Abstract
Purpose
Emergency general surgery patients undergoing laparoscopic surgery are at reduced risk of mortality and may require reduced length of critical care stay. This study investigated the effect of laparoscopy on high-risk patients’ post-operative care requirements.
Methods
Data were retrieved for all patients entered into the NELA database between 2013 and 2018. Only high-risk surgical patients (P-POSSUM predicted mortality risk of ≥ 5%) were included. Patients undergoing laparoscopic and open emergency general surgical procedures were compared using a propensity score weighting approach. Outcome measures included total length of critical care (level 3) stay, overall length of stay and inpatient mortality.
Results
A total of 66,517 high-risk patients received emergency major abdominal surgery. A laparoscopic procedure was attempted in 6998 (10.5%); of these, the procedure was competed laparoscopically in 3492 (49.9%) and converted to open in 3506 (50.1%). Following inverse probability treatment weighting adjustment for patient disease and treatment characteristics, high-risk patients undergoing laparoscopic surgery had a shorter median ICU stay (1 day vs 2 days p < 0.001), overall hospital length of stay (11 days vs 14 days p < 0.001) and a lower inpatient mortality (16.0% vs 18.8%, p < 0.001). They were also less likely to have a prolonged ICU stay with an OR of 0.78 (95% CI 0.74–0.83, p < 0.001).
Conclusion
The results of this study suggest that in patients at high risk of post-operative mortality, laparoscopic emergency bowel surgery leads to a reduced length of critical care stay, overall length of stay and inpatient mortality compared to traditional laparotomy.
Keywords: Emergency general surgery, Laparoscopy, Critical care
Introduction
Morbidity and mortality risk prediction is a crucial part of the pre-operative workup for patients undergoing emergency laparotomy. Reliable risk prediction is an aide for clinicians in the appropriate counselling of, and shared decision-making with, patients and next-of-kin. In addition, it can be used for case-mix stratification, and benchmarking, and can guide resource allocation, for example informing healthcare providers on the likelihood of need for admission to critical care.
Numerous scoring tools are available to predict risk including P-POSSUM, NELA and NSQIP [1–3]. In the UK, one of the newest recommendations to improve care for this patient group is that “high-risk” patients—defined as those with a NELA score-predicted mortality of 5% or more—must be transferred to a critical care unit post-operatively [4]. This national recommendation is coupled to financial incentives, and now forms part of the Emergency Laparotomy Best Practice Tariff, an enhanced payment for healthcare providers who admit 80% or more of peri-operatively identified high-risk patients to a post-operative critical care bed.
Intensive care unit (ICU) beds are a precious resource within any hospital. They are fundamental to ensuring appropriate care for emergently admitted patients and also to ensure that cancer care and elective surgery can proceed safely. The emergence of SARS-CoV-2 and the subsequent COVID-19 pandemic has placed ICU beds under even further strain. Emergency general surgery patients are particularly resource intensive; they have longer lengths of stay and require more organ support when compared to other surgical specialties [5]. This represents a huge cost to hospitals and health care providers. In 2010, emergency surgical patients accounted for 14,000 admissions to ICU with a cost of £88 million [6]. It is now more important than ever that surgeons do as much as possible to minimise the morbidity and mortality of emergency surgery patients and utilise ICU resources appropriately.
Considering patients undergoing emergency major abdominal surgery, the majority of emergency bowel surgery is performed via laparotomy—in the UK, only 19% of cases are attempted using laparoscopy [7]. This figure has remained static over the previous 4 years. Data from single-centres and even the 7th NELA report have shown that patients undergoing laparoscopy require a reduced length of ICU stay; they have half the length of inpatient stay and a 30-day mortality a third of that of patients undergoing emergency laparotomy [7, 8]. It has been questioned whether this is an effect of selection bias, with laparoscopy reserved for the fittest and lowest-risk patients [7]. However, even when laparoscopic cases are matched with open cases at a population level, patients managed with laparoscopic surgery experience reduced blood loss and a shorter length of stay and their risk of mortality is reduced by half [9]. It is still unclear if the benefits of laparoscopy extend to high-risk patients who are at the greatest risk of death and likely they require the most resource-intensive care.
In the absence of randomised trial data, appropriately controlled observational studies, particularly when taken from large routine datasets, can provide evidence that is useful in clinical practice. In this study, a large national dataset of patients undergoing major emergency general surgery was analysed to establish what, if any, difference in outcome, including critical care utilisation, length of stay and overall mortality, was seen in high-risk patients comparing for risk-adjusted differences in surgical approach.
Material and methods
Patients entered into the NELA dataset between 2013 and 2018 were collated, anonymised and considered for inclusion in the study. NELA is estimated to have > 80% case ascertainment for patients undergoing emergency general surgery, excluding those with appendicitis, biliary disease, uncomplicated hernia or trauma [2]. Detailed inclusion criteria have been previously described [7]. The dataset from which cases were drawn for this study has been used to publish previously [10, 11].
