Clinical question
How can I improve outcomes for older adults with chronic kidney disease (CKD)?
Bottom line
Chronic kidney disease is associated with substantial morbidity and health care costs.1 Strategies and tools to predict and delay progression to end-stage kidney disease (ESKD) are vital, especially for patients with clinical frailty or with comorbidities. For a more comprehensive summary on this topic, see the in-depth article published in the Canadian Geriatrics Society Journal of CME.2
Evidence
There is physiologic decline in estimated glomerular filtration rate (eGFR) starting in one’s third and fourth decades, with a loss of approximately 8 mL/min every subsequent decade.3
A hallmark of normal age-related renal decline is the relative absence of proteinuria,4 which is associated with a better prognosis.5
Hypertension, hyperglycemia, atherosclerotic disease, smoking, and hyperlipidemia are associated with accelerated renal decline.6,7
The rate of eGFR decline can guide management; older patients with slow eGFR decline (<2 mL/min/year) are unlikely to progress to ESKD.8
Approach
While creatinine-based eGFR is affected by age, sex, and muscle mass,9 eGFR combined with albuminuria is useful in predicting progression of CKD. The Kidney Failure Risk Equation (KFRE; https://kidneyfailurerisk.com) is a validated tool that can predict 2- and 5-year risk of ESKD. Individuals with a 5-year KFRE score of greater than 5% warrant referral to a nephrologist.10
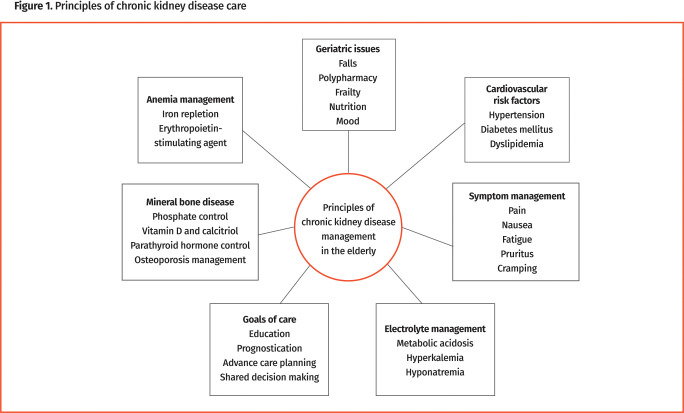
Risk factor management. Controlling blood pressure, lipid levels, and blood glucose levels are cornerstones of CKD management (Figure 1).6 Hypertension Canada recommends a target blood pressure of less than 130/80 mm Hg in patients with diabetes and less than 120/80 mm Hg in others.11,12 Kidney Disease: Improving Global Outcomes (KDIGO) 2021 guidelines recommend intensive blood pressure lowering with or without diabetes13; however, Hypertension Canada and KDIGO acknowledge limitations of evidence for blood pressure lowering in older people,11,13 and patients with substantial frailty or proclivity to falling require an individualized approach.14 One example of adverse effects due to aggressively lowering blood pressure in older patients is postural hypotension,15 which can lead to falls and trauma.
Figure 1.
Principles of chronic kidney disease care
Similarly, glycemic control needs to be individualized. Canadian guidelines recommend that hemoglobin A1c targets should depend on frailty or cognition, with a focus on avoiding extremes in blood glucose levels.16,17
The effect of lipid management is attenuated in those older than 85 years.18 Lowering statin doses should be considered in elderly people with CKD, and patients should be monitored for myopathy.19 It may be prudent to defer statin therapy in patients who are frail with poor nutrition and risk of sarcopenia.18
Other management. Anemia is common in CKD and is often related to relative erythropoietin deficiency.20 Symptoms may be magnified in elderly patients and impact quality of life. Anemia with CKD is associated with increased cardiovascular events, hospitalizations, transfusions, and death.21 Although ferritin levels are often elevated in CKD patients, iron deficiency is still possible: KDIGO recommends a trial of intravenous iron for patients with transferrin saturation of less than 30% and ferritin levels of less than 500 μg/L despite oral supplementation.22 According to Canadian Society of Nephrology guidelines, an erythropoietin-stimulating agent should be initiated when the hemoglobin level is between 90 and 100 g/L, with a target range of 100 to 110 g/L.23 Dosing and monitoring should be managed by nephrologists.
