Abstract
Background
Because adrenal glands are enveloped by Gerota's fascia, spontaneous hemostasis is achieved in most cases of traumatic adrenal injury. For this reason, adrenal injuries are often treated conservatively and rarely present a clinical problem.
Case presentation
An 85-year-old man. He presented with right adrenal injury due to blunt trauma, fracture of the right transverse process of the 1st-4th lumbar vertebra, and fracture of the right 12th rib. A small amount of hematoma was observed around the adrenal gland, but his vital signs were stable and he was treated conservatively. However, on the 20th day of hospitalization, he developed sudden onset right-sided abdominal pain, hypotension, and restlessness. Contrast-enhanced CT scan revealed hemorrhagic shock due to delayed adrenal rupture, and emergency transcatheter arterial embolization was performed. A pseudoaneurysm formed at the time of injury was considered to have ruptured late.
Conclusion
Delayed rupture after adrenal injury has never been reported in the past, and is a very rare occurrence. Prompt diagnosis and hemostatic treatment are necessary.
Keywords: Adrenal grand injury, Transcatheter arterial embolization, Delayed rupture, Pseudoaneurysm
Background
Adrenal injuries are rare, occurring in 0.15–2 % of blunt trauma patients [1], [2]. It is often accompanied by injury to other organs in the abdominal cavity [2]. Although hemostasis is sometimes required, in most cases of adrenal injury alone, hemostasis can be achieved only by observation. On the other hand, a case of delayed rupture after adrenal injury has not been reported in the past, and is therefore reported here as a rare case.
Case presentation
An 85-year-old man with aortic stenosis and hypertension was hit by a car from his right side and transported to our hospital. He was not taking any anticoagulants.
A plain CT scan on arrival at the hospital revealed a traumatic subarachnoid hemorrhage and a right acute epidural hematoma. A 6 mm thick hematoma formation was observed in the right temporal region without midline shift. The abdominal CT showed a small amount of hematoma around the duodenum and right adrenal gland (Fig. 1), and a diagnosis of right adrenal injury (AAST injury scale Grade 2) was made. In addition, fractures of the right transverse process of the 1st-4th lumbar vertebrae and the right 12th rib were observed. Since the peri-adrenal hematoma was small and vital signs were stable, the patient was treated conservatively. On the 20th day of hospitalization, the patient suddenly developed very strong spontaneous pain from the right side of the abdomen to the back. He became agitated and went into shock with a heart rate of 110 beats/min and blood pressure of 90/72 mmHg. Contrast-enhanced CT scan of the abdomen showed extravasation of contrast medium in the right adrenal parenchyma (Fig. 2). The patient was diagnosed with delayed right adrenal rupture 20 days after injury, and emergency transcatheter arterial embolization was performed.
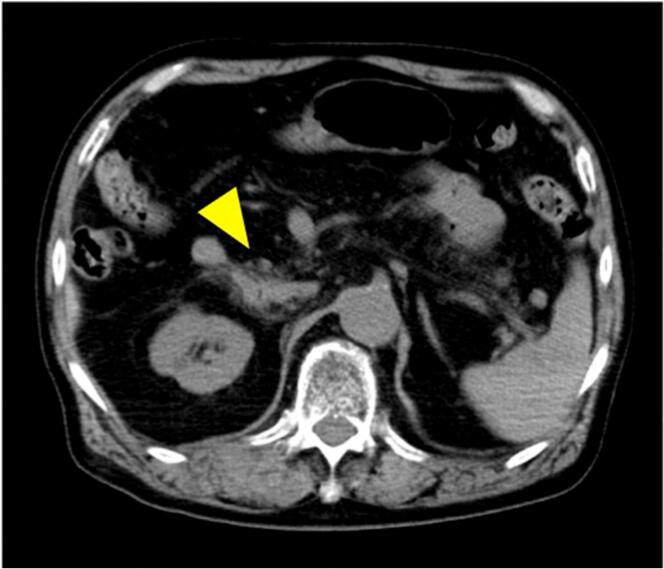
Fig. 1.
Abdominal CT on admission.
A dirty-fat area was found in the descending portion of the duodenum and right adrenal gland (arrow head).
Fig. 2.
Contrast-enhanced CT on day 20 of hospitalization.
Extravasation from right adrenal gland (arrow head).
An extravasation of contrast medium from the right middle adrenal artery was observed, and hemostasis was performed with a gelatin sponge and microcoil (Fig. 3). Blood samples showed ACTH 38.2 pg/ml and cortisol 39.2 μg/dl, with no evidence of adrenal insufficiency. The patient's postoperative course was stable and he was transferred to the hospital on day 29 of admission.
