Abstract
Background
Although the outcome of cardiopulmonary resuscitation (CPR) is still unsatisfactory, there are few studies about temporal trends of in‐hospital CPR incidence and mortality. We aimed to evaluate nationwide trends of in‐hospital CPR incidence and its associated risk factors and mortality in pediatric patients using a database of the Korean National Health Insurance between 2012 and 2018.
Methods and Results
We excluded neonates and neonatal intensive care unit admissions. Incidence of in‐hospital pediatric CPR was 0.58 per 1000 admissions (3165 CPR/5 429 471 admissions), and the associated mortality was 50.4%. Change in CPR incidence according to year was not significant in an adjusted analysis (P=0.234). However, CPR mortality increased significantly by 6.6% every year in an adjusted analysis (P<0.001). Hospitals supporting pediatric critical care showed 37.7% lower odds of CPR incidence (P<0.001) and 27.5% lower odds of mortality compared with other hospitals in the adjusted analysis (P<0.001), and they did not show an increase in mortality (P for trend=0.882).
Conclusions
Temporal trends of in‐hospital CPR mortality worsened in Korea, and the trends differed according to subgroups. Study results highlight the need for ongoing evaluation of CPR trends and for further CPR outcome improvement among hospitalized children.
Keywords: cardiac arrest, epidemiology, in‐hospital mortality, national health insurance, pediatric critical care, risk management, trend
Subject Categories: Cardiopulmonary Arrest, Epidemiology, Pediatrics
NonStandard Abbreviations and Acronyms
- HIRA
Health Insurance Review and Assessment
- KNHI
Korean National Health Insurance
- PCC
pediatric critical care
Clinical Perspective.
What Is New?
This study revealed an increasing trend in pediatric in‐hospital cardiopulmonary resuscitation (CPR) mortality rate in Korea.
The worsening mortality trends were significant in children with prolonged CPR duration (15 minutes) and hospitals without pediatric critical care support.
What Are the Clinical Implications?
In‐hospital CPR mortality has worsened even with advances in medical knowledge and technology.
Evaluation of CPR trends and affecting structures, including human and hospital resources, are required for CPR outcome improvement.
In‐hospital pediatric cardiac arrest is usually related to the progression of underlying conditions or shock, 1 while out‐of‐hospital cardiac arrest usually has an etiology related to drowning, sudden unexpected infantile death, or cardiac arrhythmia. 2 Between 0.1% and 0.9% of pediatric hospital admissions and 2% to 6% of children admitted to pediatric intensive care units (ICU) require cardiopulmonary resuscitation (CPR). 3 , 4 , 5 , 6 , 7 Although there is a lack of nationwide studies, a systematic review reported that survival to discharge after in‐hospital pediatric CPR was only 46% (upper and lower limits of 11% and 80%). 6 Since the outcomes of in‐hospital CPR are unsatisfactory, efforts are being made to improve them.
As part of the effort, CPR guidelines based on the International Liaison Committee on Resuscitation recommendations have been published to advance resuscitation knowledge and practices. 8 , 9 Large‐scale US studies demonstrated an improving trend in survival to hospital discharge after in‐hospital cardiac arrest, which was explained by an improvement in acute resuscitation survival. 10 , 11 A subsequent US study demonstrated a stagnating survival of pulseless cardiac arrest since 2010. 12 However, trend studies in other countries are hard to find. Changes in the medical environment may also affect in‐hospital CPR outcomes. Implementation of a rapid response system, increase in the number of technology‐dependent children, or development of pediatric critical care support may affect the incidence or outcomes of pediatric resuscitation. 13 , 14 , 15 Although the effects of change in medical environment may differ among hospitals or countries, trend studies of CPR on a nationwide scale are lacking, and Asian trends of in‐hospital CPR incidence and outcomes are not known.
We aimed to evaluate trends of in‐hospital CPR incidence and survival to discharge in pediatric patients and the risk factors associated with CPR incidence and mortality.
Methods
The data used in this analysis are available through the Korean Health Insurance Review & Assessment Service with an approved proposal.
Study Population and Design
This population‐based retrospective cohort study was based on the Health Insurance Review and Assessment (HIRA) from the Korean Ministry of Health. The HIRA database comprises reimbursement claims to the Korean National Health Insurance (KNHI) and Medical Aid Program. KNHI covers ≈97% of the Korean population, and the Medical Aid Program covers the remaining 3% who cannot afford the KNHI. Consequently, the HIRA database covers all therapeutic procedures and prescriptions from inpatient and outpatient visits.
We screened patients admitted to ward/ICU or emergency department from age 0 to 18 years between January 2012 and December 2018 (7 years). The KNHI system defined admission to emergency department as a longer than 6‐hour stay in the emergency room or a stay in a monitoring unit. For selection of in‐hospital CPR among the pediatric population, we defined in‐hospital admissions as those to general ward or ICU (presence of ward/ICU claim codes) or emergency department stay for >24 hours. Among in‐hospital admissions, the neonatal population (<1 month age) was excluded because of ambiguity about individual identification and different characteristics of neonatal resuscitation. Admissions to an emergency department for <24 hours without ward/ICU admission were excluded according to the operational definition of in‐hospital admission. In‐hospital CPRs from the remaining admissions were included in this study.
