Abstract
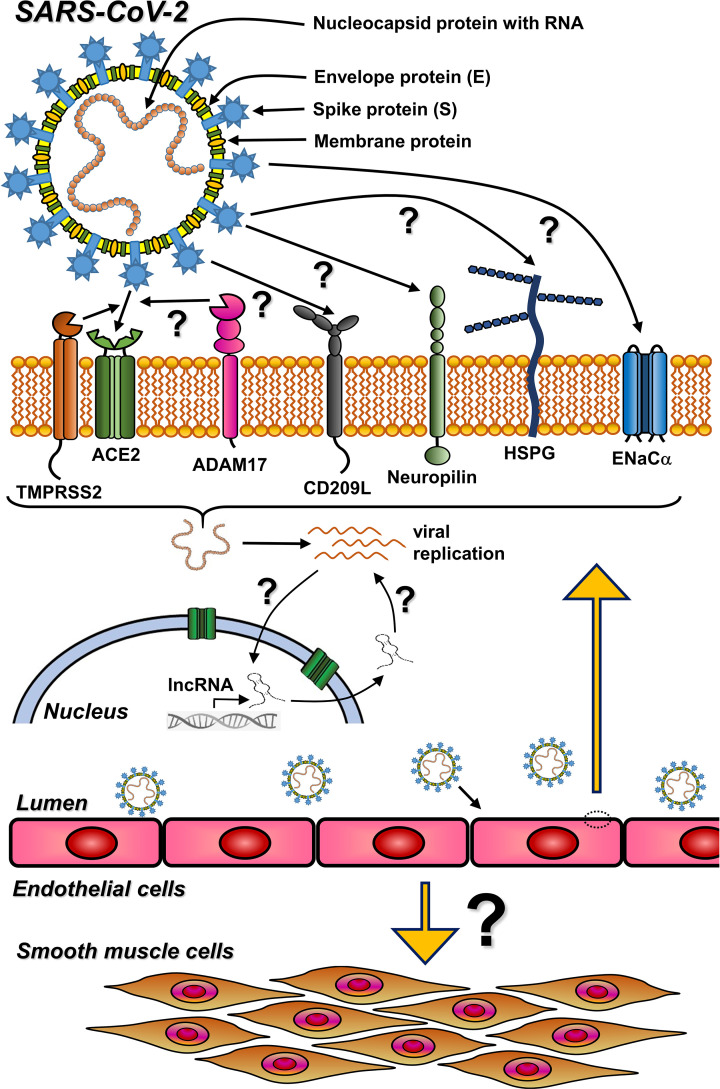
Although COVID-19 is primarily a respiratory disease, it may affect also the cardiovascular system. COVID-19 patients with cardiovascular disorder (CVD) develop a more severe disease course with a significantly higher mortality rate than non-CVD patients. A common denominator of CVD is the dysfunction of endothelial cells (ECs), increased vascular permeability, endothelial-to-mesenchymal transition, coagulation, and inflammation. It has been assumed that clinical complications in COVID-19 patients suffering from CVD are caused by SARS-CoV-2 infection of ECs through the angiotensin-converting enzyme 2 (ACE2) receptor and the cellular transmembrane protease serine 2 (TMPRSS2) and the consequent dysfunction of the infected vascular cells. Meanwhile, other factors associated with SARS-CoV-2 entry into the host cells have been described, including disintegrin and metalloproteinase domain-containing protein 17 (ADAM17), the C-type lectin CD209L or heparan sulfate proteoglycans (HSPG). Here, we discuss the current data about the putative entry of SARS-CoV-2 into endothelial and smooth muscle cells. Furthermore, we highlight the potential role of long non-coding RNAs (lncRNAs) affecting vascular permeability in CVD, a process that might exacerbate disease in COVID-19 patients.
Keywords: cardiovascular disorder (CVD), COVID-19, endothelial cells (ECs), ong non-coding RNA, SARS-CoV-2, smooth muscle cells (SMCs)
Introduction
Coronaviruses (CoVs) belong to a large and heterogeneous subfamily of Coronaviridae, causing mostly respiratory disease and severe acute respiratory syndrome (SARS) which can be fatal without proper treatment [1–3]. In December 2019, a novel coronavirus SARS-CoV-2 was identified, causing a worldwide coronavirus disease 2019 (COVID-19) with over 6 million deaths [4–6]. COVID-19 may lead to the death of susceptible people. Notably, people with advanced age and comorbidities are at higher risk of severe complications. Comorbidities not only include chronic diseases like cancer, kidney and liver disease, asthma, COPD, diabetes, and heart failure but also smoking immunosuppression and drug abuse (https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html) [2,5,7–15].
Although COVID-19 is primarily a respiratory disease, other nonpulmonary manifestations have also been described, such as renal complications, neurological, gastrointestinal, and various cardiovascular disorders [9,10,16–26]. Particularly, patients suffering from cardiovascular disorder (CVD) have the highest risk of severe COVID-19 complications, leading often to death [27]. Intriguingly, CVD patients infected by SARS-CoV-2 have shown more severe pathophysiological changes in the lung compared to individuals without CVD. Endothelial cells (ECs) at the interface between blood and the underlying vascular tissue have also been described to be involved in the COVID-19 pathologies [14,28–37], possibly leading to inflammation and endothelial dysfunction. Currently, the clinical complications in COVID-19 patients with CVD are thought to be due to SARS-CoV-2 infection and subsequent dysregulation of ECs [12,36,38,39].
However, the evidence that ECs are infected by SARS-CoV-2 has been shown only by electron microscopy [28,31,40–42]. Interestingly, studies using immunohistochemistry (IHC) or in situ hybridization did not find compelling evidence of ECs infection by SARS-CoV-2 [43–45]. Accordingly, it has been even reported that ECs are at least partially resistant to SARS-CoV-2 infection [42,46]. Meanwhile, other factors have been described that might contribute to the viral entry into the host cells, including, e.g., disintegrin and metalloproteinase domain-containing protein 17 (ADAM17), the C-type lectin CD209L, and heparan sulfate proteoglycans (HSPG) [47–55]. SARS-CoV-2 has been reported to bind also to RGD motif (Arg-Gly-Asp) of integrins and to vimentin [56,57]. These structural proteins might increase and maintain the binding affinity of the viral S protein to the cell surface, facilitating SARS-CoV-2 entry. Thus, the entry mechanisms of SARS-CoV-2, particularly into ECs, have yet to be elucidated.
Recently, increasing evidence has revealed an important role of non-coding RNAs (ncRNAs) not only in cardiovascular disorders [58–62] but also in viral infection by regulating the entry mechanism and the host antiviral response [63–67].
In this review article, we discuss current data on SARS-CoV-2 entry into endothelial and smooth muscle cells and their dysfunction following COVID-19 infection in the context of CVD. Furthermore, we discuss intracellular mechanisms of infection variability and the pivotal role of non-coding RNA in COVID-19 and CVD.
COVID-19 epidemiology and cardiovascular system
COVID-19 was first identified in Wuhan, the capital of the Hubei province of China, in December 2019. It spread rapidly throughout the world within a couple of months [2]. In August 2022, 600 million cases have been reported, resulting in over 6 million deaths worldwide [Word Health Organization, COVID-19 Dashboard, https://covid19.who.int/]. Many infected individuals have developed severe syndromes, with a global lethality of 1–3%, most of them with various comorbidities [68]. Significantly higher risks have been shown particularly in older patients, with a 3.6% mortality in 60–69 years old, 8.0% in 70–79 years old, and 14.8% in individuals older than 80 years [2].
Although COVID-19 is primarily a respiratory disease, it affects adversely also the cardiovascular system. Patients with CVD have the highest risk of contracting severe COVID-19 and death [11,15,23,24,27,69]. Besides older age (>65 years), the specific risk factors include hypertension, obesity, diabetes mellitus, chronic pulmonary disease, various vascular disorders, and heart failure [11,12,16–27,80]. CVD patients infected by SARS-CoV-2 tend to have more severe lung pathology compared to individuals without CVD. They also show elevated levels of inflammatory markers, such as C-reactive protein (CRP), interleukin (IL)-6, serum amyloid A (SAA), D-dimer, and fibrinogen, among others [9,39,70, 71–75].
Human coronaviruses and infection cycle
Coronaviruses are enveloped, single-stranded, positive (+)-sense RNA viruses. Seven CoVs have been considered contagious, including the most recent one SARS-CoV-2, closely related to SARS-CoV 2002/2003 and more distantly related to MERS-CoV [76–78]. The remaining four CoVs (HCoV-NL63, HCoV-229E, HCoV-OC43, and HKU1) are endemic in the human population and typically cause mild respiratory complications compared with highly pathogenic SARS-CoV, MERS-CoV, and SARS-CoV-2 [79,80]. The common human CoVs account for 10–30% of the cold cases in adults but in rare cases they can cause life-threatening disease in infants, elderly or immunocompromised individuals.
CoVs encode four structural proteins: spike (S), membrane (M), envelope (E), and nucleocapsid (N) proteins [2,81]. The S protein is essential for virus binding to the host cell, entry, and infection [2,77,78,81]. SARS-CoV-2 and SARS-CoV are similar in their pathology, both binding to angiotensin-converting enzyme 2 (ACE2) receptor but have distinct transmission efficacy [78,82]. After docking to ACE2, the virus is processed by cellular transmembrane protease serine (TMPRSS2), which cleaves ACE2 and activates the S protein, facilitating virus entry into the host cell [2,83]. The infection leads to a massive immune response, often referred to as a cytokine storm [83,84].
Upon entering the host cell, the virus particle uncoats and releases its positive-stranded RNA into the cytosol [6]. Genome replication takes place on cytoplasmic double-membrane vesicles (DMVs) and membranous structures with small open double-membrane spherules [78,85]. The replication depends upon the synthesis of a viral replicase-transcriptase complex, composed of viral proteins as well as several host proteins [86]. The replication of CoV is associated with the endoplasmic reticulum (ER) leading to ER stress and may trigger apoptosis [79,86]. Furthermore, some of the viral proteins repress innate immunity and arrest the cell-cycle progression [86]. During virus assembly, the N protein binds to the viral genomic RNA and interacts with other structural proteins (S, E, and M) to assemble SARS-CoV particles. Virion morphogenesis is completed upon budding into organelles of the secretory pathway, including ER, Golgi, and intermediate compartment [79].
SARS-CoV-2 cell entry through ACE2 receptor
Early studies on CoVs have described high affinity of the receptor-binding domain (RBD) of the S protein to ACE2 receptor [2,87–90] (Figure 1). Thereby, SARS-CoV-2 has a higher binding affinity to ACE2 than SARS-CoV, which may increase infectivity [87,90]. As with many cell-associated viral receptors, the ectodomain of ACE2 can be shed from the cell surface by, e.g., metalloprotease ADAM17, and consequently circulates in blood and tissue fluids [91]. Soluble receptor ectodomain may limit SARS-CoV-2 invasion into the host cells by competing with the cell-associated ACE2 for SARS-CoV-2 binding [92,93]. Unlike SARS-CoV, SARS-CoV-2 is processed by the cellular transmembrane protease serine (TMPRSS2), which not only cleaves ACE2 but also activates the S protein, facilitating SARS-CoV-2 entry into the host cell [2,14]. Notably, ACE2 and TMPRSS2 are widely expressed in bronchial secretory as well as epithelial cells [94]. In absence of TMPRSS2, the virus and ACE2 undergo endocytosis, which together with protease-mediated shedding of ACE2 down-regulates the cell surface levels of ACE2 [68] and may ease the COVID-19 disease. In addition, ACE2 has also been considered a regulator of angiogenesis [37,95–97].
Figure 1. Potential entry mechanisms of SARS-CoV-2 in vascular cells and the role of lncRNA.
ACE2, angiotensin-converting enzyme 2; ADAM17, disintegrin and metalloproteinase domain-containing protein 17; CD209L, C-type lectin membrane protein; ENaC, epithelial sodium channel-α; HSPG, heparan sulfate proteoglycans; lncRNA, long non-coding RNA; TMPRSS2, transmembrane protease serine 2.
Although ACE2 and TMPRSS2 are the best-characterized CoV entry proteins, other cellular factors might be involved in virus entry and infection as well [50]. Furthermore, controversial results regarding SARS-CoV-2 infection of vascular cells exist [28,43,46].
Alternative SARS-CoV-2 entry pathways
In general, CoVs can enter host cells by two mechanisms: cell membrane fusion, which engages ACE2 and TMPRSS2, or an endosomal pathway. Upon binding of spike (S) protein to ACE2 receptor the S protein is proteolytically primed by TMPRSS2 on the cell surface or by cathepsin B or L in the lysosomes [50,52,53] (Figure 1). Cathepsin B has been shown to be associated with SARS-CoV-2 infection of brain vascular cells, which do not express TMPRSS2 [51]. Cantuti-Castelvetri et al. and Daly et al. showed that the furin-cleaved S protein S1 binds to the neuropilin-1 receptors (NPR1) through the C-end rule peptide motive, which is present also in NRP2 and thereby significantly improved viral entry [47,98–100]. These results were extended by Giordo et al. who suggested neuropilins and CD209L, a C-type lectin membrane protein, highly expressed in human type II alveolar cells and lung ECs [47], as putative receptors facilitating SARS-CoV-2 entry into EC [100]. CD209L can mediate SARS-CoV-2 entry by interaction with the RBD domain of the viral S protein [101] (Figure 1). Other cell surface proteins and proteoglycans may also participate in SARS-CoV-2 entry. For instance, heparan sulfate proteoglycan (HSPG) was shown to be involved in the interaction between viral particles and infected cells [49,54]. Sialic acid was reported to bind to the spike proteins of SARS-CoV-2 and other human coronaviruses, possibly enhancing infection under favorable conditions [102,103].
Intriguingly, a molecular mimicry entry model of SARS-CoV-2 has also been suggested for human coronaviruses [48,89], where the S-protein may mimic the human α subunit of the epithelial sodium channel (ENaC-α). ENaC-α is associated with the renin–angiotensin system and regulates water homeostasis by modulating the level of sodium ions in lung airway tissue and controlling the volume of airway-surface liquids. Importantly, sodium channels require activation by furin cleavage to control the fluid reabsorption. Interestingly, the furin-like cleavage motif of S1/S2 proteins of SARS-CoV-2 is identical to that of ENaC-α (SARS-CoV-2 S1/S2 sequence: -RRAR x SVAS-, position 683-690; ENaC-α sequence: -RRAR x SVAS-, position 201-208; ‘x’ furin cleavage site) [102,104].