Clinical data was ascertained including indication, operative findings, patient characteristic and measures of operative risk including P-POSSUM mortality risk [1]. Predictions of mortality using the NELA prediction tool were not included as these were unavailable for more than 50% of the dataset [2]. Patients were eligible for inclusion in the study if they had a P-POSSUM predicted mortality risk of ≥ 5% (i.e. high-risk patients) and if the inpatient episode was recorded as complete (i.e. patients were not recorded as still in patients in the analysis dataset). Patients were also excluded if they were recorded as having a ‘laparoscopic assisted’ operation as this was considered too imprecise a term. Of 118,355 patients in the full dataset, 68,228 had a recorded P-POSSUM mortality risk of ≥ 5% (57.2%). Of these patients, after excluding patients in whom outcome was unknown or who underwent a laparoscopic assisted procedure, a final sample size of 66,517 was obtained (Fig. 1).
Fig. 1.
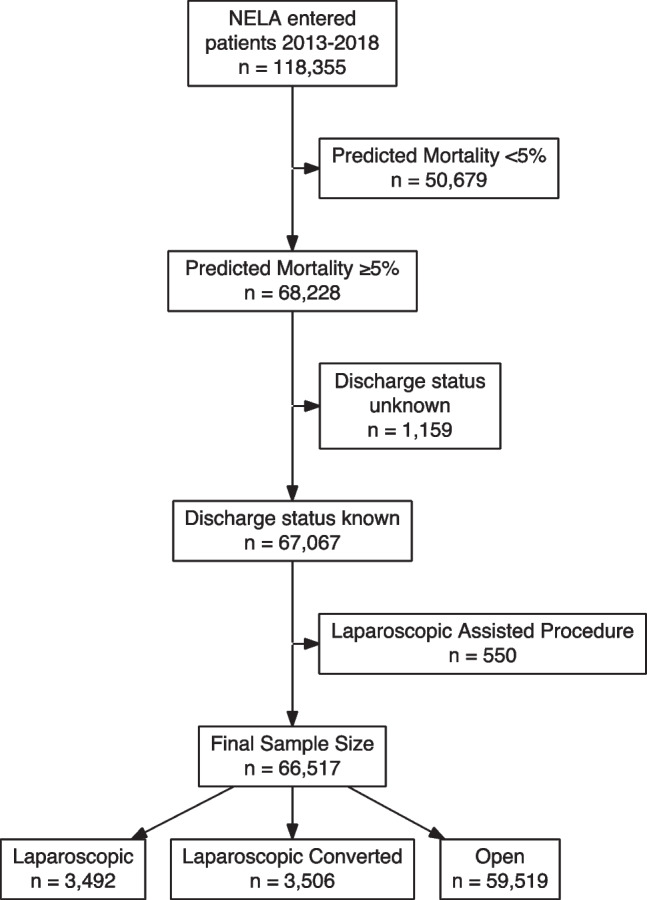
Flowchart of patient selection
The primary outcome measures were total length of intensive care (level 3) stay, overall length of stay and discharge status (alive/dead). Laparoscopic and open procedures were compared, with both laparoscopic converted and laparoscopic completed procedures considered together for the primary analysis.
Missing data was present in 5114 cases (7.7%). Timing of surgery (in hours or out of hours) was missing in 3.6% of cases, and procedure in 2.0%. All other variables had < 1% data points missing. Missingness was handled using multiple imputation by chained equations with 10 imputed datasets and 10 iterations [12].
The decision to undertake laparoscopic or open emergency surgery is influenced by patient, hospital and surgeon factors. A simple comparison of emergency laparoscopic and open surgery would be of limited value as it would describe the effect of surgical approach in two different patient groups. In order to measure the effect of laparoscopy in these non-randomised patient groups and reduce bias from selection and confounders, a propensity score weighting approach was taken [13]. The propensity score is the probability of being selected for a treatment based on a number of defined variables. The propensity score is generated by a multivariable logistic regression of receiving a treatment (in this case laparoscopic vs open surgery), and conditional on specified variables for which adjustment is to be made. Having calculated this probability for each case, the inverse of this is then used as a weight applied for all subsequent analysis with the aim of balancing the specified covariates between treatment arms. In this study, we used 18 patient, treatment and disease characteristics to balance between groups, which are listed in Table 1.
Table 1.
Characteristics used to weight analysis groups
| Patient and treatment details | Indication for surgery | Disease characteristics |
|---|---|---|
| Patient age | Peritonitis | Predicted blood boss |
| Sex | Perforation | Degree of peritoneal soiling |
| Procedure | Abscess | P-POSSUM predicted mortality |
| Operator grade | Anastomotic leak | |
| Institution case volume (quintile) | Intestinal obstruction | |
| Preoperative CT performed | Ischaemia | |
| Time of surgery | Colitis | |
| Malignancy |
The degree of covariate balance was assessed using the standardised mean difference (SMD), with a value of > 0.1 defined as indicating significant imbalance [13]. Propensity score weights were calculated individually in each imputed dataset and then combined by mean aggregation as has been described previously [14].