The study was reviewed by the Institutional Review Board of Samsung Medical Center (protocol 2022‐06‐103), and informed consent was exempted because only previously collected, deidentified administrative data were used.
Measurement
In‐Hospital CPR and Mortality
The primary outcome was the trends of incidence and mortality of in‐hospital CPR. Admissions with at least 1 CPR claim code (KNHI procedure codes: M1583, M1584, M1585, M1586, M1587, M5871, M5873, M5874, M5875, M5876, and M5877) were recorded as admissions with in‐hospital CPR. Multiple CPR codes at admission were counted as 1 CPR admission, and CPR duration was recorded according to the longest duration of the claimed CPR code at the admission. The results of survival hospital discharges were obtained from the HIRA admission database.
Other Variables
The KNHI claim database was used to identify demographic characteristics, hospital information, and procedures. The KNHI database adopted the International Classification of Disease, Tenth Revision (ICD‐10) as a diagnostic classification, and we defined primary diagnosis using the ICD‐10 as in previous studies. 16 , 17 Information on hospital type was obtained from the HIRA Medical Care Institution Database, which classifies hospitals into tertiary, general, and local hospitals as described in a previous study. 16 ICU admissions (AJ001‐AJ590) and other mechanical ventilation (M5850‐M5860) were defined by KNHI procedure codes regardless of before and after CPR. Shockable CPR was defined as CPR with defibrillation (KNHI code: M5880). Hospitals supporting pediatric critical care (PCC hospitals) were defined as hospitals with the presence of pediatric ICU admission codes (AJ004, AJ005, AJ008, AJ009, AJ043, AJ044, AJ045, and AJ046), which differentiate pediatric ICU admissions from adult ICU admissions.
Statistical Analysis
Median with interquartile range and number with percentage were used to describe the distribution of continuous variables and categorical variables, respectively. Chi‐square test was used for comparison of categorical variables. Univariable and multivariable logistic regression analyses were used to estimate the risk factors of CPR incidence and mortality. In the multivariable regression analysis, we adjusted for age (categorical variable in incidence analysis and continuous variable in mortality analysis), sex, year of CPR event, hospital type (tertiary, general, and primary), PCC hospital, use of mechanical ventilation, and underlying malignancy. P for trend was obtained for changes in incidence and mortality of CPR using the Cochrane‐Armitage test. A P value <0.05 was considered significant for all analyses. Statistical analyses were performed using SAS Visual Analytics.
Results
Among 7 253 666 pediatric admissions, 1 104 513 were excluded for neonate age or neonatal ICU admission, and 719 682 were excluded because they stayed in emergency department for <24 hours and were not admitted to ward or ICU (Figure S1). Among the 5 429 471 included admissions, the total number of pediatric in‐hospital CPR events between 2012 and 2018 was 3165. The median patient age was 2 years, and the most common primary diagnosis was circulatory disease (633 admissions, 20.0%) which included myocarditis, cardiomyopathy, and arrhythmia (Table 1). In total, 506 admissions (16.0%) were shockable CPR, and 68.7% of patients were admitted to an ICU during admission. CPR duration was <15 minutes in 1622 (51.3%) events. PCC hospitals managed 44.8% (1419) of CPR during the study period (Table 1).
Table 1.
Characteristics of Patients Receiving Cardiopulmonary Resuscitation (n=3165)
| Characteristics | Patient number (%) and median (IQR) |
|---|---|
| Demographic characteristics | |
| Age, y | 2 (0.9–10) |
| Sex, male | 1834 (58.0%) |
| Primary diagnosis | |
| Circulatory | 633 (20.0%) |
| Congenital anomaly | 457 (14.4%) |
| Neurologic | 384 (12.1%) |
| Malignancy | 377 (14.4%) |
| Respiratory | 345 (10.9%) |
| Injury | 209 (6.6%) |
| Infectious | 138 (4.4%) |
| Perinatal | 113 (3.6%) |
| Gastrointestinal | 85 (2.7%) |
| Hematologic | 78 (2.5%) |
| Event characteristics | |
| Location | |
| ICU | 2157 (68.7%) |
| Non‐ICU | 990 (31.3%) |
| Rhythm | |
| Shockable | 506 (16.0%) |
| Nonshockable | 2659 (84.0%) |
| Duration | |
| <15 min | 1622 (51.3%) |
| >15 min | 1543 (48.8%) |
| Hospital characteristics | |
| Hospital type | |
| Tertiary | 2199 (69.5%) |
| General | 932 (29.4%) |
| Local | 34 (1.1%) |
| PCC hospital | |
| Yes | 1419 (44.8%) |
| No | 1746 (55.2%) |
ICU indicates intensive care unit; IQR, interquartile range; and PCC, pediatric critical care.
