Abstract
Coronavirus disease 2019 (COVID-19) presents with symptoms that may be mild or severe. The individual with the severe form of the disease usually presents with a constellation of respiratory symptoms typical of acute respiratory distress syndrome. In this report, we present our experience of the successful management of an oxygen-dependent pregnant woman with severe COVID-19 infection who had 2 sessions of partial exchange blood transfusion. We discussed the principles that informed this intervention and the need to adopt this novel approach in the care of severe COVID-19 infection.
Keywords: ARDS, COVID-19, EBT, Exchange blood transfusion and pregnancy, Nigeria
Introduction
Coronavirus disease 2019 (COVID-19) is a disease caused by a novel strain of coronavirus that causes severe acute respiratory syndrome (SARS-CoV-2). Individuals with a severe form of the disease may present with a constellation of respiratory symptoms typical of acute respiratory distress syndrome (ARDS) 1 requiring some form of ventilatory support. We report our experience with the use of partial exchange blood transfusion for the successful management of a pregnant woman with the severe COVID-19 infection who presented with features of acute respiratory distress syndrome ARDS).
Case report
A 33-year-old gravida 3, para 2 Asian and a known asthmatic at 35 weeks gestation was referred to the Lagos University Teaching Hospital (LUTH). Prior to her referral, she had presented 3 days earlier at a private health facility with complaints of fever, cough, and breathing difficulty of one-day duration. She had no history of recent travel or contact with a confirmed case of COVID-19. She was managed for acute severe asthma without any improvement in her symptoms thus necessitating a chest radiograph that showed features suggestive of pneumonia and acute pulmonary oedema Figure 1A. She had reverse-transcription polymerase chain reaction (RT-PCR) of nasal and nasopharyngeal swabs and was confirmed to have the coronavirus disease 2019 (COVID-19) infection. On admission into the isolation unit of LUTH, her oxygen saturation (SpO2) was 76% on room air and 92% on 100% oxygen at 6 L/min via a non-rebreather mask. She was managed for acute severe asthma but her admission into the intensive care unit was not possible at this time due to the non-availability of bed spaces. The fetal heart rate was 152 beats per minute. However, on the second day of admission (DOA), she had a sudden deterioration of her clinical condition with SpO2 persistently below 88% while on 100% supplemental oxygen. Her laboratory results are as shown in Table 1.
Figure 1.
A – Chest Xray film at presentation showing multiple consolidations in the middle and lower zones predominantly and increased vascular markings
B – Chest X-ray film at discharge showing subtle consolidations in the upper lung zones.
Table 1.
Laboratory parameters
| Laboratory variables | Reference range | Day 2 | Day 3 | Day 4 | Day 7 | Day 8 | Day 9 | Day 12 | Day 14 |
| Sodium (mmol/L) | 135 – 145 | 140 | 141 | 141 | 148‡ | 145 | |||
| Potassium (mmol/L) | 3.5 – 5.1 | 2.8† | 3.6 | 3.3† | 2.5† | 3.9 | |||
| Chloride (mmol/L) | 98 – 110 | 102 | 107 | 89† | 85† | 81† | |||
| Bicarbonate (mmol/L) | 22 – 30 | 20† | 23 | >30‡ | >30‡ | >30‡ | |||
| Creatinine (µmol/L) | 39 – 91 | 37† | 40 | 31† | 20† | 40 | |||
| Urea (mmol/L) | 2.5 – 6.4 | 2.7 | 4.0 | 5.6 | 3.5 | 2.7 | |||
| Anion gap (mmol/L) | 3 – 15 | 18‡ | 11 | 22‡ | 14 | 4 | |||
| Haemoglobin (g/dl) | 12.0 – 16.0 | 10.8† | 11.0† | 11.6† | 12.2 | 10.9† | 11.1† | ||
