Abstract
Introduction:
Cancer research is critical for cancer control policies; however, the state of cancer research activities in Botswana is largely unknown. The goal of this review was to describe trends and patterns of cancer research outputs in Botswana.
Methods:
PubMed, Web of Science, EBSCOhost, African Journals Online, and African Index Medicus databases were systematically searched for peer-reviewed, primary cancer-related research articles published on the Botswana population or by Botswana institutions between January 2009 and June 2021.
Results:
Of the 86 publications included, 39 (45 %) were about cervical cancer, followed by breast cancer (10 %) and Kaposi sarcoma (7 %). The remainder (27 %) were not focused on any specific cancer type. The research activities were skewed towards three main areas of scientific interest: early detection, diagnosis, and prognosis; cancer control, survivorship, and outcomes; and treatment. Botswana was represented by authors in the first (54 %), last (53 %), and any authorship (53 %) positions. The United States of America had the strongest collaborative partnerships with Botswana, followed by the United Kingdom and South Africa. The majority of funding institutions were American (76 %) and the National Institutes of Health was the most mentioned funding organization, accounting for 33 % of all financial acknowledgments. Only 9 % of the funding acknowledgments came from Botswana.
Conclusion and policy summary:
Although cancer research in Botswana is expanding because of substantial foreign assistance, it is also hampered by a lack of local funding, minimal participation by Botswana-affiliated researchers, and research that is not aligned with disease burden. Our study highlights the need to strengthen local research capacity in Botswana.
Keywords: Bibliometrics, Cancer, Botswana, Research
1. Introduction
Cancer constitutes a significant burden of non-communicable diseases (NCDs) globally. With almost 10 million deaths in 2020, it was a leading cause of death worldwide [1]. Breast, lung, and colorectal cancers account for the vast majority of cancer research outputs worldwide, which is in line with their contribution to the global cancer burden [2,3]. However, the incidence and mortality of many types of cancer vary across different regions of the world [3]. For example, the proportion of cancers attributable to infections is highest in sub-Saharan Africa (SSA) and East and Central Asia [4]. Kaposi sarcoma and cervical cancer, caused by human herpesvirus type 8 (HHV-8) and human papilloma virus (HPV), respectively, are significant contributors to the cancer burden in SSA [5]. The burden of infection-attributable cancers in East Asia is mainly driven by Helicobacter pylori-associated gastric cancer [4]. In contrast, cancers associated with lifestyle factors (such as lung, breast, and prostate cancer) are more common in developed countries of Europe, North America, and Australasia [3]. These geographical variations in cancer burden suggest that the cancer research agenda may differ by region or country.
Botswana is an upper middle-income country [6] in SSA with health concerns such as high human immunodeficiency virus (HIV) prevalence, HIV-related co-morbidities, and increasing rates of NCDs including cancer [7–9]. Botswana also has a distinct cancer burden, with 70 % of reported cases of cancer diagnosed at advanced stages and cancer deaths accounting for 7 % of all deaths [9]. The cancer burden is exacerbated by a persistent high prevalence of HIV, despite the country being on course to attaining the UNAIDS 95–95-95 targets, with 92 % of individuals who know their HIV status on treatment and 90 % of the people accessing treatment virally suppreseed [10]. Cervical cancer (18.6 %), breast cancer (10.4 %), and Kaposi sarcoma (10 %) were the most common incident malignancies in Botswana in 2020 for both sexes and all ages [11]. While the incidence of Kaposi sarcoma has declined following increased coverage of antiretroviral therapy (ART) in Botswana, the incidence of non-Hodgkin lymphoma (NHL) and HPV-associated cancers has increased [12]. More than 60 % of cancers in Botswana arise in HIV-infected individuals [12,13] and are often diagnosed at advanced stages of the disease, resulting in poorer outcomes despite the successful ART program [14–16]. Botswana offers a cervical cancer screening program; however, the majority of women have never been screened, and those who have been screened frequently face inordinate delays in receiving a pathology diagnosis [16–18].
Botswana’s Ministry of Health (MoH) has developed a multisectoral strategy for the prevention and control of NCDs (2018–2023) in response to the increased burden of cancer and other NCDs [9]. The strategy prioritizes policy-relevant research that can improve understanding of disease burden, develop novel solutions, and assess the effectiveness of interventions. Cancer research is essential for understanding the causes of cancer and creating new treatment methods to improve patient care [19]. Therefore, building research capacity is a priority of the MoH strategy, as evidenced by its objectives to increase the number of NCD publications and Botswana-led NCD publications each by 25 % by 2023 [9].
The incidence of cancer is rising in Botswana [8,12,20]. However, the impact of rising cancer incidence on cancer research has not been investigated. A simple PubMed search showed a steady increase in cancer-related research outputs in Botswana from 2009 to 2021 (Supplementary Fig. S1) [21]. Substantial research infrastructure and research opportunities for cancer exist in Botswana [8,22]. However, cancer research outputs and participation of local institutions in cancer research have not been formally reviewed, so there is a need to evaluate cancer research outputs in Botswana. A bibliometric analysis was therefore conducted to systematically describe patterns of cancer research, including the proportionality of research outputs to disease burden, funding, and authorship, between 2009 and 2021. The findings could assist cancer researchers, funding organizations, and governments to establish cancer research priorities in Botswana.
2. Methods
2.1. Literature search
A pre-determined search strategy adapted from a previously published protocol [23] was used to search for cancer research journal articles in PubMed (MEDLINE), EBSCOhost (MEDLINE, CINAHL), and Web of Science (WoS), with assistance from a medical information specialist (KK). Briefly, the search terms were “cancer” AND “Botswana”. Synonyms of the term “cancer” were identified using the medical subject headings (MeSH) term “cancer” and were separated by the Boolean operator OR. Following the Boolean operator AND, the two largest cities in Botswana were included as follows: OR “Gaborone” OR “Francistown”. To include research from Africa published in African journals that are sometimes not indexed in international databases, a simple search was conducted on African Journals Online (AJO) and African Index Medicus (AIM) [24,25]. The search results were filtered using country (Botswana) and the time period within which Botswana experienced an increase in cancer research outputs (January 2009–June 2021) (Supplementary Fig. 1). The search strategy and history are shown in Supplementary Table S1.
