Highlights
-
•
A large proportion of the Indian population were found to have had an asymptomatic SARS-CoV-2 infection.
-
•
We estimated the reported and infection frequency difference.
-
•
There was high variability in viral transmission between states.
-
•
The distribution of seropositivity was uneven, suggesting future waves.
KEYWORDS: Antibody, Coronavirus, India, Seroprevalence, SARS-CoV-2
Abstract
In 2020, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spread across the world within a few months. The SARS-CoV-2 pandemic has had a devastating effect on humanity, with social and economic consequences. The continents of Europe and America have been hit the hardest. However, there has also been a huge loss of life in India, with the country having the fourth highest number of total deaths worldwide. Nevertheless, the infection and death rates per million and the case fatality ratio in India are substantially lower than those in many developed nations. Several explanations for this have been proposed, including genetics. Mathematical modelling has suggested that the actual number of infections is much higher than the number of reported cases. Therefore, to understand the dynamics of actual infection and the population-level immunity against SARS-CoV-2, a serosurvey (antibody testing) was performed among 2301 individuals in urban regions of 14 districts in six states of India. A notable outcome of this study was that a large proportion of the Indian population had an asymptomatic SARS-CoV-2 infection. The real infection rate in India was several fold higher than the reported number of cases. Therefore, a large number of people in the country have developed SARS-CoV-2-specific antibodies. In this survey, the seroprevalence (frequency antibody-positive) varied between 0.01 (95% CI 0.002–0.054) and 0.477 (95% CI 0.392–0.563), suggesting a high variability in viral transmission between the states and the possibility of future waves. In this study population, the frequency of asymptomatic infection was highest in the younger age groups. It was also found that the numbers of cases reported by the government were several-fold lower than the real incidence of infection. It is likely that the high number of asymptomatic cases was the main driver of this discrepancy.
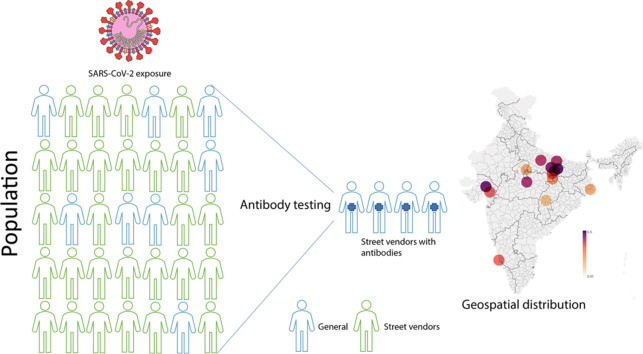
Graphical abstract
The fight against the COVID-19 pandemic continues worldwide. At this time, the number of people around the globe who have died due to infection with the causative virus – severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – is approaching seven million [1].
Before the vaccine rollout, it was highly challenging for a nation to stop the spread of this virus. Several standard precautionary measures, including strict lockdown, the use of masks, frequent hand hygiene, social distancing, contact tracing, and quarantine, have been applied widely [2,3]. Even with the introduction of the vaccine, virtually no country has yet been able to declare itself utterly free from the virus. In the early months of the pandemic, herd immunity was also considered and widely discussed [4,5]. Herd immunity against SARS-CoV-2 is a highly debated topic [2,[6], [7], [8], [9], [10]].
The first COVID-19 case in India was reported on January 30, 2020, and the total number of cases is now in excess of 45 million, with more than 0.5 million deaths [11]. Although the number of new cases is currently increasing more slowly, the three previous COVID-19 waves in India followed a perfect bell-shaped curve, with well-defined peaks in September 2020 (first wave), May 2021 (second wave), and January 2022 (third wave).
Globally, the large number of people with asymptomatic infection has added another layer of complexity, as has been the case in India [12]. Most previous studies from India have relied on mathematical modelling, which may inaccurately represent COVID-19 in the country [13], [14], [15], [16], [17]. Cases reported by the government may not represent the real number of infections in a region [11]. Within this context, random antibody testing in a population is one of the methods that can be used to obtain a real-time picture of developed immunity.