| Haematocrit (%) | 35 – 48 | 32.6† | 36.9 | 36.7 | 37.6 | 38.5 | 38.6 | ||
| Platelets (x 109/L) | 150 – 450 | 604‡ | 587‡ | 678‡ | 583‡ | 592‡ | 464‡ | ||
| White cell count (x 109/L) | 4.0 – 11.0 | 11.9‡ | 18.1‡ | 15.6‡ | 15.7‡ | 14.3‡ | 9.9 | ||
| Neutrophils (x 109/L) | 2.0 – 7.5 | 8.67‡ | 14.41‡ | 13.43‡ | 13.55‡ | 11.88‡ | 7.6‡ | ||
| Lymphocytes (x 109/L) | 1.0 – 4.0 | 2.25 | 2.59 | 1.38 | 1.58 | 1.10 | 1.10 | ||
| Monocytes (x 109/L) | 0.00 – 1.00 | 0.63 | 0.48 | 3.0 | 0.13 | 0.78 | 0.50 | ||
| Eosinophils (x 109/L) | 0.00 – 0.40 | 0.33 | 0.54 | 0.46 | 0.40 | 0.47 | 0.74 | ||
| Basophils (x 109/L) | 0.00 – 0.10 | 0.04 | 0.05 | 0.01 | 0.06 | 0.06 | 0.05 | ||
| INR | 0.9 – 1.3 | 0.85† | 0.94 | 1.02 | |||||
| ALP (U/L) | 40 – 120 | 188‡ | 105 | ||||||
| ALT/SPGT (U/L) | 10 – 40 | 31.1 | 25.4 | ||||||
| AST/SGOT (U/L) | 10 – 42 | 65.0‡ | 34.1 | ||||||
| Gamma GT T(U/L) | 7 -64 | 132‡ | 42.0 | ||||||
| PH | 7.40 | 7.36 | 7.51 | ||||||
| PaCO2 (mmHg) | 35 | 52 | 40 | ||||||
| PaO2 (mmHg) | 96 | 49 | - | ||||||
| Lactate (mmol/L) | 1.2 | 1.6 | 1.2 | ||||||
| FiO2 | 0.96 | 0.96 | - |
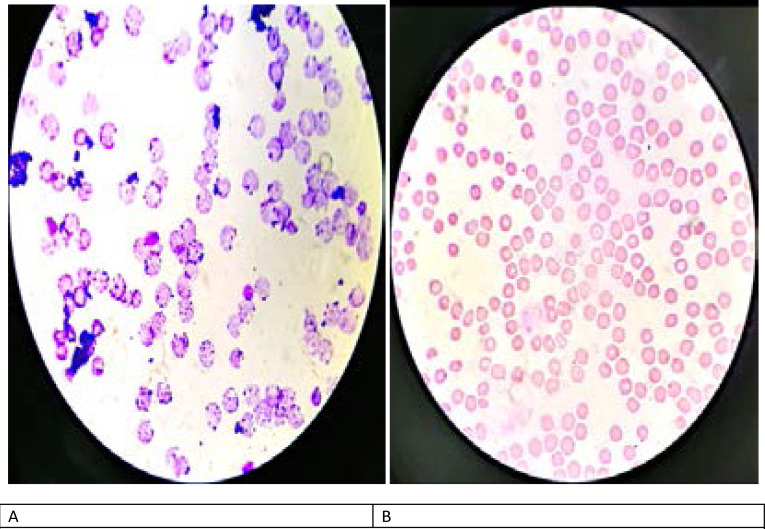
Elevated level beyond reference range
She subsequently had an emergency caesarean section performed under spinal anaesthesia and was delivered of a live female neonate weighing 3500 grams. Postoperatively, her clinical condition deteriorated further with worsening SpO2 (74 – 91%) despite being on continuous positive airway pressure (CPAP) with non-invasive ventilation delivering oxygen at 15 L/min via a non-rebreather mask. The peripheral blood film done on the 10th DOA revealed Heinz bodies (methaemoglobin) in nearly 100% of her red blood cells Figure 2A. She subsequently had 2 sessions of EBT on the 12th DOA with a total of 4 units of whole blood transfused over 2 days. Following this, her condition improved significantly with a minimum SpO2 of 95% while on supplemental oxygen at 3–5 L/min. Her red cells now showed a significant reduction in methaemoglobin level Figure 2B. She was later transferred to the regular postnatal ward on the 16th DOA, having tested negative for COVID-19. She was discharged home with her baby after 22 DOA and then scheduled for a postnatal follow-up visit 2 weeks later. Figure 1B shows her chest X-ray at discharge.
Figure 2.
A – Patient red cells showing Heinz bodies pre-exchange transfusion X100
B – Patient red cells 4 days post-exchange transfusion (Heinz bodies hardly visible) X100
Discussion
Our knowledge regarding COVID-19 infection is still evolving at this time. The new thinking is that COVID-19 induced hypoxaemia as described in our patient may not solely be related to pulmonary pathology thus the premise for the use of EBT in our management. Oxygen is getting to the lungs but the red cells flowing in the alveolar capillary may have haemoglobin incapable of extracting and complexing with the oxygen. Wenzhong et al have shown that some SARS-CoV-2 regulatory proteins can impair haem synthesis and also cause dissociation of ferrous ion (Fe2+) from already formed haemoglobin, resulting in the inability of haemoglobin to transport oxygen to the tissues2. In particular, Coronavirus non-structural proteins OrfLab, ORF3a and the ORF10 were shown to be capable of complexing with the haem of the β -1 haemoglobin chain. This complex formation results in the dissociation of iron from the haem and the oxidation of Fe2+ to ferric ion (Fe3+) resulting in the formation of methaemoglobin2 which is incapable of carrying oxygen.
