Abstract
Objective
Undernutrition contributes to decreased physical and cognitive functional status, higher healthcare consumption, premature institutionalisation and increased mortality. So, the objective of this study was to determine the pooled prevalence and factors associated with undernutrition among older adults in Ethiopia.
Design
Systematic review and meta-analysis was used. Articles that presented original data on undernutrition using body mass index (BMI) were included. We made an inclusive literature search from PubMed, Medline and Google Scholar. The I2 test was used to examine the heterogeneity of the studies considered in this meta-analysis. Stata software V.14 and METANDI command were used.
Setting
Studies conducted in Ethiopia were included.
Participants
Eight independent studies were eligible and enrolled for final analysis.
Outcome
Prevalence and determinants of undernutrition. A selection of publications, data extraction and reported results for the review was designed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Results
A total of eight unique studies were enrolled for final analysis. The pooled prevalence of undernutrition was 20.53% (95% CI 17.39% to 23.67%). The study revealed that males had lesser odds of being undernutrition with AOR 0.17 (95% CI 0.15 to 0.20). Older adults in the age range of 65–74 years were less likely to be undernourished as compared with those whose age was above 85 years with Adjusted Odds Ratio (AOR) 022 (95% CI 0.22 to 0.25). Older adults who were depressed had higher odds of undernutrition as compared with their counterparts with AOR 1.27 (95% CI 1.19 to 1.37). However, older adults from households with poor wealth indexes were two times more likely to be undernourished as compared with those who were from rich households.
Conclusion
The burden of undernutrition in Ethiopia is significant. The limitation of the current study was that all included studies were observational, mainly cross-sectional.
Keywords: Nutrition, PUBLIC HEALTH, PREVENTIVE MEDICINE
Strengths and limitations of this study.
The study was registered in PROSPERO.
The quality of each original study was assessed using the Newcastle Ottawa Scale, a three-part approach, for observational studies quality assessment and the Grading of Recommendations, Assessment, Development, and Evaluations checklist.
Coming to the limitation only eight studies were eligible for the study.
The present systematic review was about observational studies, mainly cross-sectional.
From the total included studies, only a few studies evaluated place of residence, dietary diversity and meal frequency.
Introduction
According to a factsheet released by the WHO, around 12% of the global population (900 million people) was aged 60 years or over in 2015, with forecasts that this number will nearly double to 22% (2 billion people) by 2050.1
Chronic diseases and disabilities are becoming a public health challenge as the world’s population ages, particularly in developing nations where the healthcare system is underdeveloped and resources are scarce.2 Furthermore, the older adult population in developing countries is expanding at a faster rate than in developed countries.3 This rapid demographic shift leaves these countries with insufficient time to construct their health, economic and social infrastructures to deal with the ageing population. Another issue is that in developing countries, population ageing is accompanied by persistent poverty.4
Healthy diets and exercise are frequently emphasised in nutrition to reduce the chance of acquiring lifestyle diseases such as cancer, diabetes and cardiovascular disease. However, as people get older, their nutritional objectives shift to fulfilling greater nutrient needs while consuming less energy and preventing lean muscle loss.5 6
In older adults, undernutrition is a common and dangerous condition. Undernutrition contributes significantly to morbidity and mortality in older adults today, without a doubt.7
The number of existing geriatric disorders had a positive association with the probability of undernutrition. Poor nutritional status was linked to depression, dementia, functional dependency and various comorbidities.8 Undernutrition and poor nutritional status in the older population are major concerns. Undernutrition and accidental weight loss contribute to health decline, decreased physical and cognitive functional status, higher healthcare consumption, premature institutionalisation and increased mortality.9
Weight loss in older persons is frequently accompanied by a decrease in muscle mass, which can harm functional status. The advancement to undernutrition is mostly treacherous and often unnoticed. Undernutrition in older people is linked to problems and early death.10 On the other side, they are overweight and obese due to a lack of mobility and a sedentary lifestyle.11
In Ethiopia, there is an underlying respect for older people in Ethiopia where family and community support systems are relatively strong. However, a significant number of older people have no family and community support, mainly due to the death of relatives or separation caused by famine, war, disease and displacement and the weakening of family and community support structures.12
In 1973, during the Imperial regime, almost 3 million Ethiopians were affected by food shortages, and total excess mortality in the country hovered at around 250 000.13 Elderlies of the current study were below the age of 15 years during that time. Even though they were survivors of the famine, the famine may have a consequence to their current nutritional status during old age.
Undernutrition in older adults may be reduced if the overall prevalence and determinant factors were addressed. So, the objective of this study is to see the prevalence and determinants of undernutrition among older adults in Ethiopia. There are many original types of research on elderly undernutrition, and this systematic review and meta-analysis evaluates and summarises the findings of all relevant individual studies in Ethiopia on elderly malnutrition, thereby making the available evidence more accessible to decision makers.