Among the 5 429 471 pediatric hospital admissions, the incidence of CPR was highest (1.40 per 1000 admissions) in infants (<1 year), while mortality (40.5%) was lowest (Table 2). The incidence of CPR was higher in PCC hospitals than in hospitals not supporting PCC (no‐PCC hospitals) (2.16 versus 0.37 per 1000 admission, P<0.001). Mortality of CPR was lower in PCC hospitals than in no‐PCC hospitals (45.1% versus 54.8%, P<0.001) (Table 2).
Table 2.
Incidence and Mortality of Cardiopulmonary Resuscitation According to the Characteristics
| Variable | Total admissions, n | CPR, n (per 1000 admissions) | P value | Mortality (%) | P value |
|---|---|---|---|---|---|
| Overall | 5 429 471 | 3165 (0.58) | 1596 (50.4%) | ||
| Sex | 0.146 | 0.038 | |||
| Male | 3 076 724 | 1834 (0.60) | 896 (48.9%) | ||
| Female | 2 352 747 | 1331 (0.57) | 700 (52.6%) | ||
| Age | <0.001 | <0.001 | |||
| <1 y | 765 065 | 1076 (1.40) | 436 (40.5%) | ||
| 1–12 y | 3 796 036 | 1465 (0.39) | 784 (53.5%) | ||
| ≥13 y | 868 370 | 624 (0.72) | 376 (60.3%) | ||
| Hospital type | <0.001 | <0.001 | |||
| Tertiary | 1 496 187 | 2199 (1.47) | 1062 (48.3%) | ||
| General | 2 806 599 | 932 (0.33) | 520 (55.8%) | ||
| Primary | 1 126 685 | 34 (0.03) | 14 (41.2%) | ||
| PCC hospital | <0.001 | <0.001 | |||
| Yes | 654 597 | 1419 (2.16) | 640 (45.1%) | ||
| No | 4 774 874 | 1746 (0.37) | 956 (54.8%) | ||
| Mechanical ventilation use | <0.001 | <0.001 | |||
| Yes | 24 441 | 2366 (88.3) | 1325 (56.0%) | ||
| No | 5 405 030 | 799 (0.15) | 271 (33.9%) | ||
| Shockable | <0.001 | 0.005 | |||
| Yes | 979 | 506 (340.74) | 287 (56.7%) | ||
| No | 5 428 492 | 2659 (0.49) | 1309 (49.2%) | ||
| ICU admission | <0.001 | <0.001 | |||
| Yes | 44 526 | 2175 (46.57) | 1158 (53.2%) | ||
| No | 5 384 945 | 990 (0.18) | 438 (44.2%) | ||
| Underling malignancy | <0.001 | <0.001 | |||
| Yes | 190 828 | 377 (1.97) | 258 (68.4%) | ||
| No | 5 238 643 | 2788 (0.53) | 1338 (48.0%) |
CPR indicates cardiopulmonary resuscitation; ICU, intensive care unit; and PCC, pediatric critical care.
CPR incidence was associated with mechanical ventilation use (88.3 vesus 0.15 per 1000 admissions, P<0.001), ICU admissions (46.57 versus 0.18 per 1000 admissions, P<0.001), and primary diagnosis of malignancy (1.97 versus 0.53, P<0.001). CPR mortality was also associated with mechanical ventilation use (56.0 versus 33.9, P<0.001), ICU admissions (53.2 versus 44.2%, P<0.001), and malignancy (68.4 versus 48.0%, P<0.001). A shockable rhythm was identified in 506 (16.0%) of total CPR admissions and showed 56.7% mortality, which was significantly higher than the mortality of 49.2% in nonshockable CPR (P=0.005) (Table 2).
Incidence and mortality of CPR changed with age. The CPR mortality increased from 40.5% in patients aged 0 to 55.7% in patients aged 17 years (P for trend<0.001). The incidence of CPR peaked at age 0, with an incidence of 1.40/1000 admissions. The incidence of CPR then decreased to 0.40/1000 admissions at age 1 and increased again at age 17 to 0.76/1000 admissions (Figure 1).
Figure 1. Incidence and mortality of cardiopulmonary resuscitation by age.
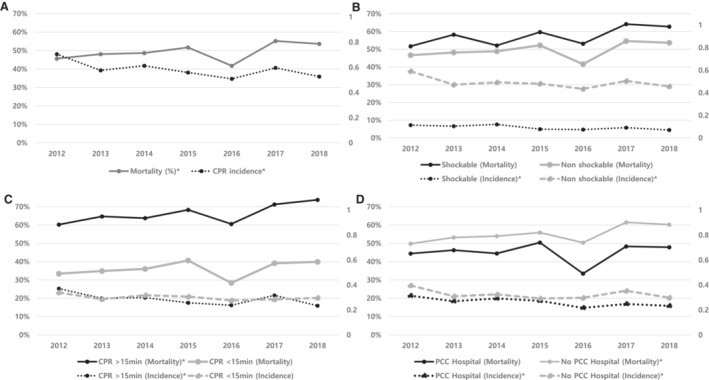
X‐axis indicates age (year) of patients. Left, y‐axis indicates mortality (%). Right, y‐axis indicates incidence of cardiopulmonary resuscitation per 1000 hospital admissions‐year. CPR indicates cardiopulmonary resuscitation.