2.2. Screening and selection
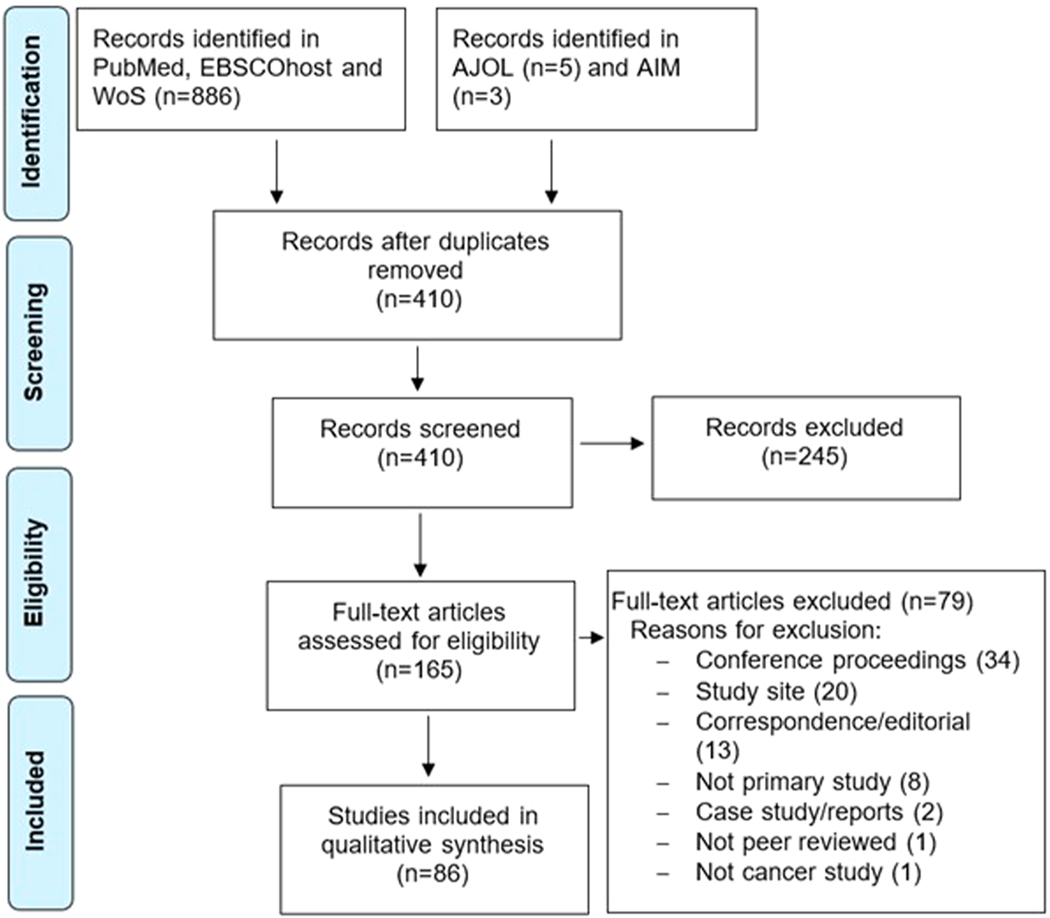
Results were imported from the databases into Mendeley Desktop reference management software (version 19), where they were organized into folders by source. The eligibility and relevance criteria were full-text, peer-reviewed, original journal articles published between January 2009 and June 2021, describing cancer research conducted in Botswana or on Botswana population. Studies involving the use of models such as cell lines, laboratory animals, bioinformatics, or mathematical models were also included if one or both of the first or last authors had a Botswana affiliation. During the import, exact duplicates across databases were automatically deleted. Article titles and abstracts were screened for eligibility and relevance using the selection criteria. Reviews, commentaries, editorials, case reports, conference abstracts, and letters to the editor that did not involve collection of primary data were excluded. A summary of the selection process is shown in Fig. 1.
Fig. 1.
Screening and selection of cancer research studies in Botswana.
2.3. Classification of cancer research outputs
Cancer research outputs were classified by cancer type and research domain, following a modified common scientific outline (CSO) classification of the international cancer research partnership (ICRP) version 2, as described previously [23]. Common scientific outline is a common language used by ICRP partners for evaluating their cancer research portfolios. In the current review, cancer research outputs were classified into six domains according to the main scientific interest as follows: Biology (CSO 1); Etiology (CSO 2); Prevention (CSO 3); Early Detection, Diagnosis, and Prognosis (CSO 4); Treatment (CSO 5); Cancer Control, Survivorship, and Outcomes (CSO 6). The types of cancer classified according to ICRP categories are also mapped to ICD-10 codes [23,26]. Studies that were not specific to one cancer type were classified as “Non-Site-Specific” [26].
2.4. Data extraction
Data from eligible studies were extracted using a structured data extraction form. Data points included bibliographic information (first author’s surname, title, year of publication, journal), research domains (CSO 1 to CSO 6), type of cancer (ICRP or equivalent ICD-10 code), authorship (number of authors, number of authors affiliated to Botswana, affiliation of first author and last author), funding information (number of grants, funding organizations) and main findings. A minimum of 2 authors independently completed the data extraction form for each study and thereafter met to assess consistency and completeness. Any differences were resolved through consensus by all authors.
2.5. Data analysis and interpretation
Frequencies and percentages were used for descriptive analyses and summarized using graphs and tables. The number of articles was summarized by year of publication, cancer type, and research domain, as well as by research domain within each cancer type. Change in the focus of research was shown by the number of studies in each domain over 3-year time periods between 2009 and 2020. The alignment of cancer research to disease burden was determined as previously described [27]. Briefly, incidence data were obtained from the Botswana National Cancer Registry (BNCR) from 2009 to 2018 [28]. Cancers arising from lip, tongue, mouth, salivary glands, tonsil, oropharynx, nasopharynx, hypopharynx, and larynx were grouped as head and neck cancer (HNC), trachea and bronchi as lung cancer, and colon and rectum as colorectal cancer. From the number of eligible articles (n = 86), the percentage of each type of cancer was used to calculate its expected number of articles. Finally, the difference between observed and expected numbers of articles for each cancer type was plotted on a graph. To analyze collaborative networks, a subset of 70 articles indexed in Web of Science was used to construct and visualize bibliometric networks among countries and organizations, based on co-authorship, using VOSviewer software version 1.6.17 [29].
3. Results
3.1. Search results
The database searches yielded 894 records, including 308 studies from PubMed, 398 from EBSCOhost, 180 from Web of Science, and 8 from African databases (AJOL and AIM). After duplicate records were removed, titles and abstracts of 410 unique articles were screened for eligibility and 245 were excluded. Consequently, 165 articles were subjected to full-text review, after which 79 were excluded. The excluded records comprised 34 conference proceedings, 20 with incorrect study sites, 13 correspondences/editorials, eight secondary studies, two case reports, one non-peer reviewed article, and one irrelevant to cancer. The final review included 86 papers. Fig. 1 depicts the flow chart for selecting studies.