In addition to the primary analysis, a series of planned subgroup analyses were undertaken to examine the breadth of applicability of any demonstrated effects. Propensity scores were recalculated on each occasion as has been described previously [15]: firstly very-high-risk patients (P-POSSUM mortality > 10% and > 20%), followed by patients undergoing colorectal procedures, analysis of laparoscopic converted and laparoscopic completed procedures separately; patients operated on out of hours; and finally including only patients admitted to ICU. Analysis was conducted in R 4.0.1 with hypothesis testing using weighted statistical tests (Mann–Whitney U and chi-square test) and logistic regression.
Results
Cohort characteristics
Characteristics of the 66,517 high-risk patients who received emergency major abdominal surgery (as defined by NELA inclusion criteria) and were included in the study are shown in Table 2. A laparoscopic procedure was attempted in 6998 (10.5%), and of these the procedure was competed laparoscopically in 3492 (49.9%) and converted to open in 3506 (50.1%). Prior to weighting, the most notable differences between patients undergoing laparoscopic and open surgery were P-POSSUM mortality risk (median, laparoscopic 12.2% vs 17.7% open, p < 0.001), procedure performed (fewer resections of small bowel or colon, and more washout, peptic ulcer repair and adhesiolysis for laparoscopic approaches) and predicted blood loss, which was less in patients undergoing laparoscopic surgery.
Table 2.
Characteristics of high-risk patients who received emergency major abdominal surgery pre- and post-weighting
| Overall | Open | Laparoscopic | Pre weighting SMD | Post weighting SMD | ||
|---|---|---|---|---|---|---|
| n | 66,517 | 59,519 | 6998 | |||
| Hospital volume | Highest quintile | 22,676 (34.1) | 20,303 (34.1) | 2373 (33.9) | 0.103* | 0.038 |
| 2nd quintile | 14,933 (22.4) | 13,188 (22.2) | 1745 (24.9) | |||
| 3rd quintile | 12,775 (19.2) | 11,622 (19.5) | 1153 (16.5) | |||
| 4th quintile | 9928 (14.9) | 8935 (15.0) | 993 (14.2) | |||
| Lowest quintile | 6205 (9.3) | 5471 (9.2) | 734 (10.5) | |||
| Age | 18–30 | 2020 (3.0) | 1657 (2.8) | 363 (5.2) | 0.196* | 0.012 |
| 30–40 | 2326 (3.5) | 1923 (3.2) | 403 (5.8) | |||
| 40–50 | 4304 (6.5) | 3765 (6.3) | 539 (7.7) | |||
| 50–60 | 7291 (11.0) | 6492 (10.9) | 799 (11.4) | |||
| 60–70 | 13,142 (19.8) | 11,870 (19.9) | 1272 (18.2) | |||
| 70–80 | 20,383 (30.6) | 18,431 (31.0) | 1952 (27.9) | |||
| 80 + | 17,051 (25.6) | 15,381 (25.8) | 1670 (23.9) | |||
| Male sex | 32,605 (49.0) | 29,251 (49.1) | 3354 (47.9) | 0.024 | 0.020 | |
| Preoperative CT scan | 56,866 (86.3) | 51,046 (86.6) | 5820 (84.0) | 0.072 | 0.001 | |
| Predicted blood loss | < 100 ml | 19,930 (30.0) | 16,842 (28.3) | 3088 (44.2) | 0.351* | 0.029 |
| 101–500 ml | 39,917 (60.1) | 36,412 (61.3) | 3505 (50.2) | |||
| 501–999 ml | 4825 (7.3) | 4535 (7.6) | 290 (4.1) | |||
| 1000 ml + | 1746 (2.6) | 1641 (2.8) | 105 (1.5) | |||
| Senior surgeon present | Consultant | 60,105 (90.4) | 53,631 (90.2) | 6474 (92.6) | 0.085 | 0.014 |
| Non-consultant Career grade | 2545 (3.8) | 2334 (3.9) | 211 (3.0) | |||
| Trainee | 3802 (5.7) | 3494 (5.9) | 308 (4.4) | |||
| Operation performed out of hours | 27,576 (43.0) | 25,158 (43.9) | 2418 (35.8) | 0.166* | 0.007 | |
| P-POSSUM predicted mortality | 16.90 [8.80, 38.90] | 17.70 [9.00, 40.60] | 12.20 [7.40, 25.80] | 0.337* | 0.056 | |
| Type of procedure | General | 33,493 (51.4) | 29,635 (50.8) | 3858 (56.4) | 0.261* | |
| Upper gastrointestinal | 5418 (8.3) | 4523 (7.7) | 895 (13.1) | |||
| Colorectal | 26,296 (40.3) | 24,213 (41.5) | 2083 (30.5) | |||
| Procedure | Washout only | 1803 (2.8) | 1328 (2.3) | 475 (6.9) | 0.448* | 0.079 |
| Peptic ulcer repair/oversew | 4611 (7.1) | 3872 (6.6) | 739 (10.8) | |||
| Gastric surgery (other) | 807 (1.2) | 651 (1.1) | 156 (2.3) | |||