In order to understand the geodynamics of COVID-19 in India during the first wave, real-time antibody testing was performed in urban populations of 14 districts in six states during the months of September to December 2020. The aim was to estimate the level of SARS-CoV-2 infection among urban street vendors. The rationale behind this was to obtain the upper bound of seropositivity of street vendors, as they represent the most exposed cohort (Supplementary text). The Indian Council of Medical Research (ICMR) conducted a structured nationwide serosurvey on 28 000 people in May to June 2020, during the first wave, and reported seropositivity of around 1% [18]. The low seropositivity in that survey was likely due to the high frequency of samples from rural areas (0.74). In contrast, the survey presented here was conducted during September to December 2020 and focused only on urban street vendors.
The seroprevalence survey covered districts from western, northern, eastern, central, and southern regions of India: two districts in Gujarat (western region), seven districts in Uttar Pradesh (northern region), three districts in Madhya Pradesh and Chhattisgarh (central region), and a single district in each of West Bengal (eastern region) and Karnataka (southern region) (Table 1).
Table 1.
The detailed district-wise data of seroprevalence. The frequency of Government cases has been calculated by the number of reported cases/urban census. The number of times was calculated by dividing seroprevalence by the frequency of Government reported cases.
| Survey data |
Government data |
|||||||
|---|---|---|---|---|---|---|---|---|
| State | District | Survey month | Participants, n | Frequency Ab-positive (95% CI) | Frequency a | Reported cases, n | Urban Census, n | Difference in frequency between survey and government data, times (X)b (95% CI) |
| Gujarat | Ahmedabad | Dec 2020 | 50 | 0.460 (0.329-0.597) | 0.011 | 60848 | 5600000 | 42 (30-54) |
| Baroda | Dec 2020 | 50 | 0.280 (0.175-0.417) | 0.017 | 27755 | 1671000 | 17 (10-25) | |
| Uttar Pradesh | Varanasi | Sept 2020 to Dec 2020 | 406 | 0.409 (0.362-0.457) | 0.012 | 23360 | 2000000 | 35 (30-38) |
| Jaunpur | Sept 2020 to Dec 2020 | 263 | 0.441 (0.382-0.502) | 0.019 | 6697 | 347000 | 23 (20-26) | |
| Ghazipur | Sept 2020 to Dec 2020 | 128 | 0.477 (0.392-0.563) | 0.043 | 5236 | 121000 | 11 (9-13) | |
| Mirzapur | Oct 2020 | 100 | 0.300 (0.219-0.396) | 0.014 | 3441 | 246000 | 21 (16-18) | |
| Gorakhpur | Oct 2020 | 98 | 0.388 (0.297-0.487) | 0.031 | 21364 | 695000 | 13 (10-16) | |
| Lucknow | Oct 2020 | 72 | 0.375 (0.272-0.491) | 0.029 | 81276 | 2817000 | 13 (9-17) | |
| Jhansi | Nov 2020 | 100 | 0.07 (0.035-0.138) | 0.019 | 10399 | 548000 | 4 (2-7) | |
| Madhya Pradesh | Sagar | Sept 2020 to Dec 2020 | 250 | 0.392 (0.334-0.454) | 0.015 | 5367 | 370000 | 27 (22-30) |
| Singrauli | Sept 2020 to Oct 2020 | 384 | 0.154 (0.121-0.193) | 0.008 | 1907 | 227000 | 18 (15-24) | |
| Chhattishgarh | Raipur | Sept 2020 | 100 | 0.010 (0.002-0.054) | 0.047 | 53106 | 1124000 | 0.2 (0-1) |
| West Bengal | Kolkata | Dec 2020 | 100 | 0.080 (0.042-0.15) | 0.009 | 127656 | 14036000 | 9 (5-17) |
| Karnataka | Mangalore | Dec 2020 | 200 | 0.275 (0.218-0.341) | 0.054 | 33701 | 624000 | 5 (4-6) |
Ab, antibody; CI, confidence interval.
This survey performed in 14 districts of six states showed a high level of variability between the regions (Figure 1). The lowest frequency of antibody-positive people was observed in Raipur District of Chhattisgarh State (0.01, 95% confidence interval (CI) 0.002–0.054), while the maximum frequency of antibody-positive individuals was found in Ghazipur District of Uttar Pradesh State (0.477, 95% CI 0.392–0.563) (Figure 1, Table 1). The mean seroprevalence among the studied districts was 0.306 (95% CI 0.287–0.325). The high prevalence of antibodies in many districts suggests a high level of infection. However, the frequency of antibody-positive people was observed to be variable, with regions like eastern Uttar Pradesh showing a largely uniform seroprevalence (Figure 1). The mean value in this region was 0.41 (95% CI 0.38–0.44). The major districts of this region – Varanasi, Jaunpur, and Ghazipur – all had a seroprevalence frequency of >0.40. The variation among districts suggests that the spread of the virus among districts in India has been asymmetrical. Regions with a low seroprevalence may be hit by another wave in the future.
