Key Points
Question
How do trauma team activation fees in the US vary by region and hospital characteristic?
Findings
In this cross-sectional study of 523 trauma centers in the US, the median tier 1 trauma activation fee was $9500, and fees ranged widely from $1000 to $61 734. Trauma activation fees were higher in the West and in for-profit hospitals.
Meaning
These findings suggest that some patients who sustain serious traumatic injuries will incur disproportionately high trauma activation fees depending on the trauma center to which they are brought and that standardization of trauma activation fees is warranted.
Abstract
Importance
Trauma centers must be readily equipped to handle a variety of life-threatening injuries and consequently may charge a fee for the activation of their trauma team. Regional and hospital-related variations in trauma activation fees across the US have not been formally assessed.
Objective
To evaluate the variability of trauma activation fees from trauma centers across the US and examine whether certain hospital characteristics are associated with higher activation fees.
Design, Setting, and Participants
This cross-sectional study used data from the American College of Surgeons website to identify all trauma centers in the US that were listed as verified from inception of the verification database through March 4, 2022 (N = 546). Five military hospitals were excluded, and trauma activation fees could not be found for 18 trauma centers; the remaining 523 hospitals were included in the analysis. Each hospital’s publicly available chargemaster (a comprehensive list of a hospital’s products, procedures, and services) was searched to obtain its trauma activation fees. Two levels of trauma activation fees were recorded: tier 1 (full activation) and tier 2 (partial activation). Hospital-specific data were obtained from the American Hospital Association website. All data were collected between January 2 and March 11, 2022. Linear regression analyses were performed to assess potential associations between hospital characteristics (type of control [for profit, government, church, or other nonprofit], hospital system [owner], number of staffed beds, and academic vs nonacademic status) and trauma activation fees.
Main Outcomes and Measures
Median and mean trauma activation fees nationally and stratified by location, hospital system, and other hospital characteristics.
Results
Of 523 trauma centers included in the analysis, most were located in the Midwest (180 centers) and West (129 centers). There were 176 adult level I trauma centers and 200 adult level II trauma centers; 69 centers had for-profit status, and 415 were academic. Overall, the median (IQR) tier 1 trauma activation fee was $9500 ($5601-$17 805), and the mean (SD) tier 1 trauma activation fee was $13 349 ($11 034); these fees ranged from $1000 to $61 734. Median (IQR) trauma activation fees were highest in the West ($18 099 [$10 741-$$27 607]), especially in California, where the median (IQR) activation fee was $24 057 ($15 979-$33 618). Trauma activation fees were also higher at for-profit hospitals, most of which were owned by the HCA Healthcare system, which had 43 trauma centers and a median (IQR) tier 1 trauma activation fee of $29 999 ($20 196-$37 589).
Conclusions And Relevance
In this study, trauma activation fees varied widely among hospitals in the US. Regional variation in these fees was substantial, with hospitals in the West charging substantially more than those in other locations. In addition, for-profit hospitals charged more than other types of hospitals. These findings suggest that some patients with serious traumatic injuries will incur disproportionately high trauma activation fees depending on the trauma center to which they are brought. Therefore, standardization of trauma activation fees is warranted.
This cross-sectional study examines the variability of trauma activation fees at trauma centers across the US and assesses whether certain hospital characteristics are associated with higher fees.
Introduction
Traumatic injuries are a major contributor to total US health care spending.1 Patients with serious traumatic injuries often receive care at trauma centers where the cost is high, at least in part because trauma centers must be continuously prepared to treat life-threatening injuries.2 However, trauma centers have been found to improve survival rates among patients with serious injuries.3,4 At the same time, previous data have suggested that more than one-third of patients brought to trauma centers do not meet field triage guidelines for transport to trauma centers.5 These patients or their insurance payers may thus bear the monetary expense of a visit to a trauma center without having a medical need for it.
Among the charges that may be accrued for a visit to a trauma center is the trauma activation fee, which is a charge for the mobilization of the medical professionals who make up the trauma team. Trauma activation fees were first approved in 2002 after it was argued that the high cost of running trauma centers threatened to shut down many essential trauma centers.6 While a trauma activation fee may be justified, popular media articles have decried the large amounts charged for trauma activation for, in some cases, very minor injuries.7,8,9 Moreover, data from 1 study10 found a large variation in trauma activation fees at trauma centers in Florida, with for-profit hospitals charging substantially more. However, to our knowledge, no published studies have performed a comprehensive analysis of trauma activation fees, and little is known about the variability of trauma activation fees on a national level. We thus performed a cross-sectional study to evaluate the variability of trauma activation fees in the US and examine whether there were hospital characteristics that were associated with higher fees.
