, incident fracture, physical activity, self-reported health, and current alcohol intake p-value for trend = <0.0001
After confirming the assumption that hazards rates were proportional, we used Cox proportional hazards analyses to determine the association between kyphosis and all-cause mortality. We calculated hazard ratios (HR) and 95% confidence intervals (CI) for men with 2, 3 and 4+ blocks-measured kyphosis, with 0–1 blocks serving as the referent group. We performed a test of trend to evaluate correlation.
All multivariable models were initially adjusted for clinic site and age at the time of kyphosis assessment. Models were then additionally adjusted for several potential confounders of the association between kyphosis and mortality. Candidate potential confounders were included in multivariate-adjusted models based upon biological plausibility and if they were significantly associated with both the kyphosis measure (p≤0.10) and with all-cause mortality (p≤0.10 or changed beta-estimate by ≥10%) in age and clinic-adjusted models. The final multivariable-adjusted models included clinic site, and the following variables: age, race, BMI, comorbidity count (0 through 8), total hip BMD, incident clinical fracture (assessed post visit 3), physical activity, alcohol use, and self-reported health. To investigate potential mediators by which kyphosis might be associated with all-cause mortality, we also individually added either walking speed or chair stand ability (classified into quintiles of increasing time to complete the chair stand with the lowest quintile also including those who were unable to complete the task) to the final multivariable model. Finally, we added prevalent radiographic vertebral fractures to determine whether spine fractures might offer an explanation for any kyphosis-mortality association.
Results
The study sample included 2,931 men with a mean age of 79.3 years (SD 5.2). Baseline characteristics are listed in Table 1. The minority of men required only 0–1 blocks to achieve a neutral head position (20.3%, n=595), with 29.9% (n=875) requiring 2 blocks, 28.0% (n=821) requiring 3 blocks, and 21.8% (n=640) requiring 4+ blocks. Men requiring more blocks tended to be older, Caucasian, had slightly greater BMI, reported worse health, had more comorbidities, were less physically active, less likely to be current drinkers, had lower hip BMD, and were more likely to have an incident fracture. During a mean follow-up of 8.3 years (SD 3.2), 1,393 participants died.
Given that not all the men who attended visit 3 had the blocks measurement of kyphosis, we compared baseline characteristics of those who were and were not included in these analyses to test for any significant differences. We found that men without blocks measurement of kyphosis tended to be older, Caucasian, less likely to drink, report worse self-reported health status, and less physically active (see Supplementary Table S1).
In a model adjusted for age, race and clinical site, compared with 0–1 blocks, the hazards ratio for mortality increased from 1.26 for 2 blocks up to 1.53 for 4+ blocks (Table 2). With further multivariable adjustment, the hazards ratios were slightly attenuated by about 7–8%, but each model retained statistical significance. The p value for this trend was <0.0001.
As there is a known close relationship between prevalent vertebral fractures and kyphosis,11,12 we examined how adjustment for prevalent vertebral fractures assessed at visit 2 (2005–2006) may influence the association between blocks kyphosis and mortality risk (Table 2). Even after adding prevalent vertebral fracture to the fully adjusted model, the association between blocks-measured kyphosis and mortality retained significance in the two most kyphotic groups of men (3 blocks vs 0–1 blocks, HR 1.21 [1.02–1.44]; 4+ blocks vs. 0–1 blocks, HR 1.32 [1.10–1.58]) but not in those with mild kyphosis (2 blocks vs. 0–1 blocks, HR 1.18 [0.99 – 1.39]).
To consider whether the association between blocks and mortality might be explained by worse physical performance, we separately added walking speed to the multivariable model, and the association between hyperkyphosis and all-cause mortality was not substantially attenuated and remained statistically significant (Table 2). When we substituted chair stand performance for walking speed, the worst category of kyphosis was modestly associated with mortality, with the magnitude of association similar to that after consideration of prevalent vertebral fracture.
Considering Cobb angle kyphosis and mortality risk, there were 1479 men who died over the mean follow-up time of 13.0 (SD = 5.8) years. Whether investigating the overlapping sample of men who were included in the blocks kyphosis analysis (n = 1137) or the entire sample of men who had Cobb angle kyphosis measured (n = 2351) at Visit 1, we found no significant associations in age, race and clinic adjusted models between Cobb angle kyphosis and mortality risk (HR per degree increase of kyphosis = 1.00; 95% CI: 0.95 – 1.06, p value = 0.96). Considering threshold effects of either quartiles or quintiles, the results remained non-significant.