| Small-bowel resection | 10,394 (15.9) | 9697 (16.6) | 697 (10.2) | |||
| Left colectomy | 2244 (3.4) | 2039 (3.5) | 205 (3.0) | |||
| Right colectomy | 8266 (12.7) | 7495 (12.8) | 771 (11.3) | |||
| Subtotal/panproctocolectomy | 4037 (6.2) | 3738 (6.4) | 299 (4.4) | |||
| Hartmann’s procedure | 10,551 (16.2) | 9843 (16.9) | 708 (10.4) | |||
| Other | 10,139 (15.5) | 9112 (15.6) | 1027 (15.0) | |||
| Adhesiolysis | 6934 (10.6) | 6154 (10.5) | 780 (11.4) | |||
| Drainage of abscess | 1934 (3.0) | 1531 (2.6) | 403 (5.9) | |||
| Formation of stoma | 3487 (5.3) | 2911 (5.0) | 576 (8.4) | |||
| Peritoneal soiling | None | 18,759 (28.3) | 16,749 (28.2) | 2010 (28.8) | 0.138* | 0.010 |
| Serous fluid only | 16,488 (24.9) | 15,081 (25.4) | 1407 (20.2) | |||
| Localised pus | 7143 (10.8) | 6234 (10.5) | 909 (13.0) | |||
| Free pus, blood or bowel contents | 23,894 (36.0) | 21,247 (35.8) | 2647 (38.0) | |||
| Malignancy | None | 49,118 (74.1) | 43,796 (73.8) | 5322 (76.3) | 0.064 | 0.023 |
| Primary | 7667 (11.6) | 6948 (11.7) | 719 (10.3) | |||
| Nodal | 3123 (4.7) | 2841 (4.8) | 282 (4.0) | |||
| Disseminated | 6394 (9.6) | 5746 (9.7) | 648 (9.3) | |||
| Indication | Peritonitis | 17,606 (26.5) | 15,572 (26.2) | 2034 (29.1) | 0.065 | 0.007 |
| Perforation | 20,563 (30.9) | 18,319 (30.8) | 2244 (32.1) | 0.028 | 0.030 | |
| Abscess | 4905 (7.4) | 4261 (7.2) | 644 (9.2) | 0.075 | 0.004 | |
| Anastomotic leak | 6785 (10.2) | 6019 (10.1) | 766 (10.9) | 0.027 | 0.019 | |
| Obstruction | 10,679 (16.1) | 9939 (16.7) | 740 (10.6) | 0.179* | 0.020 | |
| Ischaemia | 6884 (10.3) | 6443 (10.8) | 441 (6.3) | 0.162* | 0.042 | |
| Colitis | 2005 (3.0) | 1687 (2.8) | 318 (4.5) | 0.091 | 0.006 | |
Values are count (percentage) and median (IQR). SMD standardised mean difference. *SMD > 0.1, indicating significant imbalance between groups. Propensity score weighting minimises imbalance in all measured characteristics
A standardised mean difference of > 0.1 (indicating significant imbalance) prior to weighting was seen in 10 out of 18 variables used for inverse probability of treatment weighting (IPTW), all of which were reduced to < 0.1 by the weighting process. The mean SMD was also reduced from 0.145 to 0.012, suggesting that IPTW has been effective in creating a dataset suitable for analysis and that residual differences in the specified covariates between these groups are small.
Outcomes
Prior to weighting, shorter ICU stay (median 0 vs 2 days, p < 0.001) and overall length of stay (median 11 vs 14 days, p < 0.001) were observed, and patients were more likely to be discharged alive (89.0% vs 80.7%, p < 0.001). Fewer patients undergoing laparoscopic surgery were admitted to ICU in comparison to those undergoing an open operation (47.9% vs 61.7%, p < 0.001).
Following IPTW and adjustment for patient disease and treatment characteristics, patients undergoing laparoscopic surgery had a shorter median ICU stay (1 day vs 2 days p < 0.001), overall hospital length of stay (11 days vs 14 days p < 0.001) and a lower inpatient mortality (16.0% vs 18.8%, p < 0.001). They were also less likely to have a prolonged ICU stay (greater than 75th percentile of ICU stay for all patients, i.e. 4 days) with an OR of 0.78 (95% CI 0.74–0.83, p < 0.001, 19.6% vs 24.1% p < 0.001).
Subgroup analyses
Analysis was carried out in various subgroups, with IPTW recalculated and applied separately. Excellent balance was achieved in all subgroups, with no covariates exhibiting a residual SMD > 0.1. Results were broadly consistent with the primary analysis (Table 3), with a shorter length of stay both overall and on ICU and a lower in hospital mortality for patients undergoing laparoscopic surgery. For patients where the procedure was converted to open, in hospital mortality was not statistically different (17.8% laparoscopic converted, 19.1% open, p = 0.061); however a reduced ICU and overall length of stay was still seen.
Table 3.