ACE is a key regulator of the renin–angiotensin system
The renin–angiotensin system (RAS) plays a key role in the regulation of blood pressure, vascular tone, water and electrolyte homeostasis, cardiovascular and renal health [105–110]. Its activation is initiated by liver-derived angiotensinogen that is cleaved by renin into angiotensin I (Ang I). Ang I is further enzymatically modified into angiotensin II (Ang II) by ACE. The receptor ACE2, a homolog to ACE, cleaves Ang I and Ang II to Ang-(1-9) and Ang-(1-7), respectively [111]. Thereby, ACE promotes inflammation, vasoconstriction, and fibrosis, whereas ACE2 has anti-inflammatory, antiproliferative, vasodilatory, and antifibrotic effects [87].
The ACE2 receptor has various biological functions [88]. First, through Ang-(1-7) it exhibits various protective functions, including anti-inflammatory and anti-proliferative effects and reduction of oxidative stress, leading to vasodilation and maintenance of cardiovascular health [111]. Second, in the kidney and intestine, ACE2 activity is required for the uptake of amino acids across the epithelia [88]. Third, human CoVs use ACE2 as an entry portal into cells [88,93,112]. In addition, ACE2 has also been considered a regulator of angiogenesis [37,95–97,113]. Accordingly, increased levels of proangiogenic factors such as vascular endothelial growth factor (VEGF), fibroblast growth factor-2, and hypoxia-inducible factor-1α (HIF-1α) have been detected in COVID-19 patients [34,114–116]. Angiogenetic factors increase endothelial permeability, promoting the infiltration of inflammatory cells into the vessel wall. These circumstances contribute also to atherosclerosis in CVD patients [117–121].
All vascular cells, including ECs, SMCs, fibroblasts, and pericytes, express the ACE2 receptor as well [120,122]. Thereby, CVD can affect the expression of ACE2 promoting oxidative stress, inflammation and endothelial dysfunction [33]. In addition, cigarette smoking, diabetes, chronic pulmonary obstructive disease, certain tumors, age, and sex can also influence the expression of ACE2 [123].
COVID-19 and endothelial cells in CVD
A common denominator of CVDs is endothelial dysfunction. ECs play a vital role in the maintenance of vascular haemostasis. Currently, the clinical complications in patients with COVID-19 and CVD are supposed to be the direct consequences of SARS-CoV-2 infection and dysregulation of ECs [13,14,31,32,38,116,124–128]. Under normal physiological conditions, the vascular endothelium regulates the systemic blood flow, immune response, coagulation, and tissue perfusion in line with the underlying SMCs or pericytes of the microvasculature [19,23,28,31,72,75,129–131].
Thereby, SARS-CoV-2 exacerbates or triggers endothelial damage either by infecting ECs directly or indirectly, by infecting other cell types, leading to hyperinflammation and impaired antiviral response [28,42]. Interestingly, similar processes lead to the development of CVD and promote atherosclerosis [23,37,106]. Thus, COVID-19-related hyperinflammation and endothelial damage might enhance and accelerate atherosclerotic progression, vulnerable plaques, and increase the risk of ischemic stroke or heart attack. Furthermore, an elevated neutrophil count in the blood of COVID-19 patients may enhance the formation of neutrophil extracellular traps (NETs) and thereby increase disease severity, thrombosis, and coagulopathy [116,132–134]. NETs are part of a rapid immune defence system against pathogens and initiate thrombosis by activating coagulation pathways [116,133]. In this context, increased levels of NET remnants have been detected in the serum of COVID-19 patients, including cell-free DNA, and factors promoting thrombosis and inflammation of the arterial wall [134].
Remarkably, endothelial pathology is also strongly associated with mitochondrial dysfunction and oxidative stress [33,135]. Many signaling pathways in inflammation are regulated by mitochondria and may have a role in COVID-19 pathology [33,136]. Mitochondrial reactive oxygen species (ROS) are potent oxidizers that can directly damage DNA, proteins, and lipids or activate downstream pathways that promote inflammation and endothelial dysfunction [13,137]. The infection of ECs by SARS-CoV-2 might contribute to mitochondrial dysfunction and enhanced oxidative stress, possibly initiating a feedback loop that promotes chronic inflammation and endothelial damage even after the virus has been cleared. Furthermore, oxidative stress and mitochondrial failure are associated with premature senescence of ECs, characterized by shortened telomeres, cell growth arrest, secretion of inflammatory cytokines, and growth factors [138]. Specifically, the NLRP3 inflammasome can be activated by ROS from dysfunctional mitochondria and is associated with EC senescence [139]. Cellular senescence in turn might have an impact on the regulation of ACE and the expression of ACE2, exhibiting a higher ACE/ACE2 ratio and thereby increasing susceptibility to SARS-CoV-2 [33]. Furthermore, COVID-19 infection can lead not only to mitochondrial dysfunction but may also facilitate the senescence of the host cell. These changes are irreversible, which is particularly relevant for patients recovered from COVID-19 disease [33]. Senescence promotes apoptosis and negatively affects nitric oxide synthase activity, thus increasing the risk of vascular damage and endothelial leakage [140]. The senescence-induced loss of nitric oxide would explain the results of Varga et al., who found patterns consistent with EC apoptosis in COVID-19 patients [31].
Notably, SARS-CoV-2 can induce endothelial-to-mesenchymal transition (EMT) in ECs characterized by the complete loss of endothelial features and acquisition of a fibroblast-like phenotype. This dedifferentiation process may involve TGF-β, a cytokine that is significantly increased in COVID-19 patients [33,141,142]. Consequently, a better mechanistic understanding of how SARS-CoV-2 affects ECs is necessary for the development of efficient therapeutic strategies for COVID-19 patients, particularly those suffering from CVD.
SARS-CoV-2 infection of endothelial cells?
Viruses of many families can lead to endothelial infection and dysfunction, some of them involving cell adhesion molecules acting as receptors [28,35,124–126,130]. In turn, the activation of ECs may result in increased expression of adhesion molecules, such as ICAM-1, VCAM-1, E-selectin, P-selectin, MCP-1, and von Willebrand factor, thus enhancing the immune reaction and accumulation of inflammatory cells within the arterial wall [23,29,30,75,116].
Evidence that ECs are infected by SARS-CoV-2 comes from thin section analyses by electron microscopy [25,31,42,87]. For instance, Varga et al. found viral particles in ECs across vascular beds in different organs from COVID-19 patients [31]. Furthermore, other histological analyses of COVID-19 patients demonstrated that the increase in the inflammatory reaction is mainly associated with the dysfunctional endothelium, as well as with apoptotic bodies and cell death [22,42–44]. From these data, the authors suggested that SARS-CoV-2 can directly infect ECs. Notably, other studies found no evidence of viral particles in ECs using in situ hybridization or immunohistochemistry (IHC) on ex vivo tissue samples from patients with COVID-19 [28,43]. These results are not surprising given the sparsity of SARS-CoV-2 infected cells in the respiratory epithelium, which represents the entry gate for the virus into the body [116]. Further discrepancies have been observed between SARS-CoV-2 tropism and the cellular distribution of ACE2 and TMPRSS2 [43]. In addition, Bradley et al. found SARS-CoV-2-like particles post-mortem from COVID-19 patients only in renal ECs but not in other organs or arteries [143]. Another study using IHC ex vivo and in cell cultures did not detect any viral remnants in the vascular endothelium [45]. Yang et al. have reported that ECs derived from pluripotent stem cells are widely resistant to SARS-CoV-2 infection [46]. Furthermore, using in situ hybridization of liver biopsies, no viral particles were detected in the corresponding ECs [7]. It is thus not clear if thin-section electron microscopy in absence of immunostaining is able to unequivocally identify SARS-CoV-2-like particles [8,40,41,144]. High-resolution cryo-EM tomography might be required to identify the SARS-CoV-2 like structures. For example, Bernard et al. infected healthy human lung microvascular cells with SARS-CoV-2 in vitro and detected only modest viral RNA levels, indicating that ECs might be only moderately permissive to SARS-CoV-2 infection, even if they express both ACE2 and TMPRSS2 [28]. In other experiments, Hou et al. did not find any GFP-positive cells using the SARS-CoV-2-GFP reporter virus and human primary lung ECs [145]. Consequently, whether SARS-CoV-2 infects ECs has not yet been clarified and further studies are necessary.
Only a few studies focused on human ECs and a handful of them reported on the SARS-CoV-2 entry or expression of ACE2 [54,55,60,100,146–157]. In these studies, commercially available pulmonary, aortic, umbilical, or cardiac primary ECs were applied. So far, the results have been controversial, emphasizing the necessity of further research to clarify the impact of SARS-CoV-2 on ECs, particularly in CVD patients, in order to account for conditions of increased oxidative stress, inflammatory cytokines, reduced vasodilation and antithrombotic features, reflecting atherosclerotic changes within the arterial wall [13,135,158–160].
For instance, in vitro infections of HUVEC, microvascular endothelial cells (HLMVEC), coronary artery endothelial cells (HCAEC), and pulmonary arterial cells (HPAEC) with SARS-CoV-2 revealed no intracellular double-stranded viral RNA [150]. Furthermore, following SARS-CoV-2 infection, no intracellular double-stranded viral RNA was detected by immunofluorescence [161]. Using in situ hybridization, Targosz-Korecka et al. found no evidence for viral genomes in hepatic or endothelial cells [154]. The authors suggested that endothelial glycocalyx might shield the interaction of the SARS-CoV-2 S protein with the ACE2 receptor, thus protecting ECs from infection. This, however, contrasts the notion that SARS-CoV-2 efficiently infects highly polarized, well-differentiated human nasal and bronchial epithelial cells grown at the air–liquid interface even in presence of copious amounts of viscous mucus [162,163]. Potie at al. showed that blood plasma from COVID-19 patients facilitates glycocalyx shedding in ECs [155].
The evidence for the expression of ACE2, the main receptor for SARS-CoV2, on ECs is controversial [42]. Various studies and database searches have found only low expression of ACE2 receptor in human endothelial cells [25,42,87], even if ACE2 expression generally increases with age [164,165]. Nascimento Conde et al. found that healthy primary human ECs frequently lack the ACE2 receptor and resist SARS-CoV-2 infection. However, they become infected upon ectopic ACE2 expression indicating that either ECs are not primary targets of SARS-CoV-2 infection or ACE2-independent entry mechanisms are involved [146].
Regarding CVD, some studies suggested that ACE2 is significantly up-regulated in atherosclerotic ECs and in the elderly suggesting an aging-associated up-regulation of ACE2 [164–166]. Low-grade chronic inflammation has already been recognised as an important feature of aging, favoring the onset of various age-related diseases. These data might explain the higher risk and greater severity of COVID-19 disease observed in older individuals. Similar to the low-grade inflammation observed in the elderly, inflammatory reactions in COVID-19 pathogenesis, such as the up-regulation of IL1β and IFN-α, have been reported to stimulate ACE2 expression [104,105,107,123,164,165]. Taken together, further studies on COVID-19 both in vivo with CVD patients and ex vivo using vascular cells from different age groups are necessary to validate these hypotheses.
In summary, the global dysfunction of ECs together with the total or partial collapse of the endothelial barrier represents the critical step in the development of a severe course of COVID-19 disease contributing at the end to multiorgan failure and sepsis [116]. Due to the detachment and release of infected ECs into the circulation, SARS-CoV-2 infected ECs may disseminate and reach also other distant organs. Endothelial damage in turn leads to increased coagulation and other thrombotic events.
COVID-19 and smooth muscle cells
Vascular SMCs are found in the tunica media and represent the most abundant cell type in the arterial wall [142]. They participate in vessel wall remodelling, provide mechanical strength and elasticity, regulate vascular tone and resistance, and connect vessels with the extracellular matrix [167,168]. SMCs play a pivotal role in CVD and atherosclerosis [169]. Phenotypic switching, apoptosis, necrosis, and the transdifferentiation of SMCs into macrophage-like or osteoblast-like cells significantly contribute to the disease progression through a weakening of the arterial wall [119]. SMCs are the most important cells synthesizing various components of the extracellular matrix to counteract their degradation by proteolytic enzymes activated in atherosclerosis.
As described above, RAS plays a key role in the regulation of vascular tone and in maladaptive vascular remodeling [105–110]. Consequently, RAS is tightly connected with the physiological function of SMCs [170,171]. It is generally accepted that the RAS has a dual function. On the one hand, there is an axis consisting of ACE-2/Ang (1-7)/MasR3 that exerts anti-inflammatory, antiproliferative, vasodilatory, and cardiovascular protective effects. The protective aspects of ACE2 are partly due to the down-regulation of various matrix metalloproteinases (MMPs) [170]. ACE2 deficiency in ApoE knockout mice deficient for ACE2 resulted in increased atherosclerosis and overexpression of MMP-2 and -9, destabilizing the vascular wall [172]. On the other hand, through the classical axis includingACE/Ang II/AT1 receptor (AT1R) and AT2 receptor (AT2R), it promotes inflammation, vasoconstriction, and fibrosis. Thereby, the Ang II effect is mediated through Ang II receptor type 1 (AT1) and 2 (AT2), leading to vasoconstriction and increasing cell proliferation, thus having favorable effects on the function of SMCs. The cross-talk between AT1R and AT2R has been described to have a significant effect on the cardiovascular system [170,171]. Consequently, the inhibition of the Ang II/AT1 signaling is an important pharmacological tool to prevent CVD related to vascular remodeling and might also improve the outcome of COVID-19 patients suffering from CVD. For instance, AT1 receptor blocker improves the effect of ACE2, thus increasing cardiovascular remodeling and normalizing fibrosis-associated signaling pathways in CVD [171]. The ACE2 inhibitors and AT1R blockers are considered the first-line treatment for patients with hypertension, suggesting their beneficial effects on the cardiovascular system under pathological conditions. Consequently, ACE2 treatment appears a promising target also for the management of patients with COVID-19, particularly those suffering from CVD. The activation of the Ang (1-7)/MAS receptor (MasR) axis may improve the physiological function of SMCs and vascular remodelling, being favourable in hypertensive patients infected by SARS-CoV-2 [171]. Savoia at al. suggest that independently of AT2R activation, MasR stimulation may contribute to the beneficial effects of ACE inhibitors or AT1R blockers on the pathological artery remodeling under hypertensive conditions.