Figure 1.
(a) The geospatial frequency of antibodies in the study sampling locations. (b) Bar plot showing the seroprevalence frequency (with 95% confidence interval) in the districts studied. The districts are grouped into states (CG, Chhattishgarh; WB, West Bengal; KNTK, Karnataka).
Since the study strategy was to collect samples only from asymptomatic cases, focus was placed on those people in the streets who self-reported never having had any COVID-19 symptoms or SARS-CoV-2 RT-PCR-positive tests. Thus, all of the participants in this study were found to be asymptomatic; they did not know that they had ever been infected with SARS-CoV-2. This large number of seropositive people with an asymptomatic background suggests that a large proportion of the Indian population was asymptomatic for SARS-CoV-2 infection. There might be several known and unknown reasons behind this phenomenon. However, the high prevalence of the rs2285666-associated haplotype [19] and high proportion of the population aged ≤35 years (approximately 65%) in India are two highly likely explanations.
The cohort was divided into four age groups (16–25, 26–35, 36–45, 46–60 years) and the distribution of seropositive individuals in each of the groups was analysed (Figure 2). It was found that the frequency of asymptomatic infection was highest in the younger age groups, and this was statistically significantly (unpaired t-test, P < 0.0001). In this dataset, more than half of the asymptomatic people were in the age groups of 18–25 years and 26–35 years (0.572, 95% CI 0.535–0.608). The highest frequency of asymptomatic people was found in the 26–35 years age group (0.427, 95% CI 0.391–0.464), thus indicating the higher frequency of asymptomatic cases in the younger age population.
Figure 2.
Distribution of the study sample and frequency of seropositive people by age group.
To understand the magnitude of unreported cases, the frequency of government-reported cases was compared with the frequency of antibody-positive cases found in the present survey. A higher seroprevalence than for the reported cases was observed in all of the districts, except Raipur in Chhattisgarh (Table 1), ranging from 3.7 times to 42.3 times the government reported values (overall mean 17 times, 95% CI 13–22 times). Similar results were obtained in the comparison by state, with substantial differences observed: 40 times higher (95% CI 13–22) in Gujarat, 21 times (95% CI 13–22) in Uttar Pradesh, 23 times (95% CI 13–22) in Madhya Pradesh, 9 times (95% CI 13–22) in West Bengal, and 5 times (95% CI 13–22) in Karnataka; the rate was 0.2 times (95% CI 13–22) in Chhattisgarh. Interestingly, it was found that the cases reported by the government were highly correlated with the urban census (two-tailed, P < 0.0001). In contrast, no significant correlation was found between the antibody-positive frequency and urban census or government-reported cases.
As the sample coverage largely reflects the geography of India, an estimate of the total number of infections was made using the mean value of the difference between reported and real cases (Table 1). The mean value of difference obtained for all of the districts studied was 17 times (95% CI 13–22 times). The total number of cases in India reported up until the final revision of this article was 47 million. Hence the estimate of the true number of cases in India is 760 million (95% CI 581–983 million). However, this value should be viewed with caution, keeping in mind the low geographical coverage (14 districts), reinfection, multiple waves, and multiple testing of a single individual.
In summary, a novel approach was used in this study to estimate the seropositivity for SARS-CoV-2 among the exposed populations of 14 districts. On average, during the first wave, it was observed that every third street vendor in the majority of the districts studied had developed antibodies against SARS-CoV-2. Asymptomatic cases were more common among people of younger age. The number of asymptomatic cases in India was much higher than expected.
Acknowledgments
Acknowledgements
We are grateful to Biosense Technologies, India, for their kind help in this project. We thank Prof. George van Driem for his constructive comments. GC and RaM are supported by the Faculty Institute of Eminance (IOE BHU) (grant 6031), RT and GC are supported by SERB India (CRG/2018/001727), PPS and VS are supported by a CSIR fellowship, CBM is supported by a Wellcome Trust/DBT India Alliance Early Career Fellowship (IA/E/118/1/504338), RKM is supported by a Mahamana Post-Doctoral Fellowship BHU.
Declarations
Funding source: This work was supported by the ICMR ad-hoc grants (2021-6389) and (2021-11289).