Subgroup analyses
| Subgroup | Cases | ICU length of stay (median days) | Overall length of stay (median days) | In-hospital mortality | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Open | Laparoscopic | Open | Laparoscopic | p# | Open | Laparoscopic | p# | Open | Laparoscopic | p value^ | |
| P-POSSUM > 10% | 42,283 | 4194 | 2 | 2 | < 0.001* | 15 | 12 | < 0.001* | 23.8% | 20.2% | < 0.001* |
| P-POSSUM > 20% | 27,327 | 2266 | 2 | 3 | < 0.001* | 16 | 13 | < 0.001* | 30.2% | 26.5% | < 0.001* |
| Colorectal Procedures | 24,213 | 2083 | 1 | 2 | < 0.001* | 14 | 13 | < 0.001* | 17.4% | 15.5% | 0.031* |
| Laparoscopic Converted | 59,519 | 3506 | 1 | 2 | < 0.001* | 14 | 12 | < 0.001* | 19.1% | 17.8% | 0.061 |
| Laparoscopic Completed | 59,519 | 3492 | 0 | 2 | < 0.001* | 14 | 10 | < 0.001* | 18.9% | 14.8% | < 0.001* |
| Operated out of hours | 25,158 | 2418 | 1 | 2 | < 0.001* | 14 | 11 | < 0.001* | 21.4% | 19.3% | 0.012* |
| Admitted to ICU | 36,506 | 3345 | 2 | 2 | < 0.001* | 16 | 14 | < 0.001* | 24.7% | 21.4% | < 0.001* |
SMD < 0.1 was achieved for all variables in all subgroups
#Weighted Mann–Whitney U test
^Chi-square test
*p < 0.05
Discussion
The results of this study suggest that in patients at high risk of post-operative mortality, laparoscopic emergency bowel surgery leads to a reduced length of critical care stay, overall length of stay and inpatient mortality compared to traditional laparotomy. By excluding low-risk patients with an estimated mortality risk of < 5%, and by utilising a propensity score weighted approach, we have attempted to address the risk of occult selection bias, as well as differences in patient demographics and pathology, to create a balanced group of patients for analysis.
This paper specifically focusses on high-risk general surgical patients as they are a resource intensive group with poor outcomes. High-risk patients experience excess complication rates, they are frequently elderly and comorbid and they have complex needs and frequently require a prolonged length of hospital stay [6]. By including only high-risk patients undergoing surgery, this study focuses not only on the patient cohort most likely to require resource-intensive care; it also addresses clinically relevant differences in outcome such as ICU length of stay, for patients where UK national health policy now mandates post-operative care on a level 2 or 3 care unit.
The benefits of laparoscopy in gastrointestinal surgery are well established. Laparoscopy permits surgery through smaller incisions; there is reduced blood loss and there is a reduced systemic inflammatory response to surgery [15–17]. Post-operatively, data have suggested that this translates into an earlier return of respiratory and gut function and reduced analgesic requirement [16, 18]. Laparoscopy reduces length of stay and there is reduced morbidity and mortality [19]. These reductions in mortality have been shown to reduce hospital costs [20]. Longer term benefits of laparoscopy are furthermore to be expected with reduced rates of incisional hernia and adhesional intestinal obstruction [21].
The most recent NELA report observes that 19% of emergency cases were attempted with laparoscopy—this figure has remained static since 2018 [7]. It is unclear why this is the case as there is sufficient surgical ability to support the use of laparoscopy in the emergency setting. Laparoscopy is commonplace in major elective surgery; the laparoscopic approach is the gold standard for the majority of upper gastrointestinal procedures; in colorectal surgery, data from the National Bowel Cancer Audit shows that laparoscopic resection rates have increased annually since 2013 (48 to 61%). Similarly, appendicitis and acute biliary conditions are now managed overwhelmingly with laparoscopy [22, 23]. Data from randomised controlled trials, meta analyses and international guidelines increasingly support the use of laparoscopy to manage perforated peptic ulcer, small-bowel obstruction and diverticulitis [24–30]. Despite this, two recent surveys have shown that the choice of surgical approach is heavily influenced by subspecialty, time since completion of training and personal preference [31, 32].
In this study, almost half of laparoscopic procedures in high-risk general surgery cases were converted to open. Despite this, a reduced ICU stay and overall length of stay was seen where procedures are started laparoscopically when compared to operations that are performed open. This was demonstrated in a previous paper whereby patients whose case was started laparoscopically still benefitted from reduced blood loss, a shorter duration of hospital stay and a reduced risk of death even if the procedure was converted to laparotomy [9]. Without knowing the reasons for conversion, this suggests that procedures were unlikely to have been converted to open due to any ill effect of laparoscopy. Furthermore, if a procedure was converted to a laparotomy because of a negative effect of laparoscopy (such as pneumoperitoneum or extreme positioning), the impact is transient. It is our own experience that an initial laparoscopy can localise and mobilise problematic bowel resulting in a smaller abdominal incision. If a case is not amenable to laparoscopy, this is often immediately apparent and the case can be converted to laparotomy with little time wasted.