Methods
Study Design and Setting
We performed a cross-sectional evaluation of the trauma activation fees of all trauma centers in the US that were listed as verified by the American College of Surgeons (ACS) website11 from inception of the verification database through March 4, 2022. Per the Common Rule,12 this study was exempt from institutional review board review because it used publicly available data. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cross-sectional studies.
Definition of Terms and Sample
Hospitals that are adequately prepared to provide care for patients with severe traumatic injuries may be designated as trauma centers by state or local governmental agencies, but the ACS has its own verification program for trauma centers.13 Our study only included trauma centers that had been verified by the ACS. Trauma centers may be designated as level I, II, III, IV, or V (with level I having the most resources),14 but the ACS website lists verifications only for levels I to III. Therefore, level IV and level V trauma centers were not included. We also excluded military hospitals and trauma centers for which we could not obtain a trauma activation fee.
For the purposes of this study, trauma activation was defined as the mobilization of medical professionals (the trauma team) who coordinate to care for a patient with traumatic injury. The trauma team composition varies, but may include a trauma surgeon, an emergency medicine physician, an anesthesiologist, a radiologist, nurses, a radiology technician, and others.15 The decision to initiate a trauma activation is based on predefined criteria, often including vital sign abnormalities, neurological function, and mechanism of injury.16 Some trauma centers have multiple types of trauma activation such as tier 1 or level 1 (ie, full or major) activation and tier 2 or level 2 (ie, partial or minor) activation. For a tier 2 activation, the trauma team may include fewer people.17
When a trauma activation occurs, the patient usually incurs a trauma activation fee. Trauma centers bill for trauma activation using the current Healthcare Common Procedure Coding System code G0390 and revenue code 068 plus trauma center certification level. To bill under these codes, prearrival notification is required.18 Some hospitals bill for trauma team activation without prehospital notification or trauma team evaluation or consultation using different billing codes, but those types of activations were not assessed in this study.
Data Collection
We initially recorded a list of all verified trauma centers from the ACS website11 on November 8, 2021, and updated the list on March 4, 2022. From the ACS website, we also recorded the location and level of each trauma center and whether the center was verified for adult patients, pediatric patients, or both. Hospital locations were stratified by state and region. Four regions (Midwest, Northeast, South, and West) were defined according to the Centers for Disease Control and Prevention boundaries.19 Next, we used the American Hospital Association directory20 to record the following information for each trauma center: type of control (for profit, government, church, or other nonprofit), hospital system (owner), number of staffed beds, and academic vs nonacademic status . For the purposes of this study, a trauma center was considered to be academic if it had both a medical school affiliation and medical residents working in the hospital.
We searched each hospital’s website for their publicly available chargemaster (a comprehensive list of a hospital’s products, procedures, and services), which is required by federal law.21 We searched each chargemaster file to obtain the standard charges for trauma activation fees. If the chargemaster reported 2 levels of fees (such as full and partial activations), we recorded both fees, which we considered tier 1 (full activation) and tier 2 (partial activation).
All data were collected between January 2 and March 11, 2022, by 1 medical student and 1 physician, both of whom were trained by the principal investigator (T.Z.). The 2 abstractors both searched for the trauma activation fees for all trauma centers, which allowed for an assessment of the interrater reliability. The data were verified and adjudicated by 2 other physician investigators (T.Z. and O.J.M.). When an activation fee was not found by one of the abstractors, one of the other 2 physicians searched for it in the hospital’s chargemaster for verification. Similarly, if the 2 data abstractors recorded different values for an activation fee, one of the other 2 physicians acted as an adjudicator. In this manner, the abstracted trauma activation fees were all confirmed by a second individual.
If none of the investigators could locate the trauma activation fee on the hospital website, we emailed and called the hospital. If we were still unable to obtain the activation fee, the fee was deemed unavailable, and the trauma center was excluded from analysis.
Study Outcomes
The primary outcome of this study was the typical charges for trauma activation in the US and the variability of those charges. Hospital characteristics associated with higher trauma activation fees were also examined.
Statistical Analysis
We calculated the median (IQR) for each continuous hospital characteristic and the number (percentage) for each categorical characteristic. In addition, we calculated the median (IQR) and mean (SD) trauma activation fees for trauma centers nationally and stratified by each hospital characteristic. We performed univariate and multivariable linear regression analyses to assess associations between hospital characteristics and trauma activation fees. Hospital characteristics (type of control, hospital system, number of staffed beds, and academic vs nonacademic status) were used as variables for our regression models based on an a priori hypothesis and previous data10 suggesting possible associations between these characteristics and trauma activation fees. Associations were measured using the slopes of the regression lines, which represented the expected change in the trauma activation fee per unit change in the variable.
Next, we performed an exploratory analysis to examine whether certain hospital systems were outliers with regard to the amount they charged for trauma activation. For this analysis, we calculated the median and mean tier 1 activation fees for the hospital systems with at least 5 trauma centers. We then identified the hospital systems with the highest and lowest median tier 1 trauma activation fees. We compared the characteristics of hospitals for which we were unable to obtain the activation fees with the characteristics of hospitals included in our analysis.