Throughout the study (from 2012–2018), overall CPR incidence decreased (P for trend<0.001), while the overall CPR mortality increased (P for trend=0.026) (Table S1) (Figure 2). CPR incidence decreased over time regardless of initial rhythm, or PCC hospital (P for trends<0.05). However, statistically significant trends in increasing mortality were observed in CPR duration of >15 minutes (P for trend=0.002), and no‐PCC hospitals (P for trend=0.036) (Figure 2) (Table S1).
Figure 2. Trends of incidence and mortality of cardiopulmonary resuscitation (CPR).
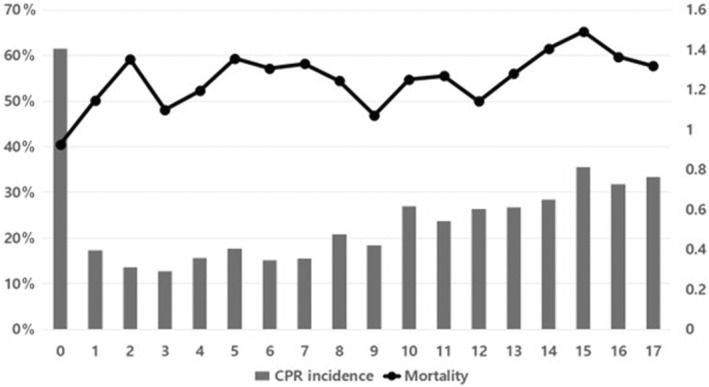
A, Overall. B, Shockable vs nonshockable. C, CPR duration <15 minutes vs CPR duration >15 minutes. D, CPR event in pediatric critical care supported hospitals vs not supported hospitals. X‐axis indicates year of CPR. Left, y‐axis indicates mortality (solid lines) (%). Right, y‐axis indicates incidence (dotted lines) of CPR per 1000 hospital admissions‐year. CPR indicates cardiopulmonary resuscitation, and PCC; pediatric critical care. *Indicates P for trends<0.05.
With each year of the study, CPR decreased by 3.7% (P<0.001) in the univariable regression analysis. This reducing effect of “year of CPR” was lost in multivariable analysis (P=0.234) (Table 3). PCC hospitals had higher CPR incidence (odds ratio [OR], 5.939 [95% CI, 5.537–6.370]) in univariable analysis, but it was a reducing factor of CPR incidence in multivariable regression analysis (OR, 0.623 [95% CI, 0.570–0.682]).
Table 3.
Logistic Regression Analysis for Incidence of Cardiopulmonary Resuscitation
| Parameter | Univariable | Multivariable* | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | P value | Odds ratio | 95% CI | P value | |
| Year of CPR | 0.963 | (0.946–0.980) | <0.001 | 0.989 | (0.971–1.007) | 0.243 |
| Sex (reference=M) | 0.949 | (0.884–1.018) | 0.146 | 0.954 | (0.886–1.027) | 0.209 |
| Age, y | ||||||
| <1 (reference) | 1 | 1 | ||||
| 1–12 | 0.274 | (0.253–0.297) | <0.001 | 0.751 | (0.689–0.818) | <0.001 |
| ≥13 | 0.511 | (0.463–0.564) | <0.001 | 1.012 | (0.908–1.128) | 0.826 |
| Hospital type | ||||||
| Tertiary (reference) | 1 | 1 | ||||
| General | 0.226 | (0.209–0.244) | <0.001 | 0.842 | (0.766–0.927) | <0.001 |
| Primary | 0.021 | (0.015–0.029) | <0.001 | 0.149 | (0.125–0.211) | <0.001 |
| PCC hospital | 5.939 | (5.537–6.370) | <0.001 | 0.623 | (0.570–0.682) | <0.001 |
| Mechanical ventilation use | 724.885 | (668.30–786.26) | <0.001 | 481.188 | (408.99–566.11) | <0.001 |
| ICU admission | 279.305 | (258.93–301.28) | <0.001 | 1.353 | (1.162–1.576) | <0.001 |
| Underlying malignancy | 0.269 | (0.242–0.300) | <0.001 | 2.082 | (1.846–2.349) | <0.001 |
CPR indicates cardiopulmonary resuscitation; ICU, intensive care unit; and PCC, pediatric critical care.
The model adjusted for year of cardiopulmonary resuscitation, sex, age (as categorical variables), hospital type, pediatric critical care hospital, mechanical ventilation use, intensive care unit admission, and underlying malignancy.
CPR mortality increased by 4.0% each study year (P=0.026) in univariable logistic regression analysis and by 6.6% each study year (P<0.001) in multivariable logistic analysis. ICU admission had a 43.5% increased odds of CPR mortality in univariable analysis but was a 19.4% odds‐reducing factor of CPR mortality in multivariable analysis (Table 4).
Table 4.
