Abstract
Introduction
The South African government responded swiftly to the first wave of novel coronavirus (SARS-CoV-2) with a nationwide lockdown. Initial restrictions from March–July 2020 required people to stay at home unless accessing essential, life-saving services. We sought to understand how the COVID-19 pandemic and resulting lockdowns affected young people’s access to sexual and reproductive health services in a high-prevalence HIV setting.
Methods
We analysed data from a cross-sectional web-based questionnaire conducted with 15–24 year-olds from September–December 2020 in Eastern Cape, South Africa. The questionnaire was promoted through social media platforms. Participants were asked whether and how the COVID-19 pandemic and related restrictions affected their access to sexual and reproductive health services, through closed-ended and open-ended questions. Descriptive statistics using proportions were used to summarise responses, and open text was analysed using thematic analysis.
Results
Of 3431 respondents, the proportions reporting ‘more difficulty’ accessing HIV testing services, HIV self-screening kits, condoms, pre-exposure prophylaxis and antiretroviral treatment since the COVID-19 pandemic were 16.8%, 13.7%, 13.9%, 11% and 7%, respectively. In 796 open-text responses, participants described challenges accessing HIV services due to clinics being overwhelmed and prioritising patients with COVID-19, resulting in young people being turned away. Some were afraid of contracting COVID-19 at or en route to clinics. Others were unable to reach clinics because of restricted transport or financial insecurity.
Discussion
Young people in Eastern Cape rely on local clinics for services, and large proportions of young males and females faced difficulties or fears accessing clinics during the COVID-19 lockdown. Clinics became overwhelmed or inaccessible, limiting young people’s access to sexual and reproductive health services. In high HIV risk contexts, prevention services and tools must be more accessible to young people, outside of clinics and within the communities and spaces that young people can access without fear or cost.
Keywords: Adolescent Health, COVID-19, Health services research, HIV
WHAT IS ALREADY KNOWN ON THIS TOPIC
Young people face significant barriers accessing sexual health services in South Africa, but we are still discovering how COVID-19 further affected young people’s access to service and the long-term ramifications of service disruptions. Understanding young people’s experiences accessing services during the pandemic is needed to make health systems more accessible and resilient.
WHAT THIS STUDY ADDS
Through a remote online questionnaire, young people in South Africa shared their experiences with struggling to access sexual health services due to overwhelmed clinics during the pandemic. They described the wide-ranging barriers they encounter while trying to access services, including limited transport, income loss, lockdown regulations and fear of contracting COVID-19. Without being able to access their services through clinics, young people had very few alternatives of where they could receive affordable services.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The barriers and experiences young people present support the need for sexual and reproductive health services to become more reliable and accessible to young people by providing a variety of affordable services outside of clinics and within the communities.
Background
On 23 March 2020, the South African government announced a nationwide ‘lockdown’ to control the spread of the first wave of the novel coronavirus (SARS-CoV-2). The strictest levels of lockdown, from March to July 2020, restricted people to stay at home unless accessing essential services. In government-issued guidance, sexual and reproductive health (SRH) services were included in the definition of ‘essential’ medical services. However, there were reports of confusion and misinterpretation of what were considered ‘essential’ services within communities and among healthcare professionals, resulting in people feeling unable to seek services or sometimes being turned away at clinics.1 Emerging evidence has shown that the COVID-19 epidemic had a significant impact on health services including tuberculosis (TB), maternal and child health and SRH services, including HIV services, due to the diversion of key resources to address COVID-19 and lockdowns that deterred people from seeking services.2–7 Some of the consequences of these disruptions resulted in increases in neonatal mortality, reduced access to contraception and a decline in child immunisations, TB and HIV-testing and antiretroviral treatment (ART) initiation.2–5 7 8
South Africans rely on SRH services mostly offered in local clinics to access HIV medication, testing and prevention, contraception, treatment of sexually transmitted infections (STIs), abortion and antenatal services. Even short disruptions to these services could have significant impacts including unplanned pregnancy, STI and HIV transmission, or HIV treatment interruptions. SRH services are particularly important in South Africa, the country with the largest HIV epidemic in the world. With over 7.8 million people living with HIV, South Africa accounts for 21% of the global HIV burden and 14% of new HIV infections.9 10 The South African government and non-governmental organisations have invested substantial funds into HIV education and testing, antiretroviral therapy and pre-exposure prophylaxis (PrEP) while implementing universal test and treat.11
For 15–24 year olds, who constitute roughly 16% of the population in South Africa, access to SRH services is essential to live healthy and productive lives.12 As young people begin to engage in sexual relationships so too begins their need for HIV services including testing, treatment and prevention. The risk for acquiring HIV accelerates quickly from adolescence among females and slightly later among young men.13 14 The 2017 South African National household-based HIV Prevalence, Incidence, Behaviour and Communication Survey estimated HIV incidence at 1.51% per year among those aged 15–24 years, higher than any other age group with young women baring significantly more of the burden.15 Young people also depend on SRH services for diagnosis of STI and bacterial vaginosis, which are highly prevalent in South Africa and associated with HIV and poor reproductive and sexual health.16 17 Young women rely on contraception services to prevent unplanned pregnancy and antenatal care if they become pregnant.18 The estimated pregnancy rate among women aged 15–24 years in South Africa is around 16%–22%.19 Despite their need and desire to seek SRH services, many young people avoid healthcare services because of real and perceived barriers to care including stigma, cost and healthcare worker judgement, and loss of privacy.20–26
This study investigates the impact of the COVID-19 pandemic and resulting government restrictions on young people’s access to SRH services in Eastern Cape, South Africa. In this high-risk context, understanding whether and how services are disrupted can help to ensure that ‘essential’ SRH and HIV services are resilient and accessible to young people.