Data were aggregated using Excel software, version 16.60 (Microsoft Corporation), and analyzed using R Studio software, version 2022.02.2 (R Foundation for Statistical Computing). Using 2-sided hypothesis tests, we considered P < .05 to be statistically significant.
Results
Sample and National Data
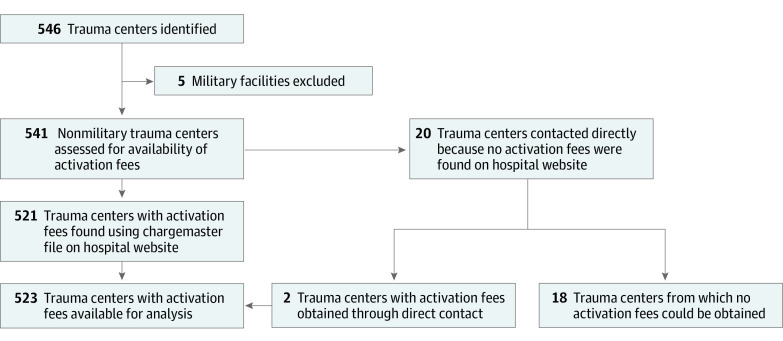
As of March 4, 2022, there were 546 verified trauma centers listed on the ACS website. Five military facilities were excluded from analysis. There were 35 trauma centers for which the 2 data abstractors recorded different tier 1 trauma activation fees (or for which at least one of the abstractors could not locate the fee on the hospital website). The overall interrater agreement was 93.5%, with a fixed marginal κ of 0.88 (95% CI, 0.79-0.96). Through additional searches of chargemaster files and direct contact with hospitals, we confirmed the trauma activation fees for 17 of the 35 hospitals with initially uncertain fees. We were unable to obtain the trauma activation fees for 18 trauma centers. We thus used 523 trauma centers for the analysis (Figure).
Figure. Included and Excluded Trauma Centers.
Among the 523 analyzed facilities, 410 (78.4%) were adult-only trauma centers, 37 (7.1%) were pediatric-only trauma centers, and 76 (14.5%) were both adult and pediatric trauma centers. Among the 486 trauma centers that treated adults, 176 (36.2%) were adult level I trauma centers, 200 (41.2%) were adult level II trauma centers, and 110 (22.6%) were adult level III trauma centers. Regarding location, 180 centers (34.4%) were in the Midwest, 96 (18.4%) were in the Northeast, 118 (22.6%) were in the South, and 129 (24.7%) were in the West. In addition, 69 trauma centers (13.2%) were for-profit facilities, and 415 (79.3%) were academic.
For all analyzed trauma centers, the median (IQR) tier 1 trauma activation fee was $9500 ($5601-$17 805), and the mean (SD) tier 1 trauma activation fee was $13 349 ($11 034). The minimum tier 1 activation fee was $1000, and the maximum was $61 734. A tier 2 trauma activation fee was reported by 379 of the 523 analyzed facilities (72.5%). Among those, the median (IQR) tier 2 activation fee was $7914 ($4406-$13 591), and the mean (SD) tier 2 activation fee was $10 519 ($8685). The tier 2 activation fees ranged from $325 to $45 257. The difference between the mean tier 1 and tier 2 fees was $2830 (95% CI, $1490-$4170).
Analysis of Differences by States and Regions
The median and mean trauma activation fees for the 10 states with the most trauma centers are shown in Table 1. California had the highest number of trauma centers (63) and, among those 10 states, the most expensive activation fees (median [IQR] tier 1 fee, $24 057 [$15 979-$33 618]). The median (IQR) activation fee in Massachusetts was $3491 ($2654-$6091), which was the lowest among those 10 states. Among all states (eTable in Supplement 1), Nevada had the highest median (IQR) tier 1 activation fee at $27 544 ($14 640-$34 625), and West Virginia had the lowest median (IQR) tier 1 fee at $1782 ($1434-$2821). In addition, the median (IQR) activation fees were highest in the West ($18 099 [$10 741-$27 607]) and lowest in the Northeast ($5841 [$2951-$7626]) (Table 2).
