Abstract
Background:
Medical professionals (doctors and other medical staff) in the field of healthcare everyday must make calculated decisions which have important consequences, impacting patients on the individual level, local (community), national or global level. Healthcare professionals must at times make these choices with limited information, resources, and knowledge, and yet is is expected that these decisions are highly calculated and accurate. It is important to familiarise oneself with the exact definitions regarding medical decision making.
Objective:
The aim of this study was to describe application of the most important rules to help decision makers to be good or excellent decision makers in medical practice at every level of health care system.
Methods:
The author used descriptive method of explanation teoretical and practical issues regarding application of od decision making processes in the praxis, based on searchied scientific literature about this topic deposited in online databases.
Results and Discussion:
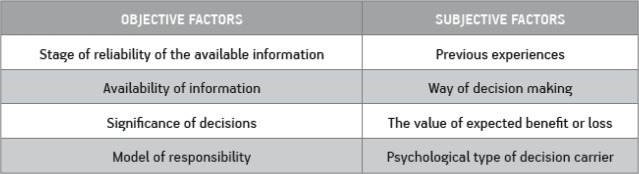
The author of this paper discussed about important topics: a) the importance of medical decision in emergency situations; b) the varies of decision making with solving problems by medical professionals; c) the limitations when it comes to medical decison making; and d) what doctors need to follow regarding decision making in the praxis. Two factors that have influenced to the decision process: a) degree of uncertainty about future events; b) usefulness of outcomes in any particular case. The clinical decision problem analysis process demands: a) explicit formalization of a decision making problem or the description of the medical problem decision with a registration of all possible actions which have to be undertaken and registration of all the possible so determined outcomes. b) construction of the decision tree which presents all described actions and outcomes with predictions of the probabilities and the choice of the most optimal action based on the probability outcome and its use. Doing this allows us to delve deeper into more intricate options present within medical decision making. Simple put, a decision is a choice between two options. The person or entity conducting that decision is the decision maker. The exact definition is “Under the decision should imply some specific action which is selected from several variables or which satisfies the expectation that is previously set”.Many different factors and individuals may be involved in medical decision making, with varying consequences, according to different players and settings.
Conclusion:
A vital component of medical decision making is evaluation. Decision makers must concisely evaluate situations, in order to make better choices. For example, when examining a health care system, their decisions should consider the following questions, such as, what is the health status of the given population? What economic resources are at the disposal of our patients, and government? How effective is the current healthcare model that is already in place? Does the existing social system pay enough attention to the healthcare protection? Does the organisation structure of the healthcare system satisfy? Are the existing practice and the healthcare technologies secure, effective, and suitable? Are the planning, programming, determination and the choice of priority the adequate to the needs of people? How are the monitoring and evaluation of healthcare system quality organised? These are a few examples of evaluation in medical decision making.
Keywords: Medical Decision Making, Decision makers
1. BACKGROUND
Everyday, doctors and individuals in the field of healthcare must make calculated decisions which have important consequences, impacting patients on the individual level, and communities and nations on a more global level (1-4). Healthcare professionals must at times make these choices with limited information, resources, and knowledge, and yet is is expected that these decisions are highly calculated and accurate (5-8).
Thus, the importance of medical decision making could not be greater, as, quite literally, lives are at stake. We have all witnessed, or directly been exposed to, medical decision making, and will certainly be continuously exposed to it, which is the reason why it could not be of more important. The intricate aspects of medical decision making will be discussed in this reiew.
A decision is a choice varying between several different courses of action that may be pursued (4). Each decision comes as a result of complex processes which provide two or more options providing results, as well as intro and retrospection, and examination or perspective into the future (9). As is in everyday life, the principles of decision making are present in medicine as well.
In the world of medical informatics, decisions may rely on the available systems of information provided to the decision maker through medical documentation (4).