Materials and methods
Study protocol registration
The protocol in this study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database and can be accessed with a protocol number CRD42021254805.
Search strategy
We made an inclusive literature search conducted from October 2021 to November 2021 from PubMed, Medline and Google Scholar, in parallel using search strings adapted to the requirements of each database. A selection of publications, data extraction and reported results for the review was designed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA guidelines. Throughout the comprehensive literature search, the following search terms were used: ‘Undernutrition OR Nutritional Deficiency OR Undernutrition OR malnourishment OR undernourishment OR cachexia OR Low BMI OR nutritional status OR starvation AND Aged OR Older adults OR older adults OR geriatrics OR advanced years AND Ethiopia’. Furthermore, we checked the reference lists of published studies to identify additional articles. The identification and selection of the papers in all the researched databases were made independently by three researchers (HY, MAZ and ATD), respecting the eligibility criteria and without the use of filters. Then, the duplications between the databases were eliminated. Next, a refinement was performed to select studies regarding the theme addressed, by reading the titles and abstracts. In the event of disagreement between the investigators, the study was re-evaluated, and the doubts obtained in the process of applying the eligibility criteria were discussed until a consensus was reached among the members.
Eligibility criteria
The eligibility criteria used were: articles that presented original data on prevalence and determinants of undernutrition using body mass index (BMI) <18.5 among older adults in Ethiopia. The study included all studies done so far in Ethiopia. All available and eligible studies were observational cross-sectional studies. The selected language of publication was English. We excluded studies that used secondary data, reviews of reviews and those studies that did not report the outcome of interest.
Selection and identification of studies
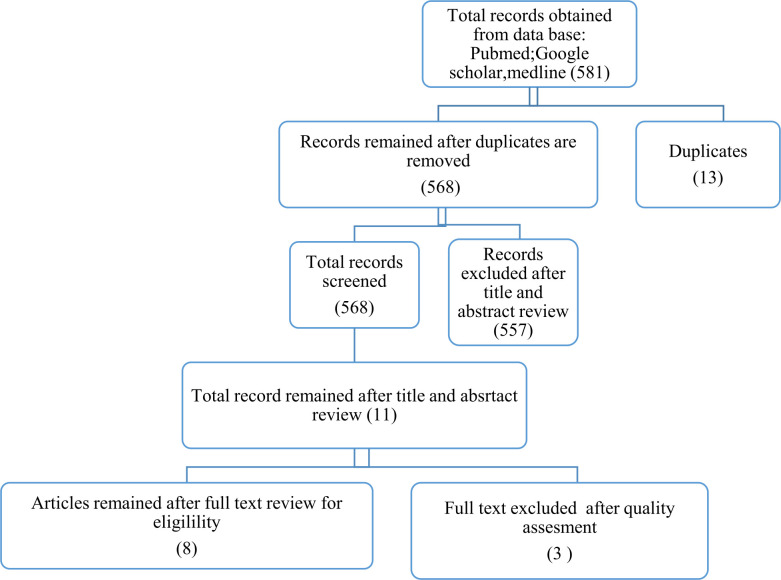
All studies identified through different databases were combined, exported and managed using COVIDENCE software. All duplicated studies were removed, and the full text of the articles was searched manually using Endnote software. A total of 581 studies were identified from the literature search. Of these studies, 13 articles of duplicate records were identified and removed. A total of 510 articles were excluded after reviewing the titles, and 47 articles were excluded after reviewing abstracts because they were irrelevant. After assessing the full texts of the remaining 11 articles were left, three additional articles were excluded because of the following: poor quality and articles do not report outcome interest. Therefore, a total of eight unique studies were eligible and enrolled for final analysis (figure 1).
Figure 1.
Flow diagram depicting the selection process for articles included in this review and meta-analysis.
The selected studies were: (1), Abate et al 2020 from Addis Ababa14; (2) Abdu et al, 2020 from Eastern Ethiopia15; (3) Legesse et al 2019 Aykel town, Ethiopia16; (4) Wassie et al 2014 Northwest Ethiopia,17; (5)Wondiye et al from Wolaita Sodo, Ethiopia,18; (6) Mezemir et al19 2020 from Debre Birhan Ethiopia; (7) Adhana et al 2019 from Debre Markos20; and (8) Yisak et al 2021 from South Gondar Zone, Ethiopia.21 A detailed description of selected studies is indicated in table 1.
Table 1.
