Abstract
In elderly chronic kidney disease (CKD) patients, isolated systolic hypertension is common, the rate of renal function decline is slow, and there is a high possibility of physical damage due to side effects such as drug use-related orthostatic hypotension. Therefore, there are still many questions about whether lowering blood pressure in elderly patients will actually improve prognosis. Since many blood pressure-related clinical studies exclude advanced CKD and the elderly, it is particularly difficult to define target blood pressure in these populations. A randomized controlled trial is needed to establish optimal blood pressure targets and treatment strategies in elderly patients with CKD. This review seeks to summarize the guidelines available at this time.
Keywords: Hypertension, Elderly, Chronic kidney disease
INTRODUCTION
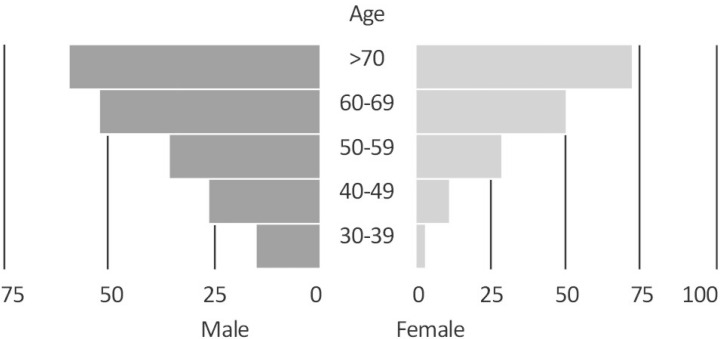
The prevalence of hypertension among Korean men over the age of 60 is over 50%, and in Korean women older than 70, it is over 70% (Fig. 1). However, there is no clear policy on hypertension treatment for elderly chronic kidney disease (CKD) patients in Korea and other countries. As a result, clinicians continue to make decisions based on their personal experience with controlling blood pressure. The 2012 KDIGO (Kidney Disease: Improving Global Outcomes) CKD Hypertension Guidelines were updated in 2021, but did not mention elderly hypertension1,2). There are several guidelines for the management of hypertension in elderly patients without CKD, but there are no guidelines for hypertension among elderly with CKD or for patients with CKD undergoing dialysis3,4). As an aging society, elderly patients will become more and more common, and we are not sure whether clinicians are controlling blood pressure adequately among such patients. A prospective study is needed to set optimal blood pressure targets and treatment strategies for elderly patients with CKD in the future. This review seeks to summarize the guidelines available at this time.
Fig. 1. Korea Centers for Disease Control and Prevention (KCDC) Chronic Disease Health Statistics 2019 Prevalence of Hypertension.
1. Current status of hypertension management in elderly CKD patients
In Korea, there are only data of patients with all typed hypertension not specific condition like CKD. In the results of the National Health and Nutrition Examination Survey of the Korea Centers for Disease Control and Prevention, the proportion of patients with blood pressure less than 140/90 mmHg was only 45.1%. Among patients with diabetes, CKD, or cardiovascular disease, a lower result is likely considering a treatment rate of less than 130/80 mmHg (disease specific guideline). In one study, 75% of hypertensive patients aged 75 years and older did not reach their target blood pressure, and 50% did not understand the medical staff's explanation of hypertension5). Why are elderly patients who have been diagnosed with CKD passive in the treatment of hypertension? First, the medical staff understands isolated systolic hypertension as a phenomenon of aging and considers diastolic hypotension feeling pressure, and the medical staff passively responds to treatment. Second, they are hesitant to apply the guideline of <130/80 mmHg to elderly patients due to a lack of evidence because elderly patients were not included in many clinical studies6). However, after the SPRINT study (meta-analyses of randomized trials, more intensive versus standard BP control was associated with a lower risk of all-cause mortality in patients with CKD and albuminuria but not in those without CKD), targeting a blood pressure of <130/80 mmHg with appropriate office blood pressure measurements may be an option for patients with CKD. The presence of albuminuria should be further considered to determine individualized BP targets7).
