ABSTRACT
Stroke in the young is an uncommon condition resulting in significant morbidity and as result trammels the integrity of healthcare systems [1]. We present an unusual case of a 37-year-old male presenting with neurologic signs of right parietal lobe infarction with evidence of vertebral artery dissection and persistent carotid-vertebrobasilar anastomosis as a conduit for thromboembolism.
INTRODUCTION
Stroke in the young goes against all expectation as its occurrence is more fitting for the more aged population. Cervical artery dissection, described as the splitting of the arterial wall of the carotid or vertebral artery, accounts for up to 20% of stroke in the young [2]. Vertebral artery dissections present half as many times as internal carotid artery (ICA) dissections with an annual incidence rate of 0.97 versus 1.72 per 100 000 [3]. Both young and aged populations present with local symptoms of occipital headache and neck pain. However, they are exclusively different in neurological signs and symptoms with respect to the cerebral territories they supply. It is unusual for anterior circulation infarction to occur from a posterior circulation lesion, but is possible through an aberrant carotid-basilar anastomosis. As a result, the patient presents with features of vertebral artery embolism and dissection. There is only one case reported in the medical literature indicating an association with vertebral artery dissection in the presence of persistent primitive trigeminal artery (PPTA) [4], but there was no associated anterior circulation infarct. We report a patient with a right parietal ischemic infarct secondary to a left vertebral artery dissection and right PPTA.
CASE REPORT
A 37-year-old right-handed Indo-Trinidadian male was accepted into the emergency department with acute left-sided weakness with numbness of left upper limb, sudden loss of consciousness, dizziness, dysphasia and blurred vision within 2 h of the onset of these symptoms. The patient had no medical history of hypertension, diabetes mellitus, dyslipidemia, heart disease, immunocompromised states, connective tissue disorders, autoimmune disorders or illicit drug use. Family history is positive for myocardial infarction and diabetes mellitus. The history of most recent event was one of being seated at rest when there was a sudden onset of the presenting symptoms. There was no violent coughing nor sneezing, chiropractic activity, no trauma to the cervical spine nor falls.
He was conscious with no hemodynamic instability including systolic blood pressure of 110 mmHg, heart rate of 70 beats/min and temperature of 36.4°C. Neurological assessment revealed dysarthria, left-sided hemiparesis, loss of two-point discrimination in left upper extremity and right-sided facial paralysis. Review of other systems demonstrated no clinical significance. Laboratory findings on presentation included HbA1c 5.1%, fasting glucose 95 mg/dL, cholesterol 188 mg/dL (desirable < 200 mg/dL), triglycerides 110 mg/dL (normal < 150 mg/dL), High-Density Lipoprotein 31 mg/dL (40–60 mg/dL), Low-Density Lipoprotein 102 (<100 mg/dL), Cholesterol 135 mg/dL (50–160 mg/dL), Very Low-Density Lipoprotein 22 mg/dL (0–38 mg/dL), risk ratio 6.1(low 3.0, average 5.0, high 13.0). Coagulation screen: partial thromboplastin time 30.1 (control 30.1 s), prothrombin time 11.1 (control 11.6), International Normalized Ratio 0.95. Cardiac triage: creatine kinase-MB 10.00 (0.00–16.00 U/L), troponin T < 50 ng/L (acute myocardial infarction NOT LIKELY). Myoglobin 32.0 (16–76 ng/ml). Autoimmune screen: cardiolipin Ig (immunoglobulin) A 4.78 (negative < 15APL, cardiolipin IgG 2.31 (< 10 GPL), cardiolipin IgM 1.32 (negative < 15 MPL), ANA IgG 0.05 (<0.9 no detectable ANA IgG by ELISA). Hematology: platelets 256 (150–410 ×103/mm3), hemoglobin 15.3 (13–17 g/dL), hematocrit 45 (40–50%), low mean corpuscular volume 79 (83–101 fl). Factor V Leiden 2.57 (ratio 2.18–3.38), fibrinogen 4.09 (3.08–6.13 g/L), lupus anticoagulant screen 1.52 (ratio positive > 1.2. C-reactive protein < 5.0 (<10 mg/dL), erythrocyte sedimentation rate 10 (male, 17–50 years ≤ 10 mm/h), protein C 123 (70.0–140.0% activity), elevated protein S 155 (63.0–135.0% activity), antithrombin III 96 (83–128% activity). Biochemistry: creatinine 0.81 (0.66–1.25 mg/dL), serum sodium 145 (135–148 mmol/L), serum potassium (3.8–5.2 mmol/L), mildly elevated serum chloride 110 (95–106 mmol/L), blood urea nitrogen 15 (9.0–20.0 mg/dL). D-dimer 0.26 (<0.5 ug/ml), liver profile: elevated globulin 3.7 (2.3–3.5 g/dL). Electrocardiogram showed normal sinus rhythm. Echocardiography was negative for valvular pathology or thrombus, no pericardial effusion with normal left ventricular wall motion (ejection fraction Simpson: 60%). Also, on presentation at the emergency department, a contrast computerized tomography (CT) of the head and neck showed a right vertebral artery arising from the right subclavian artery, but is small in caliber and does not fully opacify and dissection flap within the right vertebral artery. The left vertebral and common and internal carotid arteries are normal in caliber. A PPTA is present on the right side without associated cerebral aneurysm or vascular malformations noted. The aortic arch is normal in outline. A cerebral axial diffusion-weighted magnetic resonance imaging (MRI) performed also at the time of presentation to the emergency department demonstrated an area of hyperintensity in the right parietal lobe adjacent to the Sylvian fissure (right middle cerebral artery territory) consistent with clinical findings, a right PPTA and diffuse narrowing of visualized part of the right vertebral artery, possibly hypoplastic (Fig. 1). A 3D time of flight magnetic resonance angiography (3D-TOF MRA) on 1.5 Tesla demonstrated crescent sign in left vertebral artery indicating dissection (Fig. 2A), and PPTA between right ICA and distal basilar artery with normal diameter of both ICAs (Fig. 3). The patient was anti-coagulated with intravenous heparin [10], which resulted in rapid but incomplete resolution of symptoms. This initial anticoagulation was coupled with oral antiplatelet therapy, using aspirin and clopidogrel for the purpose of long-term administration. On follow-up, a repeat contrast MRI 10 days later demonstrated a hypoplastic right vertebral artery. In addition, a color duplex ultrasonogram of vertebral arteries demonstrated a flow-dependent flap seen on cardiac cycling along the intra-foraminal left vertebral artery. Clinically, at this 1-week post-presentation, he was with full recovery of motor and sensory function on the left side with a subjective assessment of mildly slurred speech. Subsequent follow-up detailed occasional mild neck pains of no subjective concerns regarding occupational hazards. Efforts have been made to review the progress of this patient, but he has been unable to present to the outpatient clinic for even further follow-up.
Figure 1.
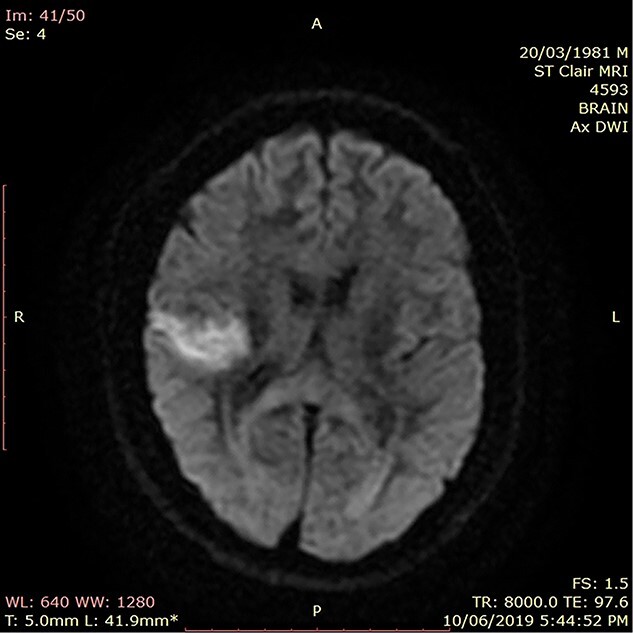
Axial DWI MRI showing hyperintensity in right parietal lobe adjacent to sylvian fissure.