Thus, the goal of Medical informatics is to provide decision makers with resources to ensure sound and correct decision making (2, 4). Additionally, it may ease and expedite the process of medical decision making, a luxury which was not always present for physicians or other medical professionals who providing health care protection.
Models of decision making must be recognised as a complex tool with many variables, and to produce a good model is to fully realise the structure and function of the real system in place, and once this is realised, only then can a health care system be totally revaluated and changed for large improvements (4).
A decision is a choice between two or more options. The person or entity conducting that decision is the decision maker. The exact definition is “Under the decision should imply some specific action which is selected from several variables or which satisfies the expectation that is previously set” (1, 4).
2. THE IMPORTANCE OF MEDICAL DECISIONS IN HEALTH CARE SYSTEM-IN EMERGENCY SITUATIONS
Decision making is particularly important in emergency situations, where fast and correct decisions must be made (1, 10). A patient’s life may be in danger, and so it is upon doctors to have excellent decision making skills. Countless examples of medical decision making that must be executed rapidly and accurately are present even outside the emergency room (4). These include, but are not limited to, the Heimlich manoeuvre in a restaurant, and homeostasis on the battle field in a violent conflict. Decision making pursues several different paths with varying courses of action and outcomes, which means that, graphically, decision making may be represented as a “decision tree” (4). With the leaves being the outcome, and the branches being courses of action. Of course, major branches multiply as decisions and outcomes become more complex.
This “tree” provides us with end results of our medical decisions. In regards to those end results, or outcomes of our medical decision making, as well as the accompanying facts associated with deciding, like resources and limitations, we find three levels of outcomes. They are strategic, tactic, and operational (technical) (Figure 1) (4, 11).
Figure 1. Three levels of decision making: strategic, tactic and operational (technical) (4).

The significance of medical decision making, as mentioned previously, is huge. On a personal level, decisions can alter the lives of patients. But on a more broader scale, decisions can result in health care system changes. This impacts the spheres of government, finance, health care, politics, and infrastructure. Thus, many different factors and individuals may be involved in medical decision making, with varying consequences, according to different players and settings. For example, medical decision making is not, and cannot, be the same in the United States, as it is in Bosnia and Herzegovina (4). Of course, there are wide differences in GDP between those two countries, and differing ethical beliefs as well. These two small examples illustrate larger differences in financial and cultural factors that constitute differences in these two countries.
A vital component of medical decision making is evaluation. Decision makers must concisely evaluate situations, in order to make better choices. For example, when examining a health care system, their decisions should consider the following questions, such as, what is the health status of the given population? What economic resources are at the disposal of our patients, and government? How effective is the current healthcare model that is already in place? Does the existing social system pay enough attention to the healthcare protection? Does the organisation structure of the healthcare system satisfy? Are the existing practice and the healthcare technologies secure, effective, and suitable? Are the planning, programming, determination and the choice of priority the adequate to the needs of people? How are the monitoring and evaluation of healthcare system quality organised (2)? These are a few examples of evaluation in medical decision making.
It is important to familiarise oneself with the exact definitions regarding medical decision making. Doing this allows us to delve deeper into more intricate options present within medical decision making. Simple put, a decision is a choice between two options. The person or entity conducting that decision is the decision maker. The exact definition is (4) “Under the decision should imply some specific action which is selected from several variables or which satisfies the expectation that is previously set”. Specifically, the bases of medical decision making lies largely with the primary decision maker, that is, the doctor. Doctors must analyse many factors while deciding, including risk, routine, certainty or lack thereof, and potential problems that may arise. They must also remember the past, to make better decisions in the future. Some of these past examples are well known, like when a doctor uses “clinical pathways for certain conditions…for example, in (the) case of (a) breast lump he will perform (a) biopsy avoiding intermediate steps. Such action is based on previous experience and knowledge” (6).
There are several schools of thought concerning medical decision making. These include the model proposed by Katz and Kahn, which considers the pressure on the decision maker, the problem type, the conductance of information retrieval, and the consideration of alternative answers (4).
