Abstract
Background
Summary measures such as disability-adjusted life years (DALY) are becoming increasingly important for the standardized assessment of the burden of disease due to death and disability. The BURDEN 2020 pilot project was designed as an independent burden-of-disease study for Germany, which was based on nationwide data, but which also yielded regional estimates.
Methods
DALY is defined as the sum of years of life lost due to death (YLL) and years lived with disability (YLD). YLL is the difference between the age at death due to disease and the remaining life expectancy at this age, while YLD quantifies the number of years individuals have spent with health impairments. Data are derived mainly from causes of death statistics, population health surveys, and claims data from health insurers.
Results
In 2017, there were approximately 12 million DALY in Germany, or 14 584 DALY per 100 000 inhabitants. Conditions which caused the greatest number of DALY were coronary heart disease (2321 DALY), low back pain (1735 DALY), and lung cancer (1197 DALY). Headache and dementia accounted for a greater disease burden in women than in men, while lung cancer and alcohol use disorders accounted for a greater disease burden in men than in women. Pain disorders and alcohol use disorders were the leading causes of DALY among young adults of both sexes. The disease burden rose with age for some diseases, including cardiovascular diseases, dementia, and diabetes mellitus. For some diseases and conditions, the disease burden varied by geographical region.
Conclusion
The results indicate a need for age- and sex-specific prevention and for differing interventions according to geographic region. Burden of disease studies yield comprehensive population health surveillance data and are a useful aid to decision-making in health policy.
Epidemiological measures such as incidence, prevalence, and deaths are essential for monitoring population health. However, examining them in isolation cannot adequately assess the significance of various diseases. Assessment of the burden of disease in the general population is therefore becoming increasingly important in supporting health policy decision-making. Summary measures of population health integrate a variety of diseases as a cause of health impairment (morbidity) and death (mortality). The significance of the different diseases for population health can be measured by applying standardized rules (1, 2). Thus, the disability-adjusted life year (DALY) measures the total burden of disease comprising mortality (years of life lost due to death [YLL]) and morbidity (years lived with disability [YLD]) (3– 6). DALY are health gap measures which quantify deviations of the current population health from a defined norm. In contrast, health expectancy measures (for example, healthy life years) represent the remaining years of life spent in good health (7).
The metrics YLL, YLD and DALY date back to the Global Burden of Disease (GBD) study (4, 8, 9). This study estimates the burden of disease for global comparisons according to variables such as sex, age and country. Since the GBD study has only limited access to data at a national level and must therefore draw upon universal assumptions and extensive statistical methods, evaluation of the burden of disease has so far not been possible for Germany at the sub-national level. Yet decisions about health care require information below the federal level. So, regional burden of disease analyses are of considerable additional value for the assessment of population health because they provide information for guiding and prioritizing health care and prevention measures. Based on an improved data basis, the pilot project BURDEN 2020 (“The Burden of Disease in Germany at the National and Regional Level”) adapted the method used for measuring disease burden on the example of selected diseases and injuries with high public health relevance (ebox). The use of claims data from statutory health insurances and own health surveys enabled for the first time regional analyses of selected diseases. Based on this continuously available information, burden of disease analyses can become a permanent component of public health surveillance in Germany (10).
eBOX. BURDEN 2020 study.
The BURDEN 2020 study is a pilot project designed to adapt existing methods for calculating burden of disease for Germany (10). A national burden of disease study like BURDEN 2020 goes beyond comparative international systems such as the GBD (Global Burden of Disease) study: Data sources such as claims data from statutory health insurances, official statistics, and primary data collection are used for Germany that are known to be reliable on a nationwide and regional level (quality), whose strengths and limitations are known, can be regularly updated, and are considered reliable (acceptance). This builds up country-specific capacities in the field of burden of disease (competence), methodological decisions can be explained in a comprehensible way (transparency), and the results can be better communicated to national stakeholders (legitimacy). This creates an information system which can be expanded with complementary other components (flexibility).
In BURDEN 2020, complex modeling algorithms lie behind the three core indicators – years of life lost due to death (YLL), years lived with disability (YLD) and disability-adjusted life years (DALY) (17, 27, e1): Thus, ill-defined causes of death were redistributed, allowing to assign valid causes of death to all deceased persons in order to properly calculate the disease burden (12). Regional prevalences were estimated and, after adjusting for age and morbidity, extrapolated to the general population (19– 21). Specific severity distributions and disease durations are included in the calculations to measure the actual burden of disease in the population (13, 27). The results were adjusted for multimorbidity, and a concept was developed to reflect the various sources of statistical uncertainty (13). As a result, extensive use of the existing diverse data in Germany laid the foundation for a consistent information system on the burden of disease (www.daly.rki.de). This allows to prioritize diseases and injuries according to their relevance for public health, to identify the needs-based prevention and health care and enhance planning and evaluation of public health measures.
Method
The burden of disease concept quantifies in life years any deviation in population health from an “ideal” health status per reference year (eMethods section 1.1) (4). The mortality-related burden of disease (years of life lost due to death [YLL]) is calculated by multiplying the number of deaths with the standard remaining life expectancy at the age when death occurs. The methodology is described in detail elsewhere (11, 12). The morbidity-related burden of disease (years lived with disability [YLD]) provides a population-based quantification of years lived with health impairments. It is calculated from the prevalence of disease or injury, the distribution of the diseased population according to severity grades (severity distributions) and, for periodically occurring diseases, also the average duration of illness as well as severity-specific weights (disability weights) (eMethods section 1.1, [13]).
The initial assumption is that each diseased person lives one year with a disability per reporting year. The average duration of symptoms is also taken into account for episodic disabilities. Furthermore, the years lived with disability are converted to a unit of time equivalent to the YLL by applying disability weights (14, 15). Disability weights multiply each severity grade by a value between 0 (state of full health) and less than 1 (1 would be equivalent to death) (15, 16). A greater weight corresponds to a greater disability and results in a higher burden of disease (eMethods section 1.2). The DALY is the sum of YLL and YLD and is interpreted by the GBD study as years of healthy life lost (4).
The present analysis takes into account a selection of diseases and injuries (henceforth referred to as causes of burden of disease). Using the GBD four-level classification system (17), this selection includes at least one cause from the three main groups of causes of disease (level 1) of the GBD classification (etable 1):
eTable 1. Presentation of the analyzed causes of burden of disease within the hierarchy of levels (morbidity).
| Level 1 | Level 2 | Level 3 | Level 4 |
| Communicable, maternal, neonatal and nutritional diseases | Respiratory infections | Lower respiratory infections | → Lower respiratory infections |
| […] | |||
| […] | |||
| Non-communicable diseases | Cancer diseases | Colorectal cancer | → Colorectal cancer |
| Tracheal, bronchial and lung cancer | → Tracheal, bronchial and lung cancer | ||
| Breast cancer | → Breast cancer | ||
| Prostate cancer | → Prostate cancer | ||
| […] | |||
| Cardiovascular diseases | Ischemic heart disease | → Ischemic heart disease | |
| Stroke | ischemic stroke | ||
| intracerebral hemorrhage | |||
| subarachnoid hemorrhage | |||
| Hypertensive heart disease | → Hypertensive heart disease | ||
| […] | |||
| Chronic respiratory diseases | Chronic obstructive lung disease | → Chronic obstructive lung disease | |
| […] | |||
| Neurological disorders | Alzheimer’s disease and other dementias | → Alzheimer’s disease and other dementias | |
| Headache disorders | Migraine | ||
| Tension type headache | |||
| […] | |||
| Mental disorders | Depressive disorders | Major depression | |
| Dysthymia | |||
| Anxiety disorders | → Anxiety disorders | ||
| […] | |||
| Alcohol, drugs and other substances | Alcohol use disorders | → Alcohol use disorders | |
| […] | |||
| Diabetes and kidney diseases | Diabetes mellitus | Type 1 diabetes mellitus | |
| Type 2 diabetes mellitus | |||
| […] | |||
| Musculoskeletal disorders | Low back pain | → Low back pain | |
| Neck pain | → Neck pain | ||
| […] | |||
| […] | |||
| Injuries | Transport injuries | Road injuries | Pedestrian road injuries |
| Cyclist road injuries | |||
| Motorcyclist road injuries | |||
| Occupant road injuries | |||
| Other road injuries | |||
| Other transport accidents | → Other transport injuries | ||
| […] |
Source: Quelle: BURDEN 2020; our own presentation derived from the GBD study [27]; → Levels 3 and 4 are identical; […] indicates that further diseases/clinical entities are missing for complete representation of the respective group
communicable, maternal, neonatal, and nutritional diseases
non-communicable diseases
injuries.
These main groups are further subdivided at levels 2 to 4 into more specific causes of burden of disease. Thus, non-communicable diseases, for instance, include neurological disorders (level 2), which in turn include headache disorders at level 3. The latter distinguish between migraine and tension type headache at level 4. The selection for the present study was conducted at Level 3 (a total of 172 causes of burden of disease) and includes 19 of the quantitatively most important causes (around 53% of the burden of disease calculated for Germany for 2017 by the GBD study) (18) (etable 2).
eTable 2. Causes of burden of disease, selected for calculation and listed according to their relative proportion of all disability-adjusted life years (DALY) (level 3) based on the GBD study (2017) (Germany, both sexes).
| Rank | Cause of burden of disease (Level 3) | Relative proportion of total DALY for Germany*1 (in %) |
| 1 | Ischemic heart disease | 9.3 |
| 2 | Low back pain | 6.6 |
| 3 | Tracheal, bronchial and lung cancer | 4.0 |
| 4 | Stroke | 4.0 |
| 5 | Chronic obstructive lung disease | 3.9 |
| 6 | Alzheimer’s disease and other dementias | 3.6 |
| 7 | Diabetes mellitus | 2.9 |
| 8 | Headache disorders | 2.7 |
| 9 | Neck pain | 2.3 |
| 10 | Depressive disorders | 2.2 |
| 11 | Colorectal cancer | 2.1 |
| 12 | Anxiety disorders | 1.9 |
| 13 | Breast cancer | 1.7 |
| 14 | Alcohol use disorders | 1.3 |
| 15 | Road injuries*2 | 1.3 |
| 16 | Lower respiratory infections | 1.2 |
| 17 | Prostate cancer | 1.0 |
| 18 | Hypertensive heart disease | 1.0 |
| Total | 53.0 |
*1 The results fluctuate due to methodological adjustments during the GBD study and are also recalculated for earlier years with each wave of results. The exact values reported here are therefore no longer available in the information systems of the GBD study.
*2 The use of road traffic accident statistics also produced the group “Other transport injuries” (level 3) after operationalization of “Road injuries” (level 3). These are not explicitly listed here because they were originally not selected as an entity for the project.