Fig. 3.

Radiological findings.
a) Angiogram of a right middle adrenal artery with extravasation.
b) Angiogram after arterial embolization with a microcoil.
Discussion
Because adrenal glands are deep trunk organs, single injury is extremely rare [1], [3], and most cases are complicated by injury to other parts of the body [4], and hemostatic treatment may be performed together with liver injury or right kidney injury [2], [3].
Possible mechanisms of adrenal injury include direct compression of the liver, kidneys, or vertebrae, shearing forces, or associated with increased pressure in the adrenal veins due to compression of the inferior vena cava [5].
Because adrenal glands are surrounded by Gerota's fascia, spontaneous hemostasis is often achieved when external force is applied, due to the packing effect of this fascia. Therefore, conservative treatment is chosen in many cases of adrenal hemorrhage. In this case, only a small amount of hematoma formation was observed around the right adrenal gland on arrival, and his vital signs were stable, so non-operative management was adopted. There has been no report of a case of delayed rupture of the adrenal gland after blunt trauma, as in this case.
Among intra-abdominal organs, cases of delayed rupture after splenic injury have occasionally been reported [6], but the mechanism of rupture is unknown. Some theories include the formation of a pseudoaneurysm or the rupture of the capsule due to increased internal pressure caused by the melting of the clot [6]. In our case, it was possible that there was pseudoaneurysm formation at the time of injury. In the case of pseudoaneurysms of the spleen, 44 % reportedly resolve in an average of 5.2 days [7], and there have been cases of spontaneous resolution by thrombus occlusion. Furthemore, our patient was on Limaprost alfadex at the time of admission, which was discontinued after admission. No anticoagulation therapy was being administered at the time of the rupture, and it is unlikely that the coagulation status played a role in the rupture. Since ours is the first report of delayed rupture of the adrenal gland, the natural history of adrenal injury is unknown. However, the fact that the adrenal gland is a parenchymal organ with terminal blood vessels and an abundant blood flow suggests the same rupture mechanism as that of pseudoaneurysms of the spleen.
Conclusion
Even in rare cases of mild adrenal injuries, where packing with Gerota's fascia can be expected, there are rare cases of delayed rupture, which must be promptly diagnosed and treated with hemostatic therapy.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial sectors.
Declaration of competing interest
None.
References
- 1.Stawicki S.P., Hoey B.A., Grossman M.D., et al. Adrenal gland trauma is associated with high injury severity and mortality. Curr. Surg. 2003;60:431–436. doi: 10.1016/S0149-7944(02)00796-1. [DOI] [PubMed] [Google Scholar]
- 2.de Camargo Galindo Gabriel Franco, Pagamisse Otávio Soriano Teruel, Lima Rafael De, et al. Nonoperative treatment of a blunt adrenal gland trauma with blush: A case report. Trauma Case Rep. 2021;32 doi: 10.1016/j.tcr.2021.100454. Mar 11. Published online 2021 Mar 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sinelnikov A.O., Abujudeh H.H., Chan D., et al. CT manifestations of adrenal trauma: experience with 73 cases. Emerg. Radiol. 2007;13:313–318. doi: 10.1007/s10140-006-0563-z. [DOI] [PubMed] [Google Scholar]
- 4.Rana A.I., Kenney P.J., Lockhart M.E., et al. Adrenal gland hematomas in trauma patients. Radiology. 2004;230:669–675. doi: 10.1148/radiol.2303021345. [DOI] [PubMed] [Google Scholar]
- 5.Karwacka I.M., Obołonczyk Ł., Sworczak K., et al. Adrenal hemorrhage: a single center experience and literature review. Adv. Clin. Exp. Med. 2018;27:681–687. doi: 10.17219/acem/68897. [DOI] [PubMed] [Google Scholar]
- 6.Kluger Y., Paul D.B., Raves J.J., et al. Delayed rupture of the spleen–myths, facts, and their importance: case reports and literature review. J. Trauma. 1994;36:568–571. [PubMed] [Google Scholar]
- 7.Muroya T., Ogura H., Shimizu K., et al. Delayed formation of splenic pseudoaneurysm following nonoperative management in blunt splenic injury: multi–institutional study in Osaka, Japan. J Trauma Acute care Surg. 2013;75:417–420. doi: 10.1097/TA.0b013e31829fda77. [DOI] [PubMed] [Google Scholar]