2. Criteria for hypertension among elderly CKD patients
The 2012 KDIGO guidelines suggested a target blood pressure of less than 130/80 mmHg in those with a 24-hour urine albumin of 30 mg or more. In the 2021 KDIGO guidelines, a target blood systolic pressure of less than 120 mmHg was recommended for the urine albumin-creatinine ratio exceeded 30 mg (A3) for all CKD patients not on dialysis1,2). In the 2017 SPRINT study, more than 40% of patients with CKD were aged 75 years or older and the low BP target reduced mortality even in this subgroup. This means beneficial effect of strict BP control for elderly CKD patients, directly not applied to extremely elderly above 90 years old patients8). In another study, renal function was associated with mortality in CKD patients aged 60 years and older, and there was no difference in mortality between systolic blood pressures (SBP) 140-169 mmHg, while SBP less than 120 mmHg was rather increased mortality9).
The ACC/AHA guidelines place importance on clinical judgment and patient preference when setting blood pressure targets for elderly patients with limited life expectancy as well as multiple comorbidities, frequent falls, progressive cognitive impairment. The ACC/AHA also argues for the need for further randomized controlled trials (RCTs) of blood pressure in elderly patients10). The 2018 European Society of Cardiology/European Society for Hypertension (ESC/ESH) BP guidelines classify the elderly into two subgroups. 'Elderly' refers to patients aged between 65 and 79, and 'super-elderly' refers to those over 80 years of age. The guidelines recommend that drug treatment should be provided to all elderly patients with an SBP of 160 mmHg or greater, and that low treatment targets for SBP 130-139 and diastolic blood pressure (DBP) 70-79 mmHg should also be achieved in elderly patients (≥65 years, but not >80 years)11). Drug therapy may also be considered for healthy individuals over 80 years of age with an initial SBP ≥160 mmHg and/or DBP ≥90 mmHg targeting a blood pressure of 130-139/70-79 mmHg. These decisions are based on a thorough review of biological age and comorbidities. The need for close monitoring of side effects of treatment, especially in frail patients, is emphasized. Although definitions and treatment thresholds differ between the US and European guidelines, both acknowledge the importance of BP treatment in the elderly to lower the risk of cardiovascular disease, but recommend a cautious approach and close monitoring of these patients (Table 1)4,11,12).
Table 1. A Comparison of blood pressure thresholds and targets between ACC/AHA, ACP/AAFP, and ESC/ESH guidelines.
ACC/AHA, American college of cardiology/American heart association; ACP/AAFP, American College of Physicians/American Academy of Family Physicians; ESC/ESH, European Society of Cardiology/European Society of Hypertension; SBP, systolic blood pressure; DBP, diastolic blood pressure
3. Ambulatory blood pressure monitoring (ABPM) in elderly patients with CKD
Clinic BP measurements, even when corrected by home self-measurements, cannot quantify 24-h blood pressure patterns and sleep BP levels, and thus may misclassify as many as half of all adults assessed. ABPM should be considered the new standard for diagnosing true hypertension, accurately assessing the resulting tissue/organ and CVD risk, and individualizing treatment for hypertension. ABPM may be an appropriate blood pressure measurement method for those with a blunted nocturnal decrease in blood pressure and who may be at increased risk for CVD in the elderly and obese, as well as patients with CKD13,14). Although rarely studied in elderly patients with chronic kidney disease, aging itself causes decreases in cardiac output and heart rate, ventricular hypertrophy, decreased left ventricular filling, plasma renin, and decreases in renal and peripheral resistance. Aging also causes increased arterial stiffness, decreased compliance, increased pulse pressure, and leads to increased ISH frequency with increased peripheral resistance. There are other concomitant diseases such as diabetes, chronic kidney disease, lung disease, depression, neoplasia, etc. that must be considered when making diagnosis and treatment decisions15,16).
A major limitation of both ABPM and HBPM as primary measures of hypertension management is the lack of clinical trials using these BPs to determine treatment eligibility and treatment goals. However, the role of ABPM in accurately measuring changes in blood pressure in elderly patients with chronic kidney disease is more important than in general patients, and should be used to determine the criteria for drug use through many studies17,18).
4. Specific issues and the purpose of treatment of hypertension in elderly patients with CKD
1) Isolated systolic hypertension
The diastolic hypotension seen in the elderly can be an important variable in blood pressure control in CKD patients. In a study reported in China, most elderly CKD patients with uncontrolled hypertension had isolated systolic hypertension, and risk factors included stage 3 or 4 CKD, obesity, and diabetes19). If a subject with isolated systolic hypertension appears to have an “optimal” diastolic blood pressure (DBP) of 70 mmHg, but SBP above 130 mmHg, it becomes difficult for the clinician to determine the correct course of treatment. A more rational antihypertensive regimen that targets SBP levels without excessively lowering DBP is needed, as DBP below 60 mmHg in frail elderly patients is associated with aortic stiffness and decreased survival independent of left ventricular function20).