A sound decision made specifies that connection between the means and the outcome. A rational decision maker will choose the best possible outcome that involves the least amount of resources. A rational individual will consider many different factors. Applied to the fields of medi-cine, these may include, but are not limited to, price of treatment, effectiveness of treatment compliance of the patient, pain and satisfaction of the patient, rules and regulations of the healthcare system, and many other factors. Of course, rational individuals, to maximise their outcomes, should be an expert, as will be mentioned in the following paragraph.
It is of the utmost importance that the rational decision maker is highly knowledgable, and has immediate and almost unlimited access to information. If this is the case, our decision maker is in the position to make better decisions. Of course, this is where modern technology and the organisation provided by medical informatics serves a crucial role. However, even the best doctors and decision makers are susceptible to error. These mistakes stem from a wide array of problems, particularly the fact that the human mind is limited in its ability to calculate multiple probabilities, as well as its occasionally tendency to lapse in judgement as well as memory. It is known that doctors often have problems while attempting to incorporate medical information regarding potential diseases outcomes into their decisions (1).
Perhaps most importantly, human emotion is what often alters the course of action conceived by medical decision makers. Doctors may change their choices due to sympathy or lack thereof, and so human emotions that are expressed may help or even hurt patients.
As a result of these factors and influences, the theory of adapted decision making emerges. This is one of the oldest theories, and it involves trial and error. It is upon the medical professional to concoct a plan of action for the patient, and then to periodically check to see the outcomes. If the patient is not improving, a new decision must be made. Doctors may, throughout this adapted decision making, analyse new facts, gather new information, alter existing decisions and treatment, or simply await for a solution (4). The progress must accurately and concisely noted, to serve as an instru-ment for current or future work.
Table 1. Type of medical decision making.
Table 2. In the relation to available knowledge and information the all physicians can be divided into four types of the decision carrier (4).
Table 3. The judgment of the decision carrier about that which actions should undertake in the accordance to the expected risk is calle (4)d the attitude according to the risk.
3. THE VARIES OF DECISION MAKING WITH SOLVING PROBLEMS BY MEDICAL PROFESSIONALS
Decision making varies according to the type of problem that awaits the medical professional (4). Medical decision making cannot be the same for a patient that is suffocating, and a patient that has cancer. Thus, some decisions must be made quickly while others take time. Some decisions are made that are not expensive, while others require vast amounts of financial aid and resources.
Medical decision making differs regarding the number of decision makers. Often, it is not only the physician who makes the decision, but also the patient. In addition, groups of physicians may be involved in the treatment of a patient. Finally, it must be mentioned that groups of individuals who are not doctors may make medical decisions, such as politicians concerned with the improvement of healthcare systems. For example, the most important part of introducing healthcare into the realms of politics is the arrival of questions of ethical controversies. Politicians have varying opinions regarding medical decisions, for example the permissibility of abortion. However it must be noted that in fact, it is ethics that should be the, “saving bridge between healthcare politics and the quantity and quality of the realisation of that politics” (3).
Despite the same goal of medical informatics and thus medical decision making, strong differences exist between varying parties under the umbrella of health care systems (4, 12-16). For example, “between research and education, curative and preventive medicine, and so on” (17). Additionally, politicians, economists, doctors, patients, and lawyers may all have different views and thus ideas and courses of action regarding the best methods when it comes to medical decision making and health care.
4. THE LIMITATIONS WHEN IT COMES TO MEDICAL DECISON MAKING
Unfortunately, there are many limitations when it comes to medical decision making. Specifically, these include uncertainty and ambiguity, on both ends of the spectrum. Uncertainty and its related ambiguities, are the essential limitations of medical decision making, even though other fac-tors contribute to poor or difficult medical decision making, although uncertainty is certainly the largest debilitating factor (12).