The calculation of YLD is based on primary and secondary data sources, in particular age, sex and, in most cases, morbidity-adjusted claims data of patients insured by the local statutory health care fund AOK (etable 3) (13, 19– 22). Survey data on pain and addiction disorders (23– 25), road traffic accident statistics (26), and groundwork done within the GBD study were also used (27). For both YLL and YLD uncertainty concepts (95% uncertainty intervals [UI]) were developed and merged (13). YLD were adjusted for age-related multimorbidity to avoid overestimation of the total (13, 28). The results are reported as absolute values as well as crude rates and age-standardized rates per 100 000 population (pop) for the year 2017 (European standard population 2013 [29]).
eTable 3. Data sources and methodologies (morbidity component).
| Cause of burden of disease | Regional divisions* | Excluded age groups | Components | Data source | Year | Reference | Unit | Methodology |
| Lower respiratory infections | D, FS, SPR | none | Incidence | AOK claims data | 2017 | (19, 20) | Rate (cases per 100 000 person-years) | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | GBD study | 2017 | (27, e5) | Relative proportion of case rate | ||||
| Duration | GBD study | 2017 | (27, e5) | Days per year | ||||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Tracheal, bronchial and lung cancer | D, FS, SPR | <25 years (data limitation) | Prevalence | AOK claims data | 2017 | (19, 20) | 10-year prevalence | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | AOK claims data | 2017 | (19, 20) | Relative proportion of 10-year prevalence | Age and sex stratification | |||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Breast cancer | D, FS, SPR | <20 years (data limitation) | Prevalence | AOK claims data | 2017 | (19, 20) | 10-year-prevalence | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | AOK claims data | 2017 | (19, 20) | Relative proportion of 10-year prevalence | Age stratification (females only) | |||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Prostate cancer | D, FS, SPR | <40 years (data limitation) | Prevalence | AOK claims data | 2017 | (19, 20) | 10-year prevalence | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | AOK claims data | 2017 | (19, 20) | Relative proportion of 10-year prevalence | Age stratification (males only) | |||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Colorectal cancer | D, FS, SPR | <20 years (data limitation) | Prevalence | AOK claims data | 2017 | (19, 20) | 10-year prevalence | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | AOK claims data | 2017 | (19, 20) | Relative proportion of 10-year prevalence | Age and sex stratification | |||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Coronary heart disease | D, FS, SPR | Myocardial infarction <25 years, angina pectoris none, heart failure <25 years (expert opinion) | Prevalence | AOK claims data | 2017 | (19, 20) | 1-year prevalence; rate (cases per 100 000 person years) | Age, sex and morbidity-adjusted extrapolation (21); rate corresponds to myocardial infarctions as proportion of heart disease |
| Severity distribution | AOK claims data; GBD study | 2017 | (19, 20, 27) | Relative proportion of 1-year prevalence or 1-year rate | Age and sex stratification (heart failure and myocardial infarction); angina pectoris taken from GBD study | |||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Stroke | D, FS, SPR | none | Prevalence | AOK claims data | 2017 | (19, 20) | 10-year prevalence | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | GBD study | 2017 | (27, e6) | Relative proportion of 10-year prevalence | ||||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Hypertensive heart disease | D, FS, SPR | <25 years (expert opinion) | Prevalence | AOK claims data | 2017 | (19, 20) | 1-year prevalence | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | AOK claims data | 2017 | (19, 20) | Relative proportion of 1-year prevalence | Age and sex stratification | |||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Chronic obstructive lung disease | D, FS, SPR | <35 years (expert opinion) | Prevalence | AOK claims data | 2017 | (19, 20) | 1-year prevalence | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | GBD study | 2013 | (27, e7) | Relative proportion of 1-year prevalence | ||||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Alzheimer’s disease and other dementia | D, FS, SPR | <40 years (expert opinion) | Prevalence | AOK claims data | 2017 | (19, 20) | 1-year prevalence | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | GBD study | 2017 | (27, e6) | Relative proportion of 1-year prevalence | ||||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Alcohol use disorders | D | <18 and >64 years (survey-related restriction) | Prevalence | Epidemiological survey of substance abuse | 2018 | (25) | 1-year prevalence | Extrapolation considering sampling approach |
| Severity distribution | GBD study | 2017 | (27, e6) | Relative proportion of 1-year prevalence | ||||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Anxiety disorders | D, FS, SPR | none | Prevalence | AOK claims data | 2017 | (19, 20) | 1-year prevalence | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | GBD study | 2017 | (27, e6) | Relative proportion of 1-year prevalence | ||||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Depressive disorders | D, FS, SPR | Major depression and dysthymia < 15 years (expert opinion) | Prevalence | AOK claims data | 2017 | (19, 20) | 1-year prevalence | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | AOK claims data, GBD study | 2017 | (19, 20, 27) | Relative proportion of 1-year prevalence | Age and sex stratification (major depression: AOK claims data; dysthymia: GBD study) | |||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Duration | RKI study data | 2009–2012 | (36) | Days per year | Extrapolation considering sampling approach (major depression) | |||
| Diabetes mellitus | D, FS, SPR | Type 1 diabetes none, Type 2 diabetes <10 years (expert opinion) | Prevalence | AOK claims data | 2017 | (19, 20) | 1-year prevalence | Age, sex and morbidity-adjusted extrapolation (21) |
| Severity distribution | AOK claims data | 2017 | (19, 20) | Relative proportion of 1-year prevalence | Age and sex stratification | |||
| Disability weight | GBD study | 2017 | (27, e8, e9) | Weight | ||||
| Low back pain | D | <18 years (restriction due to telephone survey) | Prevalence | RKI survey data | 2019/2020 | (23) | 1-year prevalence | Extrapolation considering sampling approach |
| Severity distribution | RKI survey data | 2019/2020 | (23) | Relative proportion of 1-year prevalence | Extrapolation considering sampling approach | |||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Duration | RKI survey data | 2019/2020 | (23) | Days per year | Extrapolation considering sampling approach | |||
| Neck pain | D | <18 years (restriction due to telephone survey) | Prevalence | RKI survey data | 2019/2020 | (23) | 1-year prevalence | Extrapolation considering sampling approach |
| Severity distribution | RKI survey data | 2019/2020 | (23) | Relative proportion of 1-year prevalence | Extrapolation considering sampling approach | |||
| Disability weight | GBD study | 2017 | (27) | Weight | ||||
| Duration | RKI survey data | 2019/2020 | (23) | Days per year | Extrapolation considering sampling approach | |||
| Road injuries | D, FS, SPR | none | Prevalence | Road injury statistics | 2017 | (26, e10, e11) | 1-year prevalence | Number of transport injuries corrected for the proportion of accidents not recorded by the police by using survey data (see [13] for details) |
| Severity distribution | GBD study | 2017 | (27) | Relative proportion of 1-year prevalence | Proportion of injuries (or groups of injuries) within the respective road traffic accident; use of the Global Burden of Disease results (see [13] for details) | |||
| Disability weight | GBD study | 2017 | (27) | Weight | Use of average disability weights (see [13] for details) | |||
| Headache disorders | D | <18 years (restriction due to telephone survey) | Prevalence | RKI survey data | 2019/2020 | (24) | 1-year prevalence | Extrapolation considering sampling approach |
| Severity distribution | RKI survey data | 2019/2020 | (24) | Proportion of days per year with symptoms of all days of the year | Extrapolation considering sampling approach | |||
| Disability weight | GBD study | 2017 | (27) | Weight |
* D, Germany; FS, federal states; SPR, spatial planning regions
Results
The selected causes of burden of disease in the German population in 2017 produced 12.1 million DALY (UI: 11.9–13.1) (30). Women account for 6.0 million DALY (UI: 5.9–6.8), about as much burden of disease as men with 6.1 million DALY (UI: 6.0–6.6).
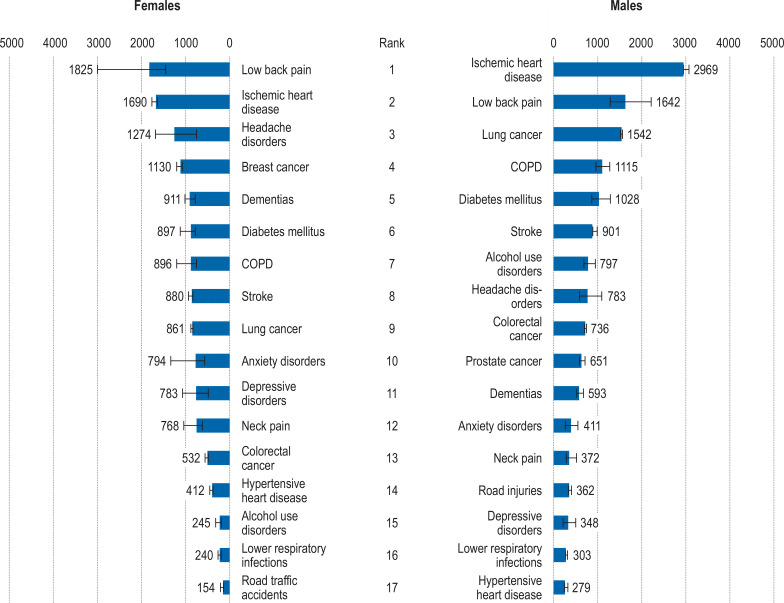
Without standardizing for age, this translates into a relative 14 584 DALY per 100 000 population, with a lower rate for women (14 303 DALY) than for men (14 872 DALY). When comparing all examined causes of burden of disease, ischemic heart disease (IHD) had the highest overall rate (2321 DALY), followed by low back pain (1735 DALY). At ranks 3 to 5 follow tracheal, bronchial, and lung cancer (henceforth referred to as “lung cancer” for short) with a rate of 1197 DALY, headache disorders with 1032 DALY, and chronic obstructive pulmonary disease (COPD) with 1004 DALY. Gender comparisons show clear differences with regard to the respective causes of burden of disease (figure 1). IHD is ranked first for men (2969 DALY) and second for women with 1690 DALY after low back pain (1825 DALY). Furthermore, ranks 3 to 5 for women are occupied by headache disorders (1274 DALY), breast cancer (1130 DALY), and Alzheimer’s disease and other dementias (henceforth “dementias” for short) (911 DALY). In men, on the other hand, lung cancer (1542 DALY), COPD (1115 DALY), and diabetes mellitus (1028 DALY) are ranked 3 to 5. Alcohol use disorders produce more than three times as much burden of disease in males than in females. In contrast, women experience more than twice as much burden of disease from depressive disorders.
Figure 1.
Total burden of disease (DALY per 100 000 population [pop]) for selected causes of burden of disease by sex (Level 3, Germany), error bars correspond to the 95% UI; source: BURDEN 2020; YLL: cause of death statistics 2017 (31), Federal Statistical Office of Germany 2018 (32); YLD: eTable 3; our own calculations; only 17 ranks each are presented here since no DALY were calculated for prostate cancer in women and breast cancer in men, and the residual category “Other transport injuries” is not shown (eTable 1, eTable 2); data limitations must be taken into account when making a direct comparison of DALY (etable 3); COPD, chronic obstructive pulmonary disease; DALY, disability-adjusted life years; RI, road injuries; YLL, years of life lost due to death; YLD, years lived with disability
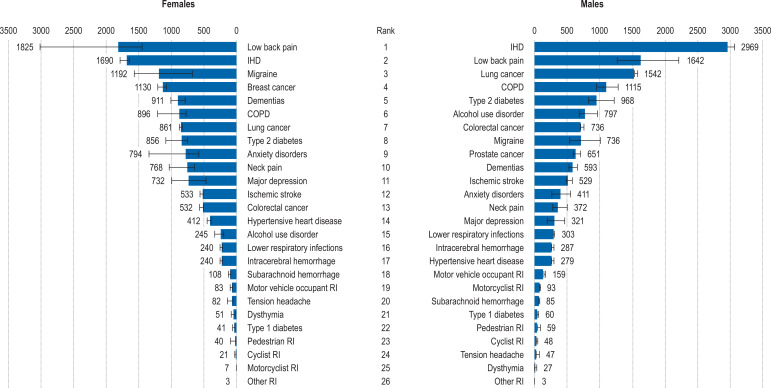
A differentiated breakdown of the burden of disease at level 4 (efigure 1) demonstrates hardly any significant shifts at the upper ranks in comparison with level 3. It is evident, however, that certain level-4 causes are responsible for the degree of level-3 burden of disease (etable 4). Thus, type 2 diabetes (level 4) is responsible for 95% of the DALY of diabetes mellitus (Level 3), migraine accounts for 94% of the DALY of headache disorders, and major depression for 93% of the burden of disease due to depressive disorders.
eFigure 1.