Mortality, morbidity and length of stay are frequently used as endpoints to demonstrate the superiority of laparoscopy over open surgery. This paper is unique in that it investigates the impact of laparoscopy on critical care stay. ICU stay is a useful marker for severity of illness, organ failure and response to surgery. Laparoscopy was seen to reduce the length of ICU stay independent of patient and disease characteristics. Reducing length of ICU stay has benefits for both patients and healthcare providers. There is evidence that patients with a prolonged length of critical care stay have worse short-term outcomes. These start to become apparent as soon as after 48 h of critical care admission [33]. Similarly, a prolonged length of ICU stay is associated with worse long-term physical, psychological and cognitive outcomes [33]. Reducing the length of ICU stay has been shown to reduce the length of overall stay, and analysis of a large North American database has shown that for every day spent in a critical care bed patients spend an extra 1.5 days in a regular ward bed [34]. For healthcare providers, there is a potential financial advantage—ICU patients are resource intensive, a large proportion of hospital budgets are spent on a small number of patients. Critical care treatment is most expensive in the first 5 days of admission. The exact cost of critical care treatment per day is difficult to calculate as this varies according to the complexity of the patient and condition being managed, but data from Canada has shown that reducing the length of critical care stay by one day can reduce hospital expenditure by 1% or equivalent to £500,000 in a year [35].
It is important that surgeons use intensive care services appropriately and reduce the demand for beds where possible. ICU beds are currently under extreme demand. The UK has a reduced number of beds per capita compared to North American and European nations [36]. Prior to the pandemic, these beds were operating at 81% capacity [37]. The highest level recommended for safe and efficient patient care is 85% [38]. There is expected to be an annual increase in demand for critical care services of around 4% per year [39]. These beds are likely to be occupied by our ageing and increasingly comorbid population [27]. When demand for ICU beds outstrips supply, there is an impact on the provision of elective surgery and in extreme cases the quality of care [40]. A recent national audit demonstrated that a lack of critical beds was the leading cause for cancelled surgery [41]. Prior to the pandemic, it was estimated that nationally 280 urgent operations are cancelled each month due to a lack of ICU beds [37]. Cancellation of procedures causes emotional distress, has financial implications and has been demonstrated to lead to worse clinical outcomes amongst patients [42].
Any interrogation of the NELA database is inevitably limited by the quality and completeness of data inputted and omitted. This will inevitably introduce bias into the dataset which may not be addressed by our analytic approach with unpredictable consequences. However, our study used well-validated methods, including multiple imputation and propensity score weighting, to address known sources of bias which facilitates robust analysis. A further limitation is that we have only observed the length of critical care admission and not the interventions provided by ICU such as the level of organ support. Given the unpredictable nature of emergency surgery, it is challenging to conduct large-scale RCTs. Analyses from large population-based data are fundamental to inform best practice.
The quality of care for emergency general surgery patients is dependent on support from theatres, radiology teams and critical care capacity. This must be supported by appropriate consultant, medical and nursing cover [43, 44]. These all require training, recruitment and infrastructure change. This costs money and change can be slow. Most gastrointestinal surgeons utilise laparoscopy in their elective work and most hospitals possess laparoscopic equipment. A conscious decision to increase the uptake of laparoscopy for emergency cases could yield immediate improvements to outcomes at both patient and system level, with little extra cost.
Conclusion
This analysis suggests that across a large nationwide dataset, superior outcomes are seen when high-risk emergency general surgery procedures are conducted laparoscopically when compared to open surgery, even when adjusted for a broad range of confounding factors.
Authors’ contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Saqib Rahman and Stuart Mercer. The first draft of the manuscript was written by Iain Wilson and Saqib Rahman and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data availability
All data used in this study was provided by NELA. The complete dataset is available from the NELA study group.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Prytherch DR, Whiteley MS, Higgins B, et al. POSSUM and Portsmouth POSSUM for predicting mortality. Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity. Br J Surg. 1998;85:1217–1220. doi: 10.1046/j.1365-2168.1998.00840.x. [DOI] [PubMed] [Google Scholar]