3.2. Publication trends
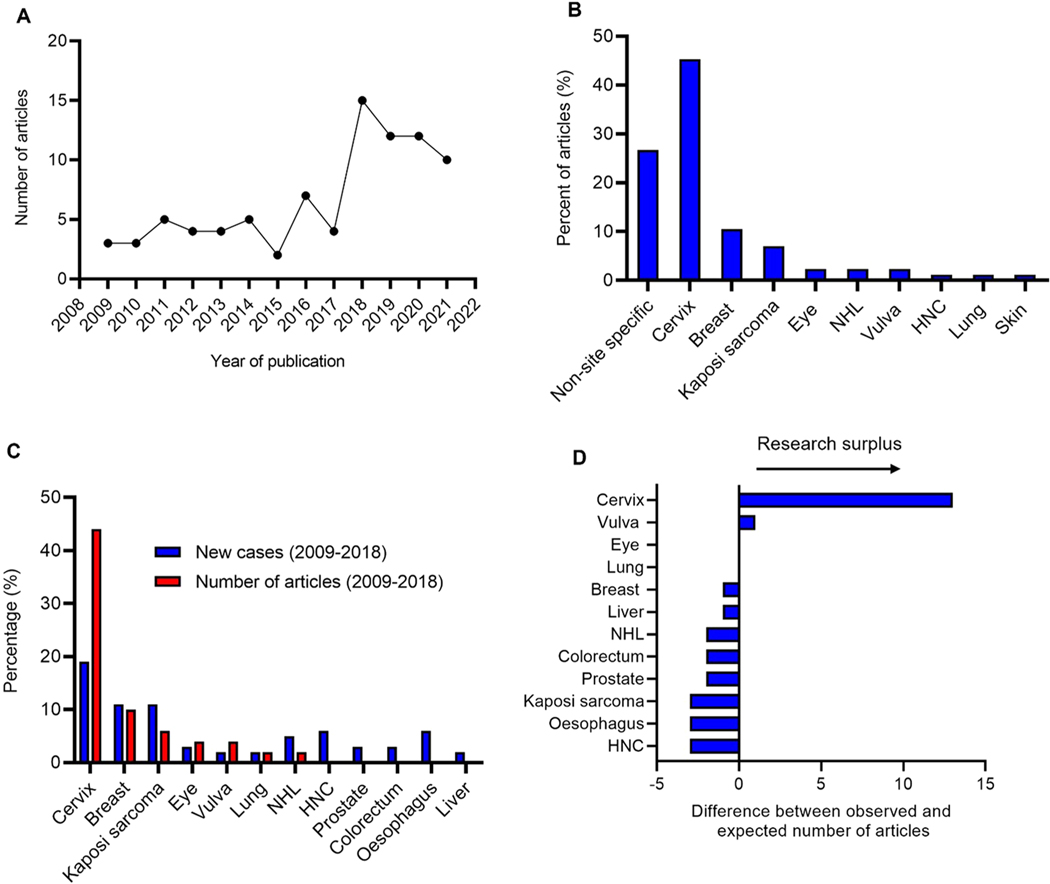
Between 2009 and 2017 the number of primary cancer research outputs in Botswana was generally low, averaging 4 papers per year, with the lowest number (n = 2) in 2015 and the highest (n = 7) in 2016 (Fig. 2A). Between 2018 and 2021 there was a substantial increase in the number of articles, with an average of 12 articles each year in this period. The highest number of articles (n = 14) was published in 2018. Of all the articles included in the analysis, 27 % were not specific to a particular type of cancer (non-site-specific) (Fig. 2B). The most common site-specific articles were on cervical cancer (45 %), breast cancer (10 %), and Kaposi sarcoma (7 %). Eye cancer, NHL and vulva cancer each accounted for 2 % of the cancer research outputs. Head and neck cancer, lung, and skin cancer (other than melanoma) were the least- researched cancers with 1 article (1 %) each.
Fig. 2.
Trend analysis of primary cancer research outputs in Botswana between 2009 and 2021. (A) The number of articles published every year from 2009 to 2021. (B) The percentage of articles published on each type of cancer. Studies that were not specific to one type of cancer were classified as non-site specific. (C) The percentage of new cases and research outputs by cancer type during the period 2009–2018. (D) Observed and expected research outputs for each type of cancer. Abbreviations: HNC-Head and neck cancer; NHL-Non-Hodgkin Lymphoma.
Incidence data from the BNCR were used to calculate the percentage of new cases for each cancer type, and those percentages were then compared with the total number of articles per cancer type. In comparison to its prevalence, the proportion of cervical cancer research outputs was high (Fig. 2C). Our estimate of the alignment of research outputs to the burden of each kind of cancer also showed that cervical cancer was the most commonly researched malignancy, followed by vulva cancer (Fig. 2D). In comparison, research outputs on the two other most common cancers, breast cancer and Kaposi sarcoma, were relatively low (Fig. 2C, D). Although HNC, prostate, esophageal, liver, and colorectal cancers were among the top 12 cancers in Botswana, no primary research output was observed in each of these cancers during the review period. Collectively, the data showed that cancer research outputs were not aligned to prevalence for most cancers, with cervical cancer being the most researched and HNC, esophageal cancer, and Kaposi sarcoma the least researched types.
3.3. Cancer research focus
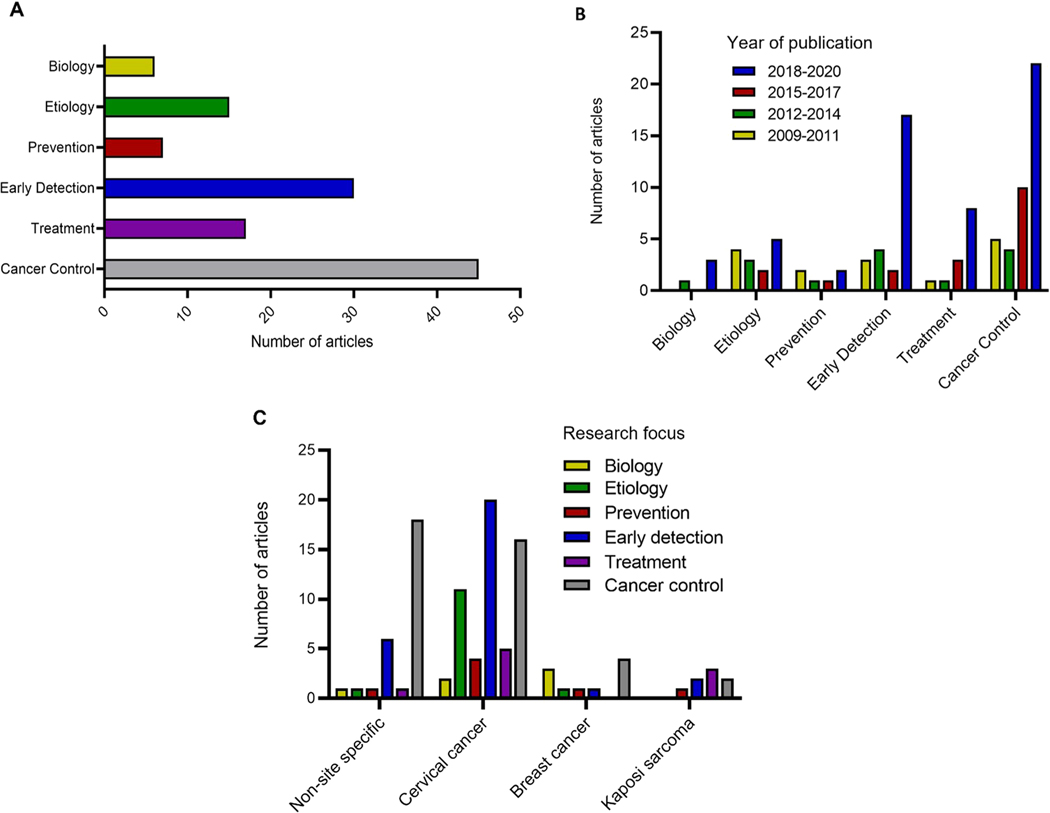
To determine the focus of cancer research in Botswana from 2009 to 2021, cancer research outputs were grouped by CSO classification. Since some outputs encompassed more than one research focus, the sum of articles by research focus exceeded the total number of articles included in the study. Overall, articles on cancer control, survivorship, and outcomes were the most prevalent (n = 45) (Fig. 3A). This was followed by research on early detection, diagnosis, and prognosis (n = 30); treatment (n = 17); and etiology (n = 15). Prevention and biology were the least researched areas (n = 7 and n = 6 articles, respectively). Changes in research focus over 3-year periods between 2009 and 2020 were then determined. Compared to the time period 2009–2011, all main areas of cancer research (except for prevention) registered an increase in research outputs during the 2018–2020 period (Fig. 3B). For research on cancer etiology, this increase was preceded by declines during the periods of 2012–2014 and 2015–2017. Research into treatment and cancer control, survivorship, and outcomes increased in the recent periods of 2015–2017 and 2018–2020.