Summary of included studies to assess the prevalence and associated factors of undernutrition among older adults in Ethiopia, 2021
| S.no | Author name | Study year | Study design | Region | Sample size | Response rate (%) | Prevalence (%) | Quality score |
| 1 | Abate et al | 2020 | CBCS | Addis Ababa | 682 | 97 | 26.6 | 8 |
| 2 | Abdu et al | 2019 | CBCS | Harari | 630 | 93.4 | 15.7 | 7 |
| 3 | Legesse M, Abebe Z, Woldie H | 2018 | CBCS | Amhara | 921 | 96.8 | 17.6 | 7 |
| 4 | Wassie et al | 2013 | CBCS | Amhara | 757 | 100 | 21.9 | 7 |
| 5 | Wondiye et al | 2017 | CBCS | SNNP | 578 | 95.8 | 17.1 | 8 |
| 6 | Mezemir et al | 2020 | CBCS | Amhara | 347 | 98.3 | 21.2 | 6 |
| 7 | ZK Adhana | 2015 | CBCS | Amhara | 423 | 100 | 22.7 | 8 |
| 8 | Hiwot Yisak et al | 2020 | CBCS | Amhara | 300 | 96.6 | 27.6 | 6 |
prevalences of under nutrition
CBCS, community-based cross-sectional study; SNNP, Southern Nations Nationalities and People.
Evaluation of study quality
The Grading of Recommendations, Assessment, Development, and Evaluations method was used to evaluate the quality of studies included in the review. This instrument assesses factors that may diminish (risk of bias, inconsistency of results, inaccuracy, indirect evidence and publication bias) or increase (magnitude of effect and decrease of confounders). Since all of the reviewed articles are observational studies, the score starts with low quality (2 points). Then, for each present factor that can decrease the quality of the evidence, it is deducted from 1 to 2 points, according to the magnitude of the factor. The presence of factors that increase the quality of evidence adds an initial score of 1–2 points. After the final sum, the studies were classified as low (<2 points) and good quality (>2 points); we did not identify publication bias and selective reporting of studies. Studies with >2 points were included in the review.
The quality of each original study was assessed using the Newcastle Ottawa Scale, a three-part approach, for observational studies quality assessment.22 The tool is made up of three main components. The methodological quality of each article was the focus of the first component, which was rated on a scale of one to five stars. The study’s comparability is evaluated in the second part, which has a possible two-star rating. The results and statistical analysis of each original research were the emphases of the third component, which was graded out of three stars. The two reviewers’ disagreements were resolved through discussion. High-quality articles were those rated on a scale of 6 out of 10.
Statistical analysis
By dividing the number of positive subjects in all studies by the total number of study participants, the prevalence of undernutrition was estimated. The I2 test was used to examine the heterogeneity of the studies considered in this meta-analysis. The degree of diversity in each research is referred to as heterogeneity. Based on the I2 value less than 50%, 50%–75% and above >75%, the studies’ heterogeneity was characterised as low, moderate and high, respectively. Stata software (V.14, STATA Corp) was used to conduct the meta-analysis; METANDI command was used, and p<0.05 was regarded statistically significant.
Patient and public involvement
There is no public and patient involvement.
Results
Prevalence of undernutrition among older adults
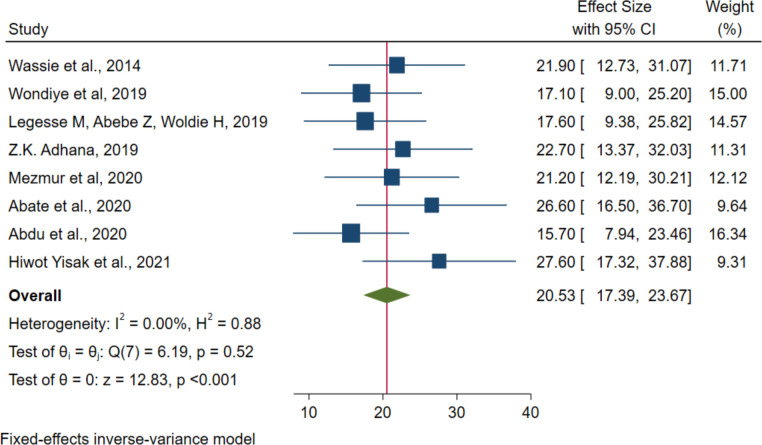
In the estimation of the pooled prevalence of undernutrition, a total of 4628 older adults from eight studies were included. I2 test statistics were used to check the heterogeneity of the studies after a detailed examination by the authors. I2 test statistics of <50%, 50%–75% and >75% were declared as low, moderate and high heterogeneity, respectively.23 Based on this, this study revealed that there was no variation across studies (I2=0.00% and p<0.001). The pooled prevalence of undernutrition (BMI less than 18.5 kg/m2) among older adults in Ethiopia was 20.53% (95% CI 17.39%, 23.67%) (figure 2).