That is why the goal of some medical decision action is reduction of uncertainty (5). We may find many doctors who fall under this parameter previously mentioned. They include doctors who:
• Know that they do know
These doctors are perhaps the best decision makers. They are aware that they know how to resolve the problem, and will pursue a proper course of action. Doctors may not have to be especially intelligent or knowledgable in their area of experience to make these decisions, as there are frequent and routine medical decisions that occur in the clinical practice. These medical decisions are redundant and uniform in their consistency and are very rarely changed, so doctors may just recall those decisions and “follow instructions” (10).
• Know that they do not know
Although these physicians have limited knowledge, they are cognisant of that fact, and will as a result pursue measures after consultation with people who will help them make better decisions. A great aspect regarding these physicians is the fact that these physicians may be able to recognise the quantitative and qualitative problems associated with a certain patient, and will, based on that, assess in how much trouble a patient is in, despite not knowing how to diagnose or treat a patient. If this is the case, they will (or at least should) certainly refer the most serious conditions found in patients to more specialised caretakers (14).
• Do not know that they do know
These are doctors who may have little confidence, and yet they will, after some time, be able to help reach a sound decision. However, it is crucial that they gain confidence and/or information and knowledge, as non-acting in certain scenarios can be the wrong medical decision (13). This fact is perhaps most evident in emergency room situations, where action is vital and may save a patient’s life.
• Do not know that they do not know
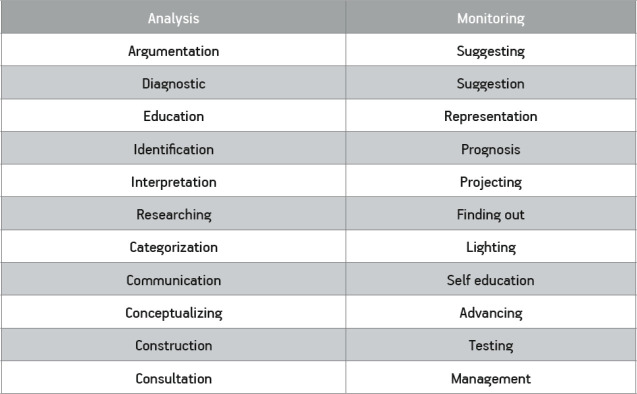
Table 4. The expert systems imitate a man in a field of knowledge and are capable for the various activities which belong to the nsultative -advising activity (4).
Table 5. The basic differnces among the clasic computers and the neuron nets (4).
Perhaps these are the worst decision makers. They may posses a false confidence that will lead to lacklustre medical decision making. At times this may not be their fault, as “psychologists emphasise that human opinion cannot bear with the complexity which is connected with the significant decisions. In the best case our brain can synchronously process seven to eight facts” (7). Even when attempting to better themselves, doctors may experience difficulties, as the process of learning is often tedious, difficult, and slow, and so a physician may repeatedly make mistakes over and over again despite their best intentions to learn and make better medical decisions.
5. WHAT DOCTORS NEED TO FOLLOW REGARDING DECISION MAKING IN THE PRAXIS
In regards to medical decision making, doctors must analyse risk in an appropriate manner. Risk, while possessing the potential to increase the reward associated with a decision, also carries with it potential for disaster. Thus, a doctor must effectively analyse risk and purse decisions care-fully. In analysing risk, a doctor must include the perception of risk, identification of risk, measurement of risk and evaluation of risk, as well as the quality and size of risk.
Additionally, risk may be accidental, and it may be forced. This is all done so that doctors may weigh risk factors, and ultimately decide upon a course of action, as the option or decision with lower risk will always be selected if the outcomes of the two respective decisions have the same benefits (15).
Doctors vary in their degree of utilisation of options that carry high levels of risk. Some are conservative while others are risk takers. Risk takers, or gamblers, will perform, for example, proce-dures that may extend, “patient life for 10 years even if they can choose (a) less risky procedure that will prolong life only five years” (16).