Thus, we premise that although our patient had a haemoglobin concentration optimal for pregnancy and puerperium, however, this only existed in a form incapable of reversible oxygen transfer. Recently, an alternative mechanism of SARS-Cov-2 induced haemoglobinopathy was also proposed – “the ferroptotic dysplasia”3. The viral protein is biodegraded by cellular proteases to smaller molecules which happen to have a remarkable resemblance to the master regulator of iron metabolism (hepcidin), thus providing the basis of the protein mimicry effect. This viral protein complexes with ferroportin and degrades it, resulting in impairment of iron release from cells into plasma (hypoferremia) and cellular iron accumulation. A situation is then created where there is a peripheral lack of iron, but the tissues are overloaded with iron. The excess cellular iron activates Fenton's chemistry with the generation of reactive oxygen species that progressively lead to cell death, a process referred to as ferroptosis4.
The ferroptotic events in erythroid blasts and red cells create a sideroblastic-like pathology with myelodysplastic features that should require the replacement of dysfunctional erythrocytes3. Finally, we also submit that the dramatic recovery observed in our patient after EBT may be due to the partial removal of inflammatory cytokines which is known to characterize severe COVID-19 infection. The virus induces severe inflammatory apoptosis (pyroptosis) resulting in the production of damaged cellular organelles resulting in Damaged-Associated-Molecular Patterns (DAMP)5. DAMP stimulates the macrophages and T-cells to produce chemokines and cytokines. These cytokines in a positive feedback mechanism caused the production of more cytokines (cytokine storm) which is associated with poor patient's survival5. Removal of these cytokines using an adsorbent agent in extracorporeal circulation has been shown to reverse severe disease in septic patients6. Therefore, an EBT may be an easier and cheaper alternative to extracorporeal blood purification in resource-limited settings such as ours.
Conclusion
Exchange Blood transfusion appeared to be key to the reversal of oxygen dependency in a patient with severe COVID-19 pneumonia and this may have a role to play as an alternative to extracorporeal blood purification especially in resource-limited settings.
Acknowledgements
The authors appreciate the index patient for agreeing and consenting for her information to be used in this case report. We also acknowledge the special contributions of Dr JO Olatosi, Dr MK Rotimi, Dr OE Ekor, Prof I Desalu, Dr O Ozoh, Dr TA Adeyemo, Dr MG Dania, Prof. I Desalu, Prof. VC Ezeaka, Prof. AC Mbakwem, Mr RW Dada, and Nurses and Doctors of the COVID-19 Isolation Ward LUTH to the management of the index patient.
Conflict of interest
None declared.
Funding Statement
The authors received no external funding for this case report.
Ethical Approval
Ethics approval for this report was obtained from the human research and ethics committee of the public tertiary hospital where the patient was being managed.
Consent
The authors certify that they have obtained all appropriate patient consent. In the form, she has given her consent for her images and other clinical information to be reported in the journal. The patient understood that all her identifiable information will not be published.
Guarantor
The corresponding author (KSO) will be the guarantor for this paper.
References
- 1.Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol. 2020;215(1):87–93. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 2.Wenzhong L, Hualan L. COVID-19 Disease: ORF8 and surface glycoprotein inhibit heme metabolism by binding to porphyrin. Chem Rxiv. 2020 doi: 10.26434/chemrxiv.11938173.v3. Preprint. [DOI] [Google Scholar]
- 3.Cavezzi A, Troiani E, Corrao S. COVID-19: hemoglobin, iron, and hypoxia beyond inflammation. A narrative review. Clin Pract. 2020 May 28;10(2):1271. doi: 10.4081/cp.2020.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hirschhorn T, Stockwell BR. The development of the concept of ferroptosis. Free Radic Biol Med. 2019;133:130–143. doi: 10.1016/j.freeradbiomed.2018.09.043. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet Internet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Q, Hu Z. Successful recovery of severe COVID-19 with cytokine storm treating with extracorporeal blood purification. Int J Infect Dis. 2020;96:618–620. doi: 10.1016/j.ijid.2020.05.065. [DOI] [PMC free article] [PubMed] [Google Scholar]