Interestingly, RAS is also responsible for the regulation of ADAM17 expression. ADAM17-dependent ACE2 shedding is induced by Ang II via AT1R as well as by SARS-CoV-2 [173–175]. Following RAS activation, ADAM17 is up-regulated, leading to enhanced ectodomain shedding of ACE2 and increasing the soluble form of ACE2 in blood circulation [176]. The role of ACE2 shedding under physiological and pathological conditions is still insufficiently understood. Increased ADAM17 activity was detected in CVD, hypertension, diabetes mellitus, neurological, and oncological diseases [173,177].
In SMCs, ADAM17 is primarily responsible for the shedding of the epidermal growth factor receptor (EGFR) trans-activation induced by Ang II [178]. The ADAM17/EGFR signaling axis is one of the most key events by which RAS through Ang II affects vascular remodeling [179]. For instance, in AAA a significant up-regulation of ADAM17 was reported [180]. Deletion of ADAM17 in a mice model prevented AAA formation through attenuation of oxidative stress, inflammation, and extracellular matrix disruption [179]. Genome-wide transcriptional profiling identified AT1, ADAM17, and EGFR as important factors associated with vascular disorders induced by Ang II. Thus, ADAM17 represents potential therapeutic target for the prevention of CVD. In this context it is to mention that, despite low ACE2 expression, patients with CVDs have still higher COVID-19 mortality, caused probably by the imbalance between ADAM17 expression required for cleavage of ACE2 for virus uptake, and TMPRSS2, which is required for spike glycoprotein priming. Even if ACE inhibitors or AT1R blockers are well-established in the treatment of hypertension and other cardiovascular complications, their inhibition in patients with chronic comorbidities appears at the moment unjustified or at least questionable [152,177]. Further studies are necessary to evaluate the impact of ACE2 and AT1R inhibitors on the outcome of COVID-19 patients suffering from CVD. A critical aspect in the maintenance of the biological function of arteries is the cross-talk between ECs and SMCs. Aberrant EC–SMC communication is associated with various diseases, including atherosclerosis [169]. The cross-talk between SMCs and ECs is reciprocal. Alterations in SMCs may also change EC morphology and the expression of EC-specific genes [28,120]. Endothelial dysfunction is associated with changes in nitric oxide bioavailability and the release of various vasoactive compounds, conditions found when SARS-CoV-2 infects or affects ECs. This process may directly affect the function of SMCs and contribute to the severity of cardiovascular outcomes in COVID-19 patients. In this context, phosphodiesterase type 5 inhibitors (tadalafil) and estrogens increase the formation of endogenous nitric oxide and might thus exhibit a protective effect of these drugs in severe cases of COVID-19 [181].
Interestingly, despite the importance of SMCs in the maintenance of arterial function and the underlying pathologies, there are no data on the role of these vascular cells in COVID-19 patients suffering from CVD. Likewise, it is unknown whether SARS-CoV-2 can directly infect SMCs or whether and how far SMCs are affected by the dysfunctional ECs.
Only a handful of articles have explored the role of SMCs in the context of COVID-19 [148,182–187]. One of them focused exclusively on the expression of ACE2 in ECs, mentioning SMCs only on the side [183]. Marchiano et al. showed that human pluripotent stem cell-derived SMCs can be infected by SARS-CoV-2 [184]. Suzuki et al. treated pulmonary artery SMCs with the SARS-CoV-2 S protein [148], and the last study explored the effect of estrogen and testosterone on the expression level of ACE2 in human airway SMCs [183]. In the context of SMCs, it is again important to mention that there are significant differences in the expression levels of ACE2 between healthy and atherosclerosis-derived vascular cells [182]. Taken together, little is known about the role of SMCs in COVID-19 disease, particularly in patients suffering from CVD. Further studies are necessary, using e.g. CVD patient-derived vascular cells.
In this context, it is to note that SMCs in patients with CVD may be directly exposed to SARS-CoV-2. In advanced atherosclerotic lesions or aneurysms, the endothelial layer is largely damaged, enabling access of SARS-CoV-2 into the vessel wall to infect also the underlying SMCs, which express ACE2 [122,149]. Furthermore, the down-regulation of ACE2 in SARS-CoV-2-infected ECs leads to endothelial leakage and increased permeability, thus potentially allowing viral particles to access SMCs through the vessel wall [126,188]. Suzuki et al. [148] treated pulmonary artery SMCs with a recombinant SARS-CoV-2 spike protein S1 causing activation of cell growth signaling. These findings are consistent with the thickening of the pulmonary vascular wall in COVID-19 patients. By infecting human pluripotent stem cell-derived cardiomyocytes and SMCs with SARS-CoV-2, Marchiano et al. [184] observed only marginal viral entry in SMCs. On contrary, cardiomyocytes were heavily infected. SARS-CoV-2 infection of cardiomyocytes impaired their electrophysiological and contractile function and frequently led to cardiomyocyte death. These results are in line with the severe cardiac symptoms in COVID-19 patients, particularly suffering from CVD.
In addition, the role of pericytes, precursors of SMCs, is not to be neglected. Pericytes are mural multifunctional cells surrounding ECs of capillaries [189]. They contribute to maintaining hemostatic functions of the endothelium, stabilizing small vessels, and regulating the capillary blood flow. As mentioned above, single-cell RNAseq studies demonstrated that unlike healthy ECs, pericytes and SMCs express high levels of ACE2 [42]. Accordingly, immunohistochemical staining of capillaries might confuse ACE2-positive pericytes or SMCs with ECs. These results support again the indirect activation of ECs by SARS-CoV-2 infecting neighbouring cells, platelets, and inflammatory cells.
Currently, the role of pericytes and SMCs in COVID-19 disease is unclear. Khaddaj-Mallat et al. [185] reported that expression of ACE2 in brain vascular pericytes is significantly increased following interaction with S protein. These infected pericytes underwent profound phenotypic changes expressing more contractile and myofibrogenic proteins. In addition, the spike protein induced oxidative stress, similar to the immune reaction activated by NF-κB signaling pathway supporting hypoxia. All these features are associated with pathomorphology in COVID-19 patients. Furthermore, Tzankov at al. [187] reported that SMCs of COVID-19 patients exhibited increased expression and density of various chondroitin sulfates. These conditions might contribute, e.g., to arterial stiffness. Zhang et al. [186] reported that airway smooth muscles can also be infected by SARS-CoV-2. These cells are stimulated by IL-13 and IL-17, affecting their fate and phenotype. Thus, airway smooth muscles and pro-inflammatory factors may play an important role in the progression and severity of COVID-19 course.
Finally, it remains an open question whether infection of ECs by SARS-CoV-2 might also change the expression profile of SMCs or facilitate their trans-differentiation, a process, which is tuned by interactions between ECs and SMCs [169]. Thus, whether SMCs can be directly infected by SARS-CoV-2 or are indirectly affected by EC signaling and inflammatory response following COVID-19 is yet to be elucidated.
The role of long noncoding RNAs in viral infection
Cell-to-cell variability of virus infection has been a major unexplained feature in infectious diseases [190]. In recent years, increasing evidence has demonstrated a crucial role of particularly long noncoding RNAs (lncRNAs, >200 nt) in various biological processes, such as epigenetic modification, regulation of transcriptional as well as post-transcriptional gene expression, and aging [58–60,191–193]. Specific interactions of lncRNAs with DNA, mRNA and proteins can modulate chromatin function, mRNA stability and translation as well as cell signaling. LncRNAs also contribute to the severity of CVD [59,60,194–196]. Multiple studies have shown that lncRNA significantly influence vascular permeability, proliferation, migration, phenotypic switching, and apoptosis in the context of vascular dysfunction well as crosstalk between ECs and SMCs [58,61,62,196–198].
LncRNAs may also be of importance in the regulatory network controlling virus entry, innate immunity and infection, as shown for HIV, hepatitis B virus, influenza virus or hepatitis C virus, for example [64,65,199,200]. In particular, lncRNAs have been observed to regulate the expression of interferon (IFN) stimulated genes (ISGs), targeting the corresponding upstream transcription factors and acting through epigenetic modifications [64,200]. For instance, IFN-α induces the expression of lncRNAs lncBST2 and lncISG15, which are positive regulators of the IFN-stimulated genes [201]. On the contrary, e.g. lncRNA NRAV has been found as a negative regulator of antiviral response, promoting the replication of the influenza virus [67].
Regarding their potential protective antiviral function, lncRNAs can bind to the complementary sequences of viral RNA, forming a double-stranded RNA, which is then degraded by the internal RNA-induced silencing complex (RISC) [202]. In general, lncRNA/viral RNA interactions can either repress the viral mRNA translation and inhibit viral replication, or stabilize the viral RNA, enhancing the viral replication [203–205].
A variety of human viruses, such as herpes simplex virus (HSV) [206,207], human immunodeficiency virus (HIV) [206], hepatitis B virus (HBV) [207,208], and SARS-CoV [201] have been shown to dysregulate the expression of several host lncRNAs, increasing infectivity. Among them, the lncRNA HULC (highly up-regulated in liver cancer) and HEIH (highly expressed in HCC) have been reported to play important roles in HBV-related carcinogenesis. Furthermore, HIV infection has been shown to up-regulate the lncRNA nuclear paraspeckle assembly transcript 1 (NEAT1) expression [206]. NEAT1 is essential for the integrity of the nuclear paraspeckle substructure, which is an important subcellular organelle for HIV-1 replication. In addition, the lncRNA called metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) has been up-regulated in HIV-infected T-cells and macrophages, affecting apoptosis of these cells [210,211].
Regarding the innate immune system in the host antiviral response, lncRNA#32 was observed to regulate the expression of ISGs and IFN signaling [63]. Repression of lncRNA #32 significantly increased susceptibility to encephalomyocarditis virus and HBV. In particular, the expression of several chemokines and innate immune response genes was significantly repressed in the lncRNA #32 depleted cells. Other studies demonstrated that the lncRNA negative regulator of antiviral response (NRAV) was highly expressed in cells infected with influenza A virus (IAV) [67]. Furthermore, following infection with HIV or hantavirus, lncRNA NEAT1 interaction with other proteins and transcription factors has been found to repress the IFN-associated genes, facilitating infections [212,213]. Here is to note that many of these lncRNAs, such as NEAT1, MALAT1, and H19 play an important role also in CVD and atherosclerosis [58–60].
It is also worth mentioning that RNA viruses manipulate and hijack the host lncRNAs to promote their replication [199]. For instance, lncRNA–ACOD1 reduces antiviral innate response and is induced by various animal viruses, including Sendai virus, a severe pathogen of mice, and vesicular stomatitis virus infecting equidae, sheep and goat. Following infection, the viral machinery may not only alter the expression pattern to augment the cell conditions for virus replication and dissemination but also avoid and down-regulate the immune response [203,214].
The role of long noncoding RNAs in vascular dysfunction of COVID-19
As described above, virus infection of host cells changes not only the expression pattern of many lncRNAs but also plays an essential role in antiviral immunity. Thus, the susceptibility to SARS-CoV-2 infection might be defined not only by the surface proteins such as ACE2 and TMPRSS2 but also by the expression of host-derived lncRNAs [215]. In the context of SARS-CoV, infection of various mouse strains (PWK/PhJ (PWK), CAST/EiJ (CAST), 129S1/SvImJ (129/S1), and WSB/EiJ (WSB) mice) appears to be associated with differential expression of several hundred lncRNAs [208]. Most changes correlated with the activation of the IFN response, akin to broad IFN-dependent and independent anti-viral effects of short blunt end double-stranded RNAs [216]. One of these lncRNAs involved in antiviral response was NeST, and it was associated with altered histone methylation of the IFNG promoter, and stimulating IFN-γ gene expression [217]. These data suggest that lncRNAs may particularly affect antiviral responses through the transcriptional activation of IFN-associated genes by recruiting transcription and epigenetic factors.
Emerging clinical evidence suggest that lncRNAs play a decisive role in COVID-19 patients [218–226]. These articles mainly focused on the analysis of lncRNAs as circulating biomarkers in blood using existing genomic databases [219,222–224]. For instance, Li et al. performed whole transcriptome analysis of peripheral blood samples and identified 23 differentially expressed miRNAs and 410 differentially expressed lncRNAs in the COVID-19 samples compared with healthy controls [223]. MALAT1, NEAT1, HOTAIRM1 (HOX transcript antisense RNA M1), VDR (vitamin D receptor), and SNHG6 (small nucleolar RNA host gene 6) were among the identified lncRNAs, and they were confirmed by other studies [209,218,220,221]. These bioinformatic analyses of pre-existing genomic data revealed dysregulation of miRNA/lncRNA interactions and their effects on ACE2 and TMPRSS2 [219], indicating that some lncRNAs might contribute to the regulation of the expression of these infection regulators at the cell surface and thus has an influence on SARS-CoV-2 susceptibility.
Regarding EC dysfunction in COVID-19 patients, short non-coding RNA miR-200c regulating the expression of ACE2 was reported [224]. This goes along with reports at patient levels showing that lncRNA H19 can bind to this family of miRNAs, reducing their availability in the host cell, leading to higher responsiveness to SARS-CoV-2 [226]. To identify cellular pathways during SARS-CoV-2 infection, another study analyzed transcriptome data from human bronchial epithelial cells (NHBE) infected with SARS-CoV-2 [225]. Activating the innate immune response has been shown to up-regulate IFN-responsive genes in particular. Interestingly, changes in the expression of MALAT1 and NEAT1 have also been observed [225]. However, in the context of COVID-19 and the dysfunction of ECs and SMCs, no studies on lncRNAs have been reported so far.