2) Renal outcomes and hypertension in elderly patients
According to the Kidney Early Evaluation Program(KEEP) study, the risk of end-stage renal disease was increased when SBP exceeded 140 mmHg in the community base sample, and that risk was higher in those of DBP higher than 90 mmHg rather less than 60 mmHg. The risk of end-stage renal disease did not increase with age when SBP was adjusted in this study21). The chronic renal insufficiency cohort study (a prospective longitudinal study) showed a strong correlation between the progression of CKD and SBP >130 mmHg, but the average age was 58 years, making it difficult to apply to elderly patients22). In the SPRINT study, lowering SBP from less than 140 mmHg to less than 120 mmHg in non-diabetic patients was meaningful in lowering cardiovascular mortality, but it did not lead to significant improvement in renal clinical outcomes9). KDIGO's 2021 Chronic Kidney Disease Hypertension Treatment Guidelines suggested targets according to diabetes and proteinuria, but failed to provide age-specific blood pressure targets or drug treatment policies because no solid evidence was provided2). For the purpose of improving renal outcomes in elderly patients with CKD, caution is needed when lowering blood pressure. In particular, there is little evidence for lowering it below 120 mmHg.
3) Cardiovascular outcomes and hypertension in elderly patients
The risk of cardiovascular complications according to blood pressure increases in CKD patients over 60 years of age, but there is no significant effect in patients over 70 years of age9). In an analysis of stage 4 CKD and myocardial infarction, heart failure, and stroke, no statistically significant difference was found even when SBP increased to 180 mmHg or decreased below 120 mmHg9). Although mortality increases as blood pressure rises, it can be interpreted to mean that there are many causes of death other than cardiovascular disease in the CKD elderly patients. In the SPRINT study, setting the enrollment criteria to include a group with a high risk of cardiovascular complications has implications in terms of prevention of cardiovascular complications in elderly patients with CKD. Even if progression of CKD and incidence of end-stage renal disease cannot be reduced, it is better to lower blood pressure in the elderly in order to prevent cardiovascular complications unless the risk increases2).
4) Cognitive function and hypertension in elderly patients
Age was found to be factors that predicted cognitive dysfunction at different functional levels of CKD23). The risk of ESKD development was higher in subjects diagnosed with Alzheimer disease, suggesting that central nervous system diseases can adversely affect kidney function in elderly people24).
Hypertension contributes to the development of various cardiovascular diseases in elderly patients and is associated with cognitive decline and dementia, and cognitive impairment increases morbidity and mortality in elderly patients with hypertension25). We found that the correlation between BP and cognitive function risk is non-linear and depends on the age of the patient, and intensive blood pressure control is generally not recommended, especially in the elderly. Increased blood pressure variability and orthostatic hypotension in older adults also increase the risk of cognitive decline26). Recent studies have linked changes in active blood pressure to cognitive function. High nocturnal SBP levels27), Non-dipper status28) and exaggerated blood pressure variability are suggested as important determinants of cognitive impairment. Additionally, ABPM has been shown to be an independent factor for brain atrophy in older adults29). Therefore, active blood pressure control for high-risk groups such as chronic kidney disease using ABPM is expected to be helpful17).
4. Drug therapy for elderly patients with CKD
In the case of elderly patients, the selection and dose of antihypertensive drugs should consider the risk of side effects such as hypotension, electrolyte imbalance, and impaired renal function30). In particular, the incidence of hyperkalemia, acute kidney injury, and orthostatic hypotension due to the use of antihypertensive drugs in elderly patients with CKD is higher than in elderly patients without CKD31,32). Currently, guidelines such as KDIGO do not mention how to prescribe antihypertensive drugs for elderly patients with CKD.
According to the guidelines for hypertension in elderly patients published in China in 2019, if a CKD patient has proteinuria, angiotensin converting enzyme inhibitor (ACEI) or angiotensin II receptor blocker (ARB) should be used, starting with a low dose and increasing to the highest dose3). Patients with CKD stage 3-4 should start at half the initial dose, and potassium and renal function tests should be conducted. Simultaneous use of ACEI and ARB is not recommended, and loop diuretics should be used for edema in CKD stages 4 and 53). Calcium channel blocker (CCBs) should be used in patients with apparent renal function decline or salt sensitivity, and alpha/beta receptor blockers should be considered in patients with resistant hypertension3).