There is an elevated risk of fragility fractures in patients with CKD.24 Bone densitometry scans can be difficult to interpret in CKD but newer guidelines recommend using them to follow treatment effects.25 As CKD progresses, the ability to hydroxylate 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D wanes, and supplementation with calcitriol is often required.26 More information on osteoporosis and mineral management can be found on the Canadian Geriatrics Society website.27
Loss of bicarbonate and decreased excretion of acids resulting in metabolic acidosis can be found in those with CKD.28 Chronic metabolic acidosis may contribute to osteopenia, muscle catabolism, and systemic inflammation, all of which contribute to frailty. There is increased mortality associated with bicarbonate levels of less than 22 mmol/L; KDIGO recommends initiating treatment with oral bicarbonate when serum levels fall below this threshold.29
Patients with ESRD may experience uremic symptoms including fatigue, decreased appetite, metallic taste (dysgeusia), dyspnea, edema, and cognition changes.30 Although dialysis may provide survival and symptom improvement, these benefits are often modest in patients who are frail31 and can result in reduced quality of life and decreased independence.32,33 Elderly patients undergoing dialysis experience substantial symptom burden, with an average of 5 to 6 symptoms and the predominant being fatigue.34 Home-based modalities such as peritoneal dialysis may be better tolerated and can be provided with the help of home care programs.35
Implementation
Patients with a KFRE score of more than 5% over 5 years should be referred to a nephrologist, and those at higher risk of advanced progressive kidney disease (KFRE >10%) should be managed in a multi-care kidney clinic by a team that includes nurses, pharmacists, dietitians, social workers, and physicians. Management of elderly patients must incorporate geriatric competencies including evaluation of frailty, cognitive impairment, and multiple medications.
Goals of care planning
As renal function declines, it becomes imperative to discuss future planning and goals related to ESKD and renal replacement therapy.36 It is important for the patient and their family to participate in shared decision making with providers and to be told potential benefits and harms or consequences of renal replacement therapy.37
Conservative renal care without dialysis may be a good option in patients with comorbidities and frailty. This focuses on palliating symptoms and avoiding invasive therapies that provide little benefit in terms of symptoms and survival.38 Tools such as the Clinical Frailty Scale39 can be useful to identify patients who would benefit from conservative management. Fostering partnerships between family medicine, nephrology, geriatrics, and palliative medicine would help establish a holistic approach to care and ensure that patients’ goals and values are incorporated into management of CKD.
Geriatric Gems are produced in association with the Canadian Geriatrics Society Journal of CME, a free peer-reviewed journal published by the Canadian Geriatrics Society (http://www.geriatricsjournal.ca). The articles summarize evidence from review articles published in the Canadian Geriatrics Society Journal of CME and offer practical approaches for family physicians caring for elderly patients.
Footnotes
Competing interests
None declared
This article is eligible for Mainpro+ certified Self-Learning credits. To earn credits, go to https://www.cfp.ca and click on the Mainpro+ link.
La traduction en français de cet article se trouve à https://www.cfp.ca dans la table des matières du numéro de janvier 2023 à la page e14.