COVID-19 and the role of endothelial infection in CVD
COVID-19 patients suffering from CVD have a more than 5-fold increased risk of mortality [37]. These individuals are having atherosclerotic plaques and thus are more vulnerable to plaque activation and risk of cardiovascular failure [16,22]. Furthermore, current evidence suggest that COVID-19 is an endothelial disease and that EC dysfunction triggers various associated factors causing excessive inflammation, oxidative stress, coagulopathy, platelet and fibrinogen activation, and thromboembolism [13,95,130,227–230]. Current data indicate that endothelial dysfunction is not limited to the lungs but can be considered a whole-body disease. Approximately 5% of COVID-19 patients develop multiple organ failure and excessive immune response [72,74,158]. Various studies have shown that COVID-19 patients have more often not only pulmonary embolism but also venous thromboembolism with up to 70% [37,95,228,229]. Other associated complications have been observed as well: acute kidney injury, coagulation disorders, and electrolyte disturbances [37,75,128]. Interestingly, most of the cardiac injuries in COVID-19 patients occurred in the absence of coronary thrombosis and were associated with myocarditis, cardiomyopathy, arrhythmias, and inflammatory cytokine dysregulation [37,96]. In addition, it has been reported that COVID-19 patients can develop new cardiovascular events, such as right and left diastolic dysfunction, indicating the involvement of small coronary capillaries [11,231]. The observed diastolic dysfunction was also attributed to nonischemic myocarditis [39,232]. Even if the cardiac complications are associated with the various stages of EC dysfunction, the underlying mechanisms are not sufficiently understood.
Furthermore, SARS-CoV-2 infection may accelerate atherosclerotic plaque formation toward a vulnerable state and vascular thrombosis. Hypertension, obesity, and diabetes mellitus, frequently accompanying patients with CVD, have already been considered risk factors for severe COVID-19 course [12,24,233]. A recent meta-analysis with 125,446 patients found that the most common comorbidity was hypertension (32%), followed by obesity (25%), diabetes (18%), CVD (16%), lung disease (9%), and chronic kidney disease (6%) [15,135]. Additional risk factor associated with the death of patients with COVID-19 is older age [234]. The comorbidity in the elderly significantly correlates with a high level of D-dimer. More than 20% of COVID-19 patients with severe course have higher blood pressure (HBP) rates exceeding 50% [23]. The contribution of hypertension to the morbidity and mortality in COVID-19 is however still unclear. High blood pressure (>50%) affects various components of cell-mediated immunity that are normally protective against viral infections [23]. Furthermore, hypertension stimulates overexpression of various cytokines, particularly interferon (IFN)-γ and TNF-α [32,74,158]. These cytokines affect renal epithelium and raise blood pressure by increasing oxidative stress and renal sodium reabsorption [23]. Plasma levels of IL-6 are also associated with hypertension as well as higher morbidity of COVID-19 patients [235]. Increased blood pressure predisposes also endothelial injury. Further accompanying diseases of COVID-19 are frequently endotheliitis and vasculitis, however, not only in the pulmonary tract but also in other organs such as kidney [26,31], liver ]31], intestine [127], or heart [128]. In addition, vascular occlusion, stiffness, and altered reactivity have been reported [26,73,236].
Interestingly, venous complications in COVID-19 patients have been more often described than e.g. arterial complications such as on the peripheral arterial system [37,95,229]. Even if it seems that only less than 1% of COVID-19 patients develop systemic arterial thrombotic events, the mortality is high with up to 30% [37]. Thromboembolism in peripheral vessels is less predictable in patients infected by SARS-CoV-2 than in the usual atherosclerotic patients suffering from peripheral arterial disease (PAD). In addition, COVID-19 patients experience more frequently ischemic stroke, with an incidence of 0.05–5.7% [21,37,95–97].
The dysregulation of the normal functions of ECs in COVID-19 patients contributes also to the thrombo-inflammatory storm, formation of blood clot, diffuse coagulopathy, and multiple organ failure, which are frequently associated with mortality and severe course of the disease [36]. These pathologies affect not only the lung capillaries but also to other blood vessels. COVID-19 disease has been described as being accompanied by arterial and venous thrombotic events, particularly in patients suffering from CVD [95,116,237]. Up to 30% of COVID-19 patients admitted to the intensive care unit acquired various thrombotic complications [74,131,237]. The pathophysiology of coagulopathy associated with COVID-19 disease involves several pathways. The initial trigger is mainly the systemic inflammatory response following SARS-CoV-2 infection, activating various coagulation pathways. Accordingly, COVID-19 patients showed increased fibrinogen and D-dimer levels [116,227]. Interestingly however, only a few patients with COVID-19 developed disseminated intravascular coagulation, compared with patients with septic shock (30–40%). The endothelial damage can be further facilitated by very high levels of von Willebrand factor (VWF) in the blood circulation, which in turn contributes to the high inflammatory reaction following SARS-CoV-2 infection [238]. Furthermore, the severe course of COVID-19 leads to hypoxemic pneumonia and hypoxemia in the pulmonary capillaries, resulting in vasoconstriction. Vessel narrowing reduces in turn blood flow in the arteries, thereby facilitating vascular occlusion [116]. In addition, vascular thrombosis and vasculitis have been frequently described as common post mortem pathological findings in COVID-19 patients [14,32].
In summary, the global dysfunction of ECs together with the total or partial collapse of the endothelial barrier represents the critical step in the development of the severe course of COVID-19 disease, leading to multiorgan failure and sepsis [116]. The underlying pathomechanism is the endothelial dysfunction and activation of various inflammatory and adhesive molecules in or through changes in the expression pattern of ECs. The detachment of SARS-CoV-2 infected ECs may disseminate the virus through the circulation and reach other distant organs. These cells can in turn contribute to various thromboembolic events. Nevertheless, it is still unclear how vascular ECs are targeted by SARS-CoV-2. Moreover, it is unknown, how SARS-CoV-2 contributes to vascular complications and where is the link between cardiovascular risk factors such as ageing and accompanying diseases and COVID-19 pathologies.
Conclusion
Although COVID-19 is primarily a respiratory disease, it has a significant impact on the cardiovascular system, and vice versa, a dysregulated cardiovascular system appears to exacerbate COVID-19. Particularly COVID-19 patients with CVD frequently develop more severe and complicated disease course than patients without CVD. A common denominator of CVD is the dysfunction of vascular cells, increased permeability, endothelial-to-mesenchymal transition, inflammation, and coagulation. It has been assumed that clinical complications are due to SARS-CoV-2 infection of ECs through the ACE2 receptor pathway. However, recent studies have shown significant discrepancies and controversial results, suggesting that noncanonical viral interference or immune reactions with ECs may account for EC dysfunction. Such processes might comprise alternative cell entry pathways of SARS-CoV-2, e.g. involving ADAM17, HSPG, sialic acid, NRP or CD209L, although further studies are required to support such assumption. Regardless, vascular dysfunction in CVD patients might facilitate and accelerate viral entry and infection of damaged ECs and also SMCs. Consequently, it is important to explore the infection mechanism in vascular cells in the context of cardiovascular disorders. Likewise, the role of SMCs in COVID-19 merits further investigations. Other promising areas are diagnostic and therapeutic approaches against COVID-19, in particular considering lncRNAs in the context of CVD. Notably, the importance of lncRNAs is increasingly appreciated, also due to advances in RNAseq technology and single cell analyses addressing mechanisms of infections by considering the ubiquitous nature of cell-to-cell variability [190]. Such approaches might further illuminate the role of lncRNAs in SARS-CoV-2 infection and open new opportunities for drug and therapeutic strategies, particularly in the context of CVD.
Abbreviations
- ACE2
angiotensin-converting enzyme 2
- ADAM17
disintegrin and metalloproteinase domain-containing protein 17
- APN
alanine aminopeptidase
- AT1R
AT1 receptor
- AT2R
AT2 receptor
- COPD
chronic obstructive pulmonary disease
- CoV
coronavirus
- COVID-19
coronavirus disease 2019
- CRP
C-reactive protein
- CVD
cardiovascular disorder
- DMV
double-membrane vesicle
- DPP4
dipeptidyl peptidase-4
- EC
endothelial cell
- EGFR
epidermal growth factor receptor
- ENaC
epithelial sodium channel-α
- FGF-2
fibroblast growth factor-2
- HBV
human hepatitis B virus
- HCAEC
human coronary artery endothelial cell
- HIV
human immunodeficiency virus
- HLMVEC
human lung microvascular endothelial cell
- HPAEC
human pulmonary arterial cell
- HSPG
heparan sulphate proteoglycans
- HUVEC
human umbilical vein endothelial cell
- IAV
influenza A virus
- ICAM-1
intercellular adhesion molecule 1
- IL
interleukin
- INF
interferon
- lncRNA
long noncoding RNA
- MALAT1
metastasis-associated lung adenocarcinoma transcript 1
- MasR
MAS receptor
- MCP-1
monocyte chemoattractant protein-1
- NEAT1
nuclear assembly transcript 1
- NET
neutrophil extracellular trap
- NRP1
neuropilin-1
- ROS
reactive oxygen species
- SAA
serum amyloid A
- SARS
severe acute respiratory syndrome
- SMC
smooth muscle cell
- TMPRSS2
transmembrane protease serine subtype 2
- TNF-α
tumor necrosis factor α
- VCAM-1
vascular cell adhesion molecule 1
- VEGF
vascular endothelial growth factor
Data Availability
No datasets have been used in producing this work.
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
SARS-CoV-2 research in the Greber lab has been supported by the Swiss National Science Foundation [grant number 31CA30_196177 / 1] and a special grant from the University of Zurich.
CRediT Author Contribution
Jaroslav Pelisek: Conceptualization, Writing—review & editing. Benedikt Reutersberg: Writing—review & editing. Urs Greber: Writing—review & editing. Alexander Zimmermann: Writing—review & editing.
References
- 1.Drosten C., Günther S., Preiser W., van der Werf S., Brodt H.R., Becker S.et al. (2003) Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N. Engl. J. Med. 348, 1967–1976 10.1056/NEJMoa030747 [DOI] [PubMed] [Google Scholar]
- 2.Rabi F.A., Al Zoubi M.S., Kasasbeh G.A., Salameh D.M. and Al-Nasser A.D. (2020) SARS-CoV-2 and coronavirus disease 2019: what we know so far. Pathogens 9, pii: E231 10.3390/pathogens9030231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. International Committe of Taxonomy of Viruses (ICTV): Report 9th (2009), Coronaviridae ( https://ictv.global/report_9th/RNApos/Nidovirales/Coronaviridae)
- 4.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J.et al. (2020) China novel coronavirus investigating and research team. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X.et al. (2020) China medical treatment expert group for Covid-19. Clinical characteristics of coronavirus disease 2019 in china. N. Engl. J. Med. 382, 1708–1720 10.1056/nejmoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y.et al. (2020) Early transmission dynamics in Wuhan, China of novel coronavirus-infected pneumonia. N. Engl. J. Med. 382, 1199–1207 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fassan M., Mescoli C., Sbaraglia M., Guzzardo V., Russo F.P., Fabris R.et al. (2021) Liver histopathology in COVID-19 patients: a mono-institutional series of liver biopsies and autopsy specimens. Pathol. Res. Pract. 221, 153451 10.1016/j.prp.2021.153451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Calomeni E., Satoskar A., Ayoub I., Brodsky S., Rovin B.H. and Nadasdy T. (2020) Multivesicular bodies mimicking SARS-CoV-2 in patients without COVID-19. Kidney Int. 98, 233–234 10.1016/j.kint.2020.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li M., Dong Y., Wang H., Guo W., Zhou H., Zhang Z.et al. (2020) Cardiovascular disease potentially contributes to the progression and poor prognosis of COVID-19. Nutr. Metab. Cardiovasc. Dis. 30, 1061–1067 10.1016/j.numecd.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee I.C., Huo T.I. and Huang Y.H. (2020) Gastrointestinal and liver manifestations in patients with COVID-19. J. Chin. Med. Assoc. 83, 521–523 10.1097/JCMA.0000000000000319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ejaz H., Alsrhani A., Zafar A., Javed H., Junaid K., Abdalla A.E.et al. (2020) COVID-19 and comorbidities: deleterious impact on infected patients. J. Infect. Public Health 13, 1833–1839 10.1016/j.jiph.2020.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gao Y.D., Ding M., Dong X., Zhang J.J., Kursat Azkur A.et al. (2021) Risk factors for severe and critically ill COVID-19 patients: a review. Allergy 76, 428–455 10.1111/all.14657 [DOI] [PubMed] [Google Scholar]
- 13.Libby P. and Lüscher T. (2020) COVID-19 is, in the end, an endothelial disease. Eur. Heart J. 41, 3038–3044 10.1093/eurheartj/ehaa623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Menter T., Haslbauer J.D., Nienhold R., Savic S., Hopfer H., Deigendesch N.et al. (2020) Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology 77, 198–209 10.1111/his.14134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thakur B., Dubey P., Benitez J., Torres J.P., Reddy S., Shokar N.et al. (2021) A systematic review and meta-analysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19. Sci. Rep. 11, 8562 10.1038/s41598-021-88130-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corrales-Medina V.F., Madjid M. and Musher D.M. (2010) Role of acute infection in triggering acute coronary syndromes. Lancet Infect. Dis. 10, 83–92 10.1016/S1473-3099(09)70331-7 [DOI] [PubMed] [Google Scholar]