Another type of physician is the detective. “The physician as a detective is using the iron logic to achieve conclusions. He prefers hypothetical deductive method and chooses two and more active hypothesis and collect data in order to test hypothesis. The physician with more experience considers fewer hypotheses. This type of physician is more interested in case then in patient. Problems and riddles could be obsession of such physician. He will search for rare disease in cases where more common disorder occurs. The detectives are usually cautious to neutral; they prefer their ingenuity to risky actions” (16).
These two doctors are not the only kinds. There is also the artist. “The artists use imagination and intuition in the process of clinical judgment and decision making. They can be cautious but in same situation when benefit is significant they can take risk. They use heuristic in such situation that can be delusive. The main principles of physician artist are following: In the significant measure they use the available heuristic; Rank the criteria (goals) according to the significance and focus on the main criterion; The decisions and actions evaluate in pairs, for example, the disease A, the disease B, and mutually compare the outcomes of every state; When they examine two events, greater attention is paid to an event with the severe consequences, even when that event is less probable; When the situation is uncertain or ambiguous, they search for new data and information” (16).
Unfortunately, doctors often have limited resources and conflicts of interests when it comes to medical decision making. For example, perhaps a doctor wishes to pursue an effective and yet expensive treatment for a patient, but is unable to do so due to limited financial capability. Thus, the doctor must opt for a cheaper, and perhaps less effective, medical decision. Additionally, physicians are prone to conflicts of interest. This means that they may pursue a course of action due to their own personal interests and goals, which may not be aligned with the best outcome for the patient. This may be done in the pursuit of research, or financial gain.
While doctors are at times criticised for their actions, it is upon the physician to inform their patient that their wishes may be illogical and irrational, in their choice to undergo a certain therapy (19) or to make poor decisions on their own (20). While doctors are the main decision makers in medicine, the patient as the medical decision maker must also be recognised. Patients, through informed consent, have the right to be included in the decision making process. This may result in agreement or disagreement with the doctor and/or health care system. However, this does not diminish the importance of the patient’s right to be a decision maker. A patient’s preferences must be considered, and full information of the diagnosis and potential treatment must be disclosed to the patient, meaning informed consent. Patients differ in their reasoning, and so a course of medical action for one patient may not be sufficient, or may be too difficult, for another.
Thus, due to these limitations, “one person, even if it is physician, can rarely make decisions for other person. In fact, for the optimal decision making in the medicine most often the both physi-cian and patient with their knowledge and clearly determined goals participate together in the decision making” (4, 22).
However, what is quite common, is the following. A “patient enters the system of the healthcare protection, he makes with a doctor a special social agreement, according which he leaves all of his/her own expectations regarding the healthcare and the diseases leave to the knowledge and the responsibility of a doctor. They both follow their social and professional expectation. The pa-tient answers to the certain number of questions in order to diagnosing the patient disease and start adequate therapy. This relationship consider the fact that physician knows best what is best for patient and that there is no need to explain to patient the diagnostic and therapeutic procedures that should be done. Such attitude is widely spread in society. Such attitudes frequently neglect the in-terest of both participant of communication” (23-26).
This agreement between the patient and his physician is known as group decision making, or mutual decision making. It is of the utmost importance that there is full concordance between the two parties. Problems arise typically due to the fact that doctors may feel that they know much more than the patient, and may pursue decisions which are not comfortable for the patient. Likewise, patients may not be satisfied with a doctors diagnosis or treatment plan for them. However, the most effective medical decisions made, especially in so far as the implementation goes, lies in the agreement of the two parties, that is a mutual decision made. The joint work between these two parties will also be more easily assessed, as both parties may provide input as to whether or not the goals have been achieved (18). In the realm of psychology and psychiatry this is well codified and understood.