Table 1. Trauma Activation Fees for the 10 States With the Most Trauma Centers in the US.
| Location of trauma centers | Tier 1 trauma activation fees | Tier 2 trauma activation fees | ||||
|---|---|---|---|---|---|---|
| Trauma centers, No./total No.a | Fees, $ | Trauma centers, No./total No.a | Fees, $ | |||
| Median (IQR) | Mean (SD) | Median (IQR) | Mean (SD) | |||
| Entire US | 523/541 | 9500 (5601-17 805) | 13 349 (11 034) | 379/541 | 7914 (4406-13 591) | 10 519 (8685) |
| State | ||||||
| California | 63/63 | 24 057 (15 979-33 618) | 26 383 (13 815) | 49/63 | 19 970 (13 490-27 322) | 20 508 (8819) |
| Ohio | 48/50 | 8999 (4900-11 844) | 9725 (5965) | 36/50 | 7481 (2528-7974) | 5998 (4651) |
| Michigan | 46/47 | 8723 (6909-12 370) | 10 948 (7026) | 40/47 | 6379 (4920-9558) | 9161 (7408) |
| Texas | 44/46 | 15 670 (10 941-29 005) | 19 138 (11 697) | 35/46 | 11 106 (8144-16 845) | 13 764 (8556) |
| New York | 40/44 | 6047 (2339-7511) | 6028 (4220) | 21/44 | 3243 (1816-5250) | 4176 (2970) |
| Indiana | 23/23 | 11 466 (5298-17 220) | 13 527 (10 767) | 19/23 | 8972 (3392-9450) | 8979 (6190) |
| Arizona | 18/18 | 16 008 (5993-21 085) | 15 467 (8920) | 13/18 | 10 645 (10 645-18 366) | 13 370 (7650) |
| Colorado | 17/17 | 19 709 (10 827-25 573) | 18 737 (9327) | 14/17 | 13 290 (5331-20 489) | 13 640 (8772) |
| Massachusetts | 14/17 | 3491 (2654-6091) | 4593 (2616) | 7/17 | 3250 (2368-6640) | 4367 (2851) |
| Florida | 13/13 | 11 297 (7000-24 500) | 15 388 (11 343) | 3/13 | 8207 (5214-14 104) | 10 143 (9046) |
The number of trauma centers for which the trauma activation fee was obtained among the total number of verified trauma centers in the country or state.
Table 2. Trauma Activation Fees for Trauma Centers in the US, Stratified by Hospital Characteristic.
| Characteristic | Trauma centers, No./total No.b | Tier 1 trauma activation fees, $ | Association of characteristic with trauma activation feesa | ||
|---|---|---|---|---|---|
| Median (IQR) | Mean (SD) | Expected change in fee, $c | P value | ||
| Region | |||||
| Midwest | 180/183 | 8354 (5265-12 119) | 10 268 (8148) | −4697 | <.001 |
| Northeast | 96/104 | 5841 (2951-7626) | 6437 (4524) | −8466 | <.001 |
| South | 118/124 | 13 355 (7418-23 059) | 15 596 (10 878) | 2902 | .01 |
| West | 129/130 | 18 099 (10 741-27 607) | 20 735 (13 097) | 9805 | <.001 |
| Trauma center level | |||||
| Adult | |||||
| I | 176/181 | 10 291 (6189-16 792) | 12 962 (10 083) | −582 | .57 |
| II | 200/205 | 11 786 (7247-23 924) | 16 454 (12 732) | 5028 | <.001 |
| III | 110/116 | 5906 (3536-9122) | 7871 (6479) | −6937 | <.001 |
| Pediatric | |||||
| I | 61/65 | 10 189 (6816-15 535) | 12 574 (9343) | −878 | .56 |
| II | 52/52 | 10 446 (6822-16 212) | 13 970 (11 215) | 690 | .67 |
| Type of control | |||||
| For profit | 69/70 | 24 500 (14 690-34 184) | 24 551 (12 737) | 12 904 | <.001 |
| Church | 75/78 | 9552 (6190-18 070) | 12 745 (9702) | −705 | .61 |
| Government | 77/79 | 10 741 (6165-18 279) | 13 619 (11 231) | 317 | .82 |
| Other nonprofit | 302/314 | 7976 (5034-13 985) | 10 870 (9191) | −5865 | <.001 |
| Hospital sized | |||||
| Small | 16/17 | 5140 (3440-7574) | 6394 (5274) | −7175 | .01 |
| Medium | 344/355 | 9711 (5458-19 829) | 13 925 (11 527) | 1684 | .10 |
| Large | 163/169 | 10 053 (6818-15 240) | 12 815 (10 133) | −775 | .46 |
| Academic hospitale | 415/427 | 9533 (5781-16 795) | 12 932 (10 479) | −2017 | .09 |
Association was assessed using univariate linear regression analysis.
The number of trauma centers for which the trauma activation fee was obtained among the total number of verified trauma centers.
Values shown are the slopes of the regression lines, which represent the expected change in the tier 1 trauma activation fee per unit change in the variable.
Small was defined as fewer than 100 staffed beds, medium as 100 to 499 staffed beds, and large as more than 500 staffed beds.
An academic hospital was defined as a hospital having both resident physicians and a medical school affiliation.