- 17.Guo T., Fan Y., Chen M., Wu X., Zhang L., He T.et al. (2020) Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 5, 811–818 10.1001/jamacardio.2020.1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S.et al. (2020) Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 180, 934–943 10.1001/jamainternmed.2020.0994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sardu C., Gambardella J., Morelli M.B., Wang X., Marfella R. and Santulli G. (2020) Hypertension thrombosis kidney failure and diabetes: is COVID-19 an endothelial disease? A comprehensive evaluation of clinical and basic evidence J. Clin. Med. 9, 1417 10.3390/jcm9051417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Behzad S., Aghaghazvini L., Radmard A.R. and Gholamrezanezhad A. (2020) Extrapulmonary manifestations of COVID-19: Radiologic and clinical overview. Clin. Imaging 66, 35–41 10.1016/j.clinimag.2020.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ellul M.A., Benjamin L., Singh B., Lant S., Michael B.D., Easton A.et al. (2020) Neurological associations of COVID-19. Lancet Neurol. 19, 767–783 10.1016/S1474-4422(20)30221-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bonow R.O., Fonarow G.C., O'Gara P.T. and Yancy C.W. (2020) Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardio. 5, 751–753 10.1001/jamacardio.2020.1105 [DOI] [PubMed] [Google Scholar]
- 23.Dayaramani C., De Leon J. and Reiss A.B. (2021) Cardiovascular disease complicating COVID-19 in the elderly. Medicina (Kaunas). 57, 833 10.3390/medicina57080833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang C., Liu F., Liu W., Cao G., Liu J., Huang S.et al. (2021) Myocardial injury and risk factors for mortality in patients with COVID-19 pneumonia. Int. J. Cardiol. 326, 230–236 10.1016/j.ijcard.2020.09.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maruhashi T. and Higashi Y. (2021) Pathophysiological association of endothelial dysfunction with fatal outcome in COVID-19. Int. J. Mol. Sci. 22, 5131 10.3390/ijms22105131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ma Z., Yang K.Y., Huang Y. and Lui K.O. (2022) Endothelial contribution to COVID-19: an update on mechanisms and therapeutic implications. J. Mol. Cell Cardiol. 164, 69–82 10.1016/j.yjmcc.2021.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nägele M.P., Haubner B., Tanner F.C., Ruschitzka F. and Flammer A.J. (2020) Endothelial dysfunction in COVID-19: current findings and therapeutic implications. Atherosclerosis 314, 58–62 10.1016/j.atherosclerosis.2020.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernard I., Limonta D., Mahal L.K. and Hobman T.C. (2020) Endothelium infection and dysregulation by SARS-CoV-2: evidence and caveats in COVID-19. Viruses 13, 29 10.3390/v13010029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Escher R., Breakey N. and Lämmle B. (2020) Severe COVID-19 infection associated with endothelial activation. Thromb. Res. 190, 62 10.1016/j.thromres.2020.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang J., Tecson K.M. and McCullough P.A. (2020) Endothelial dysfunction contributes to COVID-19-associated vascular inflammation and coagulopathy. Rev. Cardiovasc. Med. 21, 315–319 10.31083/j.rcm.2020.03.126 [DOI] [PubMed] [Google Scholar]
- 31.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S.et al. (2020) Endothelial cell infection and endotheliitis in COVID-19. Lancet 395, 1417–1418 10.1016/S0140-6736(20)30937-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sbirkov Y., Dzharov V., Todorova K., Hayrabedyan S. and Sarafian V. (2020) Endothelial inflammation and dysfunction in COVID-19. Vasa 51, 62–70 10.1024/0301-1526/a000991 [DOI] [PubMed] [Google Scholar]
- 33.Chang R., Mamun A., Dominic A. and Le N.T. (2021) SARS-CoV-2 mediated endothelial dysfunction: the potential role of chronic oxidative stress. Front. Physiol. 11, 605908 10.3389/fphys.2020.605908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rovas A., Osiaevi I., Buscher K., Sackarnd J., Tepasse P.R., Fobker M.et al. (2021) Microvascular dysfunction in COVID-19: the MYSTIC study. Angiogenesis 24, 145–157 10.1007/s10456-020-09753-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mezoh G. and Crowther N.J. (2021) Endothelial dysfunction as a primary consequence of SARS-CoV-2 infection. Adv. Exp. Med. Biol. 1321, 33–43 10.1007/978-3-030-59261-5_3 [DOI] [PubMed] [Google Scholar]
- 36.Dupont A., Rauch A., Staessens S., Moussa M., Rosa M., Corseaux D.et al. (2021) Vascular endothelial damage in the pathogenesis of organ injury in severe COVID-19. Arterioscler. Thromb. Vasc. Biol. 41, 1760–1773 10.1161/ATVBAHA.120.315595 [DOI] [PubMed] [Google Scholar]
- 37.Strauss S.A., Seo C., Carrier M. and Jetty P. (2021) From cellular function to global impact: the vascular perspective on COVID-19. Can. J. Surg. 64, E289–E297 10.1503/cjs.023820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jung F., Krüger-Genge A., Franke R.P., Hufert F. and Küpper J.H. (2020) COVID-19 and the endothelium. Clin. Hemorheol. Microcirc. 75, 7–11 10.3233/CH-209007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kar M. (2022) Vascular dysfunction and its cardiovascular consequences during and after COVID-19 infection: a narrative review. Vasc. Health Risk Manag. 18, 105–112 10.2147/VHRM.S355410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goldsmith C.S., Miller S.E., Martines R.B., Bullock H.A. and Zaki S.R. (2020) Electron microscopy of SARS-CoV-2: a challenging task. Lancet 395, e99 10.1016/S0140-6736(20)31188-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roufosse C., Curtis E., Moran L., Hollinshead M., Cook T., Hanley B.et al. (2020) Electron microscopic investigations in COVID-19: not all crowns are coronas. Kidney Int. 98, 505–506 10.1016/j.kint.2020.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McCracken I.R., Saginc G., He L., Huseynov A., Daniels A., Fletcher S.et al. (2021) Lack of evidence of angiotensin-converting enzyme 2 expression and replicative infection by SARS-CoV-2 in human endothelial cells. Circulation 143, 865–868 10.1161/CIRCULATIONAHA.120.052824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bojkova D., McGreig J.E., McLaughlin K.M., Masterson S.G., Widera M., Krähling V.et al. (2021) Differentially conserved amino acid positions may reflect differences in SARS-CoV-2 and SARS-CoV behaviour. Bioinformatics 37, 2282–2288 10.1093/bioinformatics/btab094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robinot R., Hubert M., de Melo G.D., Lazarini F., Bruel T., Smith N.et al. (2021) SARS-CoV-2 infection induces the dedifferentiation of multiciliated cells and impairs mucociliary clearance. Nat. Commun. 12, 4354 10.1038/s41467-021-24521-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hui K.P.Y., Cheung M.C., Perera R.A.P.M., Ng K.C., Bui C.H.T., Ho J.C.W.et al. (2020) Tropism, replication competence, and innate immune responses of the coronavirus SARS-CoV-2 in human respiratory tract and conjunctiva: an analysis in ex-vivo and in-vitro cultures. Lancet Respir. Med. 8, 687–695 10.1016/S2213-2600(20)30193-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang L., Han Y., Nilsson-Payant B.E., Gupta V., Wang P., Duan X.et al. (2020) A human pluripotent stem cell-based platform to study SARS-CoV-2 Tropism and model virus infection in human cells and organoids. Cell Stem Cell 27, 125–136 10.1016/j.stem.2020.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jeffers S.A., Tusell S.M., Gillim-Ross L., Hemmila E.M., Achenbach J.E., Babcock G.J.et al. (2004) CD209L (L-SIGN) is a receptor for severe acute respiratory syndrome coronavirus. Proc. Natl. Acad. Sci. U. S. A. 101, 15748–15753 10.1073/pnas.0403812101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou-Suckow Z., Duerr J., Hagner M., Agrawal R. and Mall M.A. (2017) Airway mucus inflammation and remodeling: emerging links in the pathogenesis of chronic lung diseases. Cell Tissue Res. 367, 537–550 10.1007/s00441-016-2562-z [DOI] [PubMed] [Google Scholar]
- 49.Walls A.C., Park Y.J., Tortorici M.A., Wall A., McGuire A.T. and Veesler D. (2020) Structure function and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell 183, 1735 10.1016/j.cell.2020.11.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sungnak W., Huang N., Bécavin C., Berg M., Queen R., Litvinukova M.et al. (2020) Lung biological network SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat. Med. 26, 681–687 10.1038/s41591-020-0868-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bocci M., Oudenaarden C., Sàenz-Sardà X., Simrén J., Edén A., Sjölund J.et al. (2021), Infection of Brain Pericytes Underlying Neuropathology of COVID-19 Patients., Int. J. Mol. Sci. 22, 11622 10.3390/ijms222111622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jackson C.B., Farzan M., Chen B. and Choe H. (2021) Mechanisms of SARS-CoV-2 entry into cells. Nat. Rev. Mol. Cell Biol. 5, 1–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Koch J., Uckeley Z.M., Doldan P., Stanifer M., Boulant S. and Lozach P.Y. (2021) TMPRSS2 expression dictates the entry route used by SARS-CoV-2 to infect host cells. EMBO J. 40, e107821 10.15252/embj.2021107821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Barbosa L.C., Gonçalves T.L., de Araujo L.P., Rosario L.V.O. and Ferrer V.P. (2021) Endothelial cells and SARS-CoV-2: an intimate relationship. Vascul. Pharmacol. 137, 106829 10.1016/j.vph.2021.106829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Guney C. and Akar F. (2021) Epithelial and endothelial expressions of ACE2: SARS-CoV-2 entry routes. J. Pharm. Pharm. Sci. 24, 84–93 10.18433/jpps31455 [DOI] [PubMed] [Google Scholar]
- 56.Amraei R., Xia C., Olejnik J., White M.R., Napoleon M.A., Lotfollahzadeh S.et al. (2022) Extracellular vimentin is an attachment factor that facilitates SARS-CoV-2 entry into human endothelial cells. Proc. Natl. Acad. Sci. U. S. A. 119, e2113874119 10.1073/pnas.2113874119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bugatti A., Filippini F., Bardelli M., Zani A., Chiodelli P., Messali S.et al. (2022) SARS-CoV-2 infects human ACE2-negative endothelial cells through an α(v)β(3) integrin-mediated endocytosis even in the presence of vaccine-elicited neutralizing antibodies. Viruses 14, 705 10.3390/v14040705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Leeper N.J. and Maegdefessel L. (2018) Non-coding RNAs: key regulators of smooth muscle cell fate in vascular disease. Cardiovasc. Res. 114, 611–621 10.1093/cvr/cvx249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fasolo F., Di Gregoli K., Maegdefessel L. and Johnson J.L. (2019) Non-coding RNAs in cardiovascular cell biology and atherosclerosis. Cardiovasc. Res. 115, 1732–1756 10.1093/cvr/cvz203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maegdefessel L. (2014) The emerging role of microRNAs in cardiovascular disease. J. Intern. Med. 276, 633–644 10.1111/joim.12298 [DOI] [PubMed] [Google Scholar]
- 61.Zhong J.Y., Cui X.J., Zhan J.K., Wang Y.J., Li S., Lin X.et al. (2020) LncRNA-ES3 inhibition by Bhlhe40 is involved in high glucose-induced calcification/ senescence of vascular smooth muscle cells. Ann. N. Y. Acad. Sci. 1474, 61–72 10.1111/nyas.14381 [DOI] [PubMed] [Google Scholar]
- 62.Chen B., Li J., Chi D., Sahnoune I., Calin S., Girnita L.et al. (2019) Non-coding RNAs in IGF-1R signaling regulation: the underlying pathophysiological link between diabetes and cancer. Cells 8, 1638 10.3390/cells8121638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nishitsuji H., Ujino S., Yoshio S., Sugiyama M., Mizokami M., Kanto T.et al. (2016) Long noncoding RNA #32 contributes to antiviral responses by controlling interferon-stimulated gene expression. Proc. Natl. Acad. Sci. U.S.A. 113, 10388–10393 10.1073/pnas.1525022113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Feng J., Yang G., Liu Y., Gao Y., Zhao M., Bu Y.et al. (2019) LncRNA PCNAP1 modulates hepatitis B virus replication and enhances tumor growth of liver cancer. Theranostics 9, 5227–5245 10.7150/thno.34273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.She'n L., Wu C., Zhang J., Xu H., Liu X., Wu X.et al. (2020) Roles and potential applications of lncRNAs in HIV infection. Int. J. Infect. Dis. 92, 97–104 10.1016/j.ijid.2020.01.006 [DOI] [PubMed] [Google Scholar]
- 66.Wang Y., Wang Y., Luo W., Song X., Huang L., Xiao J.et al. (2020) Roles of long non-coding RNAs and emerging RNA-binding proteins in innate antiviral responses. Theranostics 10, 9407–9424 10.7150/thno.48520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ouyang J., Zhu X., Chen Y., Wei H., Chen Q., Chi X.et al. (2014) NRAV a long noncoding RNA modulates antiviral responses through suppression of interferon-stimulated gene transcription. Cell Host Microbe 16, 616–626 10.1016/j.chom.2014.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kordyukova L.V. and Shanko A.V. (2021) COVID-19: myths and reality. Biochemistry (Mosc) 86, 800–817 10.1134/S0006297921070026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Teuwen L.A., Geldhof V., Pasut A. and Carmeliet P. (2020) COVID-19: the vasculature unleashed. Nat. Rev. Immunol. 20, 389–391 10.1038/s41577-020-0343-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Paneni F., Diaz Cañestro C., Libby P., Lüscher T.F. and Camici G.G. (2017) The aging cardiovascular system: understanding it at the cellular and clinical levels. J. Am. Coll. Cardiol. 69, 1952–1967 10.1016/j.jacc.2017.01.064 [DOI] [PubMed] [Google Scholar]