Total burden of disease (DALY per 100 000 population [pop]) of the selected causes of burden of disease by sex (level 4, Germany), error bars correspond to the 95% UI
Source: BURDEN 2020; YLL: Cause of death statistics 2017 (31), Federal Statistical Office of Germany 2018 (32); YLD: (etable 3); our own calculations; only 26 ranks each are presented here because no DALY were calculated for prostate cancer in women and breast cancer in men, and the residual category “Other transport injuries” is not shown (eTable 1, eTable 2); data limitations must be taken into account when making a direct comparison of DALY (etable 3); COPD, chronic obstructive pulmonary disease; DALY, disability-adjusted life years; RI, Road injuries; YLL, years of life lost due to death; YLD, years lived with disability
eTable 4. Total burden of disease (disability-adjusted life years [DALY] absolute numbers and relative contributions) for the selected causes of burden of disease (levels 3 and 4, Germany, both sexes).
| Cause of burden of disease (levels 3 and 4) | DALY | Proportion of level 3 to 4 (in percent) | ||||
| DALY | UI_lb | UI_ub | Proportion | UI_lb | UI_ub | |
| Lower respiratory infections | 224 306 | 222 505 | 238 565 | – | – | – |
| Tracheal, bronchial and lung cancer | 989 188 | 981 443 | 1 012 245 | – | – | – |
| Breast cancer | 473 366 | 454 905 | 527 690 | – | – | – |
| Prostate cancer | 265 264 | 246 455 | 300 985 | – | – | – |
| Colorectal cancer | 523 155 | 512 617 | 550 669 | – | – | – |
| Ischemic heart disease | 1 918 193 | 1 897 796 | 2 033 859 | – | – | – |
| Stroke | 735 883 | 727 508 | 799 155 | – | – | – |
| – subarachnoid hemorrhage | 79 902 | 78 564 | 93 831 | 10.9 | 10.3 | 12.3 |
| – intracerebral hemorrhage | 217 344 | 211 666 | 234 109 | 29.5 | 27.6 | 30.8 |
| – ischemic stroke | 438 638 | 425 609 | 484 579 | 59.6 | 57.6 | 61.6 |
| Hypertensive heart disease | 286 381 | 266 860 | 331 850 | – | – | – |
| Chronic obstructive lung disease | 829 714 | 696 238 | 965 784 | – | – | – |
| Alzheimer’s disease and other dementias | 623 515 | 539 034 | 711 638 | – | – | – |
| Alcohol use disorders | 427 545 | 366 548 | 501 661 | – | – | – |
| Depressive disorders | 469 767 | 391 219 | 607 266 | – | – | – |
| – dysthymia | 32 399 | 18 940 | 61 783 | 6.9 | 3.7 | 12.8 |
| – major depression | 437 369 | 350 627 | 562 627 | 93.1 | 87.2 | 96.3 |
| Anxiety disorders | 500 130 | 366 541 | 702 047 | – | – | – |
| Diabetes mellitus | 794 940 | 665 042 | 1 050 903 | – | – | – |
| – Type 2 diabetes mellitus | 753 404 | 633 899 | 991 637 | 94.8 | 92.8 | 95.9 |
| – Type 1 diabetes mellitus | 41 536 | 37 759 | 53 284 | 5.2 | 4.1 | 7.2 |
| Low back pain | 1 434 132 | 1 117 225 | 1 815 326 | – | – | – |
| Neck pain | 473 413 | 383 336 | 681 440 | – | – | – |
| Road injuries | 212 245 | 208 370 | 263 745 | |||
| – pedestrian road injury | 40 967 | 23 628 | 70 115 | 19.3 | 10.7 | 28.0 |
| – cyclist road injury | 28 518 | 25 406 | 40 668 | 13.4 | 11.1 | 17.7 |
| – motorcyclist road injury | 40 981 | 40 376 | 45 855 | 19.3 | 16.4 | 21.2 |
| – occupant road injury | 99 393 | 95 063 | 113 043 | 46.8 | 39.8 | 50.7 |
| – other road injury | 2387 | 1999 | 7353 | 1.1 | 0.9 | 3.2 |
| Other transport injuries | 16 461 | 15 485 | 26 584 | – | – | – |
| Headache disorders | 853 028 | 666 889 | 1 104 548 | – | – | – |
| – tension headache | 799 418 | 601 368 | 1 024 549 | 93.7 | 87.7 | 94.8 |
| – migraine | 53 610 | 44 542 | 98 706 | 6.3 | 5.2 | 12.3 |
ub, upper bound; lb, lower bound; UI, 95% uncertainty interval
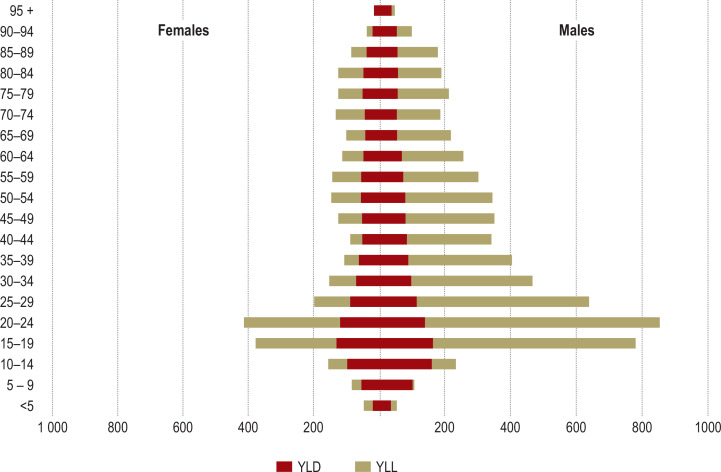
In relative terms, the burden of disease increases with age overall and for both sexes, although ranking and, in turn, the importance of the selected causes of burden of disease vary with age (Table, eTable 5). Headache disorders, low back pain, road injuries, alcohol use disorders, and anxiety disorders lead the DALY rankings in younger adulthood. Cardiovascular diseases, stroke, dementias, diabetes mellitus, and COPD dominate with advancing age (eTable 5, [30]). An age-related decrease of DALY rates is evident for lung cancer, alcohol use disorders, and headache disorders.
Table. Total burden of disease (DALY per 100 000 population) of the selected causes of burden of disease with increasing age (Level 3, Germany, both sexes).
| Total | 20 – 24 | 25 – 29 | 30 – 34 | 35 – 39 | 40 – 44 | 45 – 49 | 50 – 54 | 55 – 59 | 60 – 64 | 65 – 69 | 70 – 74 | 75 – 79 | 80 – 84 | 85 – 89 | 90 – 94 | 95 + |
| Lower respiratory infections | 29 | 23 | 31 | 36 | 33 | 67 | 104 | 166 | 265 | 359 | 581 | 836 | 1435 | 2318 | 3297 | 4073 |
| COPD | 99 | 180 | 336 | 657 | 1199 | 1932 | 2575 | 3226 | 3274 | 3668 | 4085 | 4106 | 3596 | |||
| Lung cancer | 5 | 19 | 93 | 250 | 588 | 1152 | 2277 | 3241 | 3740 | 3861 | 3017 | 2290 | 1639 | 996 | 478 | |
| Breast cancer | 2 | 44 | 165 | 304 | 436 | 591 | 731 | 837 | 961 | 1179 | 1302 | 1344 | 1469 | 1460 | 1597 | 1654 |
| Prostate cancer | 1 | 9 | 72 | 177 | 421 | 711 | 1113 | 1538 | 1717 | 1882 | 1485 | 1001 | ||||
| Bowel cancer | 4 | 24 | 90 | 112 | 196 | 336 | 539 | 792 | 1111 | 1459 | 1772 | 1969 | 2232 | 2470 | 2557 | 2142 |
| IHD | 43 | 92 | 224 | 485 | 854 | 1350 | 2138 | 3092 | 4215 | 5406 | 7367 | 11 162 | 16 308 | 21 215 | 24 962 | |
| Stroke | 31 | 40 | 71 | 123 | 178 | 327 | 430 | 658 | 935 | 1396 | 2128 | 3117 | 4762 | 6633 | 8294 | 8705 |
| Hypertensive heart disease | 1 | 2 | 3 | 25 | 39 | 76 | 126 | 245 | 370 | 593 | 1044 | 2087 | 3925 | 6667 | 10 115 | |
| Diabetes mellitus | 33 | 51 | 84 | 129 | 251 | 414 | 668 | 981 | 1504 | 2041 | 2598 | 3210 | 4198 | 4793 | 4868 | 4436 |
| Dementias | 16 | 20 | 49 | 108 | 250 | 521 | 1 273 | 2 646 | 5 537 | 9 823 | 14 075 | 17 795 | ||||
| Depressive disorders | 248 | 303 | 378 | 486 | 618 | 657 | 762 | 832 | 895 | 910 | 889 | 967 | 1038 | 1023 | 1067 | 1091 |
| Anxiety disorders | 402 | 468 | 544 | 601 | 671 | 735 | 815 | 846 | 831 | 815 | 777 | 736 | 705 | 654 | 603 | 536 |
| Alcohol use disorders | 959 | 740 | 679 | 524 | 584 | 619 | 746 | 690 | 671 | 395 | 234 | 161 | 110 | 48 | 25 | 6 |
| Low back pain | 1397 | 1674 | 1635 | 1758 | 1754 | 2447 | 2318 | 2084 | 2217 | 2645 | 2863 | 2539 | 1770 | 1770 | 1688 | 1610 |
| Headache disorders | 1607 | 1967 | 2042 | 1565 | 1532 | 1515 | 1197 | 995 | 839 | 560 | 425 | 340 | 290 | 273 | 274 | 232 |
| Neck pain | 346 | 397 | 592 | 525 | 589 | 914 | 894 | 771 | 720 | 914 | 748 | 839 | 685 | 613 | 534 | 440 |
| Road injuries | 645 | 429 | 316 | 258 | 218 | 240 | 248 | 224 | 185 | 156 | 159 | 164 | 153 | 121 | 56 | 23 |
| Legend | <1340 | 1340 <3900 | 3900 <9000 | 9000 <17 000 | ≥ 17 000 | |||||||||||
Source: BURDEN 2020; YLL: Cause of death statistics 2017 (31), Federal Statistical Office of Germany 2018 (32); YLD: eTable 3; our own calculations; due to data limitations, a comparison of the causes of burden of disease is only presented from the age group of 20 year-olds onwards (etable 3); both grouping and the resulting color scheme were created using the natural breaks method (33); COPD, chronic obstructive pulmonary disease; DALY, disability-adjusted life years; IHD, ischemic heart disease
eTable 5. Total burden of disease (DALY per 100 000 population [pop]) of the selected causes of burden of disease with increasing age and according to sex (level 3, Germany).