Fig. 3.
Analysis of primary cancer research outputs by research focus in Botswana between 2009 and 2021. (A) The number of articles by cancer research focus. (B) Changes in cancer research focus between 2009 and 2020. (C) Frequencies of research focus in non-site-specific cancer and the three most-studied cancers.
Analysis of research focus by type of cancer showed that non-site- specific cancer research was dominated by research into cancer control, survivorship, and outcomes (n = 18), followed by early detection, diagnosis, and prognosis (n = 6) (Fig. 3C). Research on cervical cancer was mainly focused on early detection, diagnosis, and prognosis (n = 20) followed by cancer control, survivorship, and outcomes (n = 16). Cervical cancer also had the highest number of articles on etiology (n = 11), prevention (n = 4), and treatment (n = 5). The highest number of articles on biology (n = 3) and treatment (n = 3) were observed in breast cancer and Kaposi sarcoma, respectively. Interestingly, there were no articles about breast cancer treatment, or Kaposi sarcoma biology.
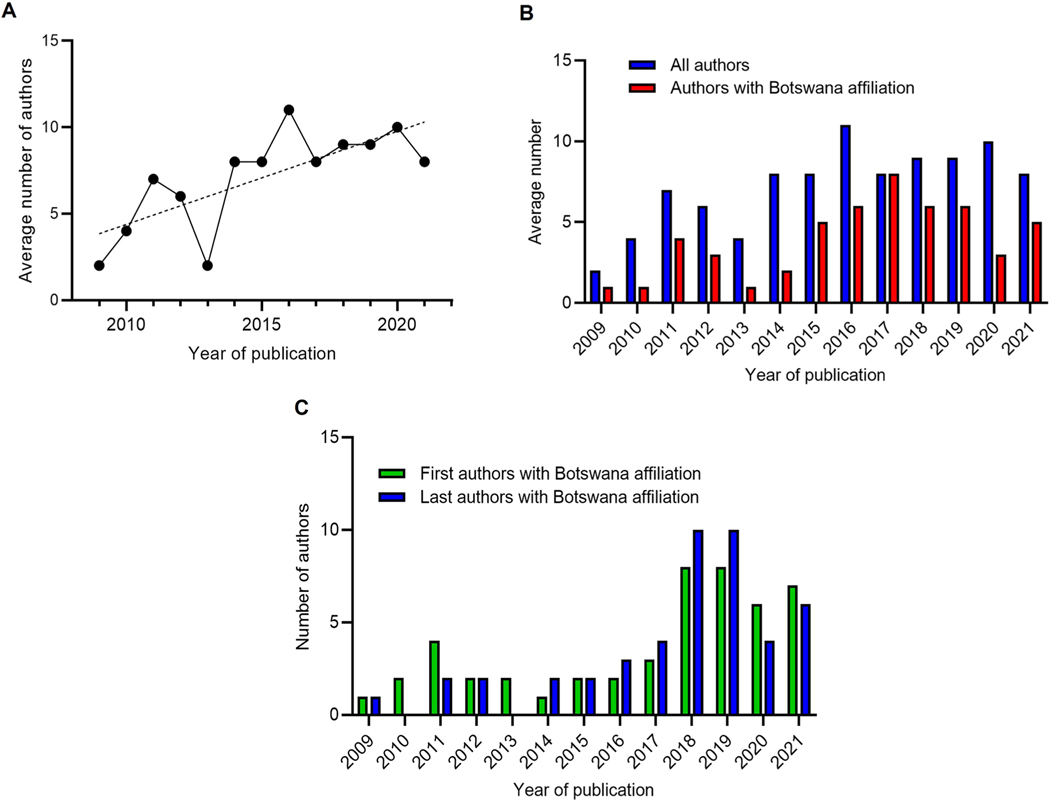
3.4. Authorship
The overall average number of authors per article during the study period was 8, and a trend analysis showed that the yearly average increased from two in 2009 to ten in 2020 (Fig. 4A). Cumulatively, the 86 cancer research outputs in this study were authored by a total of 700 authors. Of these, 370 (53 %) had any affiliation with an institution in Botswana, with an average of four Botswana-affiliated authors per output. Fig. 4B shows the average number of authors with Botswana affiliation during each year alongside the average number of all authors in that particular year. The yearly average number of authors with any Botswana affiliation was equal to or below four until 2014, which then rose above average until 2019, before declining to three in 2020 (Fig. 4B).
Fig. 4.
Authorship of primary cancer research outputs by research focus in Botswana between 2009 and 2021. (A) The average number of authors per article in each year. (B) The average number of authors with Botswana affiliation compared with authors with any affiliation. (C) The number of first and last authors with Botswana affiliation.
The proportion of cancer research outputs with lead authors (first or last) affiliated with any Botswana institutions was also analyzed. Three articles had two co-first authors, bringing the total of first authors to 89. Of these, 54 % were affiliated with a Botswana institution. Trend analysis showed that the number of lead authors with Botswana affiliation increased steadily from 2017, followed by a slight decline in 2020 (Fig. 4C). Overall, a total of 47 (53 %) last authors were affiliated with a Botswana institution. The top three affiliations of first authors were the University of Botswana (UB) (18 %), University of Pennsylvania (14 %), and Botswana-University of Pennsylvania Partnership (BUP) (10 %) (Supplementary Table S2). Similarly, three articles had two co-last authors, resulting in a total of 89 last authors. Most last authors were affiliated with University of Pennsylvania (16 %), UB (12 %), and BUP (11 %) (Supplementary Table S3).
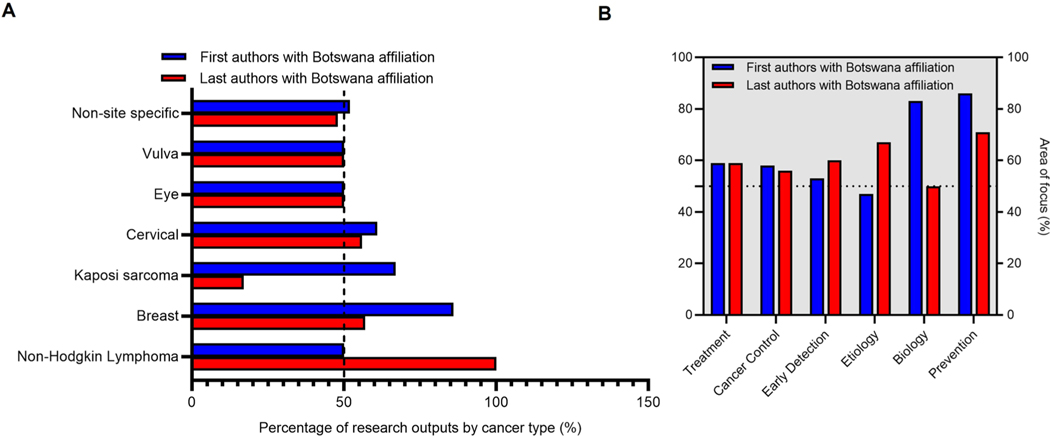
To further understand participation of local researchers, we analyzed the types of studies by local authors (Fig. 5A, B). For our analysis of local authorship by cancer type, we only considered the types of cancers reported in at least two articles. First authors with Botswana affiliations accounted for a higher proportion of articles on breast cancer (86 %), cervical cancer (61 %) and Kaposi sarcoma (67 %) (Fig. 5A). In contrast, last authors with Botswana affiliations accounted for a very low proportion of articles on Kaposi sarcoma (17 %). Considering authorship by area of focus, our results showed that authors with Botswana affiliation were more likely to be first and last authors in the majority of categories of research outputs, except cancer etiology (47 %) and biology (50 %) for first and last authors respectively (Fig. 5B). Most notably, Botswana- affiliated authors were first authors in over 80 % of cancer research outputs focusing on cancer prevention (86 %) and biology (83 %). Authors with Botswana affiliation were also last authors in 71 % of research outputs focusing on prevention.