Methods
We collected and analysed data from a web-based questionnaire launched online from September to December 2020. Questions about service disruption during COVID-19 were imbedded within a questionnaire designed for the evaluation of a mass media campaign that aimed to improve HIV outcomes among young people in the Eastern Cape. More information about the evaluation has been published elsewhere.27 The HIV prevalence in Eastern Cape province of South Africa has been estimated at 15.3% among people of all ages.28 The questionnaire was promoted through targeted advertisements to 15–24 year-olds in Mthatha, Eastern Cape, South Africa, through social media platforms, primarily Facebook. The questionnaire was also promoted in collaboration with local schools, universities, communities and clinics using their Facebook pages and WhatsApp groups. It was available on an internet data-free website, through a reverse-charging arrangement with the service provider. Instead of the participant paying to access the site with their personal internet data, the reverse charging website billed the research team. Those who completed the questionnaire received telephone airtime credit of ZAR50. The only identifying information that was captured in the questionnaire was participants’ telephone numbers. Besides telephone numbers, the self-administered questionnaire was anonymised with no name or other personal identifying information requested, and no IP address was captured. To reduce likely duplicate questionnaires, participants could only complete one questionnaire per phone number. Additionally, all questionnaires went through a screening process to identify questionnaires with the exact same answers. The questionnaire was offered in both English and isiXhosa and took 30 min to complete. Four young people who spoke both isiXhosa and English reviewed the online questionnaire and recruitment advertisements. Due to COVID-19 restrictions and the desire to capture the real-time experiences of young people, there was little time or opportunity to safely involve the public within the design of this research.
The questionnaire included questions to assess whether and how the COVID-19 pandemic and related restrictions had affected young people’s access to HIV and SRH services. Specifically, participants were asked ‘Since the COVID-19 pandemic caused by coronavirus began, have you experienced more difficulty getting the following services?’ for HIV testing services, HIV self-testing, condoms, ART or PrEP for HIV, contraception, antenatal care and domestic violence services. Descriptive statistics using frequencies and proportions were used to summarise responses, overall and by gender and age. Participants were asked an open-ended question, ‘How has the COVID-19 pandemic affected your access to these health services?’. The text responses from the open-ended questions were imported to NVivo 12 software and were analysed using thematic analysis.29 We familiarised ourselves with the data by reading all responses and noting emerging trends that appeared in the text. Data were collated into codes and as patterns emerged, codes were grouped into overarching themes. All themes were reviewed and defined, and illustrative quotes were selected to show evidence of themes within the data. Once thematic analysis was complete, we created a visual word cloud using NVivo software to identify key words and phrases based on the frequency in which they appeared in the open-ended responses. The word cloud included all words that were three or more characters. The size of the words represents the frequency in which the word appeared (ie, the larger the word the greater its frequency). The word cloud provided a visual illustration of the patterns of responses that had appeared in the open-ended text. By comparing the patterns that emerged in the thematic analysis to the patterns that emerged from the frequency word cloud, we were able to validate the findings of the thematic analysis.
Results
A total of 4145 records of the questionnaire were created, while the questionnaire was live online. Records without full consent (n=407) or gender (n=144), or which were likely duplicates (n=163) were removed leaving 3431 (83%) records for analysis. The majority of respondents resided in the city of Mthatha (72%) or elsewhere in Eastern Cape province (11%) and 16% lived in other provinces of South Africa. Respondents predominantly spoke IsiXhosa at home (80%), were female (59%) and aged 20–24 years (69% compared with 31% aged 15–19 years). Most respondents (83%) were enrolled in education, including 34% in university, 28% in technical/vocational college and 21% in primary or secondary school. Of those who were not full-time students, 10.4% reported being unemployed, while 3.1% reported employment. Many respondents experienced food insecurity with about 40% going to bed hungry at least ‘sometimes’ in the past month.
Of 3431 respondents, the proportions reporting ‘more difficulty’ accessing HIV testing services, HIV self-screening kits, PrEP and ART since the COVID-19 pandemic were 16.8%, 13.7%, 11% and 7%, respectively, with no differences by gender (table 1). A percentage of 13.9 of all participants (females and males) experienced greater difficulty accessing condoms (table 2). About 7% of both females and males reported more difficulty accessing domestic violence services. Difficulty accessing contraception, including barrier methods and hormonal methods, was reportedly greater among females (15.3%) than males (7.1%), and 6.8% of female respondents reported difficulty accessing antenatal care since the pandemic (table 2). There were no differences in antenatal care disruptions by age group, although the question was less applicable and data more likely to be missing among the younger group (15–19 years) compared with the older (20–24 years).
Table 1.