- 71.Merad M. and Martin J.C. (2020) Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat. Rev. Immunol. 20, 355–362 10.1038/s41577-020-0331-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Akbari H., Tabrizi R., Lankarani K.B., Aria H., Vakili S., Asadian F.et al. (2020) The role of cytokine profile and lymphocyte subsets in the severity of coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Life Sci. 258, 118167 10.1016/j.lfs.2020.118167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gonzalez Cañas E., Gimenez Gaibar A., Rodriguez Lorenzo L., Castro Rios J.G., Martinez Toiran A., Bella Cueto M.R.et al. (2020) Acute peripheral arterial thrombosis in COVID-19. Role of endothelial inflammation. Br. J. Surg. 107, e444–e445 10.1002/bjs.11904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Higashikuni Y., Liu W., Obana T. and Sata M. (2021) Pathogenic basis of thromboinflammation and endothelial injury in COVID-19: current findings and therapeutic implications. Int. J. Mol. Sci. 22, 12081 10.3390/ijms222112081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Six I., Guillaume N., Jacob V., Mentaverri R., Kamel S., Boullier A.et al. (2022) The endothelium and COVID-19: an increasingly clear link brief title: endotheliopathy in COVID-19. Int. J. Mol. Sci. 23, 6196 10.3390/ijms23116196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cui J., Li F. and Shi Z.L. (2019) Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 17, 181–192 10.1038/s41579-018-0118-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chen Y., Liu Q. and Guo D. (2020) Emerging coronaviruses: genome structure, replication, and pathogenesis. J. Med. Virol. 92, 418–423 10.1002/jmv.25681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.V'kovski P., Kratzel A., Steiner S., Stalder H. and Thiel V. (2021) Coronavirus biology and replication: implications for SARS-CoV-2. Nat. Rev. Microbiol. 19, 155–170 10.1038/s41579-020-00468-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lim Y.X., Ng Y.L., Tam J.P. and Liu D.X. (2016) Human coronaviruses: a review of virus-host interactions. Diseases 4, pii: E26 10.3390/diseases4030026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Corman V.M., Muth D., Niemeyer D. and Drosten C. (2018) Hosts and sources of endemic human coronaviruses. Adv. Virus Res. 100, 163–188 10.1016/bs.aivir.2018.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.van Boheemen S., de Graaf M., Lauber C., Bestebroer T.M., Raj V.S., Zaki A.M.et al. (2012) Genomic characterization of a newly discovered coronavirus associated with acute respiratory distress syndrome in humans. mBio 3, pii: e00473–12 10.1128/mBio.00473-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Greber U.F. (2021) Two years into COVID-19 - Lessons in SARS-CoV-2 and a perspective from papers in FEBS Letters. FEBS Lett. 595, 2847–2853 10.1002/1873-3468.14226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H.et al. (2020) Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 395, 565–574 10.1016/S0140-6736(20)30251-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhou G., Chen S. and Chen Z. (2020) Advances in COVID-19: the virus, the pathogenesis, and evidence-based control and therapeutic strategies. Front Med 14, 117–125 10.1007/s11684-020-0773-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wolff G., Limpens R.W.A.L., Zevenhoven-Dobbe J.C., Laugks U., Zheng S., de Jong A.W.M.et al. (2020) A molecular pore spans the double membrane of the coronavirus replication organelle. Science 369, 1395–1398 10.1126/science.abd3629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.de Wilde A.H., Snijder E.J., Kikkert M. and van Hemert M.J. (2018) Host factors in coronavirus replication. Curr. Top. Microbiol. Immunol. 419, 1–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gheblawi M., Wang K., Viveiros A., Nguyen Q., Zhong J.C., Turner A.J.et al. (2020) Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: celebrating the 20th anniversary of the discovery of ACE2. Circ. Res. 126, 1456–1474 10.1161/CIRCRESAHA.120.317015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kuba K., Imai Y., Ohto-Nakanishi T. and Penninger J.M. (2010) Trilogy of ACE2: a peptidase in the renin-angiotensin system a SARS receptor, and a partner for amino acid transporters. Pharmacol. Ther. 128, 119–128 10.1016/j.pharmthera.2010.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Heurich A., Hofmann-Winkler H., Gierer S., Liepold T., Jahn O. and Pöhlmann S. (2014) TMPRSS2 and ADAM17 cleave ACE2 differentially and only proteolysis by TMPRSS2 augments entry driven by the severe acute respiratory syndrome coronavirus spike protein. J. Virol. 88, 1293–1307 10.1128/JVI.02202-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Oxford A.E., Halla F., Robertson E.B. and Morrison B.E. (2020) Endothelial cell contributions to COVID-19. Pathogens 9, 785 10.3390/pathogens9100785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dimitrov D.S. (2003) The secret life of ACE2 as a receptor for the SARS virus. Cell 115, 652–653 10.1016/S0092-8674(03)00976-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Batlle D., Wysocki J. and Satchell K. (2020) Soluble angiotensin-converting enzyme 2: a potential approach for coronavirus infection therapy? Clin. Sci. (Lond.) 134, 543–545 10.1042/CS20200163 [DOI] [PubMed] [Google Scholar]
- 93.Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A.et al. (2003) Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 426, 450–454 10.1038/nature02145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lukassen S., Chua R.L., Trefzer T., Kahn N.C., Schneider M.A., Muley T.et al. (2020) SARS-CoV-2 receptor ACE2 and TMPRSS2 are primarily expressed in bronchial transient secretory cells. EMBO J. 18, e105114 10.15252/embj.2020105114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers D., Kant K.M.et al. (2020) Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb. Res. 191, 148–150 10.1016/j.thromres.2020.04.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hendren N.S., Drazner M.H., Bozkurt B. and Cooper L.T. Jr (2020) Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation 141, 1903–1914 10.1161/CIRCULATIONAHA.120.047349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mao L., Jin H., Wang M., Hu Y., Chen S., He Q.et al. (2020) Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 77, 683–690 10.1001/jamaneurol.2020.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cantuti-Castelvetri L., Ojha R., Pedro L.D., Djannatian M., Franz J., Kuivanen S.et al. (2020) Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science 370, 856–860 10.1126/science.abd2985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Daly J.L., Simonetti B., Klein K., Chen K.E., Williamson M.K., Antón-Plágaro C.et al. (2004) Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science 370, 861–865 10.1126/science.abd3072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Giordo R., Paliogiannis P., Mangoni A.A. and Pintus G. (2021) SARS-CoV-2 and endothelial cell interaction in COVID-19: molecular perspectives. Vasc. Biol. 3, R15–R23 10.1530/VB-20-0017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Amraei R., Yin W., Napoleon M.A., Suder E.L., Berrigan J., Zhao Q.et al. (2021) CD209L/L-SIGN and CD209/DC-SIGN Act as Receptors for SARS-CoV-2. ACS Cent Sci. 7, 1156–1165 10.1021/acscentsci.0c01537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tortorici M.A., Walls A.C., Lang Y., Wang C., Li Z., Koerhuis D.et al. (2019) Structural basis for human coronavirus attachment to sialic acid receptors. Nat. Struct. Mol. Biol. 26, 481–489 10.1038/s41594-019-0233-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Baker A.N., Richards S.J., Guy C.S., Congdon T.R., Hasan M., Zwetsloot A.J.et al. (2020) The SARS-COV-2 spike protein binds sialic acids and enables rapid detection in a lateral flow point of care diagnostic device. ACS Cent Sci. 6, 2046–2052 10.1021/acscentsci.0c00855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Anand P., Puranik A., Aravamudan M., Venkatakrishnan A.J. and Soundararajan V. (2020) SARS-CoV-2 strategically mimics proteolytic activation of human ENaC. Elife 9, e58603 10.7554/eLife.58603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhang C., Zhao Y.X., Zhang Y.H., Zhu L., Deng B.P., Zhou Z.L.et al. (2010) Angiotensin-converting enzyme 2 attenuates atherosclerotic lesions by targeting vascular cells. Proc. Natl. Acad. Sci. U. S. A. 107, 15886–15891 10.1073/pnas.1001253107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sahara M., Ikutomi M., Morita T., Minami Y., Nakajima T., Hirata Y.et al. (2014) Deletion of angiotensin-converting enzyme 2 promotes the development of atherosclerosis and arterial neointima formation. Cardiovasc. Res. 101, 236–246 10.1093/cvr/cvt245 [DOI] [PubMed] [Google Scholar]
- 107.Xu S., Ilyas I., Little P.J., Li H., Kamato D., Zheng X.et al. (2021) Endothelial dysfunction in atherosclerotic cardiovascular diseases and beyond: from mechanism to pharmacotherapies. Pharmacol. Rev. 73, 924–967 10.1124/pharmrev.120.000096 [DOI] [PubMed] [Google Scholar]
- 108.Kuriakose J., Montezano A.C. and Touyz R.M. (2021) ACE2/Ang-(1-7)/Mas1 axis and the vascular system: vasoprotection to COVID-19-associated vascular disease. Clin. Sci. (Lond.) 135, 387–407 10.1042/CS20200480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Poznyak A.V., Bharadwaj D., Prasad G., Grechko A.V., Sazonova M.A. and Orekhov A.N. (2021) Renin-Angiotensin System in Pathogenesis of Atherosclerosis and Treatment of CVD. Int. J. Mol. Sci. 22, 6702 10.3390/ijms22136702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Saravik B., Li Z., Lang C.N., Schmid B., Lang F.K., Grad S.et al. (2021) The tissue renin-angiotensin system and its role in the pathogenesis of major human diseases: Quo Vadis. Cells 10, 650 10.3390/cells10030650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Santos R.A.S., Oudit G.Y., Verano-Braga T., Canta G., Steckelings U.M. and Bader M. (2019) The renin-angiotensin system: going beyond the classical paradigms. Am. J. Physiol. Heart Circ. Physiol. 316, H958–H970 10.1152/ajpheart.00723.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Saponaro F., Rutigliano G., Sestito S., Bandini L., Storti B., Bizzarri R.et al. (2020) ACE2 in the Era of SARS-CoV-2: controversies and novel perspectives. Front. Mol. Biosci. 7, 588618 10.3389/fmolb.2020.588618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhang Q., Lu S., Li T., Yu L., Zhang Y., Zeng H.et al. (2019) ACE2 inhibits breast cancer angiogenesis via suppressing the VEGFa/VEGFR2/ERK pathway. J. Exp. Clin. Cancer Res. 38, 173 10.1186/s13046-019-1156-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pine A.B., Meizlish M.L., Goshua G., Chang C.H., Zhang H., Bishai J.et al. (2020) Circulating markers of angiogenesis and endotheliopathy in COVID-19. Pulm Circ 10, 2045894020966547 10.1177/2045894020966547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Norooznezhad A.H. and Mansouri K. (2021) Endothelial cell dysfunction coagulation and angiogenesis in coronavirus disease 2019 (COVID-19). Microvasc. Res. 137, 104188 10.1016/j.mvr.2021.104188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Smadja D.M., Mentzer S.J., Fontenay M., Laffan M.A., Ackermann M., Helms J.et al. (2021) COVID-19 is a systemic vascular hemopathy: insight for mechanistic and clinical aspects. Angiogenesis 24, 755–788 10.1007/s10456-021-09805-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Pelisek J., Eckstein H.H. and Zernecke A. (2012) Pathophysiological mechanisms of carotid plaque vulnerability: impact on ischemic stroke. Arch. Immunol. Ther. Exp. (Warsz.) 60, 431–442 10.1007/s00005-012-0192-z [DOI] [PubMed] [Google Scholar]
- 118.Pelisek J., Wendorff H., Wendorff C., Kuehnl A. and Eckstein H.H. (2016) Age-associated changes in human carotid atherosclerotic plaques. Ann. Med. 48, 541–551 10.1080/07853890.2016.1204468 [DOI] [PubMed] [Google Scholar]
- 119.Sorokin V., Vickneson K., Kofidis T., Woo C.C., Lin X.Y., Foo R.et al. (2020) Role of vascular smooth muscle cell plasticity and interactions in vessel wall inflammation. Front. Immunol. 11, 599415 10.3389/fimmu.2020.599415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Dora K.A. (2001) Cell-cell communication in the vessel wall. Vasc. Med. 6, 43–50 10.1177/1358836X0100600108 [DOI] [PubMed] [Google Scholar]
- 121.Rauti R., Shahoha M., Leichtmann-Bardoogo Y., Nasser R., Paz E., Tamir R.et al. (2021) Effect of SARS-CoV-2 proteins on vascular permeability. Elife 10, e69314 10.7554/eLife.69314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hamming I., Timens W., Bulthuis M.L., Lely A.T., Navis G. and van Goor H. (2004) Tissue distribution of ACE2 protein the functional receptor for SARS coronavirus A first step in understanding SARS pathogenesis. J. Pathol. 203, 631–637 10.1002/path.1570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Qaradakhi T., Gadanec L.K., McSweeney K.R., Tacey A., Apostolopoulos V., Levinger I.et al. (2020) The potential actions of angiotensin-converting enzyme II (ACE2) activator diminazene aceturate (DIZE) in various diseases. Clin. Exp. Pharmacol. Physiol. 47, 751–758 10.1111/1440-1681.13251 [DOI] [PubMed] [Google Scholar]
- 124.Rabelo L.A., Alenina N. and Bader M. (2011) ACE2-angiotensin-(1-7)-Mas axis and oxidative stress in cardiovascular disease. Hypertens. Res. 34, 154–160 10.1038/hr.2010.235 [DOI] [PubMed] [Google Scholar]
- 125.Patel V.B., Zhong J.C., Grant M.B. and Oudit G.Y. (2016) Role of the ACE2/angiotensin 1-7 axis of the renin-angiotensin system in heart failure. Circ. Res. 118, 1313–1326 10.1161/CIRCRESAHA.116.307708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chen L., Li X., Chen M., Feng Y. and Xiong C. (2020) The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc. Res. 116, 1097–1100 10.1093/cvr/cvaa078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Carnevale S., Beretta P. and Morbini P. (2021) Direct endothelial damage and vasculitis due to SARS-CoV-2 in small bowel submucosa of COVID-19 patient with diarrhea. J. Med. Virol. 93, 61–63 10.1002/jmv.26119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hattori Y., Hattori K., Machida T. and Matsuda N. (2022) Vascular endotheliitis associated with infections: its pathogenetic role and therapeutic implication. Biochem. Pharmacol. 197, 114909 10.1016/j.bcp.2022.114909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Geevarghese A. and Herman I.M. (2014) Pericyte-endothelial crosstalk: implications and opportunities for advanced cellular therapies. Transl. Res. 163, 296–306 10.1016/j.trsl.2014.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Yau J.W., Teoh H. and Verma S. (2015) Endothelial cell control of thrombosis. BMC Cardiovasc. Disord. 15, 130 10.1186/s12872-015-0124-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Elyaspour Z., Zibaeenezhad M.J., Razmkhah M. and Razeghian-Jahromi I. (2021) Is it all about endothelial dysfunction and thrombosis formation? The secret of COVID-19 Clin. Appl. Thromb. Hemost. 27, 10760296211042940 10.1177/10760296211042940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Thierry A.R. and Roch B. (2020) Neutrophil extracellular traps and by-products play a key role in COVID-19: pathogenesis risk factors and therapy. J. Clin. Med. 9, 2942 10.3390/jcm9092942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gould T.J., Vu T.T., Swystun L.L., Dwivedi D.J., Mai S.H., Weitz J.I.et al. (2014) Neutrophil extracellular traps promote thrombin generation through platelet-dependent and platelet-independent mechanisms. Arterioscler. Thromb. Vasc. Biol. 34, 1977–1984 10.1161/ATVBAHA.114.304114 [DOI] [PubMed] [Google Scholar]