Logistic Regression Analysis for the Mortality Risk of Cardiopulmonary Resuscitation
| Parameter | Univariable | Multivariable* | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | P value | Odds ratio | 95% CI | P value | |
| Year of CPR | 1.040 | (1.005–1.077) | 0.026 | 1.066 | (1.028–1.106) | <0.001 |
| Sex (reference=M) | 1.161 | (1.008–1.337) | 0.038 | 1.224 | (1.056–1.419) | 0.007 |
| Age, y | 1.043 | (1.030–1.056) | <0.001 | 1.031 | (1.018–1.045) | <0.001 |
| Hospital type | ||||||
| Tertiary (reference) | 1.000 | 1.000 | ||||
| General | 1.351 | (1.158–1.576) | <0.001 | 1.253 | (1.052–1.493) | 0.012 |
| Primary | 0.749 | (0.377–1.491) | 0.411 | 0.984 | (0.474–2.045) | 0.966 |
| PCC hospital | 0.679 | (0.590–0.782) | <0.001 | 0.725 | (0.616–0.853) | <0.001 |
| Mechanical ventilation use | 2.480 | (2.097–2.932) | <0.001 | 3.152 | (2.510–3.958) | <0.001 |
| ICU admission | 1.435 | (1.234–1.669) | <0.001 | 0.806 | (0.652–0.997) | 0.046 |
| Underlying malignancy | 2.347 | (1.866–2.958) | <0.001 | 2.676 | (2.090–3.427) | <0.001 |
CPR indicates cardiopulmonary resuscitation; ICU, intensive care unit; and PCC, pediatric critical care.
The model adjusted for year of cardiopulmonary resuscitation, sex, age (as categorical variables), hospital type, pediatric critical care hospital, mechanical ventilation use, intensive care unit admission, and underlying malignancy.
Discussion
This nationwide population‐based study revealed that pediatric in‐hospital CPR mortality has increased over time while pediatric in‐hospital CPR incidence did not change significantly in an adjusted analysis between 2012 and 2018. However, PCC hospitals did not show an increasing trend in CPR mortality, and admissions to PCC hospitals were a significant reducing factor in CPR incidence and mortality in the adjusted analysis.
The incidence of in‐hospital CPR in this study (0.58 per 1000 admissions) was similar to that of the United States (0.78 per 1000 admissions) but lower than those of previous studies in Austria (0.1%), Taiwan (0.9%), Finland (0.7%), and Brazil (2%). 4 , 5 , 11 , 18 , 19 , 20 The difference in incidence may arise from the study designs, including age range, hospital types, and definition of in‐hospital patients. Studies (except the US study) included only tertiary hospitals where the severity of patients is expected to be high. However, we included all hospital types in Korea. In our study, the incidence of CPR among tertiary hospital admissions was 0.15%, which was similar to the 0.1% seen in Austria (Table 2).
The pediatric in‐hospital CPR incidence decreased over the years of this study. Although studies on the time trend of pediatric CPR incidence are scarce, a large‐scale study in the United States showed the opposite results. 11 In the US study, they suspected that their increasing trend of in‐hospital CPR was attributable to the increase in illness severity of in‐patients associated with increased critical care stays and decreased non‐critical care stays. 15 , 21 However, we suspect that the decreasing trend of CPR incidence in Korea was attributable to demographic changes of age rather than improved care quality. In Korea, the fertility rate is significantly declining. 22 The proportion of infants whose CPR incidence was highest decreased over the study years (Figure 1) (Figure S2). When we adjusted for age and other confounding factors, the decreasing trend in CPR over time lost statistical significance (Table 3).
In‐hospital CPR mortality (50.4%) in this study was similar to that of the US study (45%–50%) whose study population included 50% of pulseless cardiac arrest and 50% of bradycardia with poor perfusion. 1 , 23 This survival rate is higher than the survival (32%) of children under pulseless cardiac arrest. 12 However, CPR mortality varied according to the study population and inclusion of studies: Brazil (85.3%), Africa (78.1%), and Spain (66.7%). 20 , 24 , 25
The mortality of pediatric in‐hospital CPR increased during the study period. This is contrary to previous studies from the United States and Spain, where CPR mortality decreased from 86% to 61% and 74.1% to 59%, respectively, over 10 years. 10 , 11 , 12 , 26 A recent study showed that in‐hospital pediatric CPR mortality did not improve from 2009 to 2017 in the United States. 12 Our findings on mortality trends throughout the study period were unexpected. The decreasing number of infants could be a cause of overall mortality increase since CPR mortality was low in infants. However, mortality in patients who had CPR increased each year even after adjusting for age and other confounding factors (Table 4). Increased severity might be a cause of increasing mortality. In the US study, they described severity as a cause of increasing CPR incidence, but CPR mortality did not change. 11 There was a possible safety issue during the study period. In 2017, the resident duty hour regulation was fully implemented in Korea. 27 Although activation of the resident well‐being law was gradually implemented from 2014 onward, hospitals could not hire more doctors to compensate for reduced work hours. The decreased number of doctors working day and night duty left concerns that an insufficient number of doctors in a CPR team, absence of a senior doctor to lead CPR, and short resident education time might affect patient safety. Further studies are required to evaluate these potential safety issues, since CPR mortality increased by 6.6% every year in adjusted multivariable analysis.