Reported difficulty accessing HIV services by gender
| Since the COVID-19 pandemic caused by coronavirus began, have you experienced more difficulty getting the following services? | Male | Female | Transgender | Prefer not to say | Total | |||||
| N | % | N | % | N | % | N | % | N | % | |
| HIV testing services? | ||||||||||
| No | 687 | 52.2 | 1034 | 51.2 | 13 | 61.9 | 20 | 27.4 | 1754 | 51.1 |
| Yes | 217 | 16.5 | 353 | 17.5 | 2 | 9.5 | 3 | 4.1 | 575 | 16.8 |
| Does not apply to me | 88 | 6.7 | 140 | 6.9 | 1 | 4.8 | 3 | 4.1 | 232 | 6.8 |
| Do not know | 159 | 12.1 | 208 | 10.3 | 2 | 9.5 | 1 | 1.4 | 370 | 10.8 |
| Prefer not to say | 21 | 1.6 | 14 | 0.7 | 2 | 9.5 | 42 | 57.5 | 79 | 2.3 |
| Missing/no response | 145 | 11 | 271 | 13.4 | 1 | 4.8 | 4 | 5.5 | 421 | 12.3 |
| Total | 1317 | 100 | 2020 | 100 | 21 | 100 | 73 | 100 | 3431 | 100 |
| HIV self-screening kits? | ||||||||||
| No | 680 | 51.6 | 1024 | 50.7 | 13 | 61.9 | 16 | 21.9 | 1733 | 50.5 |
| Yes | 180 | 13.7 | 286 | 14.2 | 2 | 9.5 | 3 | 4.1 | 471 | 13.7 |
| Does not apply to me | 104 | 7.9 | 186 | 9.2 | 1 | 4.8 | 4 | 5.5 | 295 | 8.6 |
| Do not know | 182 | 13.8 | 231 | 11.4 | 1 | 4.8 | 2 | 2.7 | 416 | 12.1 |
| Prefer not to say | 26 | 2 | 21 | 1 | 3 | 14.3 | 44 | 60.3 | 94 | 2.7 |
| Missing/no response | 145 | 11 | 272 | 13.5 | 1 | 4.8 | 4 | 5.5 | 422 | 12.3 |
| Total | 1317 | 100 | 2020 | 100 | 21 | 100 | 73 | 100 | 3431 | 100 |
| PrEP? | ||||||||||
| No | 651 | 49.4 | 990 | 49 | 11 | 52.4 | 18 | 24.7 | 1670 | 48.7 |
| Yes | 140 | 10.6 | 222 | 11 | 1 | 4.8 | 2 | 2.7 | 365 | 10.6 |
| Does not apply to me | 148 | 11.2 | 261 | 12.9 | 3 | 14.3 | 4 | 5.5 | 416 | 12.1 |
| Do not know | 207 | 15.7 | 257 | 12.7 | 2 | 9.5 | 3 | 4.1 | 469 | 13.7 |
| Prefer not to say | 26 | 2 | 18 | 0.9 | 3 | 14.3 | 42 | 57.5 | 89 | 2.6 |
| Missing/no response | 145 | 11 | 272 | 13.5 | 1 | 4.8 | 4 | 5.5 | 422 | 12.3 |
| Total | 1317 | 100 | 2020 | 100 | 21 | 100 | 73 | 100 | 3431 | 100 |
| Antiretroviral treatment for HIV? | ||||||||||
| No | 655 | 49.7 | 1006 | 49.8 | 10 | 47.6 | 15 | 20.5 | 1686 | 49.1 |
| Yes | 90 | 6.8 | 134 | 6.6 | 1 | 4.8 | 1 | 1.4 | 226 | 6.6 |
| Does not apply to me | 208 | 15.8 | 350 | 17.3 | 4 | 19 | 6 | 8.2 | 568 | 16.6 |
| Do not know | 196 | 14.9 | 236 | 11.7 | 2 | 9.5 | 3 | 4.1 | 437 | 12.7 |
| Prefer not to say | 23 | 1.7 | 22 | 1.1 | 3 | 14.3 | 44 | 60.3 | 92 | 2.7 |
| Missing/no response | 145 | 11 | 272 | 13.5 | 1 | 4.8 | 4 | 5.5 | 422 | 12.3 |
| Total | 1317 | 100 | 2020 | 100 | 21 | 100 | 73 | 100 | 3431 | 100 |
PrEP, pre-exposure prophylaxis.
Table 2.