| a) Females | ||||||||||||||||
| 20–24 | 25–29 | 30–34 | 35–39 | 40–44 | 45–49 | 50–54 | 55–59 | 60–64 | 65–69 | 70–74 | 75–79 | 80–84 | 85–89 | 90–94 | 95 + | |
| Lower respiratory infections | 35 | 29 | 28 | 25 | 23 | 37 | 71 | 126 | 190 | 223 | 392 | 612 | 1097 | 1890 | 2849 | 3593 |
| COPD | 101 | 167 | 308 | 583 | 1038 | 1677 | 2089 | 2574 | 2533 | 2917 | 3290 | 3460 | 3236 | |||
| Lung cancer | 8 | 19 | 73 | 224 | 513 | 887 | 1716 | 2344 | 2591 | 2547 | 1786 | 1309 | 938 | 599 | 330 | |
| Breast cancer | 3 | 92 | 339 | 615 | 877 | 1194 | 1477 | 1670 | 1877 | 2261 | 2439 | 2420 | 2489 | 2246 | 2149 | 2030 |
| Prostate cancer | ||||||||||||||||
| Bowel cancer | 6 | 33 | 53 | 110 | 186 | 311 | 447 | 573 | 751 | 1000 | 1284 | 1513 | 1836 | 2188 | 2368 | 2036 |
| IHD | 37 | 43 | 99 | 172 | 316 | 490 | 765 | 1307 | 2048 | 3127 | 4813 | 8412 | 13 646 | 19 320 | 23 749 | |
| Stroke | 36 | 62 | 78 | 121 | 179 | 309 | 353 | 501 | 635 | 977 | 1625 | 2635 | 4390 | 6471 | 8342 | 8829 |
| Hypertensive heart disease | 1 | 2 | 4 | 20 | 44 | 84 | 171 | 257 | 507 | 1009 | 2168 | 4245 | 7200 | 10 911 | ||
| Diabetes | 34 | 54 | 81 | 126 | 202 | 326 | 492 | 721 | 1107 | 1558 | 2109 | 2793 | 3922 | 4682 | 4868 | 4485 |
| Dementias | 16 | 19 | 48 | 107 | 212 | 458 | 1177 | 2508 | 5518 | 9963 | 14 523 | 18 509 | ||||
| Depressive disorders | 344 | 417 | 521 | 662 | 847 | 901 | 1035 | 1107 | 1192 | 1229 | 1186 | 1283 | 1346 | 1258 | 1231 | 1204 |
| Anxiety disorders | 520 | 618 | 716 | 798 | 879 | 968 | 1098 | 1123 | 1089 | 1087 | 1037 | 964 | 895 | 779 | 670 | 571 |
| Alcohol use disorders | 546 | 418 | 270 | 143 | 223 | 195 | 379 | 292 | 395 | 170 | 116 | 81 | 49 | 29 | 25 | 7 |
| Low back pain | 1371 | 1676 | 1618 | 1728 | 1720 | 2574 | 2444 | 2196 | 2333 | 2850 | 3067 | 2740 | 1924 | 1893 | 1764 | 1649 |
| Headache disorders | 2075 | 2646 | 2580 | 2025 | 1932 | 1961 | 1517 | 1316 | 982 | 612 | 455 | 355 | 289 | 266 | 265 | 226 |
| Neck pain | 483 | 544 | 899 | 801 | 887 | 1156 | 1135 | 994 | 930 | 1171 | 967 | 1 064 | 859 | 722 | 597 | 473 |
| Road injuries | 415 | 204 | 157 | 112 | 94 | 130 | 150 | 148 | 118 | 103 | 137 | 128 | 129 | 91 | 43 | 18 |
| b) Males | ||||||||||||||||
| 20–24 | 25–29 | 30–34 | 35–39 | 40–44 | 45–49 | 50–54 | 55–59 | 60–64 | 65–69 | 70–74 | 75–79 | 80–84 | 85–89 | 90–94 | 95 + | |
| Lower respiratory infections | 24 | 17 | 33 | 46 | 43 | 97 | 136 | 206 | 343 | 508 | 796 | 1117 | 1922 | 3115 | 4594 | 6186 |
| COPD | 97 | 192 | 363 | 730 | 1360 | 2198 | 3104 | 3974 | 4201 | 4750 | 5562 | 5976 | 5181 | |||
| Lung cancer | 2 | 19 | 113 | 276 | 662 | 1412 | 2840 | 4182 | 4993 | 5365 | 4556 | 3704 | 2942 | 2145 | 1131 | |
| Breast cancer | ||||||||||||||||
| Prostate cancer | 1 | 17 | 143 | 355 | 862 | 1486 | 2386 | 3462 | 4191 | 5379 | 5782 | 5409 | ||||
| Bowel cancer | 2 | 15 | 124 | 114 | 207 | 359 | 629 | 1012 | 1487 | 1958 | 2330 | 2538 | 2804 | 2995 | 3103 | 2608 |
| IHD | 49 | 140 | 345 | 794 | 1381 | 2194 | 3515 | 4964 | 6575 | 8014 | 10 559 | 15 125 | 21 257 | 26 700 | 30 304 | |
| Stroke | 26 | 19 | 65 | 125 | 177 | 345 | 506 | 816 | 1249 | 1853 | 2702 | 3718 | 5297 | 6934 | 8156 | 8163 |
| Hypertensive heart disease | 1 | 2 | 5 | 46 | 58 | 107 | 168 | 322 | 494 | 692 | 1087 | 1969 | 3329 | 5124 | 6613 | |
| Diabetes | 31 | 49 | 88 | 133 | 299 | 500 | 841 | 1242 | 1919 | 2568 | 3157 | 3732 | 4595 | 4998 | 4870 | 4221 |
| Dementias | 17 | 22 | 51 | 110 | 289 | 590 | 1382 | 2817 | 5564 | 9564 | 12 776 | 14 649 | ||||
| Depressive disorders | 161 | 197 | 243 | 315 | 393 | 417 | 494 | 555 | 585 | 563 | 550 | 571 | 593 | 586 | 594 | 594 |
| Anxiety disorders | 295 | 328 | 382 | 409 | 465 | 507 | 537 | 567 | 560 | 520 | 481 | 452 | 431 | 423 | 409 | 379 |
| Alcohol use disorders | 1334 | 1038 | 1068 | 897 | 940 | 1036 | 1106 | 1090 | 961 | 640 | 369 | 261 | 197 | 83 | 26 | 2 |
| Low back pain | 1421 | 1673 | 1650 | 1788 | 1788 | 2322 | 2195 | 1970 | 2095 | 2421 | 2629 | 2287 | 1549 | 1541 | 1468 | 1439 |
| Headache disorders | 1181 | 1338 | 1531 | 1116 | 1138 | 1079 | 882 | 673 | 689 | 504 | 391 | 321 | 292 | 288 | 298 | 256 |
| Neck pain | 222 | 261 | 301 | 255 | 295 | 676 | 657 | 546 | 500 | 633 | 497 | 558 | 433 | 409 | 350 | 296 |
| Road injuries | 855 | 638 | 467 | 401 | 340 | 347 | 343 | 300 | 255 | 214 | 185 | 208 | 187 | 177 | 95 | 44 |
| Legende | <1340 | 1340 <3900 | 3900 <9000 | 9000 <17 000 | ≥17 000 | |||||||||||
Source: BURDEN 2020; YLL: Cause of death statistics 2017 (31), Federal Statistical Office of Germany 2018 (32); YLD: eTable 3; own calculations; due to data limitations, a comparison of the causes of burden of disease is only presented from the age group of 20 year-olds onwards (etable 3); both grouping and the resulting color scheme were created using the natural breaks method (33); COPD, chronic obstructive pulmonary disease; DALY, disability-adjusted life years; IHD, ischemic heart disease
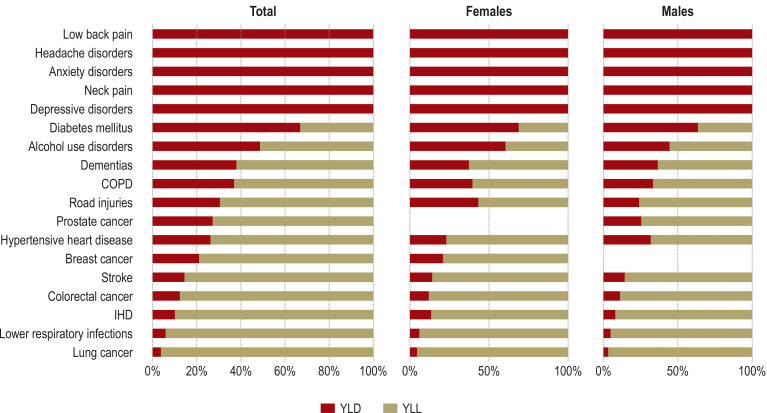
The disease-specific significance of mortality and morbidity for population health is reflected in the relative contribution of YLL and YLD to DALY. Whereas the burden of disease for pain and mental disorders is entirely attributable to morbidity, the relative contribution of mortality for the other causes of burden of disease varies (figure 2). For instance, the proportion of burden of disease due to death (YLL) is 34% for diabetes mellitus and 97% for lung cancer. The proportions differ only slightly between the sexes (with the exception of road injuries and alcohol use disorders, for example). With increasing age, the relative contribution of mortality to DALY also increases for most causes of burden of disease (30).
Figure 2.
Relative contribution of YLL and YLD to the total burden of disease (absolute DALY) for the selected causes of burden of disease (level 3, Germany, both sexes)
Source: BURDEN 2020; YLL: Cause of death statistics 2017 (31), Federal Statistical Office of Germany 2018 (32); YLD: eTable 3; own calculations; the residual category “Other transport injuries” is excluded (eTable 1, eTable 2); COPD, chronic obstructive pulmonary disease; DALY, disability-adjusted life years; IHD, coronary heart disease; YLL, years of life lost due to death; YLD, years lived with disability
An example for a striking gender difference can be given through the DALY rates for road injuries. Although road injuries are responsible for the greatest burden of disease for both sexes for the ages between 15 and 34 years, the rate for males is almost 2.4 times higher (362 versus 154 DALY per 100 000 population) (figure 1). With increasing age, more DALY resulting from road injuries are evident in men than in women for almost all age groups. This is mainly due to fatal road injuries (YLL), while the share of YLD is similar in both sexes (efigure 2).
eFigure 2.