Figure 2.
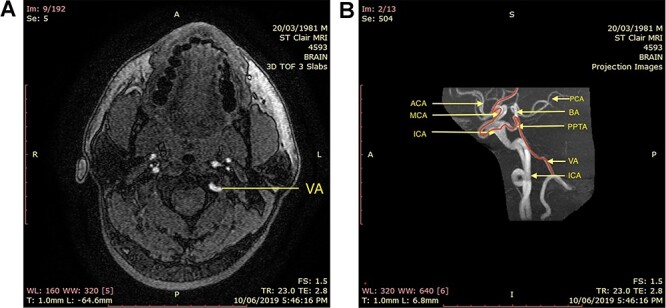
(A) axial 3D-TOF MRI showing ‘crescent sign’ or dissection of left vertebral artery. (B) Sagittal highlight of major intracranial vessels and associated PPTA.
Figure 3.
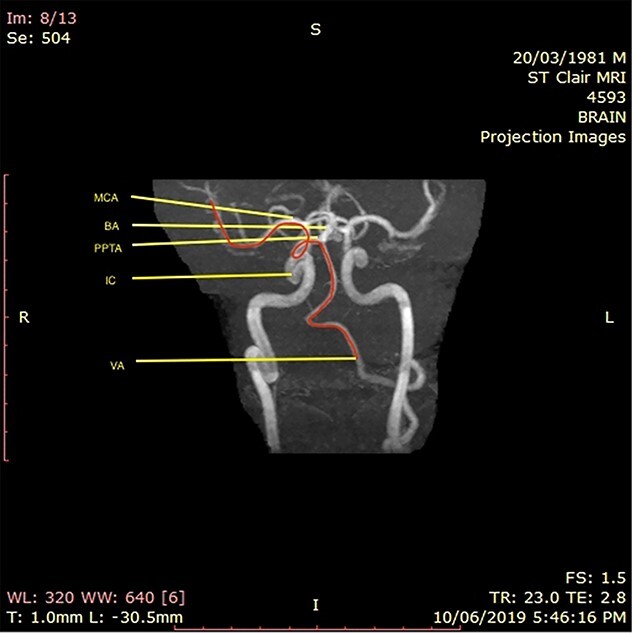
MRA showing presumed path of embolism from vertebral artery through PPTA to right ICA to right MCA.
DISCUSSION
The incidence rate of stroke in the population under the age of 40 has been increasing worldwide and varies from 8 to 100 per 100 000 person-years. However, the causes are not always well-defined. In contrast to stroke in the elderly, causes are different and rare including illicit drug use, patent foramen ovale, pregnancy, autoimmune diseases and cervical artery dissection. Cervical artery dissections are the most common cause of stroke in the young with vertebral artery dissections accounting for half as many as ICA dissections. Vertebral artery dissections are usually due to extrinsic factors such as trauma, whiplash accidents in motor vehicular accidents, direct hit, medical procedures and strangulation. Numerous reports have described rare etiologies including minor injuries from coughing, vomiting, violent sneezing, sports, roller coaster rides or chiropractic manipulation. Spontaneous dissections are also reported in those with underlying arteriopathy, such as connective tissue diseases or fibromuscular dysplasia. Due its low incidence rate, however, this may very well be also attributed to presumed minor injuries.