References
- 1.Saran R, Li Y, Robinson B, Abbott KC, Agodoa LYC, Ayanian J, et al. US Renal Data System 2015 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis 2016;67(3 Suppl 1):Svii-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chow E, Merchant AA.. An approach to chronic kidney disease in the elderly—use of the Kidney Failure Risk Equation. Can Geriatr Soc J CME 2022;11(2). [Google Scholar]
- 3.National Kidney Foundation . K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002;39(2 Suppl 1):S1-266. [PubMed] [Google Scholar]
- 4.Verma V, Kant R, Sunnoqrot N, Gambert SR.. Proteinuria in the elderly: evaluation and management. Int Urol Nephrol 2012;44(6):1745-51. Epub 2012 Jul 25. [DOI] [PubMed] [Google Scholar]
- 5.Denic A, Glassock RJ, Rule AD.. Structural and functional changes with the aging kidney. Adv Chronic Kidney Dis 2016;23(1):19-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maw TT, Fried L.. Chronic kidney disease in the elderly. Clin Geriatr Med 2013;29(3):611-24. [DOI] [PubMed] [Google Scholar]
- 7.Soares CM, Diniz JSS, Lima EM, Oliveira GR, Canhestro MR, Colosimo EA, et al. Predictive factors of progression to chronic kidney disease stage 5 in a predialysis interdisciplinary programme. Nephrol Dial Transplant 2009;24(3):848-55. Epub 2008 Oct 7. [DOI] [PubMed] [Google Scholar]
- 8.Shim RL, O’Hare AM.. Chapter 5: rate of decline in eGFR and clinical evaluation of the elderly with a low eGFR. In: Coffman TM. Online curricula: geriatric nephrology. Washington, DC: American Society of Nephrology; 2009. Available from: https://www.asn-online.org/education/distancelearning/curricula/geriatrics/. Accessed 2022 Dec 9. [Google Scholar]
- 9.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150(9):604-12. Erratum in: Ann Intern Med 2011;155(6):408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tangri N, Stevens LA, Griffith J, Tighiouart H, Djurdjev O, Naimark D, et al. A predictive model for progression of chronic kidney disease to kidney failure. JAMA 2011;305(15):1553-9. Epub 2011 Apr 11. [DOI] [PubMed] [Google Scholar]
- 11.Rabi DM, McBrien KA, Sapir-Pichhadze R, Nakhla M, Ahmed SB, Dumanski SM, et al. Hypertension Canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can J Cardiol 2020;36(5):596-624. [DOI] [PubMed] [Google Scholar]
- 12.SPRINT Research Group; Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015;373(22):2103-16. Epub 2015 Nov 9. Erratum in: N Engl J Med 2017;377(25):2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheung AK, Chang TI, Cushman WC, Furth SL, Hou FF, Ix JH, et al. Executive summary of the KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int 2021;99(3):559-69. [DOI] [PubMed] [Google Scholar]
- 14.Del Pinto R, Pietropaoli D, Ferri C.. Diastolic blood pressure and risk profile in renal and cardiovascular diseases. Results from the SPRINT trial. J Am Soc Hypertens 2018;12(7):513-23.e3. Epub 2018 May 5. [DOI] [PubMed] [Google Scholar]
- 15.Fall prevention for health professionals. Postural hypotension. Ottawa, ON: Regional Geriatric Program of Eastern Ontario; 2022. Available from: https://www.rgpeo.com/stop-falls/health-professionals/postural-hypotension/. Accessed 2022 Dec 9. [Google Scholar]
- 16.Lipska KJ, Krumholz H, Soones T, Lee SJ.. Polypharmacy in the aging patient: a review of glycemic control in older adults with type 2 diabetes. JAMA 2016;315(10):1034-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diabetes Canada Clinical Practice Guidelines Expert Committee; Imran SA, Agarwal G, Bajaj HS, Ross S.. Targets for glycemic control. Can J Diabetes 2018;42(Suppl 1):S42-6. [DOI] [PubMed] [Google Scholar]
- 18.Rich MW. Aggressive lipid management in very elderly adults: less is more. J Am Geriatr Soc 2014;62(5):945-7. Epub 2014 May 6. [DOI] [PubMed] [Google Scholar]
- 19.Strandberg TE, Kolehmainen L, Vuorio A.. Evaluation and treatment of older patients with hypercholesterolemia: a clinical review. JAMA 2014;312(11):1136-44. [DOI] [PubMed] [Google Scholar]
- 20.McGonigle RJ, Wallin JD, Shadduck RK, Fisher JW.. Erythropoietin deficiency and inhibition of erythropoiesis in renal insufficiency. Kidney Int 1984;25(2):437-44. [DOI] [PubMed] [Google Scholar]