Burden of disease (DALY per 100 000 population by YLL and YLD) for road injuries with increasing age and according to sex (level 3, Germany) Source: BURDEN 2020; YLL: Cause of death statistics 2017 (31), Federal Statistical Office of Germany 2018 (32); YLD: eTable 3; our own calculations; DALY, disability-adjusted life years; YLL, years of life lost due to death; YLD, years lived with disability
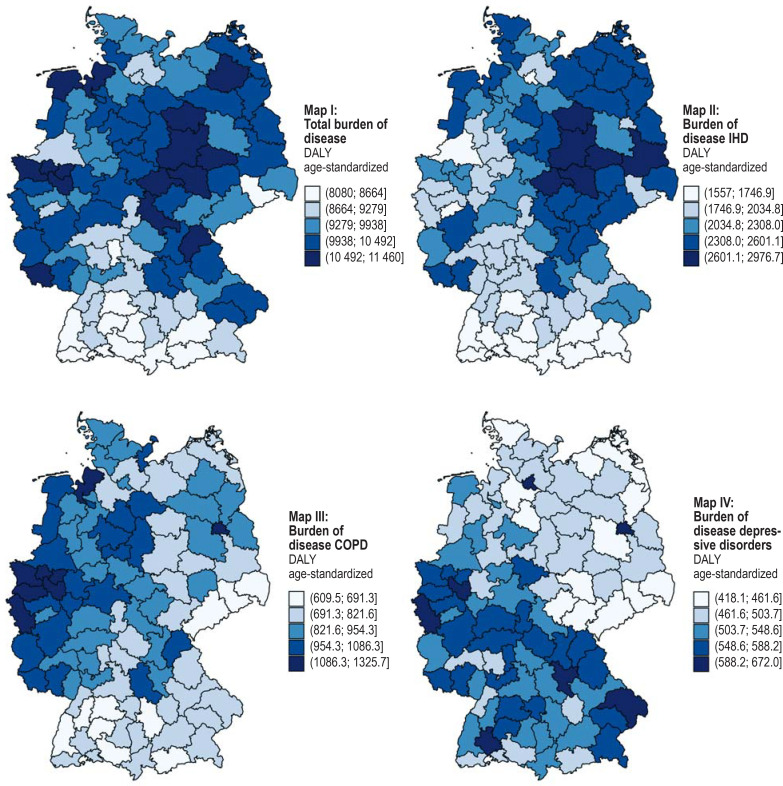
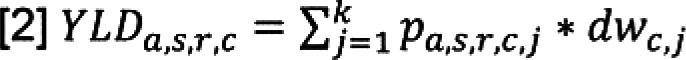
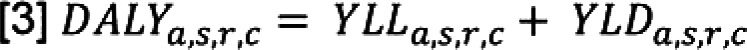
Sub-national differences are evident at the level of the 96 spatial planning regions (abbreviated to SPR), both in individual causes of burden of disease (30) and in the total of all DALY calculated so far (age-standardized per 100 000 population) (Figure 3, Map I). Overall, the regions Emscher-Lippe (North Rhine-Westphalia) and Bremerhaven have the highest burden of disease, relatively speaking, while the SPRs Munich and South Upper Rhine (Baden-Wurttemberg) have the lowest (30). Furthermore, similar sub-national patterns in the distribution of DALY emerge for certain causes of burden of disease. Higher DALY values are evident for IHD (Figure 3, Map II) in the SPRs in eastern Germany, which is exemplary for many cardiovascular diseases. On the other hand, the burden of disease for COPD (Figure 3, Map III) is highest particularly in the SPRs in western Germany and Berlin. This is similar for lung cancer. A clear difference is evident between the northern and southern SPRs for depressive disorders due to a, relatively speaking, smaller burden in northern Germany, with Berlin and Hamburg being exceptions (Figure 3, Map IV).
Figure 3.
Total burden of disease (age-standardized DALY per 100 000 population) at the spatial planning regions level (level 3, both sexes) for the sum of all causes of burden of disease (Map I), and for IHD (Map II), COPD (Map III) and depressive disorders (Map IV); range in brackets
Source: BURDEN 2020; YLL: Cause of death statistics 2017 (31), Federal Statistical Office of Germany 2018 (32); YLD: eTable 3; our own calculations; spatial planning regions, see Federal Institute for Research on Building, Urban Affairs and Spatial Development (BBSR) (34); Map I total burden of disease. Excluded from Map I are pain disorders and alcohol use disorders due to the lack of spatial data resolution (eTable); COPD, chronic obstructive pulmonary disease; DALY, disability-adjusted life years; IHD, ischemic heart disease; YLL, years of life lost due to death; YLD, years lived with disability
Discussion
The present analysis provides an overview of the burden of disease caused by disability and death in Germany for 19 of the most important causes of burden of disease for the year 2017. The advantage of looking at burden of disease as opposed to isolated information on deaths and disease prevalence is that the impact of disease (YLD) and death (YLL) on population health can be compared using a standardized summary measure. The analysis was carried out using a uniform and transparent methodology and an improved, more complete, and sub-nationally differentiated database as compared with the GBD study. Although a comparison of the results with the findings of the GBD study for the year 2017 (17, 18) is only possible to a limited degree, on the whole it does show many matches for Germany. The causes of the highest burden of disease include
IHD
low back pain
lung cancer
headache disorders
COPD
diabetes mellitus.
Gender differences were particularly apparent in the other ranks. In females, breast cancer contributes significantly to the burden of disease, while dementias also ranks highly. In males, the burden of disease from alcohol use disorders and from road injuries is higher.
Given the high level of detail of the results, it is possible to identify which single causes of burden of disease (level 4) account for the largest proportion of disease-specific DALY (level 3), for example type 2 diabetes within diabetes mellitus and migraine within headache disorders. Furthermore, the results show that the significance of certain causes of burden of disease varies with increasing age. Whereas headache disorders and alcohol use disorders lead the DALY rankings for both sexes in younger adulthood, the burden of cardiovascular diseases and dementias rises with increasing age. The comparison of morbidity-related and mortality-related burden of disease highlights the different needs for action. Thus, morbidity-related burden of disease from mostly chronic, but rarely fatal illnesses such as pain disorders and mental disorders can be reduced if sequelae and severe forms of the disease are avoided. The high proportion of mortality-related burden of disease, for example due to cancer or cardiovascular disorders, indicates a high primary need for prevention (35) and the necessity to increase survival times of those affected by providing suitable forms of treatment.
In detail, males and females differ in their share of burden of disease due to death or disability. Whereas the mortality rate due to hypertensive heart disease is higher in women than in men, the opposite applies for alcohol use disorders: Here, alcohol-related mortality is significantly higher in men. Patterns for cardiovascular diseases, COPD, and depressive disorders, amongst others, become evident when the results are differentiated down to a sub-national level. On the one hand, these findings raise questions about possible regional care needs. On the other hand, they help to identify other fields of action which should be further substantiated by sub-national analyses of environmental, behavioral, relational as well as metabolic risk factors (35).
Limitations
Fundamental limitations arise because important illnesses with a high burden of disease (for example, chronic kidney diseases or liver cirrhosis [18]) were initially not considered in the pilot project, resulting in a relevant, but nevertheless still incomplete picture for assessing burden of disease. Furthermore, a large variety of data bases was used because, whenever possible, data sources of high validity and with high spatial resolution were to be used for each of the causes of burden of disease. Whereas claims data are suitable for capturing cases reliably associated with the utilization of the health care system (for example, severe myocardial infarction), it was necessary to rely on survey data for pain disorders. Therefore, specific limitations need to be taken into consideration ([11, 12, 19, 23, 24, 36]; eMethods section 2.1). The biases associated with the respective data sources are counteracted by compensation mechanisms such as morbidity-adjusting extrapolation procedures for the claims data (21). The results based on claims data were checked for consistency as far as possible by using external data sources (see eMethods section 2.1 for a detailed discussion). Furthermore, it was not possible in the course of the project to conduct prevalence estimates based on the survey data for children and adolescents nor at a sub-national level, which resulted in limitations when making comparisons between age groups and between sub-national regions. Suitable statistical methods to close these data gaps, including the use of sub-national estimation methods (37), are currently being tested. With regard to severity distributions, it was necessary for some of the diseases to resort to preliminary work from the GBD study which draws on mainly global, i.e., non-country specific and temporally invariant distributions (see eMethods section 2.2 for methodological critique) (38). Non-country specific disability weights were fully adopted from the GBD study (39) (see eMethods section 2.2 for methodical criticism).
Conclusion
All results of the BURDEN 2020 project are entered into a health information system (www.daly.rki.de). They therefore represent an important element of public health surveillance at the Robert Koch Institute. The epidemiological measures based on claims data, such as prevalence, for example, are also readily available according to age, sex, and region (www.krankheitslage-deutschland.de). The BURDEN 2020 project is therefore useful to inform decision-making processes in health policy, such as the implementation of federal framework recommendations according to the German prevention law or regional morbidity-oriented planning. It can also be extended to include further diseases and may be supplemented by time series, forecasts, and other assessments (health impact assessments).
Supplementary Material
eMethods
1. Calculation approach and additional information about the YLD indicator
1.1 Calculation approach
Disability-adjusted life years (DALY) comprise two different complementary indicators:
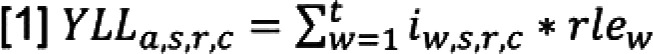
The mortality component (YLL) is calculated by summing the number of deaths (i) for individual ages t per age group a (within each age group (a), sex category (s), sub-national region (r), for a specific cause (of death) (c)) multiplied by the remaining life expectancy at age of death (w) for both sexes (11).
The morbidity component is calculated per cause (c) by summing the severity-specific (j) prevalent cases p, estimated on the basis of (point) prevalences (within each age group [a], sex category [s], and sub-national region [r]), multiplied by the severity-specific disability weight (dw). The latter corresponds to a weighting factor which varies between 0 (equivalent to perfect health) and smaller than 1 (1 would be equivalent to death), depending on the severity of the disease or health states (15). The weight quantifies the degree of health loss from disease or injury (15). Population surveys were conducted in various countries for the purpose of gathering this information. Two instruments were used in the surveys, paired comparisons [PC]) and population health equivalent questions [PHE]). The weights were derived from the results (15, 16, e2). In the present study, the lowest weight was 0.008 (uncertainty interval [UI]: 0.004–0.014) for mild injuries (within road injuries) and the highest was 0.658 (UI: 0.477–0.807) for severe major depressions.
Here, k can range between one and eight, depending on the cause (c), and corresponds to the number of levels of severity per disease. The maximum number of severity levels for the selected causes of burden of disease for the pilot project was eight.
The sum of YLL and YLD finally determines the DALY (according to age group [a], sex [s], region [r] and cause [c]).
1.2 Supplementary information about the YLD indicator
The YLD indicator can be interpreted in different ways, and various definitions are found in the literature that differ from the original version (years lived with disability [YLD]). Based on the conceptual idea behind DALY and its individual indicators, burden of disease is quantified as any deviation of current population health from an optimal health status quantified in the unit of life years (4). The difference between the actual age at death and a theoretical, statistical (more distant) life expectancy is calculated for mortality (e1). The term YLL (years of life lost) explicitly assumes that these years of life are lost to the population.
Concerning morbidity every year of life lived with disability is quantified. In order to compare the dimensions mortality and morbidity, the number of years spent with ill health are then converted into a unit of time equivalent to that of YLL by applying “disability weights” specific to the severity of the disease, in other words: YLD is weighted in relation to YLL (4, 16). After weighting, the GBD study refers to this as “years lived with disability” (YLD). However, the YLD then no longer represents the actual number of all life years spent with ill health but rather the length of time equivalent to YLL in the unit years of life.
Since the YLL are interpreted as a “lost” year of life, the equivalent time with respect to the YLD is consequently also a “lost” year of life. This conclusion often leads to other denominations and interpretations of the YLD indicator. It is therefore also referred to as “years of healthy life lost due to disability” (e3) or as “years lost to disability” (e4). This can also be implied from the fact that in the GBD study the DALY indicator is referred to, and interpreted as one “year of healthy life lost” (4). Consequently, the common metric for YLL and, after applying weights to convert years of life spent with a disease, would be a “lost” year of healthy life.