Discussion
In this cohort of community-dwelling older men, greater degree of kyphosis measured by the blocks method was associated with an increased risk of mortality. These findings are consistent with results previously reported among older men and women.1–4 There was a correlation between greater number of blocks and higher mortality risk even after adjusting for multiple potential confounders such as BMI, self-reported health, comorbidity count, hip BMD, incident clinical fractures, self-reported physical activity and other variables. Perhaps surprising was the complete null association between Cobb angle measured kyphosis and mortality risk in this group of older men.
Although Cobb angle kyphosis traditionally measured from plain lateral radiographs of the spine is thought to be the gold standard measurement of kyphosis, much of the epidemiological literature suggests that other measures of hyperkyphosis perform better in predicting adverse health outcomes. For example, in reports of kyphosis associations with poor self-reported and objective measures of physical function1,13,14, impaired pulmonary function,15 incident falls,16 and incident fractures,17 other measures of kyphotic posture including the Debrunner’s kyphometer, flexicurve, occiput-to-wall, and blocks measures of kyphosis were used instead of the traditional radiographic Cobb angle.
The blocks measure of kyphosis, similar to the occiput-to-wall measure, has now been reported in three separate cohorts, the Rancho Bernardo Study of 1,353 older community dwelling men and women residing in California,1 the Kurabachi study (n = 894 older Japanese community dwelling men and women)18 and the MrOS study.12 The advantage of the blocks measure is that, while not a precise estimation of degree, it is easy to identify a patient with clinically relevant hyperkyphosis on routine physical examination. Our study results add to the literature by indicating that not being able to lie flat on a DXA table is now associated not only with poorer physical function14 and subsequent falls,16 but also it confirms that accentuated kyphosis of >6.8 cm (equivalent to 4 blocks) to reach a neutral head position on a flat table is independently associated with increased mortality risk among men with greater degrees of kyphosis (3 or more blocks). This risk, while somewhat attenuated, remains even after adjusting for a measure of existing vertebral fracture and incident clinical fractures that are known mortality risk factors. Previously published studies of blocks-measured kyphosis and mortality risk did not adjust for prevalent radiographic vertebral fractures.1
It is reasonable to question why in this study, the Cobb angle was not associated with increased mortality risk while the blocks measure of kyphosis was. Unpublished data from the Study of Osteoporotic Fractures (SOF) and the Rancho Bernardo Study (RBS) which both had Cobb angle measures of kyphosis available demonstrated similar null findings and yet in SOF, the flexicurve standing measure of kyphosis was associated with increased mortality and in RBS, the blocks measure demonstrated a similar correlation of increasing blocks and greater mortality.1,4 In the current study, the Cobb angle was measured about 6.8 (SD = 0.3) years earlier than the blocks measure of kyphosis when the MrOS men were not only younger, but also were likely more healthy and had less kyphosis. However, based upon previous findings in other relatively large cohorts that found no association between Cobb angle kyphosis and mortality risk, we doubt that differences in who was exactly studied within the MrOS cohort is the explanation for the difference in findings.
Rather, we postulate that the need to use blocks to achieve a neutral head position while lying flat on an exam table captures an issue of fixed, flexed cervical ridigity that is associated with poorer health outcomes. The blocks measure, similar to the occiput to wall assessment serves to capture an upper thoracic and cervical postural change that is not captured with the traditional Cobb angle measure that typically ranges from T4 to T12 (lower down on the spine). Thoracic musculature may offer more flexibility than does cervical musculature where inter-spinal ligaments also play a prominent supporting role. Thus cervical kyphosis, when it develops, is less able to be corrected than thoracic kyphosis due to small muscular units and ligment inflexibility.