Reported difficulty accessing sexual and reproductive health services by gender
| Since the COVID-19 pandemic caused by coronavirus began, have you experienced more difficulty getting the following services? | Male | Female | Transgender | Prefer not to say | Total | |||||
| N | % | N | % | N | % | N | % | N | % | |
| Condoms? | ||||||||||
| No | 770 | 58.5 | 1126 | 55.7 | 14 | 66.7 | 22 | 30.1 | 1932 | 56.3 |
| Yes | 200 | 15.2 | 275 | 13.6 | 1 | 4.8 | 2 | 2.7 | 478 | 13.9 |
| Does not apply to me | 40 | 3 | 144 | 7.1 | 1 | 4.8 | 2 | 2.7 | 187 | 5.5 |
| Do not know | 146 | 11.1 | 193 | 9.6 | 1 | 4.8 | 2 | 2.7 | 342 | 10 |
| Prefer not to say | 16 | 1.2 | 9 | 0.4 | 3 | 14.3 | 41 | 56.2 | 69 | 2 |
| Missing/no response | 145 | 11 | 273 | 13.5 | 1 | 4.8 | 4 | 5.5 | 423 | 12.3 |
| Total | 1317 | 100 | 2020 | 100 | 21 | 100 | 73 | 100 | 3431 | 100 |
| Contraception? | ||||||||||
| No | 679 | 51.6 | 1054 | 52.2 | 9 | 42.9 | 17 | 23.3 | 1759 | 51.3 |
| Yes | 94 | 7.1 | 310 | 15.3 | 3 | 14.3 | 1 | 1.4 | 408 | 11.9 |
| Does not apply to me | 174 | 13.2 | 171 | 8.5 | 3 | 14.3 | 5 | 6.8 | 353 | 10.3 |
| Do not know | 200 | 15.2 | 199 | 9.9 | 1 | 4.8 | 3 | 4.1 | 403 | 11.7 |
| Prefer not to say | 25 | 1.9 | 14 | 0.7 | 4 | 19 | 43 | 58.9 | 86 | 2.5 |
| Missing/no response | 145 | 11 | 272 | 13.5 | 1 | 4.8 | 4 | 5.5 | 422 | 12.3 |
| Total | 1317 | 100 | 2020 | 100 | 21 | 100 | 73 | 100 | 3431 | 100 |
| Antenatal care? (females only) | ||||||||||
| No | 0 | 0 | 986 | 48.8 | 0 | 0 | 0 | 0 | 986 | 28.7 |
| Yes | 0 | 0 | 137 | 6.8 | 0 | 0 | 0 | 0 | 137 | 4 |
| Does not apply to me | 0 | 0 | 331 | 16.4 | 0 | 0 | 0 | 0 | 331 | 9.6 |
| Do not know | 0 | 0 | 265 | 13.1 | 0 | 0 | 0 | 0 | 265 | 7.7 |
| Prefer not to say | 0 | 0 | 28 | 1.4 | 0 | 0 | 0 | 0 | 28 | 0.8 |
| Missing/no response | 1317 | 100 | 273 | 13.5 | 21 | 100 | 73 | 100 | 1684 | 49.1 |
| Total | 1317 | 100 | 2020 | 100 | 21 | 100 | 73 | 100 | 3431 | 100 |
| Domestic violence services? | ||||||||||
| No | 722 | 54.8 | 1063 | 52.6 | 9 | 42.9 | 18 | 24.7 | 1812 | 52.8 |
| Yes | 101 | 7.7 | 143 | 7.1 | 2 | 9.5 | 1 | 1.4 | 247 | 7.2 |
| Does not apply to me | 139 | 10.6 | 287 | 14.2 | 4 | 19 | 4 | 5.5 | 434 | 12.6 |
| Do not know | 184 | 14 | 226 | 11.2 | 1 | 4.8 | 3 | 4.1 | 414 | 12.1 |
| Prefer not to say | 26 | 2 | 25 | 1.2 | 4 | 19 | 43 | 58.9 | 98 | 2.9 |
| Missing/no response | 145 | 11 | 276 | 13.7 | 1 | 4.8 | 4 | 5.5 | 426 | 12.4 |
| Total | 1317 | 100 | 2020 | 100 | 21 | 100 | 73 | 100 | 3431 | 100 |
Seven hundred and ninety-six participants wrote an open-text response to explain how the COVID-19 pandemic affected their access to the previously mentioned HIV, and SRH services. The word cloud illustrated in figure 1 highlights the frequency in which young people reported that ‘clinics’ had been ‘affected’. Words such as time, closed, queue, long and numbers described the ways in which COVID-19 had overwhelmed the clinics creating long wait times and closures. Thematic analysis revealed details about how services were affected. Due to COVID-19, clinics were often closed or running a limited service because clinical staff had contracted COVID-19.
Figure 1.
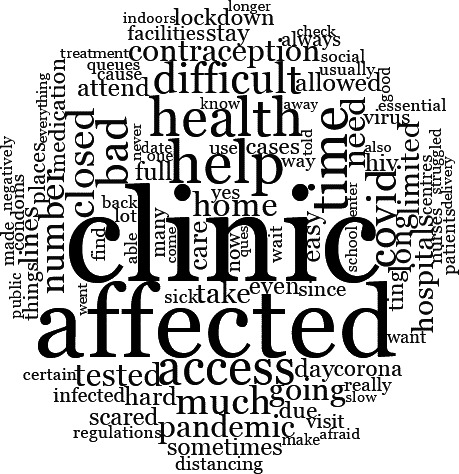
An illustrative ‘word cloud’ that captures the frequency at which participants used words to describe how they experienced more difficulty receiving SRH services since the COVID-19 pandemic.
One of the staff members in the clinic was tested positive for coronavirus. So, the facility was closed for fumigation of the facility.
Some respondents described clinics being closed for up to 14 days after positive tests were detected among staff.
I haven't gone for them since the pandemic. It affected us because when they have a case they close the clinics for 14 days, that time we could not go to clinic to get condoms and contraception.
Young people reported that many clinics were only attending to patients with COVID-19 and all other services were suspended or restricted to specific days and hours.
Clinics were mostly centred around COVID-19 and offered no contraception treatment and were sometimes not accessible.
It affected my access big time because I couldn’t go to hospitals or clinic when I was sick because they were full of people who were infected by the virus.
Hospitals have focused more on cases concerning the Coronavirus and neglecting others as if they don’t matter.
Overwhelmed clinics with limited services and an influx of patients with COVID-19 meant that respondents seeking SRH services were waiting in long lines for hours and sometimes were told to come back the next day.