Analyses of Other Hospital Characteristics
The results of univariate linear regression analyses of hospital characteristics are shown in Table 2. Level II trauma centers had higher activation fees than other levels, while level III trauma centers had lower activation fees. For-profit hospitals reported higher trauma activation fees, while nonprofit hospitals reported lower fees. Small hospitals (those with <100 staffed beds) had lower activation fees than medium and large hospitals. The primary characteristic associated with lower activation fees was location in the Northeast (expected change in fee/unit change in variable: −$8466; P < .001). The primary characteristic associated with higher activation fees was for-profit hospital status (expected change in fee/unit change in variable: $12 904; P < .001). In the multivariable analysis, characteristics that were still associated with higher trauma activation fees were location in the West (expected change in fee/unit change in variable: $9144; P < .001) and for-profit status (expected change in fee/unit change in variable: $10 088; P < .001) (Table 3).
Table 3. Association Between Trauma Center Characteristics and Tier 1 Trauma Activation Fees.
| Characteristic | Association of characteristic with trauma activation feesa | |
|---|---|---|
| Expected change in fee, $b | P value | |
| Region | ||
| Midwest | 1 [Reference] | NA |
| Northeast | −3582 | .002 |
| South | 1817 | .11 |
| West | 9144 | <.001 |
| Trauma center level | ||
| Adult | ||
| I | 1 [Reference] | NA |
| II | 660 | .55 |
| III | −5077 | <.001 |
| Pediatric only | 1629 | .35 |
| Type of control | ||
| For profit | 10 088 | <.001 |
| Church | 883 | .57 |
| Government | 1 [Reference] | NA |
| Other nonprofit | −807 | .51 |
| Hospital sizec | ||
| Small | −7179 | .006 |
| Medium | 1 [Reference] | NA |
| Large | 170 | .87 |
| Academic hospitald | −2459 | .02 |
Abbreviation: NA, not applicable.
Association was assessed using multivariable linear regression analysis.
Values shown are the slopes of the regression lines, which represent the expected change in the tier 1 trauma activation fee per unit change in the variable compared with the reference variable.
Small was defined as fewer than 100 staffed beds, medium as 100 to 499 staffed beds, and large as more than 500 staffed beds.
An academic hospital was defined as a hospital having both resident physicians and a medical school affiliation.
Analysis of Hospital Systems
We also compared the trauma activation fees of different hospital systems (Table 4). Trauma centers in the HCA Healthcare system had the highest median (IQR) tier 1 activation fee ($29 999 [$20 196-$37 589]) compared with any other hospital system, closely followed by trauma centers in the TENET Healthcare system ($29 924 [$27 723-$34 343]). Hospitals in the HCA Healthcare and TENET Healthcare systems comprised 50 of the 69 for-profit hospitals (72.5%; 43 hospitals in the HCA Healthcare system and 7 in the TENET Healthcare system) that reported tier 1 activation fees. In comparison, the median (IQR) tier 1 trauma activation fee for the 19 for-profit hospitals not in the HCA Healthcare or TENET Healthcare systems was $9185 ($4972-$14 621).
Table 4. Trauma Activation Fees for Hospital Systems With at Least 5 Trauma Centers in the US.
| Hospital system | Trauma centers, No./total No.a | Type of control | Location of trauma centers (No. of trauma centers)b | Tier 1 trauma activation fees, $ | |
|---|---|---|---|---|---|
| Median (IQR) | Mean (SD) | ||||
| HCA Healthcare | 43/43 | For-profit organization | South (27); Midwest (4); West (11); Northeast (1) | 29 999 (20 196-37 589) | 29 856 (10 521) |
| Ascension | 16/16 | Church | Midwest (14); South (2) | 10 763 (8013-12 352) | 12 518 (10 169) |
| CommonSpirit Health | 15/15 | Church | West (9); Midwest (5); South (1) | 8536 (4061-13 615) | 12 813 (14 931) |
| Trinity Health | 11/11 | Church | Midwest (8); Northeast (3) | 5846 (3029-8508) | 6914 (4983) |
| Providence | 8/8 | Church | West (6); South (2) | 23 680 (19 044-36 543) | 25 130 (13 117) |
| TENET Healthcare | 7/7 | For-profit organization | West (3); Midwest (3); South (1) | 29 924 (27 723-34 343) | 30 644 (6216) |
| Beaumont | 7/7 | Other nonprofit organization | Michigan (7) | 16 826 (16 826-16 826) | 15 559 (3353) |
| NYC Health + Hospitals | 7/7 | Government | New York (7) | 1817 (1817-1817) | 2596 (2169) |
| University Hospitals | 7/7 | Other nonprofit organization | Ohio (7) | 4900 (4900-9500) | 6871 (2459) |
| Banner Health | 7/7 | Other nonprofit organization | West (7) | 16 008 (8757-16 008) | 12 506 (4741) |
| McLaren Health Care | 6/6 | Other nonprofit organization | Michigan (6) | 7929 (6198-8646) | 7186 (1949) |
| Henry Ford Health System | 5/5 | Other nonprofit organization | Michigan (5) | 9075 (7150-9075) | 8560 (2435) |
| Intermountain Healthcare | 5/5 | Other nonprofit organization | Utah (5) | 11 728 (10 000-13 065) | 10 977 (2967) |
| Northwell Health | 5/5 | Other nonprofit organization | New York (5) | 7055 (6816-7750) | 7041 (792) |
| Mercy Health | 4/5 | Church | Ohio (4) | 16 011 (14 235-20 544) | 18 769 (6906) |
The number of trauma centers for which the trauma activation fee was obtained among the total number of verified trauma centers.