In the 2021 KDIGO guidelines, the selection of antihypertensive drugs is recommended to start with monotherapy for those over 75 years of age, and to sequentially combine ACEI or ARB with a thiazide-based diuretic (loop diuretics for advanced CKD) or CCB2). Considering the risk of thiazide induced hyponatremia, chlorothalidone had good clinical results for lowering blood pressure in advanced CKD patients33), however, the enrolled mean age was below 60 years old (HEBE-CKD trial) even if it was RCT study34). In other studies, chlorthalidone was associated with a greater incidence of hypokalemia and hyponatremia of equal dose compared with thiazide, therefore we consider to follow up the electrolyte for a while35,36). In the case of the combination of ARB and CCB, the OSCAR study (An angiotensin II receptor blocker-calcium channel blocker combination prevents cardiovascular events in elderly high-risk hypertensive patients with chronic kidney disease better than high-dose angiotensin II receptor blockade alone) confirmed that the incidence of fatal and non-fatal cardiovascular events and cerebrovascular disease was lower in elderly patients with CKD than with high-dose ARB treatment37). This study was conducted with an average age of 75 years old among those with stage 3 CKD. In elderly patients with CKD, combination therapy not only reduces side effects but also has an additional blood pressure lowering effect38).
Elderly patients with CKD and many comorbidities may have reduced drug compliance due to the large number of medications they are taking. In combination therapy, methods to increase drug compliance with a fixed-dose combination should also be considered. Finally, we summarize the guidelines available at this time and make suggestions for managing blood pressure in elderly patients with CKD (Table 2).
Table 2. Suggestion of blood pressure control in elderly chronic kidney disease.
SBP, systolic blood pressure; DBP, diastolic blood pressure; CKD, chronic kidney disease; ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker
5. Conclusion
In the current studies and guidelines, strict blood pressure control in elderly hypertensive patients with chronic kidney disease is helpful in reducing cardiovascular complications and mortality. To this end, we need additional research to set treatment criteria tailored to the characteristics of patients, determine the use of drugs, and reduce side effects of drugs.
Acknowledgements
Special thanks to: The Korean Society of Geriatric Nephrology
References
- 1.Taler SJ, Agarwal R, Bakris GL, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for management of blood pressure in CKD. Am J Kidney Dis. 2013;62:201–213. doi: 10.1053/j.ajkd.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cheung AK, Chang TI, Cushman WC, et al. Executive summary of the KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int. 2021;99:559–569. doi: 10.1016/j.kint.2020.10.026. [DOI] [PubMed] [Google Scholar]
- 3.Hua Q, Fan L, Li J Joint Committee for Guideline R. 2019 Chinese guideline for the management of hypertension in the elderly. J Geriatr Cardiol. 2019;16:67–99. doi: 10.11909/j.issn.1671-5411.2019.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brook RD, Rajagopalan S. 2017 ACC/ AHA/ AAPA/ ABC/ ACPM/ AGS/ APhA/ ASH/ ASPC/ NMA/ PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Soc Hypertens. 2018;12:238. doi: 10.1016/j.jash.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Ikeda Y, Sasaki T, Kuwahata S, et al. Management instructions for elderly patients with hypertension. Clin Exp Hypertens. 2020;42:295–301. doi: 10.1080/10641963.2019.1649685. [DOI] [PubMed] [Google Scholar]