Clinics are always full, it’s not easy getting help because you'll be on the queue for the whole day, then around the time that they close the nurses tell you to come back the next day while you didn't even get help.
Most of these services I usually get them at the clinic. But now due to this pandemic, clinics were being closed often, and even when they were open there would be a huge number of people visiting, increasing the rate of being infected.
I had to book an appointment to go to the clinic whereas I needed help right away. Sometimes they'd tell us to come back tomorrow although we had an appointment.
Respondents also explained that reporting cases of gender-based violence was difficult with police services reportedly overwhelmed with enforcing COVID-19 rules and understaffing due to COVID-19 infections among police officers.
Reporting GBV has been difficult because police were busy arresting people that smoke and drink alcohol who are not violating anyone.
Due to increased numbers of cases and the police taking their time to respond to specific cases has made it very hard for us to follow up and report cases. Also, some police stations close due to someone having tested positive in the station.
Key themes that we identified during the thematic analysis demonstrate that lockdown rules, prohibiting people from leaving their homes unless accessing essential services, created barriers to SRH services. Some respondents reported that they did not seek SRH services because they were following lockdown guidance to stay home and believed chemists and pharmacies would be closed.
Because of the lockdown most chemists and places to get screening kits were closed. Most hospitals were filled with people with COVID-19 so I couldn't risk going there. And because of this pandemic we were given curfews.
It has affected me because my mobility is limited and these services are often found in certain health institutions so I have to move from home to get them and during this COVID-19 we are encouraged not to go out unless it’s necessary.
Transport was also a large issue for young people as local taxi services, a primary mode of transport, were restricted in the lockdown. This made getting to the clinics to access essential services, like HIV medication, difficult.
It had a very big impact in such a way that it made things very difficult for me because I couldn't come into contact to people I depend to get money for transport to travel from home to where my clinic is located. So I even defaulted for about a month before I get my medication but at least now I'm getting my meds and taking them properly.
It has affected me drastically because these services are centralized in a town that is located far away from my area so I couldn't access them freely due to COVID-19 regulations.
I was affected because there was a limit in everything so I had to make sure I wake up early & the taxis were also a problem because of the lockdown conditions.
Respondents also explained that the lockdowns had affected their income sources, either through job loss or becoming isolated from family members who usually provided them with financial support. Financial losses meant respondents could not afford transport to clinics. Respondents also described the financial stresses of having to pay private clinics and pharmacies for SRH services like condoms, contraception and HIV tests that are normally free at public clinics.
I had to go buy lovers plus+ condoms in the shops. It was hard because I did not want to be in the shops in COVID times…and I had to steal some money from my mom’s wallet 2 get cash 4 the condom… I did not want corona and a baby. tough times but yah, neh…I made it happen.
When we needed some health services or medication we'd be told that the pharmacy is closed and we had to buy the medicine from private pharmacies, in some cases I didn't have money.
The word cloud captures that young people were also ‘afraid and scared’ of becoming ‘infected’ that motivated them to follow lockdown regulations and deterred them from travelling or visiting clinics where they believed they might contract the virus.
I was scared of being in a place where there is a huge number of people because of fear that I could get infected.
I am now afraid to go to the clinic because I know there can be infected people and I might get infected.
I usually go get self-screening kits but during this pandemic I couldn’t because I'm kind of scared of Coronavirus.
Discussion
Through their experiences and perspectives, young people offered explanations for why the COVID-19 and lockdown measures made it more difficult than usual for some young people in the Eastern Cape to access SRH services. They detailed accounts of clinic disruptions due to the influx of patients, restricted services and understaffing because of COVID-19 infections that resulted in long lines and young people being turned away from clinics. They also explained the difficulties in getting to the clinics due to limited transport options that had been reduced during lockdowns. COVID-19 impacted respondents’ care-seeking behaviour as they feared contracting the virus and stayed at home due to the lockdown measure regulations. Loss of income due to the pandemic and being unable to receive free clinic services quickly made SHR services inaccessible to some young people. There were few reliable or affordable back up option to clinic-based services meaning when clinics were inaccessible, young people often were unable to get the services they needed from other places.
Similar worrying trends about COVID-19’s negative impact on SRH, including young people’s and adolescents’ health, have been reported in the literature. A study of PrEP in South Africa reported that South African adolescent girls and young women substantially decreased their visits for PrEP during the COVID-19 epidemic, while rates of new HIV infection, STIs and pregnancy increased.30 In the Gauteng region of South Africa, there was a decline in family planning and termination of pregnancy services as well as a shift away from long-acting reversable contraception.31 Another study from the Eastern Cape reported a reduction in the availability of STI services resulting from the COVID-19 epidemic potentially increasing the burden of untreated STIs in the community.32 Gender-based violence prevention and response services in South Africa were impacted by the COVID-19 pandemic due to government restrictions and the failure of government to identify early on if GBV services were essential.33 34Facilities in countries across Africa with similar lockdowns to South Africa saw a drop in antenatal attendances in the first months of the pandemic.35 Data from a district health information system for KwaZulu-Natal provincial health services found an increase in neonatal mortality was linked to the disruption of health services and diversion of resources to COVID-19.5 Additionally, modelling in 2020 suggested that disruption due to COVID-19 of ART medication had a real risk of increasing mortality among at risk populations in sub-Saharan Africa.36
Those who responded to the question about how COVID-19 had affected health services primarily discussed how local government clinic services had been disrupted. In addition to the barriers created by COVID-19, literature that predates the COVID-19 pandemic reveals that young people in South Africa reported many barriers when accessing clinic-based services. Some of the reported barriers to services are long distances and travel times to clinics, limited and unaffordable transport options and inconvenient clinic hours.37 Young people also reported that they avoid services because of stigma and fear of judgement from staff.20–22 25 Reports such as these inspired the South African Department of Health to implement youth friendly services with a target to have 70% of healthcare facilities offer youth friendly services by 2012. Unfortunately, the reported provision of these services is far below the target, especially in rural areas.24–26 A 2018 study by Smith et al 38 concluded that young people in South Africa are put off by visits to local government clinics ‘which are stigmitising, time consuming, and unhelpful’. The long wait times and queues, as well as diversion of resources during COVID-19 likely made these experiences worse.