Fig. 5.
Analysis of types of cancer studies by first and last authors with Botswana affiliation. (A) Percentage of first and last authors among cancer research outputs reporting different types of cancer. (B) Percentage of first and last authors’ affiliation among research outputs with different areas of focus.
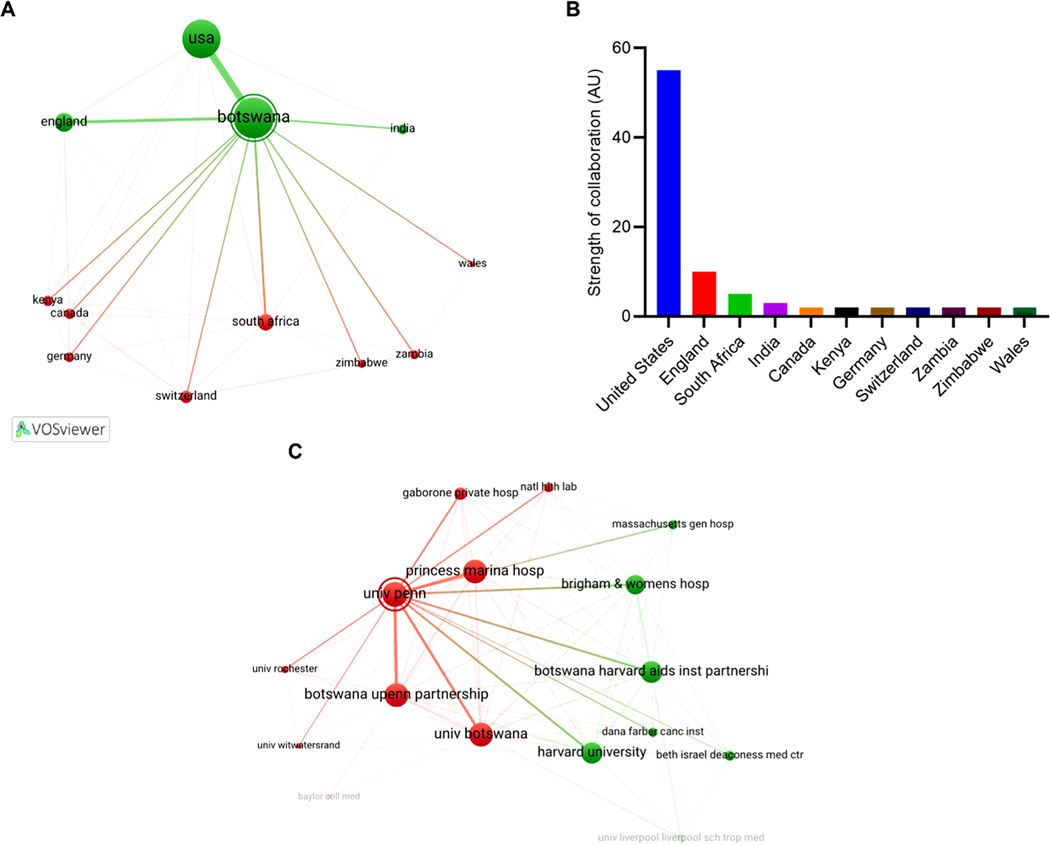
3.5. Collaboration networks
Analysis of inter-country collaborations using VOSviewer showed that Botswana collaborated most with the United States of America (USA) (link strength = 55), followed by the UK (link strength = 10), South Africa (link strength = 5), and India (link strength = 3) (Fig. 6A, B). Kenya, Zimbabwe, and Zambia were the only other African countries that collaborated with Botswana. We also evaluated the collaboration network of individual research institutions. A total of 16 institutions formed two clusters (Fig. 6C). University of Pennsylvania was the most influential institution, forming a cluster with 5 local institutions: BUP, UB, Princess Marina Hospital, Gaborone Private Hospital, and National Health Laboratory. In the second cluster, Botswana-Harvard AIDS Institute Partnership (BHP) was the most influential, forming strong links with Harvard University and Harvard Medical School affiliates.
Fig. 6.
Analysis of collaboration in cancer research in Botswana between 2009 and 2021. (A) Network visualization map of cancer research collaborations between Botswana and other countries. Countries that were affiliated with at least 2 articles were included in the analysis. The thickness of the line between any two countries is determined by the number of co-authorships; a thicker line represents more collaboration. (B) The strength of collaborations between Botswana and other countries based on the network visualization map. (C) Network visualization map of collaborating institutions publishing about cancer research in Botswana.
3.6. Funding of cancer research outputs in Botswana
To establish the funding sources for primary research on cancer in Botswana for the period 2009–2021, funding acknowledgments were evaluated from the 86 articles included in the review. A total of 23 articles (27 %) did not include any funding acknowledgment. Fifty-eight articles (67 %) had funding acknowledgments, and in five articles (6 %) the authors declared receiving no funding support. In some articles, multiple funding sources were acknowledged, so the number of funding institutions exceeded the number of articles. Therefore, the frequency of each funding source was determined. The National Institutes of Health (NIH) was the most acknowledged funding source (33 %), followed by the American Cancer Society, American Society for Clinical Oncology, UB, and the Wellcome Trust (5 % each) (Fig. 7A). Collectively, funding institutions from the USA accounted for the most funding support (n = 82, 76 %), followed by institutions in Botswana (n = 10, 9 %) and the UK (n = 8, 7 %) (Fig. 7B).
Fig. 7.
The most frequently acknowledged funding sources of cancer research in Botswana. (A) The most frequently acknowledged institutions. (B) Countries with the most frequently acknowledged funding institutions. Abbreviations: PEPFAR–The United States President’s Emergency Plan for AIDS Relief; NABSA–Network for Analytical and Bioassay Services in Africa; CRUK–Cancer Research UK; BUP-Botswana–University of Pennsylvania Partnership; AAD–American Academy of Dermatology; UPenn–University of Pennsylvania; ASCO–American Society for Clinical Oncology.
4. Discussion
The current study describes, for the first time in Botswana, trends and patterns of cancer research outputs including authorship, collaboration, and funding sources, as well as their alignment to local disease burden. Previous research has shown that Botswana is among the SSA countries with the lowest cancer research output [30]. However, the current study demonstrates that the number of cancer research outputs has consistently increased in Botswana from 2009 to 2021. Although causes for the increase are unclear, it is thought to be due to a combination of increasing cancer incidence and growing collaborations with international partners from high-income countries (HIC). The existing collaborative partnerships are mostly between American medical academic institutions and Botswana’s MoH and UB, including the BUP, BHP, Botswana-Baylor Children’s Clinical Centre of Excellence [8,31] and, more recently, the Botswana-Rutgers Partnership [32]. The cancer research outputs are therefore expected to continue to increase.