Considered in the context of prior kyphosis research, our present findings have potentially important clinical implications. Those with the most severe degrees of blocks kyphosis are at increased mortality risk regardless of underlying prevalent vertebral fractures or objectively measured poor physical function, and there was a significant correlation with p for trends, p< 0.001–0.007, regardless of covariate adjustment. Sugai et al, report that those who had blocks kyphosis progression (defined as >2 blocks) over 4 years of follow-up, were more likely to suffer from physical functional decline.18 Additionally, those who had worse kyphosis at baseline were more likely to experience worsening kyphosis over time. Given these observations, an older person who has difficulty lying flat within 3.4 cm of the table (2 blocks), might be counseled to improve posture and work on maintaining spinal muscle strength. Randomized controlled trials of back extensor strengthening demonstrate efficacy in reducing kyphosis progression.19,20
Although we adjusted our analyses for objective measures of physical function, including walking speed and timed chair stand, worsening physical function may result from worse kyphosis13,18 and be in the causal pathway between hyperkyphosis and mortality. If the hyperkyphosis precedes physical functional decline, then adjustment for measures of physical function in our study should not be made. However, the Kurabachi Study demonstrated that worsening grip strength preceded blocks kyphosis progression so we reported results with and without adjustment for measures of physical function.
It is worth noting in Table 1 that there is variability in kyphosis among the clinical sites. For example, the participants from San Diego appear to be less kyphotic than those from other sites. Although there was training across sites to optimize inter-rater reliability, it’s possible that variability in technique may have contributed to the differences between sites. Another possibility is that differences in geographic location affect the population’s health and thus their levels of kyphosis. For example, San Diego has a reputation for good weather and active lifestyle, which may confer a less kyphotic population. Nevertheless, we accounted for this site-based variability by adjusting for site in our analyses.
The current study has several important strengths, including its enrollment of a large cohort of community-dwelling older men. Additional strengths include its prospective design and the ability to adjust for multiple potential confounders. Our analyses also have several limitations. First, because MrOS participants are community-dwelling, largely healthy older men, our findings may have limited applicability to other populations. It would have been more ideal to have the blocks and Cobb angle kyphosis measures done at the same visit in the same men to allow more direct comparisons between the two. Also, since vertebral fractures are an important cause of hyperkyphosis, this study was limited in that prevalent vertebral fractures were assessed about two years prior to when the blocks measure of kyphosis was completed, so we cannot conclusively assert that it is not incident vertebral fractures that account for the observed increased mortality. Additionally, although we identified and adjusted for several confounders, there may be other unmeasured confounders not included in our analysis. Finally, it would have been interesting to look at cause-specific mortality, particularly pulmonary versus non-pulmonary causes of death, however the MrOS data set did not specify cause of death to that level of specificity.
In conclusion, our findings suggest that greater blocks-measured kyphosis is independently associated with increased risk of mortality, such that more severe kyphosis predicts earlier mortality independent of prior vertebral fractures, incident clinical fractures and objectively measured physical function. Given that randomized controlled trial results support that back extensor strengthening and posture training can improve kyphosis in older persons, these findings highlight the importance of identifying excessive kyphosis in the clinical setting, and intervening early to prevent the progression of kyphosis. The benefits of targeted kyphosis interventions on kyphosis progression and mortality warrant further study.
Supplementary Material
Supplementary Table S1. Comparison of characteristics between men with or without the blocks kyphosis measure at Visit 3
Figure 3.
Blocks kyphosis and all-cause mortality
Key Points.
Among older men, worse kyphosis as measured by placing blocks beneath their head while laying supine to achieve neutral head position was associated with earlier mortality.
This association remained even in models that adjusted for possible confounders like prevalent vertebral fracture, bone density, chair stand, and walking speed.
Why does this matter?
Hyperkyphosis on physical exam should be considered clinically significant and may warrant further evaluation and treatment.
Acknowledgments
Sponsor’s role:
The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute on Aging (NIA), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Center for Advancing Translational Sciences (NCATS), and NIH Roadmap for Medical Research under the following grant numbers: U01 AG027810, U01 AG042124, U01 AG042139, U01 AG042140, U01 AG042143, U01 AG042145, U01 AG042168, U01 AR066160, and UL1 TR000128. The National Institute on Aging (NIA) provided funding for Deborah Kado’s grant “Causes and Consequences of Hyperkyphosis in Older Persons” (R01 AG024246).
Funding information:
National Institute on Aging (NIA), Grant Numbers: U01 AG027810, U01 AG042124, U01 AG042139, U01 AG042140, U01 AG042143, U01 AG042145, U01 AG042168, R01 AG024246
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), Grant Number: U01 AR066160
National Center for Advancing Translational Science (NCATS), Grant Number: UL1 TR000128
Footnotes
Conflict of interest:
All authors have no conflicts of interest.