However, despite the barriers and short falls of the local government clinic, our findings show that very few participants sought health services from other outlets. Cost and travel expenses make it difficult for young people to access SRH services through models of care structures such as pharmacies and private doctors.23 No other models of care were mentioned in our findings. This study supports the need to ‘de-medicalise’ some HIV and SRH services to make services more resilient and accessible to young people. This includes the scale up other options for young people to access SRH services within the community or online. Providing various service models allows young people to choose the model of care that best fits their needs. This can also reduce the burden on clinics allowing them to provide quicker and better services. Other SRH models of care that have proven to be feasible and acceptable are community health worker programmes, school-based services, peer navigators and mobile health clinics; however, there has not been enough investment models of care.39–43
Telemedicine services similar to the initiatives that sprang up across the world during the pandemic to provide young people with remote and safe SRH services should be made available to digitally connected young people in South Africa,44 45 especially since South Africa has the highest number of mobile users in Africa.46 Additionally, existing online SRH social networks and forums can be harnessed to reach more young South Africans and link them to services.47 A narrative review found that telemedicine and mobile health (mhealth) interventions in South Africa that started in response to the COVID-19 pandemic showed that telemedicine and mhealth (defined as the use of mobile devices for medical and public health practice)48 can be an innovative approach to providing young adults with access to SRH treatment and information.46 However, issues with implementation and lack of funding show that there needs to be more investments in these areas for them to become reliable models of sexual and reproductive healthcare for young people in South Africa.
To reduce the risk of COVID-19 transmission, this study used only remote internet study methods. Since this questionnaire required a digital device and internet connectivity to access, it is likely that the sample is skewed towards young people who have better access to digital media. An effort was made to minimise the cost of participating in the questionnaire by making the internet questionnaire free to access and providing airtime vouchers to those who participated. However, it is likely that those who have completed the questionnaire had greater access to digital devices, reliable internet access and greater literacy. By result some of them most vulnerable, digitally unconnected young people might have been missed in this questionnaire.
Conclusion
Young people in the Eastern Cape of South Africa reported difficulties or fears accessing local clinics during the COVID-19 lockdown. Clinics became overwhelmed or inaccessible, limiting young people’s access to services for HIV prevention, contraception, antenatal care and gender-based violence. Young people appeared to have few alternative, affordable models of care for receiving HIV and SRH services. In high-risk contexts, prevention services and tools must be considered ‘essential’ and made more accessible to young people, outside of clinics and within the communities and online in spaces that young people can access without fear or cost.
Supplementary Material
Acknowledgments
The authors wish to thank all the young people who contributed their time to this study. We acknowledge the dedication of MTV Shuga peer educators in South Africa who assisted with recruitment.
Footnotes
CC and IB contributed equally.
Contributors: VB was responsible for the write up of this paper and the qualitative analysis for the open ended questions. IB, SM, SC and SS were responsible for the questionnaire design and quantitative analysis of the responses; CC, DO and DK were responsible for promoting the survey, recruiting participants and managing incoming data. GA, SP and YD were responsible for questions design and contributed to analysis team meetings. All authors contributed to the write up of the manuscript through reading draft copies and providing comments and edits. IB is responsible for the overall content as the guarantor.
Funding: This work was supported through a grant from Unitaid through a sub-contract from MTV Staying Alive Foundation to London School of Hygiene & Tropical Medicine, grant 1317919.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved byEthics was obtained from The Biomedical Research Ethics Committee at University of KwaZulu-Natal, London School of Hygiene & Tropical Medicine and the WHO. Participants gave informed consent to participate in the study before taking part.