- 21.Wouters HJCM, van der Klauw MM, de Witte T, Stauder R, Swinkels DW, Wolffenbuttel BHR, et al. Association of anemia with health-related quality of life and survival: a large population-based cohort study. Haematologica 2019;104(3):468-76. Epub 2018 Oct 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McMurray JJV, Parfrey PS, Adamson JW, Macdougall IC, Aljama P, McDonald RA, et al. Kidney Disease: Improving Global Outcomes (KDIGO) anemia work group. KDIGO clinical practice guideline for anemia in chronic kidney disease. Kidney Int Suppl 2012;2(4):279-335. Available from: https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2012-Anemia-Guideline-English.pdf. Accessed 2022 Dec 9. [Google Scholar]
- 23.Moist LM, Troyanov S, White CT, Wazny LD, Wilson JA, McFarlane P, et al. Canadian Society of Nephrology commentary on the 2012 KDIGO clinical practice guideline for anemia in CKD. Am J Kidney Dis 2013;62(5):860-73. Epub 2013 Sep 17. [DOI] [PubMed] [Google Scholar]
- 24.Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, Heckbert SR, et al. Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int 2000;58(1):396-9. [DOI] [PubMed] [Google Scholar]
- 25.Ketteler M, Block GA, Evenepoel P, Fukagawa M, Herzog CA, McCann L, et al. Executive summary of the 2017 KDIGO chronic kidney disease-mineral and bone disorder (CKD-MBD) guideline update: what’s changed and why it matters. Kidney Int 2017;92(1):26-36. Erratum in: Kidney Int 2017;92(6):1558. [DOI] [PubMed] [Google Scholar]
- 26.Sprague SM, Coyne D.. Control of secondary hyperparathyroidism by vitamin D receptor agonists in chronic kidney disease. Clin J Am Soc Nephrol 2010;5(3):512-8. Epub 2010 Feb 4. [DOI] [PubMed] [Google Scholar]
- 27.Juby A, Davis C.. Common controversies in osteoporosis therapy—helping patients make informed decisions. Can Geriatr Soc J CME 2015;5(2):49-55. Available from: https://static1.squarespace.com/static/63599251a953f80dd1922762/t/636e5f700a703c10b7b67a4d/1668177777426/6_Common+Controversies_Angela+Juby.pdf. Accessed 2022 Dec 14. [Google Scholar]
- 28.Kraut JA, Madias NE.. Consequences and therapy of the metabolic acidosis of chronic kidney disease. Pediatr Nephrol 2011;26(1):19-28. Epub 2010 Jun 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Andrassy KM. Comments on ‘KIDOGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease’ [letter]. Kidney Int 2013;84(3):622-3. [DOI] [PubMed] [Google Scholar]
- 30.O’Connor NR, Kumar P.. Conservative management of end-stage renal disease without dialysis: a systematic review. J Palliat Med 2012;15(2):228-35. Epub 2012 Feb 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chandna SM, Da Silva-Gane M, Marshall C, Warwicker P, Greenwood RN, Farrington K.. Survival of elderly patients with stage 5 CKD: comparison of conservative management and renal replacement therapy. Nephrol Dial Transplant 2011;26(5):1608-14. Epub 2010 Nov 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE.. Functional status of elderly adults before and after initiation of dialysis. N Engl J Med 2009;361(16):1539-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jassal SV, Chiu E, Hladunewich M.. Loss of independence in patients starting dialysis at 80 years of age or older. N Engl J Med 2009;361(16):1612-3. [DOI] [PubMed] [Google Scholar]
- 34.Jablonski A. The multidimensional characteristics of symptoms reported by patients on hemodialysis. Nephrol Nurs J 2007;34(1):29-38. [PubMed] [Google Scholar]
- 35.Brown EA, Finkelstein FO, Iyasere OU, Kliger AS.. Peritoneal or hemodialysis for the frail elderly patient, the choice of 2 evils? Kidney Int 2017;91(2):294-303. Epub 2016 Oct 20. [DOI] [PubMed] [Google Scholar]
- 36.Palliative care tools. Toronto, ON: Ontario Renal Network. Available from: https://www.ontariorenalnetwork.ca/en/kidney-care-resources/clinical-tools/palliative-care. Accessed 2022 Dec 9. [Google Scholar]
- 37.Koncicki HM, Swidler MA.. Decision making in elderly patients with advanced kidney disease. Clin Geriatr Med 2013;29(3):641-55. [DOI] [PubMed] [Google Scholar]
- 38.Wiggins J. Chapter 28: integrated care of the elderly with ESKD. In: Coffman TM. Online curricula: geriatric nephrology. Washington, DC: American Society of Nephrology; 2009. Available from: https://www.asn-online.org/education/distancelearning/curricula/geriatrics/. Accessed 2022 Dec 9. [Google Scholar]
- 39.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173(5):489-95. [DOI] [PMC free article] [PubMed] [Google Scholar]