The number of trauma centers for which activation fees were obtained.
Other outliers included trauma centers in the Providence system (a church-run system), which had the highest median (IQR) tier 1 activation fee ($23 680 [$19 044-$36 543]) of any hospital system with nonprofit status, and trauma centers in the NYC Health + Hospitals system (a government-run system), which had the lowest median (IQR) tier 1 trauma activation fees of any hospital system with at least 5 trauma centers ($1817 [$1817-$1817]). While trauma centers in New York generally had lower trauma activation fees (Table 1), the fees charged by trauma centers in the NYC Health + Hospitals system were substantially lower than those of trauma centers in New York that were not in that system (median [IQR], $6816 [$3552-$7750]).
Analysis of Missing Data
Despite price transparency laws, we were unable to obtain the trauma activation fees for 18 of the 541 trauma centers (3.3%) eligible for inclusion (excluding the 5 military hospitals). This group of 18 hospitals consisted of 5 level I trauma centers (27.8%), 5 level II trauma centers (27.8%), and 6 level III trauma centers (33.3%). Three of these centers (16.7%) were located in the Midwest, 8 (44.4%) were in the Northeast, 6 (33.3%) were in the South, and 1 (5.6%) was in the West. One of those hospitals (5.6%) had for-profit status, and 12 (66.7%) were academic.
Comparison of the characteristics of the group of trauma centers with missing activation fee data with the characteristics of trauma centers included in the analysis revealed that the group with missing activation fee data had a higher percentage of level III centers, a lower percentage of for-profit hospitals, and a lower percentage of academic hospitals. These differences suggested that our estimates of the national median and mean trauma activation fees may have been overestimated.
Discussion
To our knowledge, this cross-sectional study performed the most comprehensive assessment of trauma activation fees in the US to date. The data we used were all publicly available, and we implemented a system in which 2 individuals had to agree on each center’s trauma activation fee. The trauma activation fee data were thus likely to be accurate.
Although price transparency rules for hospitals have been implemented, a patient who sustains a severe traumatic injury will not be able to review costs on a hospital website before being brought to a trauma center. Therefore, the cost variation among trauma centers should be clarified to the general public, and we had several important findings in this regard. First, we identified that trauma activation fees in the US varied widely, from $1000 to $61 734. Two previous survey studies22,23 also reported large variations in trauma activation fees, but these studies were limited by low response rates such that their analyses included only a small number of trauma centers. Our study provided more complete and updated data that confirmed those previous data.
Notably, several hospital characteristics were associated with the variation in these charges. Trauma centers located in the West, especially California and Nevada, charged more for trauma activation, while trauma centers in the Northeast charged less. This difference was substantial; for example, the median tier 1 activation fee in California ($24 057) was approximately 7 times higher than the fee in Massachusetts ($3491). It was unclear why these states charged substantially more for trauma activation. Previous data revealed that California was the sixteenth most expensive state for selected common health services,24 but it has not been established that California is an extreme outlier for health care costs. California has a high cost of living compared with other states, but New York (which has relatively low trauma activation fees) has a higher cost of living.25 Similarly, Nevada has a lower cost of living than both New York and California25 but has the highest median tier 1 fee. Thus, cost of living differences did not fully explain the substantial variation in trauma activation fees.
In addition, as previously reported for trauma centers in Florida only,10 for-profit hospitals charged more for trauma activation than other types of hospitals. Our study adds important new information by not only confirming the higher trauma activation fees at for-profit trauma centers on a national level but by including an analysis of trauma activation fees by hospital system. Notably, with 43 trauma centers under their purview, the HCA Healthcare system operates more trauma centers than any other hospital system and owns the majority of for-profit trauma centers in the US. Thus, the substantially higher activation fees of for-profit trauma centers were primarily produced by HCA Healthcare centers.