References
- 1. Mbatha T. The dreadful effects of lockdown on access to sexual and reproductive health services [News Article], 2020. Spotlight. Available: https://www.spotlightnsp.co.za/2020/07/31/the-dreadful-effects-of-lockdown-on-access-to-sexual-and-reproductive-health-services/
- 2. Abdool Karim Q, Baxter C. COVID-19: impact on the HIV and tuberculosis response, service delivery, and research in South Africa. Curr HIV/AIDS Rep 2022;19:46–53. 10.1007/s11904-021-00588-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ahmed T, Rahman AE, Amole TG, et al. The effect of COVID-19 on maternal newborn and child health (MNCH) services in Bangladesh, Nigeria and South Africa: call for a contextualised pandemic response in LMICs. Int J Equity Health 2021;20:77. 10.1186/s12939-021-01414-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dorward J, Khubone T, Gate K, et al. The impact of the COVID-19 lockdown on HIV care in 65 South African primary care clinics: an interrupted time series analysis. Lancet HIV 2021;8:e158–65. 10.1016/S2352-3018(20)30359-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jensen C, McKerrow NH. Child health services during a COVID-19 outbreak in KwaZulu-Natal Province, South Africa. S Afr Med J 2020;0:13185. [PubMed] [Google Scholar]
- 6. Staden Q, Laurenzi CA, Toska E. Two years after lockdown: reviewing the effects of COVID‐19 on health services and support for adolescents living with HIV in South Africa. J Int AIDS Soc 2022;25:e25904. 10.1002/jia2.25904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bolarinwa OA. Factors associated with access to condoms and sources of condoms during the COVID-19 pandemic in South Africa. Arch Public Health 2021;79:186. 10.1186/s13690-021-00701-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pillay Y, Pienaar S, Barron P, et al. Impact of COVID-19 on routine primary healthcare services in South Africa. S Afr Med J 2021;111:714–9. 10.7196/SAMJ.2021.v111i8.15786 [DOI] [PubMed] [Google Scholar]
- 9. Myburgh H, Reynolds L, Hoddinott G, et al. Implementing 'universal' access to antiretroviral treatment in South Africa: a scoping review on research priorities. Health Policy Plan 2021;36:923–38. 10.1093/heapol/czaa094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. DATA U . Joint United nations programme on HIV/AIDS; 2021. [PubMed]
- 11. Hansoti B, Mwinnyaa G, Hahn E, et al. Targeting the HIV epidemic in South Africa: the need for testing and linkage to care in emergency departments. EClinicalMedicine 2019;15:14–22. 10.1016/j.eclinm.2019.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. South Africa Demographic and Health Survey . National department of health (NDoH), statistics South Africa (Stats SA), South African medical Research Council (SAMRC), and ICF; 2016.
- 13. UNAIDS . Miles to go: closing gaps, breaking barriers, righting injustices; 2018.
- 14. Birdthistle I, Kwaro D, Shahmanesh M, et al. Evaluating the impact of dreams on HIV incidence among adolescent girls and young women: a population-based cohort study in Kenya and South Africa. PLoS Med 2021;18:e1003837. 10.1371/journal.pmed.1003837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kunnuji MON, Robinson RS, Shawar YR, et al. Variable implementation of sexuality education in three Nigerian states. Stud Fam Plann 2017;48:359–76. 10.1111/sifp.12043 [DOI] [PubMed] [Google Scholar]
- 16. Atashili J, Poole C, Ndumbe PM, et al. Bacterial vaginosis and HIV acquisition: a meta-analysis of published studies. AIDS 2008;22:1493–501. 10.1097/QAD.0b013e3283021a37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Francis SC, Mthiyane TN, Baisley K, et al. Prevalence of sexually transmitted infections among young people in South Africa: a nested survey in a health and demographic surveillance site. PLoS Med 2018;15:e1002512. 10.1371/journal.pmed.1002512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pleaner M, Fipaza Z, Mabetha K, et al. Uptake of contraception among adolescent girls and young women PrEP clients: Leveraging the opportunity to strengthen HIV and sexual and reproductive health integration. Front Reprod Health 2021;3:684114. 10.3389/frph.2021.684114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yah CS, Ndlovu S, Kutywayo A, et al. The prevalence of pregnancy among adolescent girls and young women across the Southern African development community economic hub: a systematic review and meta-analysis. Health Promot Perspect 2020;10:325–37. 10.34172/hpp.2020.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Müller A, Röhrs S, Hoffman-Wanderer Y, et al. “You have to make a judgment call”. – Morals, judgments and the provision of quality sexual and reproductive health services for adolescents in South Africa. Soc Sci Med 2016;148:71–8. 10.1016/j.socscimed.2015.11.048 [DOI] [PubMed] [Google Scholar]
- 21. Holt K, Lince N, Hargey A, et al. Assessment of service availability and health care workers' opinions about young women's sexual and reproductive health in Soweto, South Africa. Afr J Reprod Health 2012;16:283–94. [PubMed] [Google Scholar]
- 22. Lesko N. Talking about sex: the discourses of loveLife peer educators in South Africa. Int J Incl Educ 2007;11:519–33. 10.1080/13603110701391501 [DOI] [Google Scholar]
- 23. Smith P, Tolla T, Marcus R, et al. Mobile sexual health services for adolescents: investigating the acceptability of youth-directed mobile clinic services in Cape town, South Africa. BMC Health Serv Res 2019;19:584. 10.1186/s12913-019-4423-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. James S, Pisa PT, Imrie J, et al. Assessment of adolescent and youth friendly services in primary healthcare facilities in two provinces in South Africa. BMC Health Serv Res 2018;18:809. 10.1186/s12913-018-3623-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Geary RS, Gómez-Olivé FX, Kahn K, et al. Barriers to and facilitators of the provision of a youth-friendly health services programme in rural South Africa. BMC Health Serv Res 2014;14:259. 10.1186/1472-6963-14-259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mayeye FB, Lewis HA, Oguntibeju OO. An assessment of adolescent satisfaction with reproductive primary healthcare services in the Eastern Cape Province, South Africa. West Indian Med J 2010;59:274–9. [PubMed] [Google Scholar]