Evaluating cancer research outputs by type of cancer showed that cervical cancer was the most frequently investigated, followed by breast cancer and Kaposi sarcoma. A similar trend, where HIV-related malignancies such as cervical cancer and Kaposi sarcoma dominate cancer research outputs, was reported in Zambia and this trend is likely driven in part by investment in HIV research and the associated infrastructure [30]. Data available from the BNCR for part of the review period (2009–2018) showed that cervical cancer was the most commonly diagnosed cancer in Botswana (n = 2503, 18.9 %), followed by Kaposi sarcoma (n = 1493, 11.3 %) and breast cancer (n = 1464, 11.1 %) [28]. Interestingly, the present analysis revealed a mismatch between incidence and research output for a given cancer type. Among the top three cancers by incidence, cervical cancer was most studied, while Kaposi sarcoma and breast cancer received less attention. It is thought that research outputs for cervical cancer may be driven in part by the research infrastructure established for HIV/AIDS programs in Botswana [8,22]. However, if this is the case, the same effect has not been extended to other HIV-related malignancies such as Kaposi Sarcoma and non-Hodgkin lymphoma. Cervical cancer research may have also been driven by the availability of screening data and archived specimens from Botswana’s National Cervical Cancer Prevention Programme (NCCP). The extent to which the scientific focus of funding opportunities contributed to the observed results was not investigated. Collectively, the disparities uncovered here provide a foundation to guide future cancer research agendas in Botswana.
Another critical finding of the present review was that cancer control, survivorship and outcomes research was the most common cancer research area in Botswana, followed by early detection, diagnosis and prognosis. 700,791 The two areas of cancer research were also reported to be most common in Kenya and National Institute of Cancer- designated cancer centers for SSA [33,34]. Although early detection and cancer control are important priorities, there is need to increase the scope of research in SSA, to prioritize prevention and treatment [34]. Increasing evidence suggests that cancer biology and etiologies may vary by race or geography [35] and as such, studies of the biology and etiologies of cancers that are unique to SSA populations could lead to improved prevention and treatment strategies globally [35,36].
Cancer treatment is costly, and in Botswana it is hampered by a dearth of cancer specialists, shortage of chemotherapy drugs, and inadequate radiation facilities [37–39]. For existing prevention and treatment modalities to benefit SSA countries, research is needed to develop implementation stratergies that are specific to SSA health systems. Clinical trials to optimize treatment methods in SSA are constrained by inadequate infrastructure, clinical and regulatory considerations, and this is reflected by a small number of interventional studies in SSA [34]. It is therefore not surprising that a small number of studies on cancer treatment in Botswana is reported in this review. Nonetheless, the existing focus on early detection and cancer control, mainly observed in cervical cancer research, may result in the development of innovative methods for early diagnosis and control stratergies that are tailored for a resource-constrained health care settings.
Overall, 54 % of co-authors (any authorship position) and 53 % of lead authors (first or last) were from Botswana institutions. A comparative bibliometric analysis of all countries in Africa reported that Botswana cancer researchers occupied approximately 38 % and 40 % of first and last author positions respectively [40]. Our study only included primary cancer studies and we applied strict exclusion criteria. A similar study in Zambia reported that only 33 % of cancer research outputs had a first or last author from Zambia [30]. Despite variations reported in these studies, the proportions reflect underrepresentation of African authors in cancer research outputs, including Botswana-affiliated authors. Another study evaluating cancer genomics research in Africa reported that less than half of lead authors were affiliated with an African country [41]. This underrepresentation of African authors in health research has often been attributed to lack of human research capacity [41]. SSA is home to 14 % of the world population but contributes only 0.7 % of the world’s researchers [42]. Therefore, development of local human research capacity should be a priority in Africa. The MoH in Botswana partly addresses this need by planning to build research capacity, and progress will be measured by an increase in the number of Botswana-led NCD-related publications [9]. The present review provides baseline data upon which to measure progress toward strengthening local capacity for cancer research in Botswana.
Authors with Botswana affiliation held key authorship positions (first and last) in studies of cancer prevention and of breast cancer, Kaposi sarcoma and non-Hodgkin lymphoma. Prioritization of research on cancer prevention by local researchers is important for our understanding of potentially modifiable risk factors for major types of cancers in SSA such as obesity (breast cancer), HPV (cervical cancer), HHV-8 (Kaposi sarcoma) and Epstein Barr Virus (non-Hodgkin lymphoma) [5,34,43,44]. The results also suggest that local cancer researchers recognize the need for a data-driven approach to set local research priorities based on local cancer rates [34]. This might address the mismatch between incidence rates and research outputs for certain cancers reported in this review. However, the small proportion of last authors with Botswana affiliation in articles on Kaposi sarcoma may further drive the mismatch for Kaposi sarcoma.
Our results on funding are similar to those reported by Vargas et al. [45], showing that cancer research studies in Kenya relied heavily on international funding, most notably from the USA, with little local funding or from other African countries. Our co-authorship network analysis showed strong collaboration with the USA, while collaboration with other African countries was limited. A similar relationship has previously been reported between Kenya and USA [45]. However, unlike in Botswana, Kenyan institutions were more influential than USA-based institutions, with stronger local collaborative networks. Heavy reliance on collaboration with Western countries has previously been suggested as a potential driver of underrepresentation of Africa authors, especially in first and last author positions [40]. Scarcity of local funding hampers development of South-South collaborations within Africa and further limits African researchers in assuming leadership roles in research projects [46]. However, partnerships between HIC and low- and middle-income countries (LMIC) are important for building human research capacity and research infrastructure [47], especially for the LMIC partner, whilst answering critical research questions that would not be adequately addressed in HIC settings. One such partnership is the Botswana-UPenn Research Consortium of HPV-Related Cervical Cancer in HIV Patients, a multi-disciplinary consortium between University of Pennsylvania and UB (2014–2022) [48, 49]. The consortium had a strong focus on increasing local research capacity through physical infrastructure and research training. Data from the NIH RePORTER showed that the consortium was linked to approximately 20 % of the articles included in this review [49] (data not shown). While this shows strong collaborative efforts with international partners, the scarcity of local funding (< 10 %) reveals a need for stronger local funding support from the Botswana government, charitable organizations, and industry.
We present the first review of cancer research outputs in Botswana; however, the findings should be understood in the context of their limitations. Incidence data supplied by the BNCR were only available through to 2018, so those findings could not be generalized to the entire review period (2009–2021). In addition, BNCR data may underrepresent the incidence of cancers arising from anatomical sites that are difficult to obtain biopsies from, such as liver, brain, and lung [12], due to a shortage of local specialists and specialized facilities. For the authorship analyses, authors with multiple affiliations were not investigated to determine a primary affiliation; therefore, the present findings may not reliably reflect the involvement of Botswana citizens. While we acknowledge that mentorship is critical for cancer research that is relevant for the local context of researchers [50], the design of our study did not allow investigation of whether lack of research mentorship maybe a factor in the observed poor research in local priorities. For the analysis of funding sources, it should be noted that acknowledgment of funding support is optional in some journals. Finally, due to the descriptive nature of the present review it is not possible to identify any underlying causes of the observations made.
Despite the limitations acknowledged above, we report that cancer research is increasing in Botswana, with strong support from the USA, and with a focus on cervical cancer and secondary and tertiary cancer prevention. The present findings also reflect poor local funding for cancer research in Botswana, as well as underrepresentation of Botswana-affiliated authors in cancer research outputs. Therefore, there is a need for a national strategic plan to strengthen local funding for cancer research, increase human research capacity, and align the research agenda with local needs.