- 2.Eugene N, Oliver CM, Bassett MG, et al. Development and internal validation of a novel risk adjustment model for adult patients undergoing emergency laparotomy surgery: the National Emergency Laparotomy Audit risk model. Br J Anaesth. 2018;121:739–748. doi: 10.1016/j.bja.2018.06.026. [DOI] [PubMed] [Google Scholar]
- 3.Bilimoria KY, Liu Y, Paruch JL, et al. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg. 2013;217(833–842):e1–3. doi: 10.1016/j.jamcollsurg.2013.07.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Principle standards reported by the National Emergency Laparotomy Audit (NELA). https://www.nela.org.uk/downloads/NELA%20standards.pdf
- 5.Lissauer ME, Galvagno SM, Rock P, et al. Increased ICU resource needs for an academic emergency general surgery service*. Crit Care Med. 2014;42:910–917. doi: 10.1097/CCM.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 6.Anderson ID (2011) The higher risk general surgical patient towards improved care for a forgotten group. https://www.rcseng.ac.uk/library-and-publications/rcs-publications/docs/the-higher-risk-general-surgical-patient/
- 7.(2021) Seventh Patient Report of the National Emergency Laparotomy Audit December 2019 to November 2020. https://www.nela.org.uk/Seventh-Patient-Report
- 8.Pucher PH, Carter NC, Knight BC, et al. Impact of laparoscopic approach in emergency major abdominal surgery: single-centre analysis of 748 consecutive cases. Ann R Coll Surg Engl. 2018;100:279–284. doi: 10.1308/rcsann.2017.0229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pucher PH, Mackenzie H, Tucker V, Mercer SJ. A national propensity score-matched analysis of emergency laparoscopic versus open abdominal surgery. Br J Surg. 2021;108:934–940. doi: 10.1093/bjs/znab048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rahman SA, Pickering O, Tucker V, et al. Outcomes after independent trainee versus consultant-led emergency laparotomy: inverse propensity score population dataset analysis. Ann Surg. 2021 doi: 10.1097/SLA.0000000000005352. [DOI] [PubMed] [Google Scholar]
- 11.Pucher PH, Rahman SA, Mackenzie H, et al. Feasibility of laparoscopy and factors associated with conversion to open in minimally invasive emergency major abdominal surgery: population database analysis. Surg Endosc. 2021 doi: 10.1007/s00464-021-08803-5. [DOI] [PubMed] [Google Scholar]
- 12.Buuren S van, Groothuis-Oudshoorn K (2011) mice : multivariate imputation by chained equations in R. J Stat Soft 45. 10.18637/jss.v045.i03
- 13.Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Statist Med. 2015;34:3661–3679. doi: 10.1002/sim.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mitra R, Reiter JP. A comparison of two methods of estimating propensity scores after multiple imputation. Stat Methods Med Res. 2016;25:188–204. doi: 10.1177/0962280212445945. [DOI] [PubMed] [Google Scholar]
- 15.Wang SV, Jin Y, Fireman B, et al. Relative performance of propensity score matching strategies for subgroup analyses. Am J Epidemiol. 2018;187:1799–1807. doi: 10.1093/aje/kwy049. [DOI] [PubMed] [Google Scholar]
- 16.Zeng F, Chen L, Liao M, et al. Laparoscopic versus open gastrectomy for gastric cancer. World J Surg Onc. 2020;18:20. doi: 10.1186/s12957-020-1795-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Watt DG, Horgan PG, McMillan DC. Routine clinical markers of the magnitude of the systemic inflammatory response after elective operation: a systematic review. Surgery. 2015;157:362–380. doi: 10.1016/j.surg.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 18.Abraham NS, Young JM, Solomon MJ. Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg. 2004;91:1111–1124. doi: 10.1002/bjs.4640. [DOI] [PubMed] [Google Scholar]
- 19.Mamidanna R. Reduced risk of medical morbidity and mortality in patients selected for laparoscopic colorectal resection in England: a population-based study. Arch Surg. 2012;147:219. doi: 10.1001/archsurg.2011.311. [DOI] [PubMed] [Google Scholar]
- 20.Laudicella M, Walsh B, Munasinghe A, Faiz O. Impact of laparoscopic versus open surgery on hospital costs for colon cancer: a population-based retrospective cohort study. BMJ Open. 2016;6:e012977. doi: 10.1136/bmjopen-2016-012977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Udayasiri DK, Skandarajah A, Hayes IP. Laparoscopic compared with open resection for colorectal cancer and long-term incidence of adhesional intestinal obstruction and incisional hernia: a systematic review and meta-analysis. Dis Colon Rectum. 2020;63:101–112. doi: 10.1097/DCR.0000000000001540. [DOI] [PubMed] [Google Scholar]
- 22.National Surgical Research Collaborative Multicentre observational study of performance variation in provision and outcome of emergency appendicectomy. Br J Surg. 2013;100:1240–1252. doi: 10.1002/bjs.9201. [DOI] [PubMed] [Google Scholar]
- 23.CholeS Study Group, West Midlands Research Collaborative Population-based cohort study of outcomes following cholecystectomy for benign gallbladder diseases. Br J Surg. 2016;103:1704–1715. doi: 10.1002/bjs.10287. [DOI] [PubMed] [Google Scholar]
- 24.Cirocchi R, Soreide K, Di Saverio S, et al. Meta-analysis of perioperative outcomes of acute laparoscopic versus open repair of perforated gastroduodenal ulcers. J Trauma Acute Care Surg. 2018;85:417–425. doi: 10.1097/TA.0000000000001925. [DOI] [PubMed] [Google Scholar]