Figure 2.
The pooled prevalence of undernutrition with its 95% CI among older adults in Ethiopia, 2021.
Associated factors of undernutrition among older adults
All eight studies were included in the analysis of associated factors for undernutrition. Ten associated factors of undernutrition among older adults in Ethiopia were included in the analysis. The pooled OR ranges from 0.15 to 13.07. The studies included the meta-analysis effect model with a 95% CI. Heterogeneity was observed among studies for sex, age and depression. Sex, age, depression status (which was assessed by geriatric depression score) and wealth index were found to be statically significant factors of undernutrition among older adults. (table 2).
Table 2.
Summary of meta-analysis for associated factors of undernutrition among older adults in Ethiopia, 2021
| S.no | Factors | No. of studies | AOR (95% CI) | P value | Heterogeneity | ||
| Q value | P value | I2 (%) | |||||
| 1 | Sex (male) | 5 | 0.17 (0.15 to 0.20) | <0.001 | 116.35 | <0.001 | 96.6 |
| Sex (female) | 1 | 1 | 1 | 1 | 1 | ||
| 2 | Age (old-old) (>85) | 1 | 1 | 1 | 1 | 1 | |
| Young old (65-74) | 5 | 0.22 (0.20 to 0.25) | <0.001 | 63.6 | <0.001 | 92.1 | |
| Middle old (75-84) | 4 | 1.63 (0.78 to 3.40) | 0.195 | 0.78 | 0.855 | 0.0 | |
| 3 | Depression (yes) | 3 | 1.27 (1.19 to 1.37) | <0.001 | 12.42 | 0.002 | 83.9 |
| Depression (no) | 1 | 1 | 1 | 1 | 1 | ||
| 4 | Wealth index (rich) | 1 | 1 | 1 | 1 | 1 | |
| Poor | 5 | 1.90 (1.08 to 3.32 | 0.025 | 0.19 | 0.996 | 0.0 | |
| Middle | 5 | 1.13 (0.77 to 1.66) | 0.517 | 3.54 | 0.316 | 15.3 | |
| 5 | Marital status (not married) | 3 | 1.79 (0.82 to 3.90) | 0.143 | 0.43 | 0.807 | 0.0 |
| Marital status (married) | 1 | 1 | 1 | 1 | 1 | ||
| 6 | Educational status (no education) | 4 | 2.00 (0.98 to 4.05) | 0.055 | 0.20 | 0.977 | 0.0 |
| Educational status (with education) | 1 | 1 | 1 | 1 | 1 | ||
| 7 | Residence (rural) | 2 | 2.10 (0.70 to 6.30) | 0.183 | 0.06 | 0.807 | 0.0 |
| Residence (urban) | 1 | 1 | 1 | 1 | 1 | ||
| 8 | DDS (good) | ||||||
| DDS (middle) | 2 | 1.16 (0.79 to 1.69) | 0.446 | 0.06 | 0.804 | 0.0 | |
| DDS (poor) | 2 | 4.28 (0.43 to 13.07) | 0.217 | 0.03 | 0.871 | 0.0 | |
| 9 | Meal frequency (≤2) | 2 | 1.46 (0.82 to 2.56) | 0.196 | 0.34 | 0.559 | 0.0 |
| Meal frequency (>2) | 1 | 1 | 1 | 1 | 1 | ||
| 10 | Declined food intake (yes) | 2 | 2.17 (0.44 to 10.66) | 0.338 | 0.10 | 0.757 | 0.0 |
| Declined food intake (no) | 1 | 1 | 1 | 1 | 1 | ||
Young-old=65–74 years, middle-old=75–84 years, old-old= ≥85 years.
factors associated with under nutrition
DDS, dietary diversity score; I2 (tau-square), estimated variance of the observed effect size; Q-value, implies study variability.
The study revealed that males had lesser odds of being undernutrition as compared with females with AOR 0.17 (95% CI 0.15 to 0.20). Older adults in the age range of 65–74 years (young-old) were less likely to be undernutrition as compared with those whose age was above 85 years (old-old) with AOR 022 (0.22 to 0.25). Older adults who were depressed had higher odds of undernutrition as compared with their counterparts with AOR 1.27 (1.19 to 1.37). However, older adults from households with poor wealth index had two (AOR 1.90; 95% CI 1.08 to 3.32) times more likely to be undernutrition as compared with those who were from rich.