Vertebral artery dissections typically present with occipital headache, neck pain or vertigo, with some experiencing ischemic manifestations such as posterior circulation syndromes including lateral medullary syndrome—dysphagia, dizziness, vertigo, Horner’s syndrome, nystagmus. However, due to the presentation of anterior circulation infarct in this patient, cervical artery dissection as an etiology seems highly unlikely. However, in this patient, there was no clear evidence to support a hematological, inflammatory, traumatic, nor metabolic cause via the anterior circulation. After ruling out other causes of stroke in the young, imaging also revealed a PPTA that anastomoses the distal basilic artery to the right ICA. This anastomosis provides a potential conduit for emboli from the vertebral artery dissection resulting in an anterior circulation stroke instead of a typical posterior circulation stroke.
PPTA is the most common and largest of the primitive carotid-basilar anastomoses that persist into adulthood with a prevalence of 0.1% and 0.68% [5, 6]. Other persistent primitive anastomoses include the primitive otic (acoustic) artery, the primitive hypoglossal artery and the primitive proatlantal artery. There have been infrequent reports cases of these anastomoses implicated in multi-territorial infarcts attributed to their role as conduits [7, 8].
To the best of our experience, this is the first report of vertebral artery dissection and anterior circulation stroke secondary to embolism through PPTA.
ACKNOWLEDGEMENTS
All individuals in this report have made exceptional contributions.
Contributor Information
Kymmi S Caesar, St Clair Medical Center, Port of Spain, Trinidad, West Indies.
Dale A Maharaj, St Clair Medical Center, Port of Spain, Trinidad, West Indies.
Anil Ramlakhansingh, St Clair Medical Center, Port of Spain, Trinidad, West Indies.
Alexander Sinanan, St Clair Medical Center, Port of Spain, Trinidad, West Indies.
Richard Ramsingh, St Clair Medical Center, Port of Spain, Trinidad, West Indies.
CONFLICT OF INTEREST
None applicable.
FUNDING
No acknowledgment for funding has been identified.
ETHICAL APPROVAL
None required in this instance.
CONSENT
Received and available if requested.
GUARANTOR
Dr Dale A. Maharaj.
REFERENCES
- 1. Ekker MS, Boot EM, Singhal ABet al. Epidemiology, etiology, and management of ischemic stroke in young adults. Lancet Neurol 2018;17:790–801. Available from: 10.1016/S1474-4422(18)30233-3. [DOI] [PubMed] [Google Scholar]
- 2. Smajlović D.. Strokes in young adults: epidemiology and prevention. Vascular health and risk management, 2015;11:157–164. 10.2147/VHRM.S53203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee VH, Brown RD, Mandrekar JNet al. Incidence and outcome of cervical artery dissection: a population-based study. Neurology 2006;67:1809–12. [DOI] [PubMed] [Google Scholar]
- 4. Nunes M, Ullah A, Rios Jet al. Persistent trigeminal artery playing a protective role in a case of vertebral artery dissection and stenosis. Cureus 2019;11:1–2. https://assets.cureus.com/uploads/case_report/pdf/21719/1612429044-1612429037-20210204-18203-1rvkve3.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Azab W, Delashaw J, Mohammed M. Persistent primitive trigeminal artery: a review. Turk Neurosurg 2012;22:399–406. [DOI] [PubMed] [Google Scholar]
- 6. Salas E, Ziyal IM, Sekhar LNet al. Persistent trigeminal artery: an anatomic study. Neurosurgery 1998;43:557–61. [DOI] [PubMed] [Google Scholar]
- 7. Srinivas, M. R., Vedaraju, K. S., Manjappa, B. H., Nagaraj, B. R.. Persistent Primitive Hypoglossal Artery (PPHA) - A Rare Anomaly with Literature Review. Journal of clinical and diagnostic research : JCDR, 2016;10:TD13–TD14. 10.7860/JCDR/2016/15556.7116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Peng J, Liu Z, Luo Cet al. Treatment of cervical artery dissection: antithrombotics, thrombolysis, and endovascular therapy. Biomed Res Int 2017;2017:3072098. 10.1155/2017/3072098. [DOI] [PMC free article] [PubMed] [Google Scholar]