- 134.Zuo Y., Zuo M., Yalavarthi S., Gockman K., Madison J.A., Shi H.et al. (2021) Neutrophil extracellular traps and thrombosis in COVID-19. J. Thromb. Thrombolysis 51, 446–453 10.1007/s11239-020-02324-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Alam M.S. and Czajkowsky D.M. (2022) SARS-CoV-2 infection and oxidative stress: pathophysiological insight into thrombosis and therapeutic opportunities. Cytokine growth. Factor Rev 63, 44–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Guzik T.J., Mohiddin S.A., Dimarco A., Patel V., Savvatis K., Marelli-Berg F.M.et al. (2020) COVID-19 and the cardiovascular system: implications for risk assessment diagnosis and treatment options. Cardiovasc. Res. 116, 1666–1687 10.1093/cvr/cvaa106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Li X., Fang P., Mai J., Choi E.T., Wang H. and Yang X.F. (2013) Targeting mitochondrial reactive oxygen species as novel therapy for inflammatory diseases and cancers. J. Hematol. Oncol. 6, 19 10.1186/1756-8722-6-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Vasileiou P.V.S., Evangelou K., Vlasis K., Fildisis G., Panayiotidis M.I., Chronopoulos E.et al. (2019) Mitochondrial homeostasis and cellular senescence. Cells 8, 686 10.3390/cells8070686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Yin Y., Zhou Z., Liu W., Chang Q., Sun G. and Dai Y. (2017) Vascular endothelial cells senescence is associated with NOD-like receptor family pyrin domain-containing 3 (NLRP3) inflammasome activation via reactive oxygen species (ROS)/thioredoxin-interacting protein (TXNIP) pathway. Int. J. Biochem. Cell Biol. 84, 22–34 10.1016/j.biocel.2017.01.001 [DOI] [PubMed] [Google Scholar]
- 140.Hoffmann J., Haendeler J., Aicher A., Rössig L., Vasa M., Zeiher A.M.et al. (2001) Aging enhances the sensitivity of endothelial cells toward apoptotic stimuli: important role of nitric oxide. Circ. Res. 89, 709–715 10.1161/hh2001.097796 [DOI] [PubMed] [Google Scholar]
- 141.Mahler G.J., Farrar E.J. and Butcher J.T. (2013) Inflammatory cytokines promote mesenchymal transformation in embryonic and adult valve endothelial cells. Arterioscler. Thromb. Vasc. Biol. 33, 121–130 10.1161/ATVBAHA.112.300504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Cho J.G., Lee A., Chang W., Lee M.S. and Kim J. (2018) Endothelial to mesenchymal transition represents a key link in the interaction between inflammation and endothelial dysfunction. Front. Immunol. 9, 294 10.3389/fimmu.2018.00294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bradley B.T., Maioli H., Johnston R., Chaudhry I., Fink S.L., Xu H.et al. (2020) Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: a case series. Lancet 396, 320–332 10.1016/S0140-6736(20)31305-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Dittmayer C., Meinhardt J., Radbruch H., Radke J., Heppner B.I., Heppner F.L.et al. (2020) Why misinterpretation of electron micrographs in SARS-CoV-2-infected tissue goes viral. Lancet 396, e64–e65 10.1016/S0140-6736(20)32079-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Hou Y.J., Okuda K., Edwards C.E., Martinez D.R., Asakura T., Dinnon K.H. IIIet al. (2020) SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell 182, 429.e14–446.e14 10.1016/j.cell.2020.05.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Nascimento Conde J., Schutt W.R., Gorbunova E.E. and Mackow E.R. (2020) Recombinant ACE2 expression is required for SARS-CoV-2 to infect primary human endothelial cells and induce inflammatory and procoagulative responses. mBio 11, e03185–e03220 10.1128/mBio.03185-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lu D., Chatterjee S., Xiao K., Riedel I., Wang Y., Foo R.et al. (2020) MicroRNAs targeting the SARS-CoV-2 entry receptor ACE2 in cardiomyocytes. J. Mol. Cell Cardiol. 148, 46–49 10.1016/j.yjmcc.2020.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Suzuki Y.J., Nikolaienko S.I., Dibrova V.A., Dibrova Y.V., Vasylyk V.M., Novikov M.Y.et al. (2021) SARS-CoV-2 spike protein-mediated cell signaling in lung vascular cells. Vascul. Pharmacol. 137, 106823 10.1016/j.vph.2020.106823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Xu S., Liu Y., Ding Y., Luo S., Zheng X., Wu X.et al. (2021) The zinc finger transcription factor KLF2 protects against COVID-19 associated endothelial dysfunction. Signal Transduct. Target Ther. 6, 266 10.1038/s41392-021-00690-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wagner J.U.G., Bojkova D., Shumliakivska M., Luxán G., Nicin L., Aslan G.S.et al. (2021) Increased susceptibility of human endothelial cells to infections by SARS-CoV-2 variants. Basic Res. Cardiol. 116, 42 10.1007/s00395-021-00882-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Albini A., Calabrone L., Carlini V., Benedetto N., Lombardo M., Bruno A.et al. (2021) Preliminary evidence for IL-10-Induced ACE2 mRNA expression in lung-derived and endothelial cells: implications for SARS-Cov-2 ARDS pathogenesis. Front. Immunol. 12, 718136 10.3389/fimmu.2021.718136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Aleksova A., Gagno G., Sinagra G., Beltrami A.P., Janjusevic M., Ippolito G.et al. (2021) Effects of SARS-CoV-2 on cardiovascular system: the dual role of angiotensin-converting enzyme 2 (ACE2) as the virus receptor and homeostasis regulator-review. Int. J. Mol. Sci. 22, 4526 10.3390/ijms22094526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Nader D., Fletcher N., Curley G.F. and Kerrigan S.W. (2021) SARS-CoV-2 uses major endothelial integrin αvβ3 to cause vascular dysregulation in-vitro during COVID-19. PLoS ONE 16, e0253347 10.1371/journal.pone.0253347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Targosz-Korecka M., Kubisiak A., Kloska D., Kopacz A., Grochot-Przeczek A. and Szymonski M. (2021) Endothelial glycocalyx shields the interaction of SARS-CoV-2 spike protein with ACE2 receptors. Sci. Rep. 11, 12157 10.1038/s41598-021-91231-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Potje S.R., Costa T.J., Fraga-Silva T.F.C., Martins R.B., Benatti M.N., Almado C.E.L.et al. (2021) Heparin prevents in vitro glycocalyx shedding induced by plasma from COVID-19 patients. Life Sci. 276, 119376 10.1016/j.lfs.2021.119376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ratajczak M.Z., Bujko K., Ciechanowicz A., Sielatycka K., Cymer M., Marlicz W.et al. (2021) SARS-CoV-2 entry receptor ACE2 is expressed on very small CD45(-) precursors of hematopoietic and endothelial cells and in response to virus spike protein activates the Nlrp3 inflammasome. Stem Cell Rev. Rep. 17, 266–277 10.1007/s12015-020-10010-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Imperio G.E., Lye P., Mughis H., Hamada H., Bloise E., Lye S.J.et al. (2021) Hypoxia alters the expression of ACE2 and TMPRSS2 SARS-CoV-2 cell entry mediators in hCMEC/D3 brain endothelial cells. Microvasc. Res. 138, 104232 10.1016/j.mvr.2021.104232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Fodor A., Tiperciuc B., Login C., Orasan O.H., Lazar A.L., Buchman C.et al. (2021) Endothelial dysfunction, inflammation, and oxidative stress in COVID-19-mechanisms and therapeutic targets. Oxid. Med. Cell Longev. 2021, 8671713 10.1155/2021/8671713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Cai H. and Harrison D.G. (2000) Endothelial dysfunction in cardiovascular diseases: the role of oxidant stress. Circ. Res. 87, 840–844 10.1161/01.RES.87.10.840 [DOI] [PubMed] [Google Scholar]
- 160.Vlahopoulos S., Wang K., Xue Y., Zheng X., Boldogh I. and Pan L. (2021) Endothelial dysfunction through oxidatively generated epigenetic mark in respiratory viral infections. Cells 10, 3067 10.3390/cells10113067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Jurgeit A., Moese S., Roulin P., Dorsch A., Lötzerich M., Lee W.M.et al. (2010) An RNA replication-center assay for high content image-based quantifications of human rhinovirus and coxsackievirus infections. Virol. J. 7, 264 10.1186/1743-422X-7-264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Murer L., Volle R., Andriasyan V., Petkidis A., Gomez-Gonzalez A., Yang L.et al. (2022) Identification of broad anti-coronavirus chemical agents for repurposing against SARS-CoV-2 and variants of concern. Curr. Res. Virol. Sci. 3, 100019 10.1016/j.crviro.2022.100019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Volle R., Murer L., Petkidis A., Andriasyan V., Savi A., Bircher C.et al. (2022) Methylene blue, mycophenolic acid, posaconazole, and niclosamide inhibit SARS-CoV-2 Omicron variant BA.1 infection of human airway epithelial organoids. Curr. Res. Microb. Sci. 3, 100158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Dong B., Zhang C., Feng J.B., Zhao Y.X., Li S.Y., Yang Y.P.et al. (2008) Overexpression of ACE2 enhances plaque stability in a rabbit model of atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 28, 1270–1276 10.1161/ATVBAHA.108.164715 [DOI] [PubMed] [Google Scholar]
- 165.Li M.Y., Li L., Zhang Y. and Wang X.S. (2020) Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis. Poverty 9, 45 10.1186/s40249-020-00662-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Ma S., Sun S., Li J., Fan Y., Qu J., Sun L.et al. (2021) Single-cell transcriptomic atlas of primate cardiopulmonary aging. Cell Res. 31, 415–432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Frismantiene A., Philippova M., Erne P. and Resink T.J. (2018) Smooth muscle cell-driven vascular diseases and molecular mechanisms of VSMC plasticity. Cell. Signal. 52, 48–64 10.1016/j.cellsig.2018.08.019 [DOI] [PubMed] [Google Scholar]
- 168.Grootaert M.O.J., Moulis M., Roth L., Martinet W., Vindis C., Bennett M.R.et al. (2018) Vascular smooth muscle cell death, autophagy and senescence in atherosclerosis. Cardiovasc. Res. 114, 622–634 10.1093/cvr/cvy007 [DOI] [PubMed] [Google Scholar]
- 169.Méndez-Barbero N., Gutiérrez-Muñoz C. and Colio L.M.B. (2021) Cellular crosstalk between endothelial and smooth muscle cells in vascular wall remodeling. Int. J. Mol. Sci. 22, 7284 10.3390/ijms22147284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Zhang Z., Chen L., Zhong J., Gao P. and Oudit G.Y. (2014) ACE2/Ang-(1-7) signaling and vascular remodeling. Sci. China Life Sci. 57, 802–808 10.1007/s11427-014-4693-3 [DOI] [PubMed] [Google Scholar]
- 171.Savoia C., Arrabito E., Parente R., Nicoletti C., Madaro L., Battistoni A.et al. (2020) Mas receptor activation contributes to the improvement of nitric oxide bioavailability and vascular remodeling during chronic AT1R (angiotensin type-1 receptor) blockade in experimental hypertension. Hypertension 76, 1753–1761 10.1161/HYPERTENSIONAHA.120.15527 [DOI] [PubMed] [Google Scholar]
- 172.Thomas M.C., Pickering R.J., Tsorotes D., Koitka A., Sheehy K., Bernardi S.et al. (2010) Genetic Ace2 deficiency accentuates vascular inflammation and atherosclerosis in the ApoE knockout mouse. Circ. Res. 107, 888–897 10.1161/CIRCRESAHA.110.219279 [DOI] [PubMed] [Google Scholar]
- 173.Hrenak J. and Simko F. (2020) Renin-angiotensin system: an important player in the pathogenesis of acute respiratory distress syndrome. Int. J. Mol. Sci. 21, 8038 10.3390/ijms21218038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Xu J., Mukerjee S., Silva-Alves C., Carvalho-Galvão A., Cruz J., Balarini C.et al. (2016) A disintegrin and metalloprotease 17 in the cardiovascular and central nervous systems. Front. Physiol. 7, 469 10.3389/fphys.2016.00469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Takaguri A., Kimura K., Hinoki A., Bourne A.M., Autieri M.V. and Eguchi S. (2011) A disintegrin and metalloprotease 17 mediates neointimal hyperplasia in vasculature. Hypertension 57, 841–845 10.1161/HYPERTENSIONAHA.110.166892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Xu J., Sriramula S., Xia H., Moreno-Walton L., Culicchia F., Domenig O.et al. (2017) Clinical relevance and role of neuronal AT1 receptors in ADAM17-mediated ACE2 shedding in neurogenic hypertension. Circ. Res. 121, 43–55 10.1161/CIRCRESAHA.116.310509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Schreiber B., Patel A. and Verma A. (2020) Shedding light on COVID-19: ADAM17 the missing link? Am. J. Ther. 28, e358–e360 10.1097/MJT.0000000000001226 [DOI] [PubMed] [Google Scholar]
- 178.Ohtsu H., Dempsey P.J., Frank G.D., Brailoiu E., Higuchi S., Suzuki H.et al. (2006) ADAM17 mediates epidermal growth factor receptor transactivation and vascular smooth muscle cell hypertrophy induced by angiotensin II. Arterioscler. Thromb. Vasc. Biol. 26, e133–e137 10.1161/atvb.26.9.1976 [DOI] [PubMed] [Google Scholar]
- 179.Takayanagi T., Crawford K.J., Kobayashi T., Obama T., Tsuji T., Elliott K.J.et al. (2014) Caveolin 1 is critical for abdominal aortic aneurysm formation induced by angiotensin II and inhibition of lysyl oxidase. Clin. Sci. (Lond.) 126, 785–794 10.1042/CS20130660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Satoh H., Nakamura M., Satoh M., Nakajima T., Izumoto H., Maesawa C.et al. (2004) Expression and localization of tumour necrosis factor-alpha and its converting enzyme in human abdominal aortic aneurysm. Clin. Sci. (Lond.) 106, 301–306 10.1042/CS20030189 [DOI] [PubMed] [Google Scholar]
- 181.Dal Moro F., Vendramin I. and Livi U. (2020) The war against the SARS-CoV2 infection: is it better to fight or mitigate it? Med. Hypotheses 143, 110129 10.1016/j.mehy.2020.110129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Sluimer J.C., Gasc J.M., Hamming I., van Goor H., Michaud A., van den Akker L.H.et al. (2008) Angiotensin-converting enzyme 2 (ACE2) expression and activity in human carotid atherosclerotic lesions. J. Pathol. 215, 273–279 10.1002/path.2357 [DOI] [PubMed] [Google Scholar]