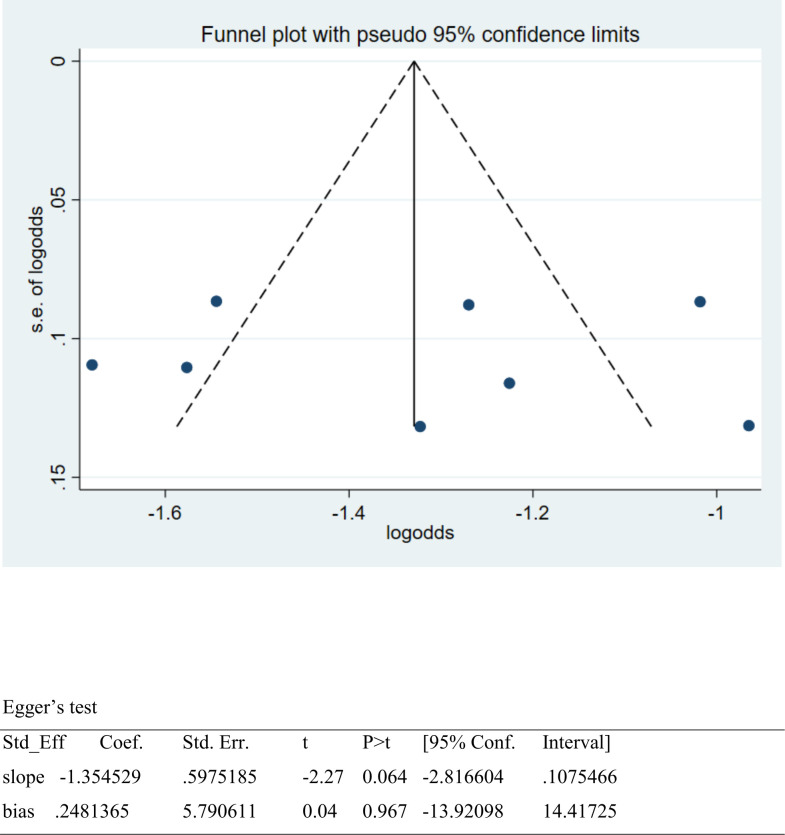
Publication bias
The presence of a small study effect was checked by using funnel plots and Egger’s test from the log-odds scale of the proportion for a better property of meta-analysis of a proportion. SE is dependent on the value of log odds and the underlying proportion. Thus, a study in which r(cases) out of n(sample size) patients were observed to have an event, gives a proportion of r/n. The associated log odds is ln(r/(n-r)) with an SE of sqrt(1 /r+1/(n-r)).24 Hence, the funnel plot showed asymmetric distribution, and the Egger’s test was 0.967; both results revealed that there was no publication bias (figure 3).
Figure 3.
Funnel plot and Egger’s test to assess publication bias for undernutrition among older adults in Ethiopia,2021.
Discussion
The pooled prevalence of undernutrition from a total of 4628 older adults from eight studies among older adults in Ethiopia is 20.53% (95% CI 17.39% to 23.67%). This indicates that undernutrition is a significant public health problem among older adults. This might be because, in Ethiopia, older adults are suffering from many challenges including poverty, deteriorated health and enervation, shrinkage of assets, financial hardship, rejection and scorn by youth, disrespect, abuse and limited social services.25 It was predicted that the prevalence of underweight in sub-Saharan Africa is expected to be up to 6%–48%.26 A systematic review in Africa found a lower pooled prevalence of undernutrition, which was 19.9%, which is comparable with the current study, but the prevalence of the current study was lower than the Central African Republic (CAR) (33.4%).27 Another study from the CAR and the Republic of Congo) reported that the prevalence of undernutrition was 19.2%, which is comparable with the current result.28 A study from Nigeria found a lower prevalence (7.8%).29
The results of this study found that older adults who were depressed had higher odds of undernutrition as compared with their counterparts with AOR 1.27 (1.19 to 1.37). This might be because depression leads to appetite and weight changes that result in undernutrition, and poor nutrition predisposes old individuals to psychiatric upset (depression, agitation and irritability).30 A study from Brazil on undernutrition and depression among community-dwelling older adult people found that nutritional deficit presented a significant association with depression (OR=4.38; 95% CI 2.23 to 8.64; p<0.001).31 Similarly, a study from southern Brazil stated that depression was positively associated with the risk of undernutrition OR 2.4 (95% CI 0.79 to 7.38).32 A population-based study on the association between undernutrition and depression in older adult people in Razavi Khorasan also concluded that there is a significant statistical difference between the prevalence of undernutrition in depressed and non-depressed individuals (p=0.047).33 Another study that was conducted in Bangladesh found that being malnourished (OR: 4.05, 95% CI 2.79 to 5.87) and people at risk of undernutrition (OR: 1.67, 95% CI 1.24 to 2.24) had a significantly higher risk of suffering from depression.34 Similarly, a multicentre, cross-sectional study from Turkey discovered that depression score (OR=95% CI 1.104 to 3.051; p=0.02) was independently associated with undernutrition.35
The current study revealed that females had higher odds of being undernutrition as compared with males with AOR 5.88 (95% CI 5.00 to 6.66). This might be because, in Ethiopia, women, the old-old, those lacking formal education and those with lower incomes reported significantly lower quality of life in the physical, psychological and social domains.36 A systematic review and meta-analysis of undernutrition and risk of undernutrition among older adults (≥60 years) in India reported that the prevalence of undernutrition was higher among females (16.67%).37 The multidimensional background of undernutrition among rural older individuals in Bangladesh investigated that the female gender (p<0.05) was independently associated with poor nutritional status.38 Another systematic review and meta-analysis found a higher risk of undernutrition among females than males (OR=1.45 (95% CI 1.27 to 1.66); p<0.00001).39