Supplementary Material
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supporting information
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.jcpo.2023.100405.
References
- [1].World Health Organization, Cancer [Internet], Factsheets, 2022. 〈https://www.who.int/news-room/fact-sheets/detail/cancer〉. (Accessed 18 April 2022).
- [2].Glynn RW, Chin JZ, Kerin MJ, Sweeney KJ, Representation of cancer in the medical literature – a bibliometric analysis, PLoS One 5 (11) (2010), e13902, 10.1371/journal.pone.0013902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F, Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries, CA Cancer J. Clin 71 (3) (2021) 209–249, 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- [4].Plummer M, de Martel C, Vignat J, Ferlay J, Bray F, Franceschi S, Global burden of cancers attributable to infections in 2012: a synthetic analysis, Lancet Glob. Health 4 (9) (2016) e609–e616. 〈https://linkinghub.elsevier.com/retrieve/pii/S2214109X16301437〉. [DOI] [PubMed] [Google Scholar]
- [5].de Martel C, Georges D, Bray F, Ferlay J, Clifford GM, Global burden of cancer attributable to infections in 2018: a worldwide incidence analysis, Lancet Glob. Health 8 (2) (2020) e180–e190, 10.1016/S2214-109X(19)30488-7. [DOI] [PubMed] [Google Scholar]
- [6].World Bank, Country Classification [Internet], World Bank Country and Lending Groups, 2022. 〈https://datahelpdesk.worldbank.org/knowledgebase/articles/906519〉. (Accessed 19 May 2022). [Google Scholar]
- [7].Chabner BA, Efstathiou J, Dryden-Peterson S, Cancer in Botswana: the second wave of AIDS in Sub-Saharan Africa, Oncologist 18 (7) (2013) 777–778 ([accessed]), 〈https://academic.oup.com/oncolo/article/18/7/777/6398854〉. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Efstathiou JA, Bvochora-Nsingo M, Gierga DP, Alphonse Kayembe MK, Mmalane M, Russell AH, Paly JJ, Brown C, Musimar Z, Abramson JS, Bruce KA, Karumekayi T, Clayman R, et al. , Addressing the growing cancer burden in the wake of the AIDS epidemic in Botswana: the BOTSOGO collaborative partnership, Int J. Radiat. Oncol 89 (3) (2014) 468–475. 〈https://linkinghub.elsevier.com/retrieve/pii/S0360301614003903〉. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Ministry of Health and Wellness Botswana, Botswana National Multisectoral Strategy for the Prevention and Control of Non-Communicable Diseases 2018. –2023, 2018. [Google Scholar]
- [10].UNAIDS, Botswana Country factsheets 2020, 〈https://www.unaids.org/en/regionscountries/countries/botswana〉, (Accessed 19 December 2023).
- [11].Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F, Global Cancer Observatory: Cancer Today, International Agency for Research on Cancer, Lyon, France. 〈https://gco.iarc.fr/today〉. (Accessed 21 February 2021). [Google Scholar]
- [12].Dryden-Peterson S, Medhin H, Kebabonye-Pusoentsi M, Seage GR, Suneja G, Kayembe MKA, Mmalane M, Rebbeck T, Rider JR, Essex M, Lockman S, Cancer incidence following expansion of HIV treatment in Botswana, PLoS One 10 (8) (2015), e0135602, 10.1371/journal.pone.0135602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Suneja G, Dryden-Peterson S, Boyer M, Musimar Z, Nsingo-Bvochora M, Ramogola-Masire D, Medhin H, Bekelman J, Lockman S, Rebbeck T, Cancer in Botswana: a prospective cohort study of cancer type, treatment, and outcomes, Int. J. Radiat. Oncol 87 (2) (2013) S492–S493. 〈https://linkinghub.elsevier.com/retrieve/pii/S036030161301972X〉. [Google Scholar]
- [14].Sadigh KS, Hodgeman RM, Tapela N, Nkele I, Bvochora-Nsingo M, Chiyapo S, Ralefala TB, Efstathiou JA, John O, Motswetla G, Grover S, Younger J, Mmalane MO, et al. , HIV is associated with decreased breast cancer survival: a prospective cohort study, in: Proceedings of the Conference on Retroviruses and Opportunistic Infections, Seattle, 2019. [Google Scholar]
- [15].Dryden-Peterson S, Bvochora-Nsingo M, Suneja G, Efstathiou JA, Grover S, Chiyapo S, Ramogola-Masire D, Kebabonye-Pusoentsi M, Clayman R, Mapes AC, Tapela N, Asmelash A, Medhin H, et al. , HIV infection and survival among women with cervical cancer, J. Clin. Oncol 34 (31) (2016) 3749–3757, https://ascopubs.org/doi/10.1200/JCO.2016.67.9613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Bhatia RK, Rayne S, Rate W, Bakwenabatsile L, Monare B, Anakwenze C, Dhillon P, Narasimhamurthy M, Dryden-Peterson S, Grover S, Patient factors associated with delays in obtaining cancer care in Botswana, J. Glob. Oncol 4 (4) (2018) 1–13, 10.1200/JGO.18.00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Anakwenze C, Bhatia R, Rate W, Bakwenabatsile L, Ngoni K, Rayne S, Dhillon P, Narasimhamurthy M, Ho-Foster A, Ramogola-Masire D, Grover S, Factors related to advanced stage of cancer presentation in Botswana, J. Glob. Oncol 4 (2018) 1–9, 10.1200/JGO.18.00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Ministry of Health and Wellness Botswana, National Cervical Cancer Prevention: Five Year Comprehensive Prevention and Control Strategy (2017–2021), 2018. [Google Scholar]
- [19].Aggarwal A, Lewison G, Rodin D, Zietman A, Sullivan R, Lievens Y, Radiation therapy research: a global analysis 2001–2015, Int. J. Radiat. Oncol 101 (4) (2018) 767–778. 〈https://linkinghub.elsevier.com/retrieve/pii/S0360301618305340〉. [DOI] [PubMed] [Google Scholar]
- [20].Livingston J, Cancer in the shadow of the AIDS epidemic in Southern Africa, Oncologist 18 (7) (2013) 783–786. 〈https://academic.oup.com/oncolo/article/18/7/783/6398848〉. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].National Library of Medicine, PubMed, 2021. 〈https://pubmed.ncbi.nlm.nih.gov/〉, (Accessed 17 June 2021).