- 27. Birdthistle I, Mulwa S, Sarrassat S, et al. Effects of a multimedia campaign on HIV self-testing and PrEP outcomes among young people in South Africa: a mixed-methods impact evaluation of 'MTV Shuga Down South'. BMJ Glob Health 2022;7:e007641. 10.1136/bmjgh-2021-007641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Health Services Research Centre . South African national HIV prevalence, incidence, behaviour and communication survey, 2017. [Google Scholar]
- 29. Clarke V, Braun V, Hayfield N. Thematic analysis, 2015: 248. [Google Scholar]
- 30. Mendelsohn AS, Gill K, Marcus R, et al. Sexual reproductive healthcare utilisation and HIV testing in an integrated adolescent youth centre clinic in Cape Town, South Africa. South Afr J HIV Med 2018;19:826. 10.4102/sajhivmed.v19i1.826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Adelekan T, Mihretu B, Mapanga W, et al. Early effects of the COVID-19 pandemic on family planning utilisation and termination of pregnancy services in Gauteng, South Africa: March–April 2020. Wits J Clin Med 2020;2:91–52. 10.18772/26180197.2020.v2n2a7 [DOI] [Google Scholar]
- 32. Maithufi R, Pinini Z, Chidarikire T. O04.3 the impact of the COVID-19 pandemic on STI services in the Eastern Cape Province of South Africa. Sexually Transmitted Infections 2021;97:A23–4. 10.1136/sextrans-2021-sti.70 [DOI] [Google Scholar]
- 33. Roy CM, Bukuluki P, Casey SE, et al. Impact of COVID-19 on gender-based violence prevention and response services in Kenya, Uganda, Nigeria, and South Africa: a cross-sectional survey. Front Glob Womens Health 2021;2:780771. 10.3389/fgwh.2021.780771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mutambara VM, Crankshaw TL, Freedman J. Assessing the impacts of COVID-19 on women refugees in South Africa. J Refug Stud 2022;35:704–21. 10.1093/jrs/feab044 [DOI] [Google Scholar]
- 35. Burt JF, Ouma J, Lubyayi L, et al. Indirect effects of COVID-19 on maternal, neonatal, child, sexual and reproductive health services in Kampala, Uganda. BMJ Global Health 2021;6:e006102. 10.1136/bmjgh-2021-006102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jewell BL, Mudimu E, Stover J, et al. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models. The Lancet HIV 2020;7:e629–40. 10.1016/S2352-3018(20)30211-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mokomane Z, Mokhele T, Mathews C, et al. Availability and accessibility of public health services for adolescents and young people in South Africa. Child Youth Serv Rev 2017;74:125–32. 10.1016/j.childyouth.2017.02.001 [DOI] [Google Scholar]
- 38. Smith P, Marcus R, Bennie T, et al. What do South African adolescents want in a sexual health service? Evidence from the South African studies on HIV in adolescents (SASHA) project. S Afr Med J 2018;108:677–81. 10.7196/SAMJ.2018.v108i8.13013 [DOI] [PubMed] [Google Scholar]
- 39. Otiso L, McCollum R, Mireku M, et al. Decentralising and integrating HIV services in community-based health systems: a qualitative study of perceptions at macro, meso and micro levels of the health system. BMJ Glob Health 2017;2:e000107. 10.1136/bmjgh-2016-000107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schriver B, Meagley K, Norris S, et al. Young people’s perceptions of youth-oriented health services in urban Soweto, South Africa: a qualitative investigation. BMC Health Serv Res 2014;14:625. 10.1186/s12913-014-0625-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shahmanesh M, Okesola N, Chimbindi N, et al. Thetha Nami: participatory development of a peer-navigator intervention to deliver biosocial HIV prevention for adolescents and youth in rural South Africa. BMC Public Health 2021;21:1393. 10.1186/s12889-021-11399-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Maheswaran H, Thulare H, Stanistreet D, et al. Starting a home and mobile HIV testing service in a rural area of South Africa. J Acquir Immune Defic Syndr 2012;59:e43–6. 10.1097/QAI.0b013e3182414ed7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Liang TS, Erbelding E, Jacob CA, et al. Rapid HIV testing of clients of a mobile STD/HIV clinic. AIDS Patient Care STDS 2005;19:253–7. 10.1089/apc.2005.19.253 [DOI] [PubMed] [Google Scholar]
- 44. Dourado I, Magno L, Soares F, et al. Adapting to the COVID-19 pandemic: continuing HIV prevention services for adolescents through Telemonitoring, Brazil. AIDS Behav 2020;24:1994–9. 10.1007/s10461-020-02927-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Barney A, Buckelew S, Mesheriakova V, et al. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J Adolesc Health 2020;67:164–71. 10.1016/j.jadohealth.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Akintunde TY, Akintunde OD, Musa TH, et al. Expanding telemedicine to reduce the burden on the healthcare systems and poverty in Africa for a post-coronavirus disease 2019 (COVID-19) pandemic reformation. Global Health Journal 2021;5:128–34. 10.1016/j.glohj.2021.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Yamauchi EK. LoveLife, MYMsta, and mizz B: evaluating a mobile phone-based social network to prevent HIV among youth in South Africa. The University of North Carolina at Chapel Hill, 2010. [Google Scholar]
- 48. Global difusion of eHealth: making universal health coverage achievable . Report of the third global survey on ehealth. licence: CC BY-NC-SA 3.0 IGO. Geneva: World Health Organization; 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on reasonable request.