The current study found that older adults from households with poor wealth index had two (AOR 1.90; 95% CI 1.08 to 3.32) times more likely to be undernutrition as compared with those who were from rich. This might be because rich individuals use healthcare services, hygiene and sanitation services in addition to having better access to balanced food as compared with the poor. By doing this, the immediate cause of undernutrition (inadequate dietary intake) can be averted. In agreement with this, a systematic review and meta-analysis of observational studies on social and economic factors and undernutrition or the risk of undernutrition in older adults indicated that low-income level (OR: 2.69; 95% CI 2.35 to 3.08; p<0.001).40 Another study on social and economic correlates of undernutrition in the Polish older adult population indicated that self-reported poverty was an independent correlate of undernutrition.41 The assessment of the multidimensional background of undernutrition among rural older individuals in Bangladesh reported that having no income (p<0.01), being illiterate (p<0.01) and not receiving regular financial support (p<0.05) were also independently associated with poor nutritional status.38
Additionally, a cross-sectional survey in South Africa reported that a significantly higher percentage of participants from the lower socioeconomic area were found to be at risk of undernutrition than those from the higher socioeconomic area (74.2% vs 37.1%) (95% CI 19.8% to 51.4%). Participants from the higher socioeconomic area consumed significantly more fluid and protein-rich foods than their counterparts.42
This study showed that older adults in the age range of 65–74 years (young-old) were less likely to be undernutrition as compared with those whose age was above 85 years (old-old) with AOR 022 (0.22 to 0.25). It is supported by the fact that ‘The prevalence of undernutrition is increasing in this population and is associated with a decline in functional status, impaired muscle function, decreased bone mass, immune dysfunction, anemia, reduced cognitive function, poor wound healing, delayed recovery from surgery, higher hospital readmission rates, and mortality’.43 Moreover, a study on the prevalence of undernutrition among institutionalised older adults people in Northern Peninsular Malaysia found that a significantly declining trend of anthropometric measurements was observed among the older adults between the age groups 60–69 years and ≥80 years.44
Conclusion
The burden of undernutrition in Ethiopia is still significant, according to this report. As a result, different intervention measures (food aid, medical care and psychosocial support) need to be provided to minimise the prevalence of undernutrition among Ethiopia’s older adults urgently needed. The current study finds some risk variables linked to undernutrition. The risk factors revealed in this study could be used by policymakers in the country to develop new intervention measures.
Supplementary Material
Footnotes
Contributors: HY is responsible for the overall content as the guarantor; HY, MAZ and AE participated in the conception, study design, execution and acquisition of data. MMA and GA did the analysis and interpretation. ATD and DTA gave final approval for the version to be published. The identification and selection of the papers in all the researched databases were made by HY, MAZ and ATD. All authors have agreed on the journal to which the article has been submitted and agree to be accountable for all aspects of the work.