Although the indicators YLL, YLD and DALY are commonly referred to as “years of healthy life lost”, they in fact quantify those years of life which deviate from an ideal state of health. In order to avoid the idea of something actually being “lost”, we instead usually refer to burden of disease in terms of the respective individual indicators YLL, YLD, and DALY. The lack of precision in naming the indicators can be explained by the conceptual ambiguity arising from the derivation of the different indicators.
2. Limitations
2.1: Limitations of the data sources used for calculating YLD
Health survey data and study data
The generalizability of the results may be limited when representative samples of a population are used to estimate epidemiological indicators. Potential sources of error include measurement errors when measuring key outcomes, processing/editing errors when conducting studies, and nonresponse errors due to the refusal of respondents to participate (e12). This results in a variety of biases. Non-response in particular can have an impact on sample composition. This concerns not only representativeness of the characteristics age and sex, but also the inclusion of subpopulations, such as the homeless and persons with a migration background. The latter have so far been insufficiently addressed in population health surveys (e13). This generally results in sample sizes being too small for certain combinations of characteristics (age, sex, migration background, education, etc.) to make statistically sound statements about morbidity rates. These potential biases in the composition of the samples are best addressed by using multivariate analysis procedures and applying weighting procedures such as design and adaptive weighting, and possibly by considering the drop-out probability in longitudinal and cohort data sets, see for example (e10, e14).
Claims data from statutory health insurances
When using claims data to calculate epidemiological key indicators, data reliability should be assessed. It should be kept in mind that claims data primarily contain information relevant for the reimbursement of services, that misclassification may result from cases where health care services have not been utilized and diagnoses not documented, and there may be biases arising from billing and justification strategies (e15, e16). Non-utilization of health care services for headache, back pain, and neck pain was considered of relevance for the BURDEN 2020 project, so health surveys were conducted to collect data for these conditions. Non-utilization is less relevant for many other diseases, as cases with more severe disease are the largest contributors to YLD and therefore more likely expected to be associated with utilization of health care services and more complete documentation of patient diagnoses (e17). For example, documentation of diagnoses of those diseases requiring hospitalization are considered reliable because coding guidelines applied in the inpatient sector (for more detailed discussion, see [22]). This may be assumed to be the case with diseases such as severe myocardial infarction or with surgery for cancer. It is therefore also assumed that for many diseases disability is sufficiently mapped in claims data and hence the major part of the disease burden can be correctly calculated using this data base. In order to minimize misclassifications in claims data, disease-specific case definitions were developed using other data sources such as information on surgical procedures, drug prescriptions, and outpatient billing items in addition to patient diagnosis information (20, 22, e18– e20). However, the restriction remains that the validity of the diagnoses for some diseases or individual diagnoses (e.g., depression, dementia types) cannot be conclusively assessed at present. In the future, linkage between claims data and other data sources like cohort studies, such as the NAKO Health Study (e21) or clinical registries, will provide new insights (e22).
Apart from questions regarding internal validity, external validity of the claims data is also of relevance for population-based burden of disease calculations. In principle, generalizability of claims data results taken from one (type of) health insurer is limited because there is currently no random sample of the general population available (21, e23). Thus, systematic deviations from the general population have been found with respect to age and gender structure as well as morbidity (e24– e27). An extrapolation procedure was therefore used to correct not only differences in population structure but also health insurer-specific differences in morbidity as compared with the German general population (21). Finally, all of the results obtained on disease prevalence and severities were checked for plausibility and compared with external data sources (see detailed discussion in [22]). For this purpose, it was possible to use a large number of available publications from Germany for diabetes, for example, and the figures from the cancer registries were applied for cancer prevalence. However, the external plausibility check was often limited by the fact that suitable information was not available for Germany. Disease prevalence and severity distributions were then checked for plausibility using international burden of disease studies (18, e28).
Despite the limitations mentioned for internal and external validity, claims data of the statutory health insurance funds do have their advantages over other data sets: For instance, biases resulting from interviewer effects are excluded, as are recall bias, sampling, non-response, or the implicit exclusion of hard-to-reach groups, such as those of advanced age, the multimorbid, or persons with a migration background (e16, e29).
Claims data from statutory insured persons are used to map measures of disease prevalence in, amongst others, the Care Atlas (www.versorgungsatlas.de), the Diabetes Surveillance (www.diabsurv.rki.de) or the Health Atlas of the WIdO (www.gesundheitsatlas-deutschland.de). The present epidemiological metrics, generated by age, sex, and region and based on claims data, and the associated methodology documentation are available at www.krankheitslage-deutschland.de.
Road traffic accident statistics
Secondary data sources used include road traffic accident statistics, which cover all accidents recorded by the police that resulted in personal injury or property damage occurring on public roads or squares (26). The cause of the accident and the degree of injury are recorded, together with the age of the casualties and the type of vehicle. However, it cannot be ruled out that some Road injuries resulted in injuries relevant for calculating burden of disease but were not recorded by the police. To make corrections for this, the proportion of accidents not recorded by the police was determined from health survey data and used for extrapolation (see [13] for the relevant procedure).
2.2: Limitations of using severity distributions and disability weights
We resorted to the preliminary work of the GBD study for those causes of burden of disease for which we were unable to estimate the severity distributions ourselves (27). Use of GBD results, however, is subject to limitations because the GBD study applies global distributions that are mostly held constant over time (27, e28). However, use of national results is preferable because previous studies have shown striking differences between globally constant versus national distributions (for cancer see [28]). All disability weights were taken from the GBD study (27). The origin of the weights is the subject of lively discussion in the scientific community, as they are an essential underlying assumption of the DALY concept and make comparison with mortality possible at all (4).
Criticism of disability weights is directed on the one hand towards their meaning as health-related disability, which ignores individual resources such as access to help with daily activities or additional income to cope with these restrictions (14). On the other hand, it is criticized that the quantification of disability weights addresses not so much the actual objective loss of health but more the individual perception of the loss (e30). This is attributed to the lay form of describing health states that are rated by respondents in terms of severity (e31). It is this evaluation that ultimately forms the basis for estimating the weights (15, 16). Criticism is also leveled at the choice of statistical methods used for calculation, which, for example, neglects adjustments for comorbidities (e31). Furthermore, the possible impact of (social) context effects on the level of weights between countries cannot be ruled out (15, e2, e31).
Acknowledgments
Translated from the original German by Dr. Grahame Larkin MD
Funding
The study “BURDEN 2020 – The Burden of Disease in Germany at the National and Regional Level” is supported by the innovation fund of the Federal Joint committee (project number: 01VSF17007). BURDEN 2020 was also supported by staff assigned to the project “Development of a National Mental Health Surveillance System at the RKI”, funded by the German Federal Ministry of Health (grant number: ZMI5–2519FSB402).
Project participants
BURDEN 2020 Study Group: Alexander Rommel, Elena von der Lippe, Annelene Wengler, Michael Porst, Aline Anton, Janko Leddin, Thomas Ziese (Robert Koch Institute, RKI), Helmut Schröder, Katrin Schüssel, Gabriela Brückner, Jan Breitkreuz (AOK Research Institute, WIdO), Dietrich Plass, Heike Gruhl (German Environmental Agency, UBA)
Acknowledgments
We would like to thank Anna Kast (WIdO) for her support with information technology and database management as well as with the extrapolations. We would also like to thank Dr. med. Nina Buttmann-Schweiger (RKI) for her advice on operationalizing cancer-related secondary data and for her valuable comments on the article. Our thanks go to the scientific advisory board of the BURDEN 2020 project for its methodological advice on calculating burden of disease.
Footnotes
Conflict of interest statement
See funding reference for funding of individual staff and authors.
The authors confirm that no conflict of interest exists.
References
- 1.van der Maas PJ. How summary measures of population health are affecting health agendas. Bull World Health Organ. 2003 [PMC free article] [PubMed] [Google Scholar]
- 2.Mathers CD, Murray CJ, Ezzati M, Gakidou E, Salomon JA, Stein C. Population health metrics: crucial inputs to the development of evidence for health policy. Popul Health Metr. 2003;1:1–4. doi: 10.1186/1478-7954-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray CJ. Quantifying the burden of disease: the technical basis for disability-adjusted life years. Bull World Health Organ. 1994;72:429–445. [PMC free article] [PubMed] [Google Scholar]
- 4.Murray CJL, Lopez AD. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020 Cambridge. Harvard School of Public Health on behalf of the World Health Organization and the World Bank. 1996 [Google Scholar]
- 5.Murray CJ, Salomon JA, Mathers C. A critical examination of summary measures of population health. Bull World Health Organ. 2000;78:981–994. [PMC free article] [PubMed] [Google Scholar]
- 6.Murray CJ, Ezzati M, Flaxman AD, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380:2063–2066. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 7.Murray CJL, Salomon JA, Mathers CD, Lopez AD. Summary measures of population health: concepts, ethics, measurement and applications. Geneva: World Health Organization. 2002 [Google Scholar]
- 8.Murray CJL, Abbafati C, Abbas KM, et al. Five insights from the Global Burden of Disease Study 2019. Lancet. 2020;396:1135–1159. doi: 10.1016/S0140-6736(20)31404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mathers CD. History of global burden of disease assessment at the World Health Organization. Arch Public Health. 2020;78 doi: 10.1186/s13690-020-00458-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rommel A, von der Lippe E, Plaß D, et al. BURDEN 2020—burden of disease in Germany at the national and regional level. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018;61:1159–1166. doi: 10.1007/s00103-018-2793-0. [DOI] [PubMed] [Google Scholar]
- 11.Wengler A, Rommel A, Plaß D, Gruhl H, Leddin J, Ziese T, von der Lippe E, on behalf of the BURDEN 2020 Study Group Years of life lost to death—a comprehensive analysis of mortality in Germany conducted as part of the BURDEN 2020 project. Dtsch Arztebl Int. 2021;118:137–144. doi: 10.3238/arztebl.m2021.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wengler A, Gruhl H, Plaß D, et al. Redistributing ill-defined causes of death—a case study from the BURDEN 2020-project in Germany. Arch Public Health. 2021;79:1–18. doi: 10.1186/s13690-021-00535-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Porst M, Leddin J, Rommel A, et al. www.daly.rki.de/publications 2022 last accessed on 25 March 2022. Berlin: Methodenbericht zur Quantifizierung der years lived with disability (YLD) im Projekt BURDEN 2020—Genese von Krankheitshäufigkeiten, Schweregraden, Dauern und disability weights sowie Sensitivitätsanalysen Robert Koch-Institut (RKI) [Google Scholar]