- 183.Kalidhindi R.S.R., Borkar N.A., Ambhore N.S., Pabelick C.M., Prakash Y.S. and Sathish V. (2020) Sex steroids skew ACE2 expression in human airway: a contributing factor to sex differences in COVID-19? Am. J. Physiol. Lung Cell. Mol. Physiol. 319, L843–L847 10.1152/ajplung.00391.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Marchiano S., Hsiang T.Y., Khanna A., Higashi T., Whitmore L.S., Bargehr J.et al. (2021) SARS-CoV-2 Infects human pluripotent stem cell-derived cardiomyocytes, impairing electrical and mechanical function. Stem Cell Rep. 16, 478–492 10.1016/j.stemcr.2021.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Khaddaj-Mallat R., Aldib N., Bernard M., Paquette A.S., Ferreira A., Lecordier S.et al. (2021) SARS-CoV-2 deregulates the vascular and immune functions of brain pericytes via Spike protein. Neurobiol. Dis. 161, 105561 10.1016/j.nbd.2021.105561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Zhang Y.H., Li Z., Zeng T., Chen L., Li H., Huang T.et al. (2021) Detecting the multiomics signatures of factor-specific inflammatory effects on airway smooth muscles. Front. Genet. 11, 599970 10.3389/fgene.2020.599970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Tzankov A., Bhattacharyya S., Kotlo K. and Tobacman J.K. (2022) Increase in chondroitin sulfate and decline in arylsulfatase B may contribute to pathophysiology of COVID-19 respiratory failure. Pathobiology 89, 81–91 10.1159/000519542 [DOI] [PubMed] [Google Scholar]
- 188.Muhl M., He L., Sun Y., Andaloussi Mäe M., Pietilä R., Liu J.et al. (2022), The SARS-CoV-2 receptor ACE2 is expressed in mouse pericytes but not endothelial cells: Implications for COVID-19 vascular research. Stem., Stem Cell Reports 17, 1089–1104 10.1016/j.stemcr.2022.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Butsabong T., Felippe M., Campagnolo P. and Maringer K. (2021) The emerging role of perivascular cells (pericytes) in viral pathogenesis. J. Gen. Virol. 102, 001634 10.1099/jgv.0.001634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Suomalainen M. and Greber U.F. (2021) Virus infection variability by single-cell profiling. Viruses 13, 1568 10.3390/v13081568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Boon R.A., Jaé N., Holdt L. and Dimmeler S. (2016) Long noncoding RNAs: from clinical genetics to therapeutic targets? J. Am. Coll. Cardiol. 67, 1214–1226 10.1016/j.jacc.2015.12.051 [DOI] [PubMed] [Google Scholar]
- 192.Batista P.J. and Chang H.Y. (2013) Long noncoding RNAs: cellular address codes in development and disease. Cell 152, 1298–1307 10.1016/j.cell.2013.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Statello L., Guo C.J., Chen L.L. and Huarte M. (2021) Gene regulation by long non-coding RNAs and its biological functions. Nat. Rev. Mol. Cell Biol. 22, 96–118 10.1038/s41580-020-00315-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Gangwar R.S., Rajagopalan S., Natarajan R. and Deiuliis J.A. (2018) Noncoding RNAs in cardiovascular disease: pathological relevance and emerging role as biomarkers and therapeutics. Am. J. Hypertens. 31, 150–165 10.1093/ajh/hpx197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Zhang C., Han B., Xu T. and Li D. (2020) The biological function and potential mechanism of long non-coding RNAs in cardiovascular disease. J. Cell. Mol. Med. 24, 12900–12909 10.1111/jcmm.15968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Pierce J.B. and Feinberg M.W. (2020) Long noncoding RNAs in Atherosclerosis and vascular injury: pathobiology biomarkers and targets for therapy. Arterioscler. Thromb. Vasc. Biol. 40, 2002–2017 10.1161/ATVBAHA.120.314222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Li M., Qian M., Kyler K. and Xu J. (2018) Endothelial-vascular smooth muscle cells interactions in atherosclerosis. Front. Cardiovasc. Med. 5, 151 10.3389/fcvm.2018.00151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Li D.Y., Busch A., Jin H., Chernogubova E., Pelisek J., Karlsson J.et al. (2018) H19 induces abdominal aortic aneurysm development and progression. Circulation 138, 1551–1568 10.1161/CIRCULATIONAHA.117.032184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Wang P., Xu J., Wang Y. and Cao X. (2017) An interferon-independent lncRNA promotes viral replication by modulating cellular metabolism. Science 358, 1051–1055 10.1126/science.aao0409 [DOI] [PubMed] [Google Scholar]
- 200.Wang Y., Huang L., Wang Y., Luo W., Li F., Xiao J.et al. (2020) Single-cell RNA-sequencing analysis identifies host long noncoding RNA MAMDC2-AS1 as a co-factor for HSV-1 nuclear transport. Int. J. Biol. Sci. 16, 1586–1603 10.7150/ijbs.42556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Barriocanal M., Carnero E., Segura V. and Fortes P. (2014) Long non-coding RNA BST2/BISPR is induced by IFN and regulates the expression of the antiviral factor tetherin. Front. Immunol. 5, 655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Agrawal N., Dasaradhi P.V., Mohmmed A., Malhotra P., Bhatnagar R.K. and Mukherjee S.K. (2003) RNA interference: biology mechanism and applications. Microbiol. Mol. Biol. Rev. 67, 657–685 10.1128/MMBR.67.4.657-685.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Trobaugh D.W. and Klimstra W.B. (2017) MicroRNA regulation of RNA virus replication and pathogenesis. Trends Mol. Med. 23, 80–93 10.1016/j.molmed.2016.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Ghosh Z., Mallick B. and Chakrabarti J. (2009) Cellular versus viral microRNAs in host-virus interaction. Nucleic Acids Res. 37, 1035–1048 10.1093/nar/gkn1004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Jopling C.L., Yi M., Lancaster A.M., Lemon S.M. and Sarnow P. (2005) Modulation of hepatitis C virus RNA abundance by a liver-specific MicroRNA. Science 309, 1577–1581 10.1126/science.1113329 [DOI] [PubMed] [Google Scholar]
- 206.Zhang Q., Chen C.Y., Yedavalli V.S. and Jeang K.T. (2013) NEAT1 long noncoding RNA LncRNA and virus and paraspeckle bodies modulate HIV-1 posttranscriptional expression. MBio 4, e00596–e00612 10.1128/mBio.00596-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Sonkoly E., Bata-Csorgo Z., Pivarcsi A., Polyanka H., Kenderessy-Szabo A., Molnar G.et al. (2005) Identification and characterization of a novel psoriasis susceptibility-related noncoding RNA gene PRINS. J. Biol. Chem. 280, 24159–24167 10.1074/jbc.M501704200 [DOI] [PubMed] [Google Scholar]
- 208.Braconi C., Kogure T., Valeri N., Huang N., Nuovo G., Costinean S.et al. (2011) microRNA-29 can regulate expression of the long non-coding RNA gene MEG3 in hepatocellular cancer. Oncogene 30, 4750–4756 10.1038/onc.2011.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Peng X., Gralinski L., Armour C.D., Ferris M.T., Thomas M.J., Proll S.et al. (2010) Unique signatures of long noncoding RNA expression in response to virus infection and altered innate immune signaling. MBio 1, e00206–e00210 10.1128/mBio.00206-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Qu D., Sun W.W., Li L., Ma L., Sun L., Jin X.et al. (2019) Long noncoding RNA MALAT1 releases epigenetic silencing of HIV-1 replication by displacing the polycomb repressive complex 2 from binding to the LTR promoter. Nucleic Acids Res. 47, 3013–3027 10.1093/nar/gkz117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Chao T.C., Zhang Q., Li Z., Tiwari S.K., Qin Y., Yau E.et al. (2019) The long noncoding RNA HEAL regulates HIV-1 replication through epigenetic regulation of the HIV-1 promoter. mBio 10, pii e02016–e02019 10.1128/mBio.02016-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Ma H., Han P., Ye W., Chen H., Zheng X., Cheng L.et al. (2017) The long noncoding RNA NEAT1 exerts antihantaviral effects by acting as positive feedback for RIG-I signaling. J. Virol. 91, e02250–16 10.1128/JVI.02250-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Imamura K., Imamachi N., Akizuki G., Kumakura M., Kawaguchi A., Nagata K.et al. (2014) Long noncoding RNA NEAT1-dependent SFPQ relocation from promoter region to paraspeckle mediates IL8 expression upon immune stimuli. Mol. Cell 53, 393–406 10.1016/j.molcel.2014.01.009 [DOI] [PubMed] [Google Scholar]
- 214.Arisan E.D., Dart A., Grant G.H., Arisan S., Cuhadaroglu S., Lange S.et al. (2020) The prediction of miRNAs in SARS-CoV-2 genomes: Hsa-miR databases identify 7 key miRs linked to host responses and virus pathogenicity-related KEGG pathways significant for comorbidities. Viruses 12, 614 10.3390/v12060614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Yang Q., Lin F., Wang Y., Zeng M. and Luo M. (2021) Long noncoding RNAs as emerging regulators of COVID-19. Front. Immunol. 12, 700184 10.3389/fimmu.2021.700184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Kannan A., Suomalainen M., Volle R., Bauer M., Amsler M., Trinh H.V.et al. (2022) Sequence-specific features of short double-strand, blunt-end RNAs have RIG-I- and type 1 interferon-dependent or -independent anti-viral effects. Viruses 14, 1407 10.3390/v14071407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Gomez J.A., Wapinski O.L., Yang Y.W., Bureau J.F., Gopinath S., Monack D.M.et al. (2013) The NeST long ncRNA controls microbial susceptibility and epigenetic activation of the interferon-gamma locus. Cell 152, 743–754 10.1016/j.cell.2013.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Taheri M., Rad L.M., Hussen B.M., Nicknafs F., Sayad A. and Ghafouri-Fard S. (2021) Evaluation of expression of VDR-associated lncRNAs in COVID-19 patients. BMC Infect. Dis. 21, 588 10.1186/s12879-021-06248-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Sabetian S., Castiglioni I., Jahromi B.N., Mousavi P. and Cava C. (2021) In silico identification of miRNA-lncRNA interactions in male reproductive disorder associated with COVID-19 infection. Cells 10, 1480 10.3390/cells10061480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Moazzam-Jazi M., Lanjanian H., Maleknia S., Hedayati M. and Daneshpour M.S. (2021) Interplay between SARS-CoV-2 and human long non-coding RNAs. J. Cell. Mol. Med. 25, 5823–5827 10.1111/jcmm.16596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Cheng J., Zhou X., Feng W., Jia M., Zhang X., An T.et al. (2021) Risk stratification by long non-coding RNAs profiling in COVID-19 patients. J. Cell. Mol. Med. 25, 4753–4764 10.1111/jcmm.16444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Mukherjee S., Banerjee B., Karasik D. and Frenkel-Morgenstern M. (2021) mRNA-lncRNA co-expression network analysis reveals the role of lncRNAs in immune dysfunction during severe SARS-CoV-2 infection. Viruses 13, 402 10.3390/v13030402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Li C.X., Chen J., Lv S.K., Li J.H., Li L.L. and Hu X. (2021) Whole-transcriptome RNA sequencing reveals significant differentially expressed mRNAs, miRNAs, and lncRNAs and related regulating biological pathways in the peripheral blood of COVID-19 patients. Mediators Inflamm. 2021, 6635925 10.1155/2021/6635925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Arora S., Singh P., Dohare R., Jha R. and Ali Syed M. (2020) Unravelling host-pathogen interactions: ceRNA network in SARS-CoV-2 infection (COVID-19). Gene 762, 145057 10.1016/j.gene.2020.145057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Vishnubalaji R., Shaath H. and Alajez N.M. (2020) Protein coding and long noncoding RNA (lncRNA) transcriptional landscape in SARS-CoV-2 Infected bronchial epithelial cells highlight a role for interferon and inflammatory response. Genes (Basel) 11, 760 10.3390/genes11070760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Pontecorvi G., Bellenghi M., Ortona E. and Care A. (2020) microRNAs as new possible actors in gender disparities of Covid-19 pandemic. Acta. Physiol. (Oxf.) 230, e13538 10.1111/apha.13538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Helms J., Severac F., Merdji H., Anglés-Cano E. and Meziani F. (2020) Prothrombotic phenotype in COVID-19 severe patients. Intensive Care Med. 46, 1502–1503 10.1007/s00134-020-06082-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Llitjos J.F., Leclerc M., Chochois C., Monsallier J.M., Ramakers M., Auvray M.et al. (2020) High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J. Thromb. Haemost. 18, 1743–1746 10.1111/jth.14869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Lodigiani C., Iapichino G., Carenzo L., Cecconi M., Ferrazzi P., Sebastian T.et al. (2020) Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb. Res. 191, 9–14 10.1016/j.thromres.2020.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.McFadyen J.D., Stevens H. and Peter K. (2020) The emerging threat of (micro)thrombosis in COVID-19 and its therapeutic implications. Circ. Res. 127, 571–587 10.1161/CIRCRESAHA.120.317447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Szekely Y., Lichter Y., Taieb P., Banai A., Hochstadt A., Merdler I.et al. (2020) Spectrum of cardiac manifestations in COVID-19: a systematic echocardiographic study. Circulation 142, 342–353 10.1161/CIRCULATIONAHA.120.047971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Grimaud M., Starck J., Levy M., Marais C., Chareyre J., Khraiche D.et al. (2020) Acute myocarditis and multisystem inflammatory emerging disease following SARS-CoV-2 infection in critically ill children. Ann. Intensive Care 10, 69 10.1186/s13613-020-00690-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Savoia C., Volpe M. and Kreutz R. (2021) Hypertension, a moving target in COVID-19: current views and perspectives. Circ. Res. 128, 1062–1079 10.1161/CIRCRESAHA.121.318054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z.et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395, 1054–1062 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Ruscica M., Macchi C., Iodice S., Tersalvi G., Rota I., Ghidini S.et al. (2021) Prognostic parameters of in-hospital mortality in COVID-19 patients-An Italian experience. Eur. J. Clin. Invest. 51, e13629 10.1111/eci.13629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Jud P., Kessler H.H. and Brodmann M. (2021) Case report: changes of vascular reactivity and arterial stiffness in a patient with Covid-19 infection. Front. Cardiovasc. Med. 8, 671669 10.3389/fcvm.2021.671669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Connors J.M. and Levy J.H. (2020) COVID-19 and its implications for thrombosis and anticoagulation. Blood 135, 2033–2040 10.1182/blood.2020006000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Goshua G., Pine A.B., Meizlish M.L., Chang C.H., Zhang H., Bahel P.et al. (2020) Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 7, e575–e582 10.1016/S2352-3026(20)30216-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets have been used in producing this work.