- 6.Fischer MJ, O'Hare AM. Epidemiology of hypertension in the elderly with chronic kidney disease. Adv Chronic Kidney Dis. 2010;17:329–340. doi: 10.1053/j.ackd.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Jung HH. Hypertension Management in Patients with Chronic Kidney Disease in the Post-SPRINT Era. Electrolyte Blood Press. 2021;19:19–28. doi: 10.5049/EBP.2021.19.2.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.SPRINT Research Group. Wright JT, Jr, Williamson JD, Whelton PK, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Masoli JAH, Delgado J, Bowman K, et al. Association of blood pressure with clinical outcomes in older adults with chronic kidney disease. Age Ageing. 2019;48:380–387. doi: 10.1093/ageing/afz006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Correction to: 2020 ACC/AHA Guideline on the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2021;143:e784. doi: 10.1161/CIR.0000000000000966. [DOI] [PubMed] [Google Scholar]
- 11.Williams B, Mancia G, Spiering W, et al. [2018 ESC/ESH Guidelines for the management of arterial hypertension] Kardiol Pol. 2019;77:71–159. doi: 10.5603/KP.2019.0018. [DOI] [PubMed] [Google Scholar]
- 12.Qaseem A, Wilt TJ, Rich R, Humphrey LL, et al. Pharmacologic Treatment of Hypertension in Adults Aged 60 Years or Older to Higher Versus Lower Blood Pressure Targets: A Clinical Practice Guideline From the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017;166:430–437. doi: 10.7326/M16-1785. [DOI] [PubMed] [Google Scholar]
- 13.International Society for Chronobiology; American Association of Medical Chronobiology and Chronotherapeutics; Spanish Society of Applied Chronobiology, Chronotherapy, and Vascular Risk; Spanish Society of Atherosclerosis; Romanian Society of Internal Medicine. Hermida RC, Smolensky MH, Ayala DE, Portaluppi F. 2013 ambulatory blood pressure monitoring recommendations for the diagnosis of adult hypertension, assessment of cardiovascular and other hypertension-associated risk, and attainment of therapeutic goals. Chronobiol Int. 2013;30:355–410. doi: 10.3109/07420528.2013.750490. [DOI] [PubMed] [Google Scholar]
- 14.Magdás A, Szilágyi L, Belényi B, Incze A. Ambulatory monitoring derived blood pressure variability and cardiovascular risk factors in elderly hypertensive patients. Biomed Mater Eng. 2014;24:2563–2569. doi: 10.3233/BME-141071. [DOI] [PubMed] [Google Scholar]
- 15.Logan AG. Clinical Value of Ambulatory Blood Pressure Monitoring in CKD. Am J Kidney Dis. 2022:S0272-6386(22)00827-00827. doi: 10.1053/j.ajkd.2022.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Maselli M, Giantin V, Franchin A, et al. Detection of blood pressure increments in active elderly individuals: The role of ambulatory blood pressure monitoring. Nutr Metab Cardiovasc Dis. 2014;24:914–920. doi: 10.1016/j.numecd.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Mediavilla García JD, Jaén Águila F, Fernández Torres C, Gil Extremera B, Jiménez Alonso J. Ambulatory blood pressure monitoring in the elderly. Int J Hypertens. 2012;2012:548286. doi: 10.1155/2012/548286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Angeli F, Verdecchia P, Poltronieri C, et al. Ambulatory blood pressure monitoring in the elderly: Features and perspectives. Nutr Metab Cardiovasc Dis. 2014;24:1052–1056. doi: 10.1016/j.numecd.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 19.Cai G, Zheng Y, Sun X, Chen X. Survey of Prevalence A, Treatment Rates in Chronic Kidney Disease Patients with Hypertension in China Collaborative G. Prevalence, awareness, treatment, and control of hypertension in elderly adults with chronic kidney disease: results from the survey of Prevalence, Awareness, and Treatment Rates in Chronic Kidney Disease Patients with Hypertension in China. J Am Geriatr Soc. 2013;61:2160–2167. doi: 10.1111/jgs.12551. [DOI] [PubMed] [Google Scholar]
- 20.Protogerou AD, Safar ME, Iaria P, et al. Diastolic blood pressure and mortality in the elderly with cardiovascular disease. Hypertension. 2007;50:172–180. doi: 10.1161/HYPERTENSIONAHA.107.089797. [DOI] [PubMed] [Google Scholar]
- 21.Peralta CA, Norris KC, Li S, et al. Blood pressure components and end-stage renal disease in persons with chronic kidney disease: the Kidney Early Evaluation Program(KEEP) Arch Intern Med. 2012;172:41–47. doi: 10.1001/archinternmed.2011.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anderson AH, Yang W, Townsend RR, et al. Time-updated systolic blood pressure and the progression of chronic kidney disease: a cohort study. Ann Intern Med. 2015;162:258–265. doi: 10.7326/M14-0488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weng SC, Shu KH, Tang YJ, et al. Progression of cognitive dysfunction in elderly chronic kidney disease patients in a veteran's institution in central Taiwan: A 3-year longitudinal study. Intern Med. 2012;51:29–35. doi: 10.2169/internalmedicine.51.5975. [DOI] [PubMed] [Google Scholar]