Media articles9,26 previously reported that HCA Healthcare hospitals charged higher trauma activation fees than other hospitals. Given its vast presence, the HCA Healthcare system is the easiest outlier to detect, but our analysis also identified other hospital systems that charged substantially more for trauma activation than other hospitals (eg, the TENET Healthcare system). As other for-profit hospitals (and some nonprofit hospitals) recognize the revenue being brought in by HCA Healthcare and TENET Healthcare hospitals, they may follow the example of those hospitals and increase their trauma activation fees. Given that patients who sustain severe injuries have little choice about the trauma center to which they are brought, standardization of trauma activation fees, allowing only for small variations by region to allow for differences in cost of living, is warranted.
Limitations
This study has several limitations. First, the standard charges for trauma activation reported in chargemaster documents generally do not equal the amount the patient is required to pay. Insurers negotiate lower rates, and uninsured patients are often given discounts. Second, we did not assess all factors that might be associated with trauma activation fees, such as regional differences in government funding for trauma care. Third, we were unable to obtain the trauma activation fees for 3.3% of eligible trauma centers; however, the fact that we were unable to obtain the trauma activation fees for some facilities is itself useful information because all hospitals are supposed to make these data publicly available. As we and several other researchers27,28 have noted, hospitals do not universally provide these data. Fourth, we only assessed the trauma activation fees for trauma centers that had been verified by the ACS, so our data may not be applicable to trauma centers only verified by their states.
Conclusions
This cross-sectional study found that trauma activation fees in the US varied widely, from $1000 to $61 734. Trauma centers in the West charged substantially more for trauma activation than those in other locations, while trauma centers in the Northeast charged the least. Even after adjusting for other hospital characteristics, for-profit hospitals charged more for trauma activation than other types of hospitals. Given that patients are unlikely to be able to assess prices in a timely manner after a serious injury, standardization of trauma activation fees should be pursued.
eTable. Median (IQR) and Mean (SD) Trauma Activation Fees (in Dollars) for All States in the US and the District of Columbia
Data Sharing Statement
References
- 1.Soni A. Top five most costly conditions among adults age 18 and older, 2012: estimates for the U.S. civilian noninstitutionalized adult population. Agency for Healthcare Research and Quality. April 2015. Statistical brief 471. Accessed October 5, 2021. http://www.meps.ahrq.gov/mepsweb/data_files/publications/st471/stat471.pdf [PubMed]
- 2.Ashley DW, Mullins RF, Dente CJ, et al. ; Georgia Research Institute for Trauma Study Group . How much green does it take to be orange? determining the cost associated with trauma center readiness. J Trauma Acute Care Surg. 2019;86(5):765-773. doi: 10.1097/TA.0000000000002213 [DOI] [PubMed] [Google Scholar]
- 3.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366-378. doi: 10.1056/NEJMsa052049 [DOI] [PubMed] [Google Scholar]
- 4.Pracht EE, Tepas JJ III, Langland-Orban B, Simpson L, Pieper P, Flint LM. Do pediatric patients with trauma in Florida have reduced mortality rates when treated in designated trauma centers? J Pediatr Surg. 2008;43(1):212-221. doi: 10.1016/j.jpedsurg.2007.09.047 [DOI] [PubMed] [Google Scholar]
- 5.Newgard CD, Staudenmayer K, Hsia RY, et al. The cost of overtriage: more than one-third of low-risk injured patients were taken to major trauma centers. Health Aff (Millwood). 2013;32(9):1591-1599. doi: 10.1377/hlthaff.2012.1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Uniform Billing Committee . UB-92 national uniform billing data element specifications as developed by the National Uniform Billing Committee. American Hospital Association. 2004. Form locator 42, UB 68X. Accessed October 5, 2021. https://www.highmarkbcbswv.com/PDFFiles/08_24_04_UB_Update.pdf
- 7.Skeptical Scalpel. What is a “trauma activation” and why does it cost so much? Physician’s Weekly. July 2, 2018. Accessed January 15, 2022. https://www.physiciansweekly.com/what-is-a-trauma-activation-and-why-does-it-cost-so-much
- 8.Gold J, Kliff S; Kaiser Health News. A baby was treated with a nap and a bottle of formula. his parents received an $18,000 bill. Vox. July 20, 2018. Accessed December 10, 2021. https://www.vox.com/2018/6/28/17506232/emergency-room-bill-fees-health-insurance-baby
- 9.Stein L, Zayas A. Florida trauma centers charge outrageous fees the moment you come through the door. Tampa Bay Times. March 8, 2014. Accessed June 28, 2022. https://www.tampabay.com/news/health/florida-trauma-centers-charge-outrageous-fees-the-moment-you-come-through/2169148/