Ethical approval: Ethical approval for this work was obtained from the ethics committees of Banaras Hindu University and VBS Purvanchal University.
Data availability: All datasets generated for this study are included in the article and Supplementary Material.
Conflict of interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Author contributions
GC conceived and designed this study. The Serosurveillance Consortium BHU, India, collected the data from the different regions of India. PPS, SKR, RK, MKS, AP, and GC analysed the data. PPS, SKR and GC wrote the manuscript with the input of the other co-authors. All authors contributed to the article and approved the submitted version.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi 10.1016/j.ijregi.2023.01.008.
Appendix. Supplementary materials
References
- 1.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jung F., Krieger V., Hufert F.T., Küpper J.-H. Herd immunity or suppression strategy to combat COVID-19. Clin. Hemorheol. Microcirc. 2020:75:13-17. doi: 10.3233/CH-209006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cominelli, Fabio, et al. ‘Textile Masks and Surface Covers—A Spray Simulation Method and a “Universal Droplet Reduction Model” Against Respiratory Pandemics.’ Frontiers in Medicine, vol. 7, 2020, doi: 10.3389/fmed.2020.00260. [DOI] [PMC free article] [PubMed]
- 4.Randolph H.E., Barreiro L.B. Herd immunity: understanding COVID-19. Immunity. 2020;52(5):737–741. doi: 10.1016/j.immuni.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Slot E., et al. Herd immunity is not a realistic exit strategy during a COVID-19 outbreak. 2020.Preprint
- 6.Anderson R.M., May R.M. Vaccination and herd immunity to infectious diseases. Nature. 1985;318(6044):323–329. doi: 10.1038/318323a0. [DOI] [PubMed] [Google Scholar]
- 7.W. Bock et al., ‘Mitigation and herd immunity strategy for COVID-19 is likely to fail,’ medRxiv, 2020.
- 8.Frederiksen L.S.F., Zhang Y., Foged C., Thakur A. The long road toward COVID-19 herd immunity: vaccine platform technologies and mass immunization strategies. Front. Immunol. 2020;11 doi: 10.3389/fimmu.2020.01817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kwok K.O., Lai F., Wei W.I., Wong S.Y.S., Tang J.W. Herd immunity–estimating the level required to halt the COVID-19 epidemics in affected countries. J. Infect. 2020;80(6):e32–e33. doi: 10.1016/j.jinf.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neagu M. The bumpy road to achieve herd immunity in COVID-19. J. Immunoassay Immunochem. 2020:1–18. doi: 10.1080/15321819.2020.1833919. [DOI] [PubMed] [Google Scholar]
- 11.“Coronavirus in India: Latest Map and Case Count.” https://www.covid19india.org (accessed May 13, 2020).
- 12.Chaubey G. Coronavirus (SARS-CoV-2) and Mortality Rate in India: The Winning Edge. Front. Public Health. 2020;8:397. doi: 10.3389/fpubh.2020.00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arti MK, Bhatnagar K. Modeling and predictions for COVID 19 spread in India. ResearchGate, DOI: DOI. 2020 Apr; 10.
- 14.Chatterjee K., Chatterjee K., Kumar A., Shankar S. Healthcare impact of COVID-19 epidemic in India: A stochastic mathematical model. Med. J. Armed Forces India. 2020;76(2):147–155. doi: 10.1016/j.mjafi.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chatterjee S., Sarkar A., Chatterjee S., Karmakar M., Paul R. Studying the progress of COVID-19 outbreak in India using SIRD model. Indian J. Phys. 2020:1–17. doi: 10.1007/s12648-020-01766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.S. Mukhopadhyay and D. Chakraborty, ‘Estimation of undetected COVID-19 infections in India,’ medRxiv, 2020.
- 17.Tiwari A. Modelling and analysis of COVID-19 epidemic in India. J. Saf. Sci. Resil. 2020;1(2):135–140. [Google Scholar]
- 18.Murhekar M.V., et al. Prevalence of SARS-CoV-2 infection in India: Findings from the national serosurvey, May-June 2020. Indian J. Med. Res. 2020;152(1):48. doi: 10.4103/ijmr.IJMR_3290_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Srivastava A., et al. Most frequent South Asian haplotypes of ACE2 share identity by descent with East Eurasian populations. PLOS ONE. Sep. 2020;15(9) doi: 10.1371/journal.pone.0238255. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.