Funding: The authors did not receive any specific grant for this research
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request. In the manuscript, all the data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Capistrant BD, Glymour MM, Berkman LF. Assessing mobility difficulties for cross-national comparisons: results from the world Health organization study on global ageing and adult health. J Am Geriatr Soc 2014;62:329–35. 10.1111/jgs.12633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rynning E. The ageing populations of Europe -- implications for health systems and patien’s' rights. Eur J Health Law 2008;15:297–306. 10.1163/157180908x338241 [DOI] [PubMed] [Google Scholar]
- 3.Zohoori N. Nutrition and healthy functioning in the developing world. J Nutr 2001;131:2429S–32S. 10.1093/jn/131.9.2429S [DOI] [PubMed] [Google Scholar]
- 4.Fuster V. Changing demographics: a new approach to global health care due to the aging population. J Am Coll Cardiol 2017;69:3002–5. 10.1016/j.jacc.2017.05.013 [DOI] [PubMed] [Google Scholar]
- 5.Agarwal E, Miller M, Yaxley A, et al. Malnutrition in the elderly: a narrative review. Maturitas 2013;76:296–302. 10.1016/j.maturitas.2013.07.013 [DOI] [PubMed] [Google Scholar]
- 6.Milne AC, Potter J, Vivanti A, et al. Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst Rev 2009;2009:CD003288. 10.1002/14651858.CD003288.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen CCH, Schilling LS, Lyder CH. A concept analysis of malnutrition in the elderly. J Adv Nurs 2001;36:131–42. 10.1046/j.1365-2648.2001.01950.x [DOI] [PubMed] [Google Scholar]
- 8.Saka B, Kaya O, Ozturk GB, et al. Malnutrition in the elderly and its relationship with other geriatric syndromes. Clin Nutr 2010;29:745–8. 10.1016/j.clnu.2010.04.006 [DOI] [PubMed] [Google Scholar]
- 9.Evans C. Malnutrition in the elderly: a multifactorial failure to thrive. Perm J 2005;9:38–41. 10.7812/TPP/05-056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hickson M. Malnutrition and ageing. Postgrad Med J 2006;82:2–8. 10.1136/pgmj.2005.037564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsiao PY, Mitchell DC, Coffman DL, et al. Dietary patterns and relationship to obesity-related health outcomes and mortality in adults 75 years of age or greater. J Nutr Health Aging 2013;17:566–72. 10.1007/s12603-013-0014-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ENN ENN . Nutritional status and handgrip strength in older refugees. field exchange 18. 2003: 4. [Google Scholar]
- 13.Vadala AA, ed. Understanding famine in ethiopia: poverty, politics and human rights. Proceedings of the 16th International Conference of Ethiopian Studies; 2009. [Google Scholar]
- 14.Abate T, Mengistu B, Atnafu A, et al. Malnutrition and its determinants among older adults people in addis ababa, ethiopia. BMC Geriatr 2020;20:498. 10.1186/s12877-020-01917-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abdu AO, Yimamu ID, Kahsay AA. Predictors of malnutrition among older adults aged above 65 years in eastern ethiopia: neglected public health concern. BMC Geriatr 2020;20:497. 10.1186/s12877-020-01911-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Legesse M, Abebe Z, Woldie H. Chronic energy deficiency and associated factors among older population in Ethiopia: a community based study. PLoS One 2019;14:e0214861. 10.1371/journal.pone.0214861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mesele M. High prevalence of undernutrition among elderly people in northwest ethiopia: a cross sectional study. JNHFS 2014;2:32. 10.15226/jnhfs.2014.00131 Available: http://symbiosisonlinepublishing.com/nutritionalhealth-foodscience/Volume2-Issue4.php [DOI] [Google Scholar]
- 18.Wondiye K, Asseffa NA, Gemebo TD, et al. Predictors of undernutrition among the elderly in sodo zuriya district wolaita zone, ethiopia. BMC Nutr 2019;5:50. 10.1186/s40795-019-0320-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mezemir Y, Egata G, Geset D, et al. Nutritional status and associated factors among the community-dwelling elderly population in Debre berhan town, North shewa zone, Ethiopia. NDS 2020;Volume 12:289–99. 10.2147/NDS.S280589 [DOI] [Google Scholar]
- 20.Adhana Z, Tessema G, Getie G. Prevalence of under nutrition and associated factors among people of old age in debre markos town. Northwest Ethiopia, 2015. [Google Scholar]
- 21.Yisak H, Maru I, Abie M, et al. Determinants of under nutrition among the elderly in south gondar zone, ethiopia. In Review [Preprint]. 10.21203/rs.3.rs-449391/v1 [DOI]
- 22.Stang A. Critical evaluation of the newcastle-ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. 10.1007/s10654-010-9491-z [DOI] [PubMed] [Google Scholar]
- 23.Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hunter JP, Saratzis A, Sutton AJ, et al. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J Clin Epidemiol 2014;67:897–903. 10.1016/j.jclinepi.2014.03.003 [DOI] [PubMed] [Google Scholar]