- 25.Sallinen V, Di Saverio S, Haukijärvi E, et al. Laparoscopic versus open adhesiolysis for adhesive small bowel obstruction (LASSO): an international, multicentre, randomised, open-label trial. Lancet Gastroenterol Hepatol. 2019;4:278–286. doi: 10.1016/S2468-1253(19)30016-0. [DOI] [PubMed] [Google Scholar]
- 26.Cirocchi R, Fearnhead N, Vettoretto N, et al. The role of emergency laparoscopic colectomy for complicated sigmoid diverticulits: a systematic review and meta-analysis. Surgeon. 2019;17:360–369. doi: 10.1016/j.surge.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 27.Tarasconi A, Coccolini F, Biffl WL, et al. Perforated and bleeding peptic ulcer: WSES guidelines. World J Emerg Surg. 2020;15:3. doi: 10.1186/s13017-019-0283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sartelli M, Weber DG, Kluger Y, et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15:32. doi: 10.1186/s13017-020-00313-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ten Broek RPG, Krielen P, Di Saverio S, et al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. 2018;13:24. doi: 10.1186/s13017-018-0185-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agresta F, Ansaloni L, Baiocchi GL, et al. Laparoscopic approach to acute abdomen from the Consensus Development Conference of the Società Italiana di Chirurgia Endoscopica e nuove tecnologie (SICE), Associazione Chirurghi Ospedalieri Italiani (ACOI), Società Italiana di Chirurgia (SIC), Società Italiana di Chirurgia d’Urgenza e del Trauma (SICUT), Società Italiana di Chirurgia nell’Ospedalità Privata (SICOP), and the European Association for Endoscopic Surgery (EAES) Surg Endosc. 2012;26:2134–2164. doi: 10.1007/s00464-012-2331-3. [DOI] [PubMed] [Google Scholar]
- 31.Heywood N, Parmar KL, Stott M, et al. The laparoscopy in emergency general surgery (LEGS) study: a questionnaire survey of UK practice. Ann R Coll Surg Engl. 2021;103:120–129. doi: 10.1308/rcsann.2020.7005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee MJ, Sayers AE, Wilson TR, et al. Current management of small bowel obstruction in the UK: results from the National Audit of Small Bowel Obstruction clinical practice survey. Colorectal Dis. 2018;20:623–630. doi: 10.1111/codi.14016. [DOI] [PubMed] [Google Scholar]
- 33.Mackie-Savage UF, Lathlean J. The long-term effects of prolonged intensive care stay postcardiac surgery. J Card Surg. 2020;35:3099–3107. doi: 10.1111/jocs.14963. [DOI] [PubMed] [Google Scholar]
- 34.Lilly CM, Zuckerman IH, Badawi O, Riker RR. Benchmark data from more than 240,000 adults that reflect the current practice of critical care in the United States. Chest. 2011;140:1232–1242. doi: 10.1378/chest.11-0718. [DOI] [PubMed] [Google Scholar]
- 35.Evans J, Kobewka D, Thavorn K, et al. The impact of reducing intensive care unit length of stay on hospital costs: evidence from a tertiary care hospital in Canada. Can J Anesth/J Can Anesth. 2018;65:627–635. doi: 10.1007/s12630-018-1087-1. [DOI] [PubMed] [Google Scholar]
- 36.Wunsch H, Angus DC, Harrison DA, et al. Variation in critical care services across North America and Western Europe. Crit Care Med. 2008;36(2787–2793):e1–9. doi: 10.1097/CCM.0b013e318186aec8. [DOI] [PubMed] [Google Scholar]
- 37.Guidelines for the provision of intensive care services - edition 2 (2019). The Faculty of Intensive Care Medicine. https://www.ficm.ac.uk/sites/ficm/files/documents/2021-10/gpics-v2.pdf
- 38.(2018) Critical Capacity. A short research survey on critical care bed capacity (2018). The Faculty of Intensive Care Medicine. https://www.ficm.ac.uk/sites/ficm/files/documents/2021-10/ficm_critical_capacity.pdf
- 39.In-depth review of the anaesthetics and intensive care medicine workforce (2015). Final Report. Centre for Workforce Intelligence. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/507348/CfWI_Anaesthetics_ICM_main_report.pdf
- 40.Bagshaw SM, Wang X, Zygun DA, et al. Association between strained capacity and mortality among patients admitted to intensive care: a path-analysis modeling strategy. J Crit Care. 2018;43:81–87. doi: 10.1016/j.jcrc.2017.08.032. [DOI] [PubMed] [Google Scholar]
- 41.Wong DJN, Harris SK, Moonesinghe SR. Cancelled operations: a 7-day cohort study of planned adult inpatient surgery in 245 UK National Health Service hospitals. Br J Anaesth. 2018;121:730–738. doi: 10.1016/j.bja.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 42.Magnusson H, Felländer-Tsai L, Hansson MG, Ryd L. Cancellations of elective surgery may cause an inferior postoperative course: the ‘invisible hand’ of health-care prioritization? Clinical Ethics. 2011;6:27–31. doi: 10.1258/ce.2011.011005. [DOI] [Google Scholar]
- 43.Symons NRA, Moorthy K, Almoudaris AM, et al. Mortality in high-risk emergency general surgical admissions. Br J Surg. 2013;100:1318–1325. doi: 10.1002/bjs.9208. [DOI] [PubMed] [Google Scholar]
- 44.Ozdemir BA, Sinha S, Karthikesalingam A, et al. Mortality of emergency general surgical patients and associations with hospital structures and processes. Br J Anaesth. 2016;116:54–62. doi: 10.1093/bja/aev372. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used in this study was provided by NELA. The complete dataset is available from the NELA study group.