- 14.Salomon JA, Haagsma JA, Davis A, et al. Disability weights for the Global Burden of Disease 2013 study. Lancet Glob Health. 2015;3:e712–e723. doi: 10.1016/S2214-109X(15)00069-8. [DOI] [PubMed] [Google Scholar]
- 15.Anand S, Hanson K. Disability-adjusted life years: a critical review. J Health Econ. 1997;16:685–702. doi: 10.1016/s0167-6296(97)00005-2. [DOI] [PubMed] [Google Scholar]
- 16.Salomon JA, Vos T, Hogan DR, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2012;380:2129–2143. doi: 10.1016/S0140-6736(12)61680-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Institute for Health Metrics and Evaluation (IHME) Global health data exchange. GBD Results Tool. http://ghdx.healthdata.org/gbd-results-tool (last accessed on 21 January 2022) [Google Scholar]
- 19.Breitkreuz J, Schüssel K, Brückner G, Schröder H. Krankheitslastbestimmung mit Prävalenzen und Schweregraden auf Routinedatenbasis. GGW. 2021;21:24–34. [Google Scholar]
- 20.Breitkreuz J, Schüssel K, Brückner G, Schröder H. Methodik zur Bestimmung von Prävalenzen und Schweregraden mit Routinedaten im Projekt BURDEN 2020—Falldefinitionen, Schweregrade, Prävalenzkonzept Berlin: Wissenschaftliches Institut der AOK (WIdO) www.krankheitslage-deutschland.de/dokumente/methodendokumentation.pdf 2021(last accessed on 25 March 2022) [Google Scholar]
- 21.Breitkreuz J, Brückner G, Burgard JP, et al. Schätzung kleinräumiger Krankheitshäufigkeiten für die deutsche Bevölkerung anhand von Routinedaten am Beispiel von Typ-2-Diabetes. AStA Wirtsch Sozialstat Arch. 2019;13:35–72. [Google Scholar]
- 22.Schüssel K, Breitkreuz J, Brückner G, Schröder H. Nutzung von Krankenkassenroutinedaten zur Bestimmung von Krankheitshäufigkeiten im Projekt BURDEN 2020. Gesundheitswesen. 2022 doi: 10.1055/a-1806-2115. [DOI] [PubMed] [Google Scholar]
- 23.von der Lippe E, Krause L, Porst M, et al. Prävalenz von Rücken- und Nackenschmerzen in Deutschland Ergebnisse der Krankheitslast-Studie BURDEN 2020. J Health Monit. 2021;6:1–14. [Google Scholar]
- 24.Porst M, Wengler A, Leddin J, et al. Migräne und Spannungskopfschmerz in Deutschland Prävalenz und Erkrankungsschwere im Rahmen der Krankheitslast-Studie BURDEN 2020. J Health Monit. 2020;5:1–26. [Google Scholar]
- 25.Atzendorf J, Rauschert C, Seitz NN, Lochbühler K, Kraus L. The use of alcohol, tobacco, illegal drugs and medicines—an estimate of consumption and substance-related disorders in Germany. Dtsch Arztebl Int. 2019;116:577–584. doi: 10.3238/arztebl.2019.0577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.FDZ der Statistischen Ämter des Bundes und der Länder. Statistik der Straßenverkehrsunfälle. 2017 DOI: 10.21242/46241.2017.00.00.1.1.0. [Google Scholar]
- 27.James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hilderink HB, Plasmans MH, Snijders BE, Boshuizen HC, Poos MR, van Gool CH. Accounting for multimorbidity can affect the estimation of the burden of disease: a comparison of approaches. Arch Public Health. 2016;74:1–16. doi: 10.1186/s13690-016-0147-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pace M, Lanzieri G, Glickman M, et al. Revision of the European standard population: report of the Eurostat’s task force. Luxembourg: Publications Office of the European Union. 2013 [Google Scholar]
- 30.Robert Koch-Institut (RKI) BURDEN 2020—Studie zur Krankheitslast in Deutschland und seinen Regionen. / www.daly.rki.de/ (last accessed on 3 May 2022) [Google Scholar]
- 31.FDZ der Statistischen Ämter des Bundes und der Länder. Todesursachenstatistik. 2017 DOI: 10.21242/23211.2017.00.00.1.1.0. [Google Scholar]
- 32.Statistisches Bundesamt. Sterbetafeln 2016/2018, nach Bundesländern, Durchschnittliche Lebenserwartung (Periodensterbetafel) https://www-genesis.destatis.de/genesis/online (last accessed on 4 May 2020) [Google Scholar]
- 33.Cox N. GROUP1D: Stata module for grouping or clustering in one dimension. EconPapers. https://econpapers.repec.org/software/bocbocode/S456844.htm (last accessed on 25 March 2022) 2007 [Google Scholar]
- 34.Bundesinstitut für Bau-, Stadt- und Raumforschung (BBSR) Laufende Raumbeobachtung—Raumabgrenzungen. Raumordnungsregionen. www.bbsr.bund.de/BBSR/DE/forschung/raumbeobachtung/Raumabgrenzungen/deutschland/regionen/Raumordnungsregionen/raumordnungsregionen.html (last accessed on 23 February 2022) [Google Scholar]
- 35.Siegrist J. Elsevier, Urban und Fischer. München: 2005. Medizinische Soziologie. [Google Scholar]
- 36.Jacobi F, Mack S, Gerschler A, et al. The design and methods of the mental health module in the German Health Interview and Examination Survey for Adults (DEGS1-MH) Int J Methods Psychiatr Res. 2013;22:83–99. doi: 10.1002/mpr.1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Münnich R BJ, Vogt M. Small Area-Statistik: Methoden und Anwendungen. AStA Wirtsch Sozialstat Arch. 2013;6:149–191. [Google Scholar]
- 38.Wyper GM, Assuncao R, Fletcher E, et al. The increasing significance of disease severity in a burden of disease framework. Scand J Public Health. 2021:1–5. doi: 10.1177/14034948211024478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Plass D, Vos T, Hornberg C, Scheidt-Nave C, Zeeb H, Krämer A. Trends in disease burden in Germany—results, implications and limitations of the Global Burden of Disease Study. Dtsch Arztebl Int. 2014;111:629–638. doi: 10.3238/arztebl.2014.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.Roth GA, Abate D, Abate KH, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E2.Haagsma JA, Maertens de Noordhout C, Polinder S, et al. Assessing disability weights based on the responses of 30,660 people from four European countries. Popul Health Metr. 2015;13 doi: 10.1186/s12963-015-0042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E3.World Health Organization (WHO) Disability-adjusted life years (DALY) www.who.int/data/gho/indicator-metadata-registry/imr-details/158 (last accessed on 25 March 2022) [Google Scholar]
- E4.Wyper GMA, Grant I, Fletcher E, Chalmers N, McCartney G, Stockton DL. Prioritising the development of severity distributions in burden of disease studies for countries in the European region. Arch Public Health. 2020;78:1–4. doi: 10.1186/s13690-019-0385-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E5.Troeger C, Blacker B, Khalil IA, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. 2018;18:1191–1210. doi: 10.1016/S1473-3099(18)30310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E6.Burstein R, Fleming T, Haagsma J, Salomon JA, Vos T, Murray CJ. Estimating distributions of health state severity for the global burden of disease study. Popul Health Metr. 2015;13:1–19. doi: 10.1186/s12963-015-0064-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E7.Vos T, Barber RM, Bell B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E8.Zhang Y, Lazzarini PA, McPhail SM, van Netten JJ, Armstrong DG, Pacella RE. Global disability burdens of diabetes-related lower-extremity complications in 1990 and 2016. Diabetes Care. 2020;43:964–974. doi: 10.2337/dc19-1614. [DOI] [PubMed] [Google Scholar]
- E9.Haagsma JA, Graetz N, Bolliger I, et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev. 2016;22:3–18. doi: 10.1136/injuryprev-2015-041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E10.Lange C, Jentsch F, Allen J, et al. Data resource profile: German Health Update (GEDA)—the health interview survey for adults in Germany. Int J Epidemiol. 2015;44:442–450. doi: 10.1093/ije/dyv067. [DOI] [PubMed] [Google Scholar]
- E11.Hoffmann R, Lange M, Butschalowsky H, et al. Querschnitterhebung von KiGGS Welle 2 - Teilnehmendengewinnung, Response und Repräsentativität. J Health Monit. 2018;3:82–96. [Google Scholar]
- E12.Davern M. Nonresponse rates are a problematic indicator of nonresponse bias in survey research. Health Serv Res. 2013;48:905–912. doi: 10.1111/1475-6773.12070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E13.Santos-Hövener C, Schumann M, Schmich P, et al. Verbesserung der Informationsgrundlagen zur Gesundheit von Menschen mit Migrationshintergrund: Projektbeschreibung und erste Erkenntnisse von IMIRA. J Health Monit. 2019;4:49–61. [Google Scholar]
- E14.Kamtsiuris P, Lange M, Hoffmann R, et al. The first wave of the German Health Interview and Examination Survey for Adults (DEGS1) Sampling design, response, weighting, and representativeness. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:620–630. doi: 10.1007/s00103-012-1650-9. [DOI] [PubMed] [Google Scholar]
- E15.Glaeske G, Rebscher H, Willich S. Versorgungsforschung: Auf gesetzlicher Grundlage systematisch ausbauen. Dtsch Arztebl. 2010;107:1295–1297. [Google Scholar]
- E16.Ohlmeier C, Frick J, Prütz F, et al. Nutzungsmöglichkeiten von Routinedaten der Gesetzlichen Krankenversicherung in der Gesundheitsberichterstattung des Bundes. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2014;57:464–472. doi: 10.1007/s00103-013-1912-1. [DOI] [PubMed] [Google Scholar]
- E17.Angelow A, Reber KC, Schmidt CO, Baumeister SE, Chenot J-F. Untersuchung der Prävalenz kardiologischer Risikofaktoren in der Allgemeinbevölkerung: Ein Vergleich ambulanter ärztlicher Abrechnungsdaten mit Daten einer populationsbasierten Studie. Gesundheitswesen. 2019;81:791–800. doi: 10.1055/a-0588-4736. [DOI] [PubMed] [Google Scholar]
- E18.Abbas S, Ihle P. Swart E, Ihle P, Gothe H, Matusiewicz D, editors. Bestimmung von Behandlungs- und Erkrankungsperioden in Routinedaten Routinedaten im Gesundheitswesen - Handbuch Sekundärdatenanalyse: Grundlagen, Methoden und Perspektiven. Bern: Huber. 2014:369–375. [Google Scholar]
- E19.Schubert I, Ihle P, Köster I. Interne Validierung von Diagnosen in GKV-Routinedaten: Konzeption mit Beispielen und Falldefinition. Gesundheitswesen. 2010;72:316–322. doi: 10.1055/s-0030-1249688. [DOI] [PubMed] [Google Scholar]
- E20.Schubert I, Köster I. Krankheitsereignis: Operationalisierung und Falldefinition Routinedaten im Gesundheitswesen - Handbuch Sekundärdatenanalyse: Grundlagen, Methoden und Perspektiven. In: Swart E, Ihle P, Gothe H, Matusiewicz D, editors. Huber. Bern: 2014. pp. 358–368. [Google Scholar]
- 21.Schipf S, Schöne G, Schmidt B, et al. Die Basiserhebung der NAKO Gesundheitsstudie: Teilnahme an den Untersuchungsmodulen, Qualitätssicherung und Nutzung von Sekundärdaten. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2020;63:254–266. doi: 10.1007/s00103-020-03093-z. [DOI] [PubMed] [Google Scholar]
- 22.Roessler M, Schmitt J, Bobeth C, et al. Is treatment in certified cancer centers related to better survival in patients with pancreatic cancer? Evidence from a large German cohort study. BMC Cancer. 2022;22:1–10. doi: 10.1186/s12885-022-09731-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schröder H, Brückner G. Unterstützung für den Landrat. Gesundheit und Gesellschaft (G+G) 2019;22:12–13. [Google Scholar]
- 24.Hoffmann F, Icks A. Diabetes ‚epidemic‘ in Germany? A critical look at health insurance data sources. Exp Clin Endocrinol Diabetes. 2012;120:410–415. doi: 10.1055/s-0032-1306331. [DOI] [PubMed] [Google Scholar]
- 25.Hoffmann F, Koller D. Verschiedene Regionen, verschiedene Versichertenpopulationen? Soziodemografische und gesundheitsbezogene Unterschiede zwischen Krankenkassen. Gesundheitswesen. 2017;79:e1–e9. doi: 10.1055/s-0035-1564074. [DOI] [PubMed] [Google Scholar]
- 26.Huber J, Lampert T, Mielck A. Unterschiede bei Gesundheitsrisiken, Morbidität und gesundheitlicher Versorgung zwischen Kindern GKV-bzw PKV-versicherter Eltern: Ergebnisse aus dem Kinder-und Jugendgesundheitssurvey (KiGGS) Gesundheitswesen. 2012;74:627–638. doi: 10.1055/s-0031-1301268. [DOI] [PubMed] [Google Scholar]
- 27.Kriwy P, Mielck A. Versicherte der gesetzlichen Krankenversicherung (GKV) und der privaten Krankenversicherung (PKV): Unterschiede in Morbidität und Gesundheitsverhalten. Gesundheitswesen. 2006;68:281–288. doi: 10.1055/s-2006-926779. [DOI] [PubMed] [Google Scholar]
- 28.Wyper GMA, Grant I, Fletcher E, McCartney G, Stockton DL. The impact of worldwide, national and sub-national severity distributions in Burden of Disease studies: a case study of cancers in Scotland. PLoS One. 2019;14 doi: 10.1371/journal.pone.0221026. e0221026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gerste B, Drogan D, Günster C. Schattauer. Stuttgart: 2016. Diagnosehäufigkeit und Inanspruchnahme von Gesundheitsleistungen In: Klauber J, Günster C, Gerste B, Robra BP, Schmacke N (eds.): Versorgungs-Report 2015/2016; pp. 391–445. [Google Scholar]
- 30.Nord E. Disability weights in the Global Burden of Disease 2010: unclear meaning and overstatement of international agreement. Health Policy. 2013;111:99–104. doi: 10.1016/j.healthpol.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 31.Chen A, Jacobsen KH, Deshmukh AA, Cantor SB. The evolution of the disability-adjusted life year (DALY) Socio-Econ Plan Sci. 2015;49:10–15. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
1. Calculation approach and additional information about the YLD indicator
1.1 Calculation approach
Disability-adjusted life years (DALY) comprise two different complementary indicators:
The mortality component (YLL) is calculated by summing the number of deaths (i) for individual ages t per age group a (within each age group (a), sex category (s), sub-national region (r), for a specific cause (of death) (c)) multiplied by the remaining life expectancy at age of death (w) for both sexes (11).