Collective responsibility is a term that must be mentioned. This is the right of groups of doctors to work together, to achieve what is best for the patient. Often, a single decision maker is not enough for the patients. And yet, with the slight help of other doctors, a collective decision may be made, which can assist the patient tremendously. Collective responsibility may also reflect the decision making on the part of a patient and the people representing him. For example, at times patients are not able to make decisions, due to, for example, the patient being in a comatose state. In these instances, the family may represent their loved one (21). Additionally, lawyers, and even the government, may represent patients who are not in a position to do so themselves (22, 26).
The Cascade Effect differs from collective responsibility in the initial phases. It results from the lack of reassurance of one party, which results in increased complications for another party. For example, if a doctor is unsure of his medical decision, and in an attempt to be safe, orders additional tests, the patient may become nervous. Thus the anxiety has encompassed not only the doctor, but now the patient as well. This patient, feeling anxious, may suffer from new problems that were non-existent before. Of course, these potentially eradicable problems arrived solely due to the lack of confidence from the original medical decision maker (4, 26-28).
Finally, we must mention and highlight the role of the inter-observer. This person or party has a given function, which involves monitoring and regulation of another persons medical decision making history and present acts. This may be one individual, or a group of people. Ideally, the inter-observer may promote positive and productive medical decisions, and may halt poor ones before a poor outcomes arises.
Recently, government agencies have stepped up to fulfil the role of inter observers, as the private market often fails to protect patients, as the main goals ae typically to maximise profit (22-25). A recent example in the United States, are select provisions under this law that serve the inter observer role for patients, often the least privileged members of society.
6. CONCLUSION
Medical decision making is highly important to doctors and patients alike, as well as the broader population. Medical decisions are vital, to both patients and society. They are difficult, and may provide positive outcomes, or poor complications. They test doctors maximally, and provide insight into the effectiveness of doctors. And finally, they are improvable, through increased financial support, legal regulations, peer monitoring and assistance, and increased levels of knowledge and information, which may stem from a strong system of medical documentation through medical informatics. A vital component of medical decision making is evaluation. Decision makers must concisely evaluate situations, in order to make better choices.
Author’s contribution:
The author was included in all phases of preparation this article and also made final proofreading before printing the text..
Conflict of interest:
None declared.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Harvey IM, Roberts CJ. Clinical guidelines, medical litigation and the current defence system. Vol. 1. Lancet; 1987. pp. 145–147. [DOI] [PubMed] [Google Scholar]
- 2.Kern J, Petrovečki M. i sur. Medical informatics/Medicinska informatika. Medicinska naklada Zagreb. 2009:179–196. [Google Scholar]
- 3.Zukanović V. Upravljački proces za razvoj zdravstva sa posebnim naglaskom na Zdravlje za sve”. Beograd: U: Menadžment u zdravstvu, Ramić H. ur. Stomatološki fakultet Univerziteta u Beogradu; 1991. pp. 9–19. [Google Scholar]
- 4.Masic I, Ridjanovic Z, Pandza H, Masic Z. Avicena. Sarajevo. Second. 2010. Medical Informatics; pp. 217–254. [Google Scholar]