- 24.Kang SC, Koh HB, Kim HW, et al. Associations among Alzheimer disease, depressive disorder, and risk of end-stage kidney disease in elderly people. Kidney Res Clin Pract. 2022:8. doi: 10.23876/j.krcp.21.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Owens DK, Davidson KW, Krist AH, et al. Screening for Cognitive Impairment in Older Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2020;323:757–763. doi: 10.1001/jama.2020.0435. [DOI] [PubMed] [Google Scholar]
- 26.Yang W, Luo H, Ma Y, Si S, Zhao H. Effects of Antihypertensive Drugs on Cognitive Function in Elderly Patients with Hypertension: A Review. Aging Dis. 2021;12:841–851. doi: 10.14336/AD.2020.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kanemaru A, Kanemaru K, Kuwajima I. The effects of short-term blood pressure variability and nighttime blood pressure levels on cognitive function. Hypertension Research. 2001;24:19–24. doi: 10.1291/hypres.24.19. [DOI] [PubMed] [Google Scholar]
- 28.Yamamoto Y, Akiguchi I, Hayashi M, Ohara T, Ozasa K, Oiwa K. The relationship between 24-hour blood pressure readings, subcortical ischemic lesions and vascular dementia. Cerebrovascular Diseases. 2005;19:302–308. doi: 10.1159/000084498. [DOI] [PubMed] [Google Scholar]
- 29.Goldstein IB, Bartzokis G, Guthrie D, Shapiro D. Ambulatory blood pressure and brain atrophy in the healthy elderly. Neurology. 2002;59:713–719. doi: 10.1212/wnl.59.5.713. [DOI] [PubMed] [Google Scholar]
- 30.Dagli RJ, Sharma A. Polypharmacy: A global risk factor for elderly people. J Int Oral Health. 2014;6:i–ii. [PMC free article] [PubMed] [Google Scholar]
- 31.Marcum ZA, Fried LF. Aging and antihypertensive medication-related complications in the chronic kidney disease patient. Curr Opin Nephrol Hypertens. 2011;20:449–456. doi: 10.1097/MNH.0b013e32834902ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ponticelli C, Sala G, Glassock RJ. Drug management in the elderly adult with chronic kidney disease: A review for the primary care physician. Mayo Clin Proc. 2015;90:633–645. doi: 10.1016/j.mayocp.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 33.Agarwal R, Sinha AD, Cramer AE, et al. Chlorthalidone for Hypertension in Advanced Chronic Kidney Disease. N Engl J Med. 2021;385:2507–2519. doi: 10.1056/NEJMoa2110730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Solis-Jimenez F, Perez-Navarro LM, Cabrera-Barron R, et al. Effect of the combination of bumetanide plus chlorthalidone on hypertension and volume overload in patients with chronic kidney disease stage 4-5 KDIGO without renal replacement therapy: A double-blind randomized HEBE-CKD trial. BMC Nephrol. 2022;23:316. doi: 10.1186/s12882-022-02930-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Blijderveen JC, Straus SM, Rodenburg EM, et al. Risk of hyponatremia with diuretics: Chlorthalidone versus hydrochlorothiazide. Am J Med. 2014 Aug;127:763–771. doi: 10.1016/j.amjmed.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 36.Dhalla IA, Gomes T, Yao Z, et al. Chlorthalidone versus hydrochlorothiazide for the treatment of hypertension in older adults: A population-based cohort study. Ann Intern Med. 2013;158:447–455. doi: 10.7326/0003-4819-158-6-201303190-00004. [DOI] [PubMed] [Google Scholar]
- 37.Kim-Mitsuyama S, Ogawa H, Matsui K, Jinnouchi T, Jinnouchi H, Arakawa K. An angiotensin II receptor blocker-calcium channel blocker combination prevents cardiovascular events in elderly high-risk hypertensive patients with chronic kidney disease better than high-dose angiotensin II receptor blockade alone. Kidney Int. 2013;83:167–176. doi: 10.1038/ki.2012.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122:290–300. doi: 10.1016/j.amjmed.2008.09.038. [DOI] [PubMed] [Google Scholar]