The morbidity component is calculated per cause (c) by summing the severity-specific (j) prevalent cases p, estimated on the basis of (point) prevalences (within each age group [a], sex category [s], and sub-national region [r]), multiplied by the severity-specific disability weight (dw). The latter corresponds to a weighting factor which varies between 0 (equivalent to perfect health) and smaller than 1 (1 would be equivalent to death), depending on the severity of the disease or health states (15). The weight quantifies the degree of health loss from disease or injury (15). Population surveys were conducted in various countries for the purpose of gathering this information. Two instruments were used in the surveys, paired comparisons [PC]) and population health equivalent questions [PHE]). The weights were derived from the results (15, 16, e2). In the present study, the lowest weight was 0.008 (uncertainty interval [UI]: 0.004–0.014) for mild injuries (within road injuries) and the highest was 0.658 (UI: 0.477–0.807) for severe major depressions.
Here, k can range between one and eight, depending on the cause (c), and corresponds to the number of levels of severity per disease. The maximum number of severity levels for the selected causes of burden of disease for the pilot project was eight.
The sum of YLL and YLD finally determines the DALY (according to age group [a], sex [s], region [r] and cause [c]).
1.2 Supplementary information about the YLD indicator
The YLD indicator can be interpreted in different ways, and various definitions are found in the literature that differ from the original version (years lived with disability [YLD]). Based on the conceptual idea behind DALY and its individual indicators, burden of disease is quantified as any deviation of current population health from an optimal health status quantified in the unit of life years (4). The difference between the actual age at death and a theoretical, statistical (more distant) life expectancy is calculated for mortality (e1). The term YLL (years of life lost) explicitly assumes that these years of life are lost to the population.
Concerning morbidity every year of life lived with disability is quantified. In order to compare the dimensions mortality and morbidity, the number of years spent with ill health are then converted into a unit of time equivalent to that of YLL by applying “disability weights” specific to the severity of the disease, in other words: YLD is weighted in relation to YLL (4, 16). After weighting, the GBD study refers to this as “years lived with disability” (YLD). However, the YLD then no longer represents the actual number of all life years spent with ill health but rather the length of time equivalent to YLL in the unit years of life.
Since the YLL are interpreted as a “lost” year of life, the equivalent time with respect to the YLD is consequently also a “lost” year of life. This conclusion often leads to other denominations and interpretations of the YLD indicator. It is therefore also referred to as “years of healthy life lost due to disability” (e3) or as “years lost to disability” (e4). This can also be implied from the fact that in the GBD study the DALY indicator is referred to, and interpreted as one “year of healthy life lost” (4). Consequently, the common metric for YLL and, after applying weights to convert years of life spent with a disease, would be a “lost” year of healthy life.
Although the indicators YLL, YLD and DALY are commonly referred to as “years of healthy life lost”, they in fact quantify those years of life which deviate from an ideal state of health. In order to avoid the idea of something actually being “lost”, we instead usually refer to burden of disease in terms of the respective individual indicators YLL, YLD, and DALY. The lack of precision in naming the indicators can be explained by the conceptual ambiguity arising from the derivation of the different indicators.
2. Limitations
2.1: Limitations of the data sources used for calculating YLD
Health survey data and study data
The generalizability of the results may be limited when representative samples of a population are used to estimate epidemiological indicators. Potential sources of error include measurement errors when measuring key outcomes, processing/editing errors when conducting studies, and nonresponse errors due to the refusal of respondents to participate (e12). This results in a variety of biases. Non-response in particular can have an impact on sample composition. This concerns not only representativeness of the characteristics age and sex, but also the inclusion of subpopulations, such as the homeless and persons with a migration background. The latter have so far been insufficiently addressed in population health surveys (e13). This generally results in sample sizes being too small for certain combinations of characteristics (age, sex, migration background, education, etc.) to make statistically sound statements about morbidity rates. These potential biases in the composition of the samples are best addressed by using multivariate analysis procedures and applying weighting procedures such as design and adaptive weighting, and possibly by considering the drop-out probability in longitudinal and cohort data sets, see for example (e10, e14).
Claims data from statutory health insurances
When using claims data to calculate epidemiological key indicators, data reliability should be assessed. It should be kept in mind that claims data primarily contain information relevant for the reimbursement of services, that misclassification may result from cases where health care services have not been utilized and diagnoses not documented, and there may be biases arising from billing and justification strategies (e15, e16). Non-utilization of health care services for headache, back pain, and neck pain was considered of relevance for the BURDEN 2020 project, so health surveys were conducted to collect data for these conditions. Non-utilization is less relevant for many other diseases, as cases with more severe disease are the largest contributors to YLD and therefore more likely expected to be associated with utilization of health care services and more complete documentation of patient diagnoses (e17). For example, documentation of diagnoses of those diseases requiring hospitalization are considered reliable because coding guidelines applied in the inpatient sector (for more detailed discussion, see [22]). This may be assumed to be the case with diseases such as severe myocardial infarction or with surgery for cancer. It is therefore also assumed that for many diseases disability is sufficiently mapped in claims data and hence the major part of the disease burden can be correctly calculated using this data base. In order to minimize misclassifications in claims data, disease-specific case definitions were developed using other data sources such as information on surgical procedures, drug prescriptions, and outpatient billing items in addition to patient diagnosis information (20, 22, e18– e20). However, the restriction remains that the validity of the diagnoses for some diseases or individual diagnoses (e.g., depression, dementia types) cannot be conclusively assessed at present. In the future, linkage between claims data and other data sources like cohort studies, such as the NAKO Health Study (e21) or clinical registries, will provide new insights (e22).
Apart from questions regarding internal validity, external validity of the claims data is also of relevance for population-based burden of disease calculations. In principle, generalizability of claims data results taken from one (type of) health insurer is limited because there is currently no random sample of the general population available (21, e23). Thus, systematic deviations from the general population have been found with respect to age and gender structure as well as morbidity (e24– e27). An extrapolation procedure was therefore used to correct not only differences in population structure but also health insurer-specific differences in morbidity as compared with the German general population (21). Finally, all of the results obtained on disease prevalence and severities were checked for plausibility and compared with external data sources (see detailed discussion in [22]). For this purpose, it was possible to use a large number of available publications from Germany for diabetes, for example, and the figures from the cancer registries were applied for cancer prevalence. However, the external plausibility check was often limited by the fact that suitable information was not available for Germany. Disease prevalence and severity distributions were then checked for plausibility using international burden of disease studies (18, e28).
Despite the limitations mentioned for internal and external validity, claims data of the statutory health insurance funds do have their advantages over other data sets: For instance, biases resulting from interviewer effects are excluded, as are recall bias, sampling, non-response, or the implicit exclusion of hard-to-reach groups, such as those of advanced age, the multimorbid, or persons with a migration background (e16, e29).
Claims data from statutory insured persons are used to map measures of disease prevalence in, amongst others, the Care Atlas (www.versorgungsatlas.de), the Diabetes Surveillance (www.diabsurv.rki.de) or the Health Atlas of the WIdO (www.gesundheitsatlas-deutschland.de). The present epidemiological metrics, generated by age, sex, and region and based on claims data, and the associated methodology documentation are available at www.krankheitslage-deutschland.de.
Road traffic accident statistics
Secondary data sources used include road traffic accident statistics, which cover all accidents recorded by the police that resulted in personal injury or property damage occurring on public roads or squares (26). The cause of the accident and the degree of injury are recorded, together with the age of the casualties and the type of vehicle. However, it cannot be ruled out that some Road injuries resulted in injuries relevant for calculating burden of disease but were not recorded by the police. To make corrections for this, the proportion of accidents not recorded by the police was determined from health survey data and used for extrapolation (see [13] for the relevant procedure).
2.2: Limitations of using severity distributions and disability weights
We resorted to the preliminary work of the GBD study for those causes of burden of disease for which we were unable to estimate the severity distributions ourselves (27). Use of GBD results, however, is subject to limitations because the GBD study applies global distributions that are mostly held constant over time (27, e28). However, use of national results is preferable because previous studies have shown striking differences between globally constant versus national distributions (for cancer see [28]). All disability weights were taken from the GBD study (27). The origin of the weights is the subject of lively discussion in the scientific community, as they are an essential underlying assumption of the DALY concept and make comparison with mortality possible at all (4).
Criticism of disability weights is directed on the one hand towards their meaning as health-related disability, which ignores individual resources such as access to help with daily activities or additional income to cope with these restrictions (14). On the other hand, it is criticized that the quantification of disability weights addresses not so much the actual objective loss of health but more the individual perception of the loss (e30). This is attributed to the lay form of describing health states that are rated by respondents in terms of severity (e31). It is this evaluation that ultimately forms the basis for estimating the weights (15, 16). Criticism is also leveled at the choice of statistical methods used for calculation, which, for example, neglects adjustments for comorbidities (e31). Furthermore, the possible impact of (social) context effects on the level of weights between countries cannot be ruled out (15, e2, e31).