Patient safety of children could also be affected by hospital policy. Hospitals not supporting pediatric critical care without a dedicated pediatric ICU (no‐PCC hospitals) showed significant increasing trends in mortality (Figure 2) (Table S1). These results may be partly attributable to the absence of a rapid response system. In Korea, a rapid response team is not reimbursed by the KNHI system. As a result, no‐PCC hospitals do not have a pediatric rapid response team, and only some PCC hospitals have ICU outreach teams responding to pediatric early warning signs. In another subgroup analysis, CPR with duration >15 minutes was more problematic than shorter CPR times. We suspect that advanced life support may not have been successful for patients who could not recover from basic life support. Prolonged CPR requires a medical team with specialized skills and equipment including advanced airway management, 28 , 29 which could be supported by the pediatric critical care team. One study reported that presence of pediatric residents and fellows improved 24‐hour survival for pediatric in‐hospital CPR. 30 The presence of a pediatric ICU with critical care fellowship programs was also associated with a decreased mortality rate. 31 , 32 In our study, PCC hospitals showed a 27.5% lower CPR mortality compared with no‐PCC hospitals in multivariable analysis. However, unlike in the United States where 257 pediatric ICUs exist, only 11 hospitals support pediatric ICUs in Korea. 33
Our study has some limitations. First, the national database used in this study collects data for administrative purposes and does not contain laboratory or clinical information. Therefore, we could not apply Utstein‐style recommendations and definitions to our data description such as causes of cardiac arrest. 34 Second, palliative discharges were not evaluated which might affect CPR survival rate. However, palliative discharges of critically ill children are rare, and few children (6.7%) die at home even in chronic complex conditions in Korea. 35 , 36 Third, this study data may not apply to other countries where the medical environment is different. Despite these limitations, the strength of this study lies in the nationwide collection of data from all hospital types in all socioeconomic and population regions over 7 years. Unlike previous studies that do not include hospitals without a quality improvement system, this study includes all hospitals without selection bias and represents the whole country.
Our findings also have implications for management of CPR and policymaking. CPR mortality could worsen over time even in an era of advanced medical technology. If you cannot measure it, you cannot improve it. Therefore, it is important to evaluate trends in CPR outcomes and measure‐related processes and structures. 37 Pediatric critical care might be one of the related structural factors affecting CPR outcomes.
In conclusion, CPR incidence and mortality have changed throughout the years in Korea. CPR incidence may be affected by changing patient demographics. Worsening CPR mortality highlights the need for ongoing evaluation of CPR trend and for further CPR outcome improvement among hospitalized children.
Sources of Funding
None.
Disclosures
None.
Supporting information
Table S1
Figures S1–S2
J. Choi and A. Y. Choi contributed equally and are co‐first authors.
For Sources of Funding and Disclosures, see page 8.
Contributor Information
Meong Hi Son, Email: meonghi.son@samsung.com.
Joongbum Cho, Email: joongbum.cho@gmail.com.
References
- 1. Morgan RW, Kirschen MP, Kilbaugh TJ, Sutton RM, Topjian AA. Pediatric in‐hospital cardiac arrest and cardiopulmonary resuscitation in the United States: a review. JAMA Pediatr. 2021;175:293–302. doi: 10.1001/jamapediatrics.2020.5039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Meert KL, Telford R, Holubkov R, Slomine BS, Christensen JR, Dean JM, Moler FW. Pediatric out‐of‐hospital cardiac arrest characteristics and their association with survival and neurobehavioral outcome. Pediatr Crit Care Med. 2016;17:e543–e550. doi: 10.1097/pcc.0000000000000969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hamzah M, Othman HF, Almasri M, Al‐Subu A, Lutfi R. Survival outcomes of in‐hospital cardiac arrest in pediatric patients in the USA. Eur J Pediatr. 2021;180:2513–2520. doi: 10.1007/s00431-021-04082-3 [DOI] [PubMed] [Google Scholar]
- 4. Tibballs J, Kinney S. A prospective study of outcome of in‐patient paediatric cardiopulmonary arrest. Resuscitation. 2006;71:310–318. doi: 10.1016/j.resuscitation.2006.05.009 [DOI] [PubMed] [Google Scholar]