References
- 1.Kado DM, Huang MH, Karlamangla AS, Barrett-Connor E, Greendale GA. Hyperkyphotic posture predicts mortality in older community-dwelling men and women: a prospective study. J Am Geriatr Soc 2004;52(10):1662–1667. [DOI] [PubMed] [Google Scholar]
- 2.Kado DM, Browner WS, Palermo L, et al. Vertebral Fractures and Mortality in Older Women: A Prospective Study. Arch Intern Med 1999;159(11):1215–1220. [DOI] [PubMed] [Google Scholar]
- 3.Milne JS, Williamson J. A longitudinal study of kyphosis in older people. Age Ageing 1983;12(3):225–233. [DOI] [PubMed] [Google Scholar]
- 4.Kado DM, Lui LY, Ensrud KE, et al. Hyperkyphosis predicts mortality independent of vertebral osteoporosis in older women. Ann Intern Med 2009;150(10):681–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study--a large observational study of the determinants of fracture in older men. Contemp Clin Trials 2005;26(5):569–585. [DOI] [PubMed] [Google Scholar]
- 6.Blank JB, Cawthon PM, Carrion-Petersen ML, et al. Overview of recruitment for the osteoporotic fractures in men study (MrOS). Contemp Clin Trials 2005;26(5):557–568. [DOI] [PubMed] [Google Scholar]
- 7.Cawthon PM, Haslam J, Fullman R, et al. Methods and reliability of radiographic vertebral fracture detection in older men: the osteoporotic fractures in men study. Bone 2014;67:152–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cawthon PM, Ewing SK, McCulloch CE, et al. Loss of hip BMD in older men: the osteoporotic fractures in men (MrOS) study. J Bone Miner Res 2009;24(10):1728–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cummings SR, Bates D, Black DM. Clinical use of bone densitometry: scientific review. JAMA 2002;288(15):1889–1897. [DOI] [PubMed] [Google Scholar]
- 10.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol 1993;46(2):153–162. [DOI] [PubMed] [Google Scholar]
- 11.Kado DM, Huang MH, Karlamangla AS, et al. Factors associated with kyphosis progression in older women: 15 years’ experience in the study of osteoporotic fractures. J Bone Miner Res 2013;28(1):179–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Woods GN, Huang MH, Lee JH, et al. Factors associated with kyphosis progression in older men: The MrOS Study. J Bone Miner Res 2020; 35(11):2193–2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katzman WB, Vittinghoff E, Ensrud K, Black DM, Kado DM. Increasing kyphosis predicts worsening mobility in older community-dwelling women: a prospective cohort study. J Am Geriatr Soc 2010;59(1):96–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katzman WB, Harrison SL, Fink HA, et al. Physical function in older men with hyperkyphosis. J Gerontol A Biol Sci Med Sci 2015;70(5):635–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Bari M, Chiarlone M, Matteuzzi D, et al. Thoracic kyphosis and ventilatory dysfunction in sunselected older persons: an epidemiological study in Dicomano, Italy. J Am Geriatr Soc 2004;52(6):909. [DOI] [PubMed] [Google Scholar]
- 16.McDaniels-Davidson C, Nichols JF, Vaida F, Marshall LM, Kado DM. Kyphosis and 3-year fall risk in community-dwelling older men. Osteoporos Int 2020;31(6):1097–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang MH, Barrett-Connor E, Greendale GA, Kado DM. Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J Bone Miner Res 2006;31(3):419–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sugai K, Michikawa T, Takebayashi T, Nishiwaki Y. Association between muscle strength, mobility, and the progression of hyperkyphosis in the elderly: the Kurabuchi cohort study. J Gerontol A Biol Sci Med Sci 2019;74(12):1987–92. [DOI] [PubMed] [Google Scholar]
- 19.Katzman WB, Vittinghoff E, Lin F, et al. Targeted spine strengthening exercise and posture training program to reduce hyperkyphosis in older adults: results from the study of hyperkyphosis, exercise, and function (SHEAF) randomized controlled trial. Osteoporos Int 2017;28(10):2831–2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katzman WB, Parimi N, Gladin A, et al. Sex differences in response to targeted kyphosis specific exercise and posture training in community-dwelling older adults: a randomized controlled trial. BMC Musculoskelet Disord 2017;18(1):509. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1. Comparison of characteristics between men with or without the blocks kyphosis measure at Visit 3