- [22].Suneja G, Ramogola-Masire D, Medhin HG, Dryden-Peterson S, Bekelman JE, Cancer in Botswana: resources and opportunities, Lancet Oncol. 14 (8) (2013) e290–e291. 〈https://linkinghub.elsevier.com/retrieve/pii/S1470204513702833〉. [DOI] [PubMed] [Google Scholar]
- [23].Moodley J, Singh V, Kagina BM, Abdullahi L, Hussey GD, A bibliometric analysis of cancer research in South Africa: study protocol, BMJ Open 5 (2) (2015), 10.1136/bmjopen-2014-006913 (e006913–e006913). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Atani M, Kabore M, African index medicus: improving access to African health information, S. Afr. Fam. Pract 49 (2) (2007) 5–7, 10.1080/20786204.2007.10873506. [DOI] [Google Scholar]
- [25].Smart P, African journals online (AJOL), Ser. Rev 31 (4) (2005) 261–265. 〈https://www.sciencedirect.com/science/article/pii/S0098791305001243〉. [Google Scholar]
- [26].International Cancer Research Partnership, Coding Guidelines, ICRP Coding Guidelines, 2018. 〈https://www.icrpartnership.org/cso〉. (Accessed 12 August 2020). [Google Scholar]
- [27].Albarqouni L, Elessi K, Abu-Rmeileh NME, A comparison between health research output and burden of disease in Arab countries: evidence from Palestine, Health Res. Policy Syst 16 (2018) 25, 10.1186/s12961-018-0302-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ministry of Health and Wellness Botswana, National Cancer Registry, Botswana: (2009–2018), 2021. [Google Scholar]
- [29].van Eck NJ, Waltman L, Software survey: VOSviewer, a computer program for bibliometric mapping (version 1.6.17), Scientometrics 84 (2) (2010) 523–538, 10.1007/s11192-009-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Kayamba V, Mutale W, Cassell H, Heimburger DC, Shu X-O, Systematic review of cancer research output from Africa, with Zambia as an example, JCO Glob. Oncol 7 (2021) 802–80810, 10.1200/GO.21.00079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Slone JS, Slone AK, Wally O, Semetsa P, Raletshegwana M, Alisanski S, Force LM, Chinyundo K, Margolin J, Agrawal AK, Anderson AR, Scheurer ME, Mehta PS, Establishing a pediatric hematology-oncology program in Botswana, J. Glob. Oncol 4 (2018) 1–9, 10.1200/JGO.17.00095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Rutgers Global Health Institute, RUTGERS GLOBAL HEALTH INSTITUTE 2020–2021, Impact report [Internet]. Impact Report, 2021. 〈https://energypedia.info/wiki/EnDev_Report_on_Impacts〉. [Google Scholar]
- [33].Manduku V, Akhavan M, Asiki G, Brand NR, Cira MK, Gura Z, Kadengye DT, Karagu A, Livinski AA, Meme H, Kyobutungi C, Moving towards an evidence-informed cancer control strategy: a scoping review of oncology research in Kenya, J. Cancer Policy 24 (2020), 100219. 〈https://linkinghub.elsevier.com/retrieve/pii/S2213538320300114〉. [Google Scholar]
- [34].Ngwa W, Addai BW, Adewole I, Ainsworth V, Alaro J, Alatise OI, Ali Z, Anderson BO, Anorlu R, Avery S, Barango P, Bih N, Booth CM, et al. , Cancer in sub-Saharan Africa: a lancet oncology commission, Lancet Oncol. 23 (6) (2022) e251–e312, 10.1016/S1470-2045(21)00720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Rebbeck TR, Cancer in sub-Saharan Africa, Science 367 (6473) (2020) 27–28, 10.1126/science.aay4743. [DOI] [PubMed] [Google Scholar]
- [36].Morhason-Bello IO, Odedina F, Rebbeck TR, Harford J, Dangou J-M, Denny L, Adewole IF, Challenges and opportunities in cancer control in Africa: a perspective from the African Organisation for Research and Training in Cancer, Lancet Oncol. 14 (4) (2013) e142–e151, 10.1016/S1470-2045(12)70482-5. [DOI] [PubMed] [Google Scholar]
- [37].Martei YM, Grover S, Bilker WB, Monare B, Setlhako DI, Ralefala TB, Manshimba P, Gross R, Shulman LN, DeMichele A, Impact of essential medicine stock outs on cancer therapy delivery in a resource-limited setting, J. Glob. Oncol 5 (5) (2019) 1–11, 10.1200/JGO.18.00230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Martei YM, Chiyapo S, Grover S, Ramogola-Masire D, Dryden-Peterson S, Shulman LN, Tapela N, Availability of WHO essential medicines for cancer treatment in Botswana, J. Glob. Oncol 4 (2018) 1–8, 10.1200/JGO.17.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Efstathiou JA, Heunis M, Karumekayi T, Makufa R, Bvochora-Nsingo M, Gierga DP, Suneja G, Grover S, Kasese J, Mmalane M, Moffat H, von Paleske A, Makhema J, et al. , Establishing and delivering quality radiation therapy in resource-constrained settings: the story of Botswana, J. Clin. Oncol 34 (1) (2015) 27–35, 10.1200/JCO.2015.62.8412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Mutebi M, Lewison G, Aggarwal A, Alatise OI, Booth C, Cira M, Grover S, Ginsburg O, Gralow J, Gueye S, Kithaka B, Kingham TP, Kochbati L, et al. , Cancer research across Africa: a comparative bibliometric analysis, BMJ Glob. Health 11 (2022), e009849. 〈http://gh.bmj.com/content/7/11/e009849.abstract〉. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Rotimi SO, Rotimi OA, Salhia B, Authorship patterns in cancer genomics publications across Africa, JCO Glob. Oncol 7 (2021) 747–755, 10.1200/GO.20.00552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].UNESCO, UNESCO Science Report: The Race Against Time for Smarter Development, Paris, 2021. [Google Scholar]
- [43].Vento S, Cancer control in Africa: which priorities? Lancet Oncol. 14 (4) (2013) 277–279, 10.1016/S1470-2045(13)70022-6. [DOI] [PubMed] [Google Scholar]
- [44].Yarchoan R, Uldrick TS, HIV-associated cancers and related diseases, N. Engl. J. Med 378 (11) (2018) 1029–1041, 10.1056/NEJMra1615896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Vargas JS, Livinski AA, Karagu A, Cira MK, Maina M, Lu Y-L, Joseph AO, A bibliometric analysis of cancer research funders and collaborators in Kenya: 2007–2017, J. Cancer Policy 33 (2022), 100331. 〈https://www.sciencedirect.com/science/article/pii/S2213538322000108〉. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Adewole I, Martin DN, Williams MJ, Adebamowo C, Bhatia K, Berling C, Casper C, Elshamy K, Elzawawy A, Lawlor RT, Legood R, Mbulaiteye SM, Odedina FT, et al. , Building capacity for sustainable research programmes for cancer in Africa, Nat. Rev. Clin. Oncol 11 (5) (2014) 251–259, 10.1038/nrclinonc.2014.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Abudu RM, Cira MK, Pyle DHM, Duncan K, Landscape of global oncology research and training at national cancer institute–designated cancer centers: results of the 2018–2019 global oncology survey, J. Glob. Oncol 5 (2019) 1–8, 10.1200/JGO.19.00308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Grover S, Zetola N, Ramogola-Masire D, Bvochora-Nsingo M, Schnader AF, Mick R, Gabaitiri L, Matlhagela K, Shen H, Chiyapo S, Balang D, Phaladze N, Nkomazana O, et al. , Building research capacity through programme development and research implementation in resource-limited settings – the Ipabalele study protocol: observational cohort studies determining the effect of HIV on the natural history of cervical cancer in Botswana, BMJ Open 9 (12) (2019), e031103, 10.1136/bmjopen-2019-031103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].National Institutes of Health, RePORT 〉 RePORTER [Internet], Report, 2022. 〈https://reporter.nih.gov/〉. (Accessed 17 March 2022).
- [50].Rubagumya F, Nyagabona SK, Msami KH, Manirakiza A, Longombe AN, Maniragaba T, Chan H, Paciorek A, Zhang L, Balandya E, Germana LH, Mmbaga EJ, Dharsee N, et al. , Attitudes and barriers to research among oncology trainees in East Africa, Oncologist 24 (9) (2019) e864–e869, 10.1634/theoncologist.2018-0805. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.