- 10.Ryan JL, Pracht EE, Langland-Orban B. Association of trauma alert response charges with volume and hospital ownership type in Florida. Health Serv Res Manag Epidemiol. 2018;5:2333392818797793. doi: 10.1177/2333392818797793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hospital and facilities. American College of Surgeons. 2022. Accessed March 4, 2022. https://www.facs.org/search/trauma-centers?country=united%20states
- 12.Office for Human Research Protections. Federal policy for the protection of human subjects (“Common Rule”). Dept of Health and Human Services. 2018. Updated November 8, 2022. Accessed December 10, 2022. https://www.hhs.gov/ohrp/regulations-and-policy/regulations/common-rule/index.html
- 13.About the verification, review, and consultation program. American College of Surgeons. 2022. Accessed December 12, 2022. https://www.facs.org/quality-programs/trauma/quality/verification-review-and-consultation-program/about-vrc/
- 14.Southern AP, Celik DH. EMS, trauma center designation. In: StatPearls. StatPearls Publishing. 2021. Updated July 18, 2022. Accessed July 22, 2021. https://www.ncbi.nlm.nih.gov/books/NBK560553 [PubMed] [Google Scholar]
- 15.Groenestege-Kreb DT, van Maarseveen O, Leenen L. Trauma team. Br J Anaesth. 2014;113(2):258-265. doi: 10.1093/bja/aeu236 [DOI] [PubMed] [Google Scholar]
- 16.Morris RS, Karam BS, Murphy PB, et al. Field-triage, hospital-triage and triage-assessment: a literature review of the current phases of adult trauma triage. J Trauma Acute Care Surg. 2021;90(6):e138-e145. doi: 10.1097/TA.0000000000003125 [DOI] [PubMed] [Google Scholar]
- 17.Kouzminova N, Shatney C, Palm E, McCullough M, Sherck J. The efficacy of a two-tiered trauma activation system at a level I trauma center. J Trauma. 2009;67(4):829-833. doi: 10.1097/TA.0b013e3181b57b6d [DOI] [PubMed] [Google Scholar]
- 18.Centers for Medicare & Medicaid Services . Critical care services. In: Medicare Claims Processing Manual: Chapter 4–Part B Hospital (Including Inpatient Hospital Part B and OPPS). Centers for Medicare & Medicaid Services; 2020:chap 160.1. Updated September 8, 2022. Accessed October 18, 2021. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c04.pdf [Google Scholar]
- 19.Census regional trends for common human coronaviruses. Centers for Disease Control and Prevention. 2021. Updated December 7, 2022. Accessed October 10, 2021. https://www.cdc.gov/surveillance/nrevss/coronavirus/region.html
- 20.American Hospital Association. AHA guide: hospital quick search. Health Forum. 2022. Accessed March 11, 2022. https://guide.prod.iam.aha.org/guide/
- 21.Medicare and Medicaid programs: CY 2020 hospital outpatient PPS policy changes and payment rates and ambulatory surgical center payment system policy changes and payment rates. price transparency requirements for hospitals to make standard charges public. Fed Regist. 2019;84(22):65524-65606. Accessed July 4, 2022. https://www.federalregister.gov/d/2019-24931 [Google Scholar]
- 22.Fakhry SM, Potter C, Crain W, Maier R. Survey of national usage of trauma response charge codes: an opportunity for enhanced trauma center revenue. J Trauma. 2009;67(6):1352-1358. doi: 10.1097/TA.0b013e3181c3fdd4 [DOI] [PubMed] [Google Scholar]
- 23.Neeki MM, Serrano J, Dong F, et al. Variation in trauma team response fees in United States trauma centers: an additional undisclosed variable cost in trauma care. Cureus. 2022;14(1):e21776. doi: 10.7759/cureus.21776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scheffler RM, Arnold DR, Fulton BD. The sky’s the limit: health care prices and market consolidation in California. California Health Care Foundation. October 3, 2019. Accessed June 2, 2022. https://www.chcf.org/publication/the-skys-the-limit/#summary
- 25.Cost of living data series. Missouri Economic Research and Information Center. 2022. Accessed July 4, 2022. https://meric.mo.gov/data/cost-living-data-series
- 26.Hancock J. In alleged health care “money grab,” nation’s largest hospital chain cashes in on trauma centers. Kaiser Health News. June 14, 2021. Accessed October 10, 2021. https://khn.org/news/article/in-alleged-health-care-money-grab-nations-largest-hospital-chain-cashes-in-on-trauma-centers/
- 27.Ji Y, Kong E. US hospital characteristics associated with price transparency regulation compliance. JAMA Health Forum. 2022;3(6):e221702. doi: 10.1001/jamahealthforum.2022.1702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mathew AT, Jain B, Dee EC, Johnson J, Chino F. Assessment of compliance with Centers for Medicare & Medicaid Services price transparency final rule. JAMA Oncol. 2022;8(8):1212-1213. doi: 10.1001/jamaoncol.2022.1783 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Median (IQR) and Mean (SD) Trauma Activation Fees (in Dollars) for All States in the US and the District of Columbia
Data Sharing Statement