- 25.Zelalem A, Gebremariam Kotecho M. Challenges of aging in rural ethiopia: old age is like the sunset: it brings disrespect and challenges. J Gerontol Soc Work 2020;63:893–916. 10.1080/01634372.2020.1814475 [DOI] [PubMed] [Google Scholar]
- 26.Kimokoti RW, Hamer DH. Nutrition, health, and aging in sub-Saharan Africa. Nutr Rev 2008;66:611–23. 10.1111/j.1753-4887.2008.00113.x [DOI] [PubMed] [Google Scholar]
- 27.Mabiama G, Adiogo D, Millimono T, et al. Undernutrition, overweight and obesity among elderly living in communities in Africa: a systematic review. Proc Nutr Soc 2021;80:CE4. 10.1017/S0029665121002810 [DOI] [Google Scholar]
- 28.Jésus P, Guerchet M, Pilleron S, et al. Undernutrition and obesity among elderly people living in two cities of developing countries: prevalence and associated factors in the EDAC study. Clin Nutr ESPEN 2017;21:40–50. 10.1016/j.clnesp.2017.05.007 [DOI] [PubMed] [Google Scholar]
- 29.Adebusoye LA, Ajayi IO, Dairo MD, et al. Nutritional status of older persons presenting in a primary care clinic in Nigeria. J Nutr Gerontol Geriatr 2012;31:71–85. 10.1080/21551197.2012.647560 [DOI] [PubMed] [Google Scholar]
- 30.Holford P. Depression: the nutrition connection. Primary Care Mental Health 2003;1:9–16. [Google Scholar]
- 31.Cabrera MAS, Mesas AE, Garcia ARL, et al. Malnutrition and depression among community-dwelling elderly people. J Am Med Dir Assoc 2007;8:582–4. 10.1016/j.jamda.2007.07.008 [DOI] [PubMed] [Google Scholar]
- 32.Pérez Cruz E, Lizárraga Sánchez DC, Martínez Esteves MDR. Association between malnutrition and depression in elderly. Nutr Hosp 2014;29:901–6. 10.3305/nh.2014.29.4.7228 [DOI] [PubMed] [Google Scholar]
- 33.Mokhber N, Majdi M, Ali-Abadi M, et al. Association between malnutrition and depression in elderly people in razavi khorasan: a population based-study in Iran. Iran J Public Health 2011;40:67–74. [PMC free article] [PubMed] [Google Scholar]
- 34.Alam MR, Karmokar S, Reza S, et al. Geriatric malnutrition and depression: evidence from elderly home care population in bangladesh. Prev Med Rep 2021;23:101478. 10.1016/j.pmedr.2021.101478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gündüz E, Eskin F, Gündüz M, et al. Malnutrition in community-dwelling elderly in turkey: a multicenter, cross-sectional study. Med Sci Monit 2015;21:2750–6. 10.12659/MSM.893894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kotecho M, Adamek ME. Gender differences in quality of life of urban elders in Ethiopia. Innov Aging 2017;1(suppl_1):879–80. 10.1093/geroni/igx004.3159 [DOI] [Google Scholar]
- 37.Kushwaha S, Khanna P, Srivastava R, et al. Estimates of malnutrition and risk of malnutrition among the elderly (≥60 years) in india: a systematic review and meta-analysis. Ageing Res Rev 2020;63:101137. 10.1016/j.arr.2020.101137 [DOI] [PubMed] [Google Scholar]
- 38.Ferdous T, Kabir ZN, Wahlin A, et al. The multidimensional background of malnutrition among rural older individuals in Bangladesh -- a challenge for the millennium development goal. Public Health Nutr 2009;12:2270–8. 10.1017/S1368980009005096 [DOI] [PubMed] [Google Scholar]
- 39.Crichton M, Craven D, Mackay H, et al. A systematic review, meta-analysis and meta-regression of the prevalence of protein-energy malnutrition: associations with geographical region and sex. Age Ageing 2019;48:38–48. 10.1093/ageing/afy144 [DOI] [PubMed] [Google Scholar]
- 40.Besora-Moreno M, Llauradó E, Tarro L, et al. Social and economic factors and malnutrition or the risk of malnutrition in the elderly: a systematic review and meta-analysis of observational studies. Nutrients 2020;12:737. 10.3390/nu12030737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Krzymińska-Siemaszko R, Mossakowska M, Skalska A, et al. Social and economic correlates of malnutrition in Polish elderly population: the results of polsenior study. J Nutr Health Aging 2015;19:397–402. 10.1007/s12603-014-0572-7 [DOI] [PubMed] [Google Scholar]
- 42.Robb L, Walsh CM, Nel M, et al. Malnutrition in the elderly residing in long-term care facilities: a cross sectional survey using the mini nutritional assessment (MNA®) screening tool. South African Journal of Clinical Nutrition 2017;30:34–40. 10.1080/16070658.2016.1248062 [DOI] [Google Scholar]
- 43.Amarya S, Singh K, Sabharwal M. Changes during aging and their association with malnutrition. Journal of Clinical Gerontology and Geriatrics 2015;6:78–84. 10.1016/j.jcgg.2015.05.003 [DOI] [Google Scholar]
- 44.Chen ST, Ngoh HJ, Harith S. Prevalence of malnutrition among institutionalized elderly people in northern peninsular malaysia: gender, ethnicity and age-specific. Sains Malaysiana 2012;41:141–8. 10.1016/S1875-6867(11)60023-7 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on reasonable request. In the manuscript, all the data are available.