- 5. Suominen P, Olkkola KT, Voipio V, Korpela R, Palo R, Räsänen J. Utstein style reporting of in‐hospital paediatric cardiopulmonary resuscitation. Resuscitation. 2000;45:17–25. doi: 10.1016/s0300-9572(00)00167-2 [DOI] [PubMed] [Google Scholar]
- 6. Bimerew M, Wondmieneh A, Gedefaw G, Gebremeskel T, Demis A, Getie A. Survival of pediatric patients after cardiopulmonary resuscitation for in‐hospital cardiac arrest: a systematic review and meta‐analysis. Ital J Pediatr. 2021;47:118. doi: 10.1186/s13052-021-01058-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tress EE, Kochanek PM, Saladino RA, Manole MD. Cardiac arrest in children. J Emerg Trauma Shock. 2010;3:267–272. doi: 10.4103/0974-2700.66528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Van de Voorde P, Turner NM, Djakow J, de Lucas N, Martinez‐Mejias A, Biarent D, Bingham R, Brissaud O, Hoffmann F, Johannesdottir GB, et al. European Resuscitation Council guidelines 2021: paediatric life support. Resuscitation. 2021;161:327–387. doi: 10.1016/j.resuscitation.2021.02.015 [DOI] [PubMed] [Google Scholar]
- 9. Topjian AA, Raymond TT, Atkins D, Chan M, Duff JP, Joyner BL Jr, Lasa JJ, Lavonas EJ, Levy A, Mahgoub M, et al. Part 4: pediatric basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S469–S523. doi: 10.1161/CIR.0000000000000901 [DOI] [PubMed] [Google Scholar]
- 10. Girotra S, Spertus JA, Li Y, Berg RA, Nadkarni VM, Chan PS. Survival trends in pediatric in‐hospital cardiac arrests: an analysis from Get With the Guidelines‐Resuscitation. Circ Cardiovasc Qual Outcomes. 2013;6:42–49. doi: 10.1161/circoutcomes.112.967968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Martinez PA, Totapally BR. The epidemiology and outcomes of pediatric in‐hospital cardiopulmonary arrest in the United States during 1997 to 2012. Resuscitation. 2016;105:177–181. doi: 10.1016/j.resuscitation.2016.06.010 [DOI] [PubMed] [Google Scholar]
- 12. Holmberg MJ, Wiberg S, Ross CE, Kleinman M, Hoeyer‐Nielsen AK, Donnino MW, Andersen LW. Trends in survival after pediatric in‐hospital cardiac arrest in the United States. Circulation. 2019;140:1398–1408. doi: 10.1161/CIRCULATIONAHA.119.041667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brilli RJ, Gibson R, Luria JW, Wheeler TA, Shaw J, Linam M, Kheir J, McLain P, Lingsch T, Hall‐Haering A, et al. Implementation of a medical emergency team in a large pediatric teaching hospital prevents respiratory and cardiopulmonary arrests outside the intensive care unit. Pediatr Crit Care Med. 2007;8:236–246; quiz 247. doi: 10.1097/01.PCC.0000262947.72442.EA [DOI] [PubMed] [Google Scholar]
- 14. Slonim AD, Patel KM, Ruttimann UE, Pollack MM. The impact of prematurity: a perspective of pediatric intensive care units. Crit Care Med. 2000;28:848–853. doi: 10.1097/00003246-200003000-00040 [DOI] [PubMed] [Google Scholar]
- 15. Halpern NA, Pastores SM. Critical care medicine in the United States 2000‐2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;38:65–71. doi: 10.1097/CCM.0b013e3181b090d0 [DOI] [PubMed] [Google Scholar]
- 16. Jung M, Park H, Kang D, Park J, Jeon K, Chung CR, Yang JH, Cho YH, Suh GY, Guallar E, et al. Age‐specific distribution of diagnosis and outcomes of children admitted to ICUs: a population‐based cohort study. Pediatr Crit Care Med. 2019;20:e301–e310. doi: 10.1097/pcc.0000000000001978 [DOI] [PubMed] [Google Scholar]
- 17. Jung M, Park H, Kang D, Park E, Jeon K, Chung CR, Yang JH, Suh GY, Guallar E, Cho J, et al. The effect of bed‐to‐nurse ratio on hospital mortality of critically ill children on mechanical ventilation: a nationwide population‐based study. Ann Intensive Care. 2020;10:159. doi: 10.1186/s13613-020-00780-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. de Mos N, van Litsenburg RR, McCrindle B, Bohn DJ, Parshuram CS. Pediatric in‐intensive‐care‐unit cardiac arrest: incidence, survival, and predictive factors. Crit Care Med. 2006;34:1209–1215. doi: 10.1097/01.CCM.0000208440.66756.C2 [DOI] [PubMed] [Google Scholar]
- 19. Wu ET, Li MJ, Huang SC, Wang CC, Liu YP, Lu FL, Ko WJ, Wang MJ, Wang JK, Wu MH. Survey of outcome of CPR in pediatric in‐hospital cardiac arrest in a medical center in Taiwan. Resuscitation. 2009;80:443–448. doi: 10.1016/j.resuscitation.2009.01.006 [DOI] [PubMed] [Google Scholar]
- 20. Reis AG, Nadkarni V, Perondi MB, Grisi S, Berg RA. A prospective investigation into the epidemiology of in‐hospital pediatric cardiopulmonary resuscitation using the international Utstein reporting style. Pediatrics. 2002;109:200–209. doi: 10.1542/peds.109.2.200 [DOI] [PubMed] [Google Scholar]
- 21. Halpern NA, Pastores SM, Thaler HT, Greenstein RJ. Changes in critical care beds and occupancy in the United States 1985‐2000: differences attributable to hospital size. Crit Care Med. 2006;34:2105–2112. doi: 10.1097/01.CCM.0000227174.30337.3E [DOI] [PubMed] [Google Scholar]