- 5.Schwartz WB, Gorry GA, Kassirer JP, Essig A. Decision analysis and clinical judgment. Am J Med. 1973;55:459–472. doi: 10.1016/0002-9343(73)90203-9. [DOI] [PubMed] [Google Scholar]
- 6.Eddy DM. Clinical Politics and the uality of clinical practice. N Engl J Med. 1982;307:343–347. doi: 10.1056/NEJM198208053070604. [DOI] [PubMed] [Google Scholar]
- 7.Campbell EJM. The diagnostic mind. Vol. 1. Lancet; 1987. pp. 849–851. [Google Scholar]
- 8.Etzioni A. The logic of business decision making. Boston: Harvard Universi-ty, Office of the Uni versity Publisher; 1991. Humble decision making; pp. 41–45. [Google Scholar]
- 9.Einhorn HJ, Hogarth RM. The logic of business decision making. Boston: Harvard University, Office of the University Publisher; 1991. Decision making: going forward in reverse; pp. 47–51. [Google Scholar]
- 10.Simon HA. The new science of management decision. Harper Row, New York: 1960. [Google Scholar]
- 11.Burch JG, Strater FR, Jr. Information Systems: Theory and Practice. Santa Barbara: John Wiley Sons; 1974. pp. 52–59. [Google Scholar]
- 12.So HC., Jr Decision analysis: a basic clinical skill. N Engl J Med. 1987;316:271–272. doi: 10.1056/NEJM198701293160509. [DOI] [PubMed] [Google Scholar]
- 13.Bosk CL. Occupational rituals in patient management. N Engl J Med. 1980;303:71–76. doi: 10.1056/NEJM198007103030203. [DOI] [PubMed] [Google Scholar]
- 14.Mc Nutt RA, Selker HP. How did the acute ischemic heart disease predictive instrument reduce un necessary coronary care unit admissions. Med Decis Making. 1988;8:90–94. doi: 10.1177/0272989X8800800204. [DOI] [PubMed] [Google Scholar]
- 15.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211:453–458. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]
- 16.Nightingale SD. Risk preference and laboratory use. Med Decis Making. 1987;7:168–173. doi: 10.1177/0272989X8700700307. [DOI] [PubMed] [Google Scholar]
- 17.Duggan JM. Resource allocation and bioethics. Vol. 1. Lancet; 1989. pp. 772–773. [DOI] [PubMed] [Google Scholar]
- 18.Forrow L, Wartman SA, Brock DW. Impli-cations for risk factor intervention. Vol. 259. JAMA; 1988. Science ethics and the making of clinical decisions; pp. 3161–3167. [PubMed] [Google Scholar]
- 19.Blackhall LJ. Must we always use. CRP N Engl J Med. 1987;317:1281–1285. doi: 10.1056/NEJM198711123172009. [DOI] [PubMed] [Google Scholar]
- 20.Brock DW, Wartamn SA. When competent patients make irrational choices. N Engl J Med. 1990;322:1595–1599. doi: 10.1056/NEJM199005313222209. [DOI] [PubMed] [Google Scholar]
- 21.Danis M, Patrick DL, Southerland LI, Green ML. Patients and families pReferences for medical intensive care. Vol. 260. JAMA; 1988. pp. 797–802. [PubMed] [Google Scholar]
- 22.Sherlock R. Resonable men and sick human beings. Am J Med. 1986;80:2–4. doi: 10.1016/0002-9343(86)90040-9. [DOI] [PubMed] [Google Scholar]
- 23.Grant ES. A definition. Vol. 260. JAMA; 1988. Quality medical care; pp. 56–61. [PubMed] [Google Scholar]
- 24.Masic Z, Pandza H, Novo A, Jahic Dz, Masic F. Application of Models and Modeling in Biomedicine. Inter J Biomed Healthc. 2016;6(1):22–34. ijbh.2018.6.22-34. [Google Scholar]
- 25.Masic I, Ridjanovic Z, Pandza H, Masic Z. Medical Informatics. Second. Sarajevo: Avicena; 2010. pp. 185–216. [Google Scholar]
- 26.Ridjanović Z, Mašić I. Medical Decisions/Medicinsko odlučivanje. Sarajevo: Avicena; 1994. p. 301. [Google Scholar]
- 27.BaraUpotreba modela u programiranju kai Z. Menadžersko odluUpotreba modela u programiranju ivanje. Sarajevo: Svjetlost; 1991. pp. 23–30. [Google Scholar]
- 28.Cebul RD. Decision making research at the interface between descriptive and prescriptive studies. Med Decis Making. 1988;8:231–232. doi: 10.1177/0272989X8800800402. [DOI] [PubMed] [Google Scholar]
- 29.Cvjetanović B. Upotreba modela u programiranju zdravstvene zaštite. Mat Soc Med Iugoslavica. 1979;2:235–242. [Google Scholar]