- 22. Yun J, Son S‐H, Bae C‐W. Trends and changes of maternal age at live birth and related statistics in Korea (1981–2019). Perinatology. 2021;32:67–74. doi: 10.14734/PN.2021.32.2.67 [DOI] [Google Scholar]
- 23. Knudson JD, Neish SR, Cabrera AG, Lowry AW, Shamszad P, Morales DL, Graves DE, Williams EA, Rossano JW. Prevalence and outcomes of pediatric in‐hospital cardiopulmonary resuscitation in the United States: an analysis of the kids' inpatient database*. Crit Care Med. 2012;40:2940–2944. doi: 10.1097/CCM.0b013e31825feb3f [DOI] [PubMed] [Google Scholar]
- 24. Olotu A, Ndiritu M, Ismael M, Mohammed S, Mithwani S, Maitland K, Newton CR. Characteristics and outcome of cardiopulmonary resuscitation in hospitalised African children. Resuscitation. 2009;80:69–72. doi: 10.1016/j.resuscitation.2008.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lopez‐Herce J, Garcia C, Dominguez P, Carrillo A, Rodriguez‐Nunez A, Calvo C, Delgado MA; Spanish Study Group of Cardiopulmonary Arrest in Children. Characteristics and outcome of cardiorespiratory arrest in children. Resuscitation. 2004;63:311–320. doi: 10.1016/j.resuscitation.2004.06.008 [DOI] [PubMed] [Google Scholar]
- 26. Lopez‐Herce J, del Castillo J, Canadas S, Rodriguez‐Nunez A, Carrillo A; Spanish Study Group of Cardiopulmonary Arrest in Children . In‐hospital pediatric cardiac arrest in Spain. Rev Esp Cardiol (Engl Ed). 2014;67:189–195. doi: 10.1016/j.rec.2013.07.017 [DOI] [PubMed] [Google Scholar]
- 27. Han ER, Chung EK. The perception of medical residents and faculty members on resident duty hour regulation. Korean J Med Educ. 2020;32:67–72. doi: 10.3946/kjme.2020.154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kendirli T, Caltik A, Duman M, Yilmaz HL, Yildizdas D, Bosnak M, Tekin D, Atay N. Effect of pediatric advanced life support course on pediatric residents' intubation success. Pediatr Int. 2011;53:94–99. doi: 10.1111/j.1442-200X.2010.03128.x [DOI] [PubMed] [Google Scholar]
- 29. Topjian AA, Raymond TT, Atkins D, Chan M, Duff JP, Joyner BL, Lasa JJ, Lavonas EJ, Levy A, Mahgoub M, et al. Part 4: pediatric basic and advanced life support 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2021;147:e2020038505D. doi: 10.1542/peds.2020-038505D [DOI] [PubMed] [Google Scholar]
- 30. Donoghue AJ, Nadkarni VM, Elliott M, Durbin D; American Heart Assocation National Registry of Cardiopulmonary Resuscitation I . Effect of hospital characteristics on outcomes from pediatric cardiopulmonary resuscitation: a report from the National Registry of Cardiopulmonary Resuscitation. Pediatrics. 2006;118:995–1001. doi: 10.1542/peds.2006-0453 [DOI] [PubMed] [Google Scholar]
- 31. Pollack MM, Patel KM, Ruttimann E. Pediatric critical care training programs have a positive effect on pediatric intensive care mortality. Crit Care Med. 1997;25:1637–1642. doi: 10.1097/00003246-199710000-00011 [DOI] [PubMed] [Google Scholar]
- 32. Pollack MM, Cuerdon TT, Patel KM, Ruttimann UE, Getson PR, Levetown M. Impact of quality‐of‐care factors on pediatric intensive care unit mortality. JAMA. 1994;272:941–946. doi: 10.1001/jama.1994.03520120051030 [DOI] [PubMed] [Google Scholar]
- 33. J‐S Y, Jhang WK, Choi YH, Lee B, Kim YH, Cho HJ, Eun BW, Kim J, Kim KW, Cho J, et al. Current status of pediatric critical care in Korea: results of 2015 national survey. J Korean Med Sci. 2018;33:e308. doi: 10.3346/jkms.2018.33.e308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Nolan JP, Berg RA, Andersen LW, Bhanji F, Chan PS, Donnino MW, Lim SH, Ma MH, Nadkarni VM, Starks MA, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry template for in‐hospital cardiac arrest: a consensus report from a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia). Circulation. 2019;140:e746–e757. doi: 10.1161/CIR.0000000000000710 [DOI] [PubMed] [Google Scholar]
- 35. Fraser LK, Fleming T, Miller M, Draper ES, McKinney PA, Parslow RC. Palliative care discharge from paediatric intensive care units in Great Britain. Palliat Med. 2010;24:608–615. doi: 10.1177/0269216310364200 [DOI] [PubMed] [Google Scholar]
- 36. Håkanson C, Öhlén J, Kreicbergs U, Cardenas‐Turanzas M, Wilson DM, Loucka M, Frache S, Giovannetti L, Naylor W, Rhee Y, et al. Place of death of children with complex chronic conditions: cross‐national study of 11 countries. Eur J Pediatr. 2017;176:327–335. doi: 10.1007/s00431-016-2837-0 [DOI] [PubMed] [Google Scholar]
- 37. Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260:1743–1748. doi: 10.1001/jama.260.12.1